Abstract
Campylobacter jejuni isolation is the standard for the diagnosis of this type of bacterial infection, but there have been no epidemiological studies of a large number of C. jejuni isolates from patients with Guillain-Barré syndrome (GBS) and Fisher syndrome (FS). For 13 years, stool specimens from GBS/FS patients have been sent from 378 hospitals throughout Japan to the Tokyo Metropolitan Institute of Public Health. A total of 113 strains (11%) were isolated from the stool specimens from 1,049 patients. The isolation rate did not differ by region. The rates were 22% for 449 patients with a history of diarrhea and 2% for the others. An additional 18 isolates were provided by various hospitals. There was no noticeable seasonal distribution in the onset of C. jejuni isolated from patients with GBS/FS. The male/female ratios were 1.7:1 for GBS and 2.2:1 for FS. The patient age range showed a peak in 10- to 30-year-old subjects who had GBS and in 10- to 20-year-old subjects who had FS. The predominance of young adults and male patients who had C. jejuni-associated GBS/FS may be related to the preponderance of young adults and male patients who had C. jejuni enteritis. The median interval from diarrhea onset to neurologic symptom onset was 10 days for GBS/FS. Penner's C. jejuni serotype HS:19 was more frequently present in GBS (67%) than in enteritis (6%) patients. HS:2 was more frequent in FS (41%) than in enteritis (14%) patients. These findings suggest that certain C. jejuni strains specifically trigger GBS and that others specifically trigger FS.
Guillain-Barré syndrome (GBS), the prototype of postinfectious autoimmune diseases, is characterized by acute onset of limb weakness and loss of tendon reflexes. Since the near elimination of poliomyelitis worldwide, GBS is the most frequent cause of acute flaccid paralysis, the mean annual incidence being 1.3 cases per 100,000 population (11). Fisher syndrome (FS) is characterized by acute onset of ophthalmoplegia, ataxia, and areflexia. It is considered a variant of GBS because some who present with FS progress to GBS. The annual incidence rate is estimated as 0.09 per 100,000 population (4). Of the identified microorganisms, the gram-negative bacterium Campylobacter jejuni, a leading cause of acute gastroenteritis, is the most frequent antecedent pathogen in GBS/FS (12). A comprehensive Japanese study showed 31% of 201 patients with GBS and 18% of 65 with FS seropositive for recent C. jejuni infection (16).
Serological studies are important for understanding the epidemiology of C. jejuni-associated GBS/FS, but there are no recommended methodologies as to the antigens to be used or the standards of judgment. A comparative study made in Japan and The Netherlands on the presence of anti-C. jejuni antibody in GBS showed that serological assay systems vary considerably between laboratories (15). C. jejuni isolation is the standard diagnosis for bacterial infection and should be used to assess the epidemiology of C. jejuni-associated GBS/FS. The latent period between preceding intestinal infection and the onset of GBS/FS, however, often exceeds the excretion period of viable C. jejuni cells in stools. Consequently, there have been no epidemiological studies done on a large number of C. jejuni isolates from patients. We analyzed the epidemiological features of more than 100 patients with GBS/FS from whom C. jejuni had been isolated and investigated the presence of Penner’s serotypes in the isolates.
MATERIALS AND METHODS
Stools of GBS and FS patients.
Stool specimens were sent from 378 hospitals throughout Japan to the Tokyo Metropolitan Institute of Public Health for C. jejuni isolation between December 1990 and November 2003. There was only one stool sampling per patient. The stools were collected in transport medium (SEEDSWAB no.1; Eiken, Tokyo Japan) immediately after patient admission. In addition to these isolates, 18 isolates from GBS (n = 15) and FS (n = 3) patients that had been provided by other hospitals were analyzed simultaneously. One of the authors (M.K.) reviewed the following information obtained from each primary physician: antecedent illness, initial symptoms, neurological signs during the illness, and clinical course. Rediagnoses were made based on the clinical criteria for GBS and FS (1, 23).
Bacterial strains.
GBS/FS-related strains that had been isolated by one of the authors (M.T.) or provided by other hospitals were used. A total of 554 strains isolated from other patients with enteritis with no neurological complications in Tokyo Metropolitan Hospitals (Komagome and Bokutoh) were the controls to test whether particular serotypes were increased in GBS/FS-related strains.
Stool culture for C. jejuni.
Each stool specimen was plated on three plates of solid selective media (i.e., CCDA, CM739, and SR155E; Oxoid, Ltd., Basingstoke, United Kingdom) without enrichment culture. The CCDA medium was incubated at 37°C for 72 h under microaerophilic conditions (5% O2, 7.5% CO2, 7.5% H2, and 80% N2) in an TE-HER CAMPYLO-INCUBATOR (Hirasawa, Tokyo, Japan). Suspicious colonies initially received a morphological check with a phase-contrast microscope. If an organism showed the typical curved, spiral morphology of Campylobacter, it was regarded as a type of C. jejuni or C. coli and replated on blood agar to obtain pure cultures. The identity of C. jejuni was confirmed by both biochemical tests and multiplex PCR techniques for assay for C. jejuni and C. coli. The biochemical tests used oxidase, hippurate hydrolysis, indoxyl acetate hydrolysis, and susceptibility to disks containing cephalothin (30 μg) and nalidixic acid (30 μg). Species-specific multiplex PCR were done with combined C. jejuni- and C. coli-specific primer sets (18, 29).
Serotyping.
Penner serotyping of C. jejuni was carried out by using a Campylobacter antisera Seiken Set (Denka Seiken, Tokyo Japan) according to the manufacturer's protocol. The antisera in the commercial set were composed of 25 groups of antisera as follows: group A, HS:1/44; group B, HS:2; group C, HS:3; group D, HS:4/13/16/43/50; group E, HS:5; group F, HS:6/7; group G, HS:8; group I, HS:10; group J, HS:11; group K, HS:12; group L, HS:15; group N, HS:18; group O, HS:19; group P, HS:21; group R, HS:23/36/53; group S, HS:27; group U, HS:31; group V, HS:32; group Y, HS:37; group Z, HS:38; group Z2, HS:41; group Z4, HS:45; group Z5, HS:52; group Z6, HS:55; and group Z7, HS:57.
Anti-ganglioside antibody assay.
Serum samples obtained during the first 4 weeks after onset, before immune treatment, were frozen and stored at −80°C until used. An enzyme-linked immunosorbent assay, performed as reported elsewhere (33), was used to measure immunoglobulin G (IgG) antibodies to GM1, GD1a, and GQ1b in serum. Serum was considered positive when the titer was ≥500.
Statistics.
Differences in frequency between groups were compared by using the Fisher exact test with SPSS 12.0J software (SPSS Inc., Chicago, Ill.). A difference was considered significant when the two-sided P value was <0.05.
RESULTS
Culture results.
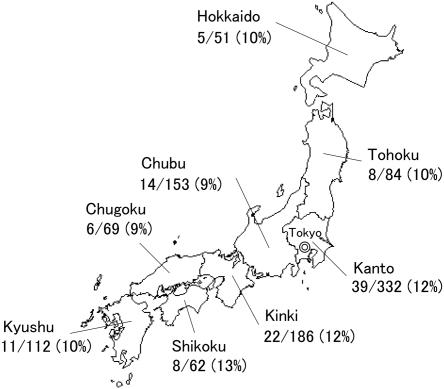
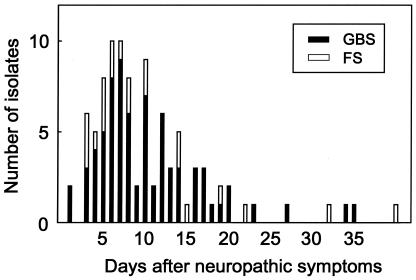
We obtained stool specimens from 1,049 patients with GBS (n = 763) or FS (n = 286). The median interval between neuropathy onset and stool sampling was 13 days (range, 1 to 150 days). Gastrointestinal symptoms occurred in 449 (43%) patients; upper respiratory symptoms occurred in 503 (48%) patients. A total of 113 C. jejuni strains (GBS, 87; FS, 26) (11%) were isolated from the 1,049 patients, although at least 11 patients had been treated with antibiotics. The combined isolation rate, 11% (GBS, 11%; FS, 9%), did not differ by region (Fig. 1). The rate was 22% for the 449 patients with a history of diarrhea and 2% for the the remaining patients (Table 1). Most C. jejuni-positive specimens were obtained within 2 weeks of neuropathy onset, some more than 1 month later (Fig. 2). Except for the of two siblings with GBS reported elsewhere (35), all cases were sporadic. C. coli (n = 2), C. curvus (n = 2), Campylobacter spp. (n = 12), and Arcobacter sp. (n = 1) were isolated from the C. jejuni-negative patients.
FIG. 1.
Isolation rate of C. jejuni by district in Japan.
TABLE 1.
Isolation rate of C. jejuni and antecedent illness in patients with GBS and FS
| Antecedent symptomsa | No. of stool specimens (%) from patients with:
|
|||
|---|---|---|---|---|
| GBS
|
FS
|
|||
| Total | C. jejuni positive | Total | C. jejuni positive | |
| GI only | 255 | 62 (24) | 49 | 17 (35) |
| GI plus URTI | 107 | 16 (15) | 38 | 4 (11) |
| URTI only | 209 | 2 (1) | 149 | 4 (3) |
| Fever only | 42 | 3 (7) | 10 | 0 |
| Others | 25 | 0 | 5 | 0 |
| None | 121 | 3 (2) | 31 | 1 (3) |
| Totalb | 759 | 86 (11) | 282 | 26 (9) |
GI, gastrointestinal infection; URTI, upper respiratory tract infection.
Eight cases were excluded because detailed information was not available.
FIG. 2.
Interval from the onset of neuropathic symptoms to the day stool specimens were obtained from C. jejuni-positive patients. Bars: ▪, GBS; □, FS.
Characteristics of C. jejuni-positive patients.
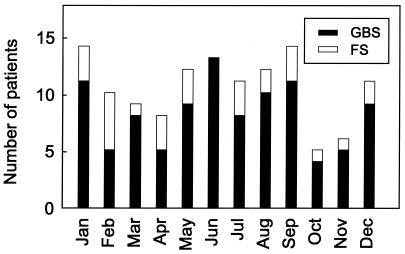
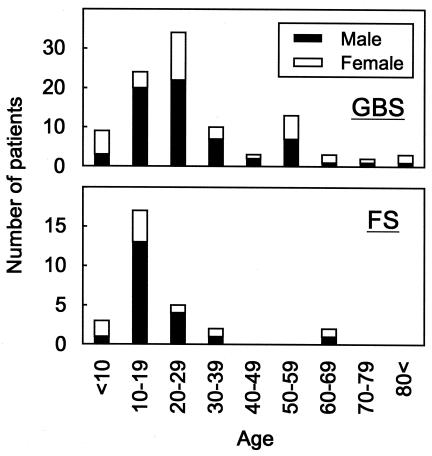
The seasonal distribution (Fig. 3) is lower in October and November. C. jejuni-associated GBS showed a peak in 10- to 30-year-olds (Fig. 4). C. jejuni-associated FS demonstrated a peak in 10- to 20-year-olds. Males predominated for both GBS (male/female ratio, 1.7:1) and FS (2.2:1).
FIG. 3.
Seasonal distributions of C. jejuni isolates in GBS and FS patients. Bars: ▪, GBS; □, FS.
FIG. 4.
Age distribution of C. jejuni-positive GBS and FS patients. Bars: ▪, males; □, females.
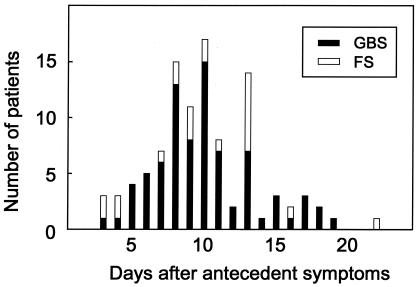
Antecedent symptoms in culture-positive patients were reported in 95% of 102 GBS patients and in 93% of 29 FS patients. The median latent period between antecedent symptoms and neuropathy onset was 10 days for both groups; within 2 weeks in most cases (Fig. 5). Gastrointestinal symptoms were most frequent in cases of GBS (90%) and FS (79%), often being accompanied by fever. Six (5%) patients with GBS/FS had a history of upper respiratory tract infectious symptoms only, and three (2%) had experienced only preceding fever. Anti-ganglioside IgG antibodies in serum were tested during the acute phase of illness in 120 of 131 patients (Table 2). Most patients had some antibodies; anti-GM1 and anti-GD1a IgG antibodies were frequent in GBS and anti-GQ1b IgG antibody in FS.
FIG. 5.
Interval from diarrhea onset to the onset of neuropathic symptoms. Bars: ▪, GBS; □, FS.
TABLE 2.
Anti-ganglioside antibodies in patients with GBS and FS from whom C. jejuni was isolated
| IgG antibody | No. of patients (%) with:
|
|
|---|---|---|
| GBS (n = 92) | FS (n = 28) | |
| Anti-GM1 | 68 (74) | 4 (14) |
| Anti-GD1a | 45 (49) | 5 (18) |
| Anti-GQ1b | 3 (3) | 23 (82) |
Serogroups of C. jejuni isolates.
HS:19 was more frequently isolated from GBS patients than from enteritis patients. The HS:2 and HS:4 complexes were isolated more frequently from FS patients than from enteritis patients. None of the GBS and FS isolates were HS:41.
DISCUSSION
Assessing the frequency of C. jejuni infection in GBS/FS patients is difficult since it depends on such varied factors as antecedent symptoms, the duration of convalescent excretion of the bacterium, and the kinds of antibiotics administered. Thus, few surveillance studies have included large numbers of patients. Kuroki et al. (17) reported that 30% of 46 GBS patients in the Kinki district of Japan had positive stool cultures. In a subsequent study, these authors isolated 13 strains (17%) of C. jejuni from 76 patients (9). In contrast, 8% of 103 patients had positive cultures in England (25), and 9% of 138 patients had positive cultures in The Netherlands (28). The isolation rate was 11% in the present study, which does not differ significantly from European values.
The latent period between intestinal infection and the onset of GBS/FS often exceeds the duration of convalescence excretion of the bacterium. GBS/FS patients therefore frequently have negative stool cultures. Kuroki's group (9) reported that all 13 positive stool specimens were obtained within 10 days after onset of GBS symptoms, and 9 of the 13 specimens were obtained within 5 days. We could isolate C. jejuni from stool specimens obtained more than 1 month after the onset of GBS (the 35th day) or FS (the 40th day). This finding is not exceptional because in some cases the excretion of C. jejuni in stools has continued for 6 to 9 weeks (14, 30).
There is no clear seasonal distribution of GBS in Western countries (11), whereas in northern China GBS peaks in late summer, which may be due to the high frequency of C. jejuni infection (10). In a previous study done in the Kinki district of Japan, the seasonal distribution of C. jejuni-associated GBS peaked in March, an autumn occurrence was relatively infrequent, and there was no seasonal difference found for the group of GBS patients without C. jejuni infection (9). We also detected no seasonal predominance. Autumn occurrences were relatively infrequent. Although the seasonality of C. jejuni enteritis in Japan is less pronounced than in other developed countries, which show a seasonal distribution with a well-defined summer peak (26), the incidence of C. jejuni enteritis tends to be higher from April to July (21).
TABLE 3.
Penner serogroup of isolates from GBS and FS and uncomplicated enteritis
| Penner serogroup | Serotype(s) | No. of C. jejuni isolates (%) from:
|
||
|---|---|---|---|---|
| GBS (n = 102)a | FS (n = 29) | Enteritis (n = 554) | ||
| A | 1, 44 | 5 (5) | 0 | 37 (7) |
| B | 2 | 6 (6) | 12 (41)c | 80 (14) |
| C | 3 | 1 (1) | 1 (3) | 21 (4) |
| D | 4, 13, 16, 43, 50 | 8 (8) | 11 (38)d | 69 (12) |
| E | 5 | 2 (2) | 0 | 6 (1) |
| F | 6, 7 | 1 (1) | 1 (3) | 10 (2) |
| G | 8 | 3 (3) | 0 | 21 (4) |
| O | 19 | 68 (67)b | 1 (3) | 34 (6) |
| U | 31 | 0 | 1 (3) | 1 (0.2) |
| Y | 37 | 3 (3) | 0 | 33 (6) |
| Z | 38 | 0 | 1 (3) | 2 (0.4) |
| Untypeable | 8 (8) | 1 (3) | 141 (25) | |
Two strains were serotyped as A/G or O/Y serogroups.
P < 0.001 (compared to the enteritis isolates; odds ratio [OR], 30.6; 95% confidence interval [CI], 17.9 to 52.4).
P < 0.001 (compared to the enteritis isolates; OR, 4.2; 95% CI, 1.9 to 9.1).
P < 0.001 (compared to the enteritis isolates; OR, 4.3; 95% CI, 1.9 to 9.5).
In North America and Europe, a bimodal age distribution has been reported for GBS, with peaks at 20 to 40 years and 60 to 70 years (2, 13). Males are more commonly affected by GBS than females (∼1.25:1) (11). In England the male/female ratio was 3.5:1 in the C. jejuni-seropositive group, whereas it was 1.5:1 in the C. jejuni-seronegative group (25). C. jejuni-associated GBS in northern China occurs mainly among children and young adults (10), the male/female ratio being 1.2:1 in C. jejuni-seropositive GBS patients and 0.8:1 in C. jejuni-seronegative patients. In the Kinki district of Japan, the age distribution showed a peak between 10 and 30 years (9). The male/female ratio was 2.4:1 for GBS patients who had had C. jejuni infection and 2.2:1 for the other GBS patients. In the present study, the age distribution showed a peak between 10 and 30 years for GBS and between 10 and 20 years for FS. A majority of male patients had both GBS and FS, the respective male/female ratios being 1.7:1 and 2.2:1. In English patients suffering from gastrointestinal symptoms, the highest C. jejuni isolation rates were for young adults, males predominating in the 15 to 24 years (1.7:1) and 45 to 54 years (1.6:1) age groups (26). The dominance of young adult and male patients among those with C. jejuni infection may therefore partly explain the findings for C. jejuni-associated GBS/FS. In England, the median interval between the onset of diarrhea and neuropathic symptoms was 9 days (range, 2 to 20) for 19 GBS patients (25). In our study, the median interval was 10 days (range, 1 to 24) for 115 GBS/FS patients.
Penner's serotyping system is a useful phenotyping technique for C. jejuni and C. coli (24). The system can divide C. jejuni and C. coli into about 60 types. C. jejuni has been isolated from patients' stools at GBS onset. A large number of Penner serotypes have been reported in the literature: HS:1, HS:2, HS:4, HS:5, HS:10, HS:13/65, HS:16, HS:19, HS:23, HS:35, HS:37, HS:41, HS:44, and HS:64 (5), but Kuroki's group showed that 75% of 16 isolates from GBS patients were HS:19 and that 1 of 2 isolates from FS patients was HS:2 (22). Elsewhere we reported that in Japan HS:19 strains are significantly over-represented in GBS patients, accounting for 52% of 31 isolates from GBS patients but only 5% of 215 control isolates (34). HS:2 was found to be over-represented in FS patients (present in 71% of the patients versus 38% of the controls), but only 7 isolates from FS patients were studied. In South Africa, 6 of 9 GBS isolates were HS:41; this serotype accounts for only 0.1% of enteritis strains (8). In contrast, in The Netherlands and Belgium only two isolates from 12 GBS patients were HS:19, and none were HS:41 (5). Only one isolate from four FS patients was HS:2 (5). Our study confirms that GBS is significantly associated with HS:19 and that statistically FS is associated with HS:2. None of our C. jejuni isolates from GBS patients were HS:41. These findings are a strong indication that certain C. jejuni strains trigger the development of GBS, others the development of FS.
HS:19 strains, whether isolated from GBS patients or enteritis patients without neurological involvement, were related clonally (7, 19, 22), whereas clonality was lacking for other serotypes associated with GBS (5, 6). The hypothesis that a “bad bug causes GBS/FS” cannot be dismissed. The methods used may simply lack the power to detect particular C. jejuni strain determinants related to GBS/FS. There is cumulative evidence of molecular mimicry between human gangliosides and that the C. jejuni lipo-oligosaccharide (LOS) causes GBS/FS (31). Anti-GM1 and anti-GD1a IgG antibodies have been detected in patients who developed GBS subsequent to C. jejuni enteritis. Sensitization with a GM1-like LOS, as well as with GM1 ganglioside, has produced an animal model of GBS (32, 36). Analysis of the genes involved in the synthesis of ganglioside-like LOS may be of great importance for clarifying which C. jejuni strains involved in the pathogenesis of GBS/FS. The presence of LOS synthesis genes (cst-II, cgtA, and cgtB) is associated statistically with GBS-related isolates (20). GQ1b ganglioside is a target molecule for IgG antibody in FS (3), and all C. jejuni strains studied that bore the GQ1b epitope had cst-II, an essential gene for production of GQ1b-like LOS (27). Whether these genes are present in our GBS/FS isolates needs to be investigated, as well as whether their presence is more frequent than in the enteritis controls.
Acknowledgments
This study was supported in part by grants-in-aid from the Ichiro Kanehara Foundation, by the Kanae Foundation for Life & Socio-Medical Science, by the Japan Intractable Diseases Research Foundation, by a grant for Scientific Research (B) (KAKENHI 14370210) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, by a Research Grant for Neuroimmunological Diseases from the Ministry of Health, Labour, and Welfare of Japan, by a Health Sciences Research Grant (Research on Psychiatric and Neurological Diseases and Mental Health) from the Ministry of Health, Labour, and Welfare of Japan, and by a grant from the Human Frontier Science Program (RGP 38/2003).
We thank the Divisions of Clinical Microbiology of the Tokyo Metropolitan Hospitals (Komagome and Bokutoh) for the isolation of the sporadic enteritis strains.
REFERENCES
- 1.Asbury, A. K., and D. R. Cornblath. 1990. Assessment of current diagnostic criteria for Guillain-Barré syndrome. Ann. Neurol. 27(Suppl.):S21-S24. [DOI] [PubMed] [Google Scholar]
- 2.Boucquey, D., C. J. M. Sindic, M. Lamy, M. Delmée, J. P. Tomasi, and E. C. Laterre. 1991. Clinical and serological studies in a series of 45 patients with Guillain-Barré syndrome. J. Neurol. Sci. 104:56-63. [DOI] [PubMed] [Google Scholar]
- 3.Chiba, A., S. Kusunoki, T. Shimizu, and I. Kanazawa. 1992. Serum IgG antibody to ganglioside GQ1b is a possible marker of Miller Fisher syndrome. Ann. Neurol. 31:677-679. [DOI] [PubMed] [Google Scholar]
- 4.Emilia-Romagna Study Group on Clinical and Epidemiological Problems in Neurology. 1998. Guillain-Barré syndrome variants in Emilia-Romagna, Italy, 1992-3: incidence, clinical features, and prognosis. J. Neurol. Neurosurg. Psychiatry 65:218-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Endtz, H. P., C. W. Ang, N. van Den Braak, B. Duim, A. Rigter, L. J. Price, D. L. Woodward, F. G. Rodgers, W. M. Johnson, J. A. Wagenaar, B. C. Jacobs, H. A. Verbrugh, and A. van Belkum. 2000. Molecular characterization of Campylobacter jejuni from patients with Guillain-Barré and Miller-Fisher syndrome [sic]. J. Clin. Microbiol. 38:2297-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engberg, J., I. Nachamkin, V. Fussing, G. M. McKhann, J. W. Griffin, J. C. Piffaretti, E. M. Nielsen, and P. Gerner-Smidt. 2001. Absence of clonality of Campylobacter jejuni in serotypes other than HS:19 associated with Guillain-Barré syndrome and gastroenteritis. J. Infect. Dis. 184:215-220. [DOI] [PubMed] [Google Scholar]
- 7.Fujimoto, S., B. M. Allos, N. Misawa, C. M. Patton, and M. J. Blaser. 1997. Restriction fragment length polymorphism analysis and random amplified polymorphic DNA analysis of Campylobacter jejuni strains isolated from patients with Guillain-Barré syndrome. J. Infect. Dis. 176:1105-1108. [DOI] [PubMed] [Google Scholar]
- 8.Goddard, E. A., A. J. Lastovica, and A. C. Argent. 1997. Campylobacter O:41 isolation in Guillain-Barré syndrome. Arch. Dis. Child. 76:526-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hao, Q., T. Saida, S. Kuroki, M. Nushimura, M. Nukina, H. Obayashi, and K. Saida. 1998. Antibodies to gangliosides and galactocerebroside in patients with Guillain-Barré syndrome with preceding Campylobacter jejuni [sic] and other identified infections. J. Neuroimmunol. 81:116-126. [DOI] [PubMed] [Google Scholar]
- 10.Ho, T. W., B. Mishu, C. Y. Li, C. Y. Gao, D. R. Cornblath, J. W. Griffin, A. K. Asbury, M. J. Blaser, and G. M. McKhann. 1995. Guillain-Barré syndrome in northern China: relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain 118:597-605. [DOI] [PubMed] [Google Scholar]
- 11.Hughes, R. A. C., and J. H. Rees. 1997. Clinical and epidemiologic features of Guillain-Barré syndrome. J. Infect. Dis. 176(Suppl. 2):S92-S98. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs, B. C., P. H. Rothbarth, F. G. A. van der Meché, P. Herbrink, P. I. M. Schmitz, M. A. de Klerk, and P. A. van Doorn. 1998. The spectrum of antecedent infections in Guillain-Barré syndrome: a case-control study. Neurology 51:1110-1115. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan, J. E., L. B. Schonberger, E. S. Hurwitz, and P. Katona. 1983. Guillain-Barré syndrome in the United States, 1978-1981: additional observations from the national surveillance system. Neurology 33:633-637. [DOI] [PubMed] [Google Scholar]
- 14.Kapperud, G., J. Lassen, S. M. Ostroff, and S. Aasen. 1992. Clinical features of sporadic Campylobacter infections in Norway. Scand. J. Infect. Dis. 24:741-749. [DOI] [PubMed] [Google Scholar]
- 15.Koga, M., C. W. Ang, N. Yuki, B. C. Jacobs, P. Herbrink, F. G. A. van der Meché, K. Hirata, and P. A. van Doorn. 2001. Comparative study of preceding Campylobacter jejuni infection in Guillain-Barré syndrome in Japan and The Netherlands. J. Neurol. Neurosurg. Psychiatry 70:693-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koga, M., N. Yuki, M. Takahashi, K. Saito, and K. Hirata. 1998. Close association of IgA anti-ganglioside with antecedent Campylobacter jejuni in Guillain-Barré syndrome. J. Neuroimmunol. 81:138-143. [DOI] [PubMed] [Google Scholar]
- 17.Kuroki, S., T. Saida, M. Nukina, T. Haruta, M. Yoshioka, Y. Kobayashi, and H. Nakanishi. 1993. Campylobacter jejuni strains from patients with Guillain-Barré syndrome belong mostly to Penner serogroup 19 and contain β-N-acetylglucosamine residues. Ann. Neurol. 33:243-247. [DOI] [PubMed] [Google Scholar]
- 18.Linton, D., A. J. Lawson, R. J. Owen, and J. Stanley. 1997. PCR detection, identification to species level, and fingerprinting of Campylobacter jejuni and Campylobacter coli direct from diarrheic samples. J. Clin. Microbiol. 35:2568-2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nachamkin, I., J. Engberg, M. Gutacker, R. J. Meinersman, C. Y. Li, P. Arzate, E. Teeple, V. Fussing, T. W. Ho, A. K. Asbury, J. W. Griffin, G. M. McKhann, and J. C. Piffaretti. 2001. Molecular population genetic analysis of Campylobacter jejuni HS:19 associated with Guillain-Barré syndrome and gastroenteritis. J. Infect. Dis. 184:221-226. [DOI] [PubMed] [Google Scholar]
- 20.Nachamkin, I., J. Liu, M. Li, H. Ung, A. P. Moran, M. M. Prendergast, and K. Sheikh. 2002. Campylobacter jejuni from patients with Guillain-Barré syndrome preferentially expresses a GD1a-like epitope. Infect. Immun. 70:5299-5303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute of Infectious Diseases and Infectious Diseases Control Division, Ministry of Health and Welfare of Japan. 1999. Campylobacter enteritis 1995-1998. Infect. Agents Surv. Rep. 20:107-108. (In Japanese.) [Google Scholar]
- 22.Nishimura, M., M. Nukina, S. Kuroki, H. Obayashi, M. Ohta, J. J. Ma, T. Saida, and T. Uchiyama. 1997. Characterization of Campylobacter jejuni isolated from patients with Guillain-Barré syndrome. J. Neurol. Sci. 153:91-99. [DOI] [PubMed] [Google Scholar]
- 23.Odaka, M., N. Yuki, and K. Hirata. 2001. Anti-GQ1b IgG antibody syndrome: clinical and immunological range. J. Neurol. Neurosurg. Psychiatry 70:50-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Penner, J. L., and J. N. Hennessy. 1980. Passive hemagglutination technique for serotyping Campylobacter fetus subsp. jejuni on the basis of soluble heat-stable antigens. J. Clin. Microbiol. 12:732-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rees, J. H., S. E. Soudain, N. A. Gregson, and R. A. C. Hughes. 1995. Campylobacter jejuni infection and Guillain-Barré syndrome. N. Engl. J. Med. 333:1374-1379. [DOI] [PubMed] [Google Scholar]
- 26.Skirrow, M. B. 1987. A demographic survey of campylobacter, salmonella, and shigella infections in England: a public health laboratory service survey. Epidemiol. Infect. 99:647-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Belkum, A., N. van den Brrak, P. Godschalk, W. Ang, B. Jacobs, M. Gilbert, W. Wakarchuk, H. Verbrugh, and H. Endtz. 2001. A Campylobacter jejuni gene associated with immune-mediated neuropathy. Nat. Med. 7:752-753. [DOI] [PubMed] [Google Scholar]
- 28.van Koningsveld, R., P. A. van Doorn, P. I. M. Schmitz, C. W. Ang, and F. G. A. van der Meché. 2000. Mild forms of Guillain-Barré syndrome in an epidemiologic survey in The Netherlands. Neurology 54:620-625. [DOI] [PubMed] [Google Scholar]
- 29.Winter, D. K., A. E. O'Leary, and M. F. Slavik. 1997. Rapid PCR with nested primers for direct detection of Campylobacter jejuni in chicken washes. Mol. Cell. Probes 11:267-271. [DOI] [PubMed] [Google Scholar]
- 30.Wright, E.P. 1982. Duration of excretion period of Campylobacter jejuni in human subjects, p. 294-298. In D. G. Newell (ed.), Campylobacter. MTP Press, Lancaster, United Kingdom.
- 31.Yuki, N. 2001. Infectious origins of, and molecular mimicry in Guillain-Barré and Fisher syndromes. Lancet Infect. Dis. 1:29-37. [DOI] [PubMed] [Google Scholar]
- 32.Yuki, N., K. Susuki, M. Koga, Y. Nishimoto, M. Odaka, K. Hirata, K. Taguchi, T. Miyatake, K. Furukawa, T. Kobata, and M. Yamada. 2004. Carbohydrate mimicry between human ganglioside GM1 and Campylobacter jejuni lipooligosaccharide causes Guillain-Barré syndrome. Proc. Natl. Acad. Sci. USA 101:11404-11409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yuki, N., Y. Tagawa, F. Irie, Y. Hirabayashi, and S. Handa. 1997. Close association of Guillain-Barré syndrome with antibodies to minor monosialogangliosides GM1b and GM1α. J. Neuroimmunol. 74:30-34. [DOI] [PubMed] [Google Scholar]
- 34.Yuki, N., M. Takahashi, Y. Tagawa, K. Kashiwase, K. Tadokoro, and K. Saito. 1997. Association of Campylobacter jejuni serotype with antiganglioside antibody in Guillain-Barré syndrome and Fisher' s syndrome. Ann. Neurol. 42:28-33. [DOI] [PubMed] [Google Scholar]
- 35.Yuki, N., and Y. Tsujino. 1995. Familial Guillain-Barré syndrome subsequent to Campylobacter jejuni enteritis. J. Pediatr. 126:162.. [DOI] [PubMed] [Google Scholar]
- 36.Yuki, N., M. Yamada, M. Koga, M. Odaka, K. Susuki, Y. Tagawa, S. Ueda, T. Kasama, A. Ohnishi, S. Hayashi, H. Takahashi, M. Kamijo, and K. Hirata. 2001. Animal model of axonal Guillain-Barré syndrome induced by sensitization with GM1 ganglioside. Ann. Neurol. 49:712-720. [PubMed] [Google Scholar]