Abstract
Background
In studies of recurrent events, it is common to consider a person who has suffered a disease episode and received curative treatment to be not at risk of suffering a new episode for a duration of time. It is a common practice to deduct this duration from the person’s observation time in the statistical analysis of the incidence data.
Methods
We examined the concepts of incidence and protective efficacy from a real life point of view. We developed simple formulae to show the relationship between the incidence rate and protective efficacy between analyses with and without deducting the curative treatment time from the observation time. We used a malaria chemoprevention and a malaria vaccine study, both previously published, to illustrate the differences.
Results
Applying the formulae we derived to a range of disease incidence that covered the two case studies, we demonstrated the divergence of the two sets of estimates when incidence rate is approximately 1 per person-year or higher. In the malaria chemoprevention study, incidence was 5.40 per person-year after the deduction of curative treatment time from observation time but 4.48 per person-year without the deduction. The chemoprevention offered 56.6 and 50.7% protection calculated with and without the deduction, respectively. In the malaria vaccine study, where disease incidence was much lower than one, the results between the two ways of analysis were similar. For answering real life questions about disease burden in the population in a calendar year and the reduction that may be achieved if an intervention is implemented, the definition without deduction of curative treatment time should be used.
Conclusions
The practice of deducting curative treatment time from observation time is not wrong, but it is not always the best approach. Investigators should consider the appropriateness of the two analytic procedures in relation to the specific research aims and the intended use of the results.
Electronic supplementary material
The online version of this article (doi:10.1186/s12874-017-0350-4) contains supplementary material, which is available to authorized users.
Keywords: Incidence rate, Prevention trials, Protective efficacy, Recurrent events
Background
Incidence rate is defined as the number of events divided by the duration of person-time [1–4]. In regression analysis of disease incidence to evaluate intervention effects, e.g. by Poisson regression or Negative Binomial regression, the duration of person-time is used as an off-set variable and the way the duration is defined affects the estimated incidence and incidence rate ratio [5]. In time-to-event analysis, the duration determines who is to be included in the risk set for evaluation. While the case definition of a disease episode (in the numerator) and the technical aspects of statistical analysis methods are often detailed in study reports, the issue of defining the denominator of incidence rates has received less attention than it should.
In prevention trials and epidemiological studies of disease incidence, the numerator of an incidence rate is often defined by the occurrence of a set of signs and symptoms and objective measurements plus the fact of presentation to a health care facility for treatment. For example, in a malaria vaccine trial, malaria was defined as temperature ≥ 37.5 °C or self-report of fever in the last 24 h, malaria parasitemia ≥ 2500 per μL, and presentation to a health care facility [6, 7].
Definitions of the denominator of an incidence rate vary subtly. Table 1 shows the denominators given in some popular references. Some of them used the phrase “at risk” in the definition, but some did not. Porta’s Dictionary of Epidemiology described a “person-time incidence rate” that used “number of person-time units at risk” in the denominator and another definition that does not involve time at all (the latter is not shown in table).
Table 1.
The denominators of incidence rate as defined in some references
It is a common practice to consider some duration of time after each episode of disease as a time period that the person is not “at risk” of the disease. For example, in studies of malaria vaccines and chemoprevention, a person who is known to have clinical malaria is given curative treatment. Antimalarials persist at therapeutic levels for a variable period depending on the pharmacokinetics of the specific drugs [6–8]. It is often assumed that malaria symptoms occurring “early” (defined variably) after initiation of curative treatment are the results of the initial infection and not the result of a new infection. The early occurrences of these symptoms are not counted as disease episodes in the numerator. A variable amount of time is then deducted from the person-time in the denominator of the incidence rate, usually 7 to 28 days depending on the specific malaria drugs used, apparently with the aim of excluding the period during which the person is supposed to be not at risk. The person-time is then said to be “adjusted for anti-malaria drug use” [6–9]. Similar practices can be found in other therapeutic areas, such as the management of pulmonary exacerbations in cystic fibrosis [10, 11] and prevention of pneumonia [12].
We define “observation time” as the total duration of time a subject is under observation, i.e. from entry to exit from study minus temporary absence from observation (if any), e.g. due to migration. Deducting curative treatment time from observation time gives “time at risk”, a denominator that is smaller than that based on observation time. For brevity, we refer to the definitions of incidence rate with and without the deduction of treatment time as “time at risk” definition and “observation time” definition. Not much discussion has been dedicated to the appropriateness of this practice of deducting the curative treatment time. Some statistics textbooks briefly mention this issue and adopt the time at risk definition [10, 11].
We maintain that not counting the early occurrences of symptoms in the numerator does not necessitate the deduction of the treatment time from the denominator, and that the practice of the deduction does not answer the questions policy makers and health programme managers seek to answer. From a real life point of view, whether in terms of efficacy or effectiveness, it is useful to know the disease burden in terms of how many disease episodes there are per calendar year in a population and how many episodes may be prevented by the introduction of an intervention per calendar year. In this context, time is the observation time a health policy or program is under evaluation. The practice of subtracting a period of curative treatment time from the actual observation time does not answer these questions. As an analogy, we find the “observation time” definition similar to intention-to-treat analysis, while the “time at risk” definition similar to per-protocol analysis [13, 14]. Intention-to-treat analysis aims to obtain the fairest estimate of the intervention benefit that would be realized in practice, and therefore does not exclude participants who deviate from the protocol in ways which could occur in real life situations, such as taking other medications or non-adherence to the intervention. In studies of preventive interventions, curative treatment of disease temporarily reduces the risk of a future disease episode. This is a feature of routine health care and so excluding the curative treatment time from the analysis is not compatible with research questions concerning real life situations.
Methods
Relationship between estimates
For the purpose of illustration, consider a 2-arm, randomized controlled trial of a preventive intervention versus placebo control.
Disease incidence
Let the observation time for subject i in group j be defined as Tij = min(τ, Cij), where τ is the maximum follow-up duration fixed by study design and Cij is the non-informative right-censored total duration of time subject i in group j is under observation, i.e. the time from entry to exit from study minus duration of temporary absence from observation (if any), e.g. due to migration, and j = 0 for control group and 1 for intervention group. Let Tj = ∑iTij be the total amount of observation time summed across all subjects in group j. Let Dijk be the curative treatment time for subject i in group j after the k-th event. To simplify notations and focus on the concepts instead of technicalities, we assume in this article that Di1k = Di0k = D. However, this assumption is not central to our argument and we will revisit this in the Discussion section. The practice of deducting curative treatment time from observation time assumes that there is no new episode of disease during the treatment period, D; any symptom occurrence observed in this period are considered relapses and not counted in the numerator.
Let Eij denote the number of episodes for subject i in group j. Let Ej = ∑iEij be the total number of episodes observed in group j. Let Ij be the incidence rate defined as total number of episodes divided by Tj, without deduction of the treatment time after each episode, in group j. That is, the “observation time” definition of incidence rate is:
If the curative treatment time is deducted from the observation time after each event, the “time at risk” definition of incidence rate obtained is approximately:
or equivalently
| 1 |
Equation 1 is approximate because if the last episode occurred within duration D from the end of the observation time, the deduction for the last episode would be smaller than D. In the Additional file 1 we show that an improved estimate of the deduction of treatment time after the last event in subject i of group j is
Therefore, the “time at risk” definition of incidence rate is
| 2 |
As will be seen in Fig. 1, for realistic values of Tj and D in public health studies, Eq. 1 gives very good approximation to Eq. 2. We focus on Eq 1 in subsequent discussion for simplicity.
Fig. 1.

Incidence rates defined with and without the deduction of curative treatment time
If D = 0, I*j = Ij. Otherwise, I*j > Ij due to the smaller denominator in I*j. In other words, the incidence rate according to the “time at risk” definition is larger than that of the “observation time” definition.
Furthermore, from (1), it can be shown that Ej = (I*jTj)/(1 + I*jD). Therefore,
| 3 |
From Eq. 3, it can be seen again that Ij is smaller than I*j unless D equals zero.
Protective efficacy
Protective efficacy (PE) is defined as 1 minus incidence rate ratio [15, 16]. We use the phrase here statistically to mean 1 – incidence rate ratio, without making a distinction between the contexts of efficacy or effectiveness studies.
Let R = I1/I0 and R* = I*1/I*0, i.e. the incidence rate ratio comparing the intervention to control group based on the “observation time” and “time at risk” definitions, respectively. By substituting I*1 = R*I*0 into Eq. 3:
| 4 |
Let PE = 1 − R and PE* = 1 − R*.
| 5 |
As such, PE* > PE unless D equals zero. The equality in Eq. 5 also holds if PE = 0. As such, for the purpose of testing a null hypothesis of no intervention effect, using PE or PE* does not matter. However, the “time at risk” definition tends to give a stronger estimate of protective efficacy than the “observation time” definition unless there is no intervention effect at all.
Results
Figure 1 illustrates the discrepancy between the incidence rates defined with and without the deduction of curative treatment time. This figure covers the range of incidence rates that includes the two case studies we will discuss. The x-axis is the number of episodes observed in one calendar year. The incidence rates based on “observation time” (solid line) formed a 45° line to the x-axis. In contrast, the incidence rates based on “time at risk” after deduction of 14 days or 28 days of treatment time (typical in malaria studies) following each episode had an accelerating slope. They began to depart visibly from the rates based on the “observation time” definition when incidence was about 1 per year. The gap expanded as incidence increased. Furthermore, the approximate (Eq. 1) and precise (Eq. 2) versions of the incidence rate estimates based on the “time at risk” definition were practically identical when 14 days were deducted. There was visible but minor difference between the approximate and precise versions when 28 days were deducted. This demonstrates the usefulness of Eq. 1.
Figure 2 contrasts the two definitions of protective efficacy in the cases of incidence in the control group being 0.1, 2, and 5 episodes in one calendar year of observation time, which roughly correspond to the range in the two case studies below. The lines for deduction of 14 and 28 days were practically identical at low incidence (0.1 per year), and hence only the line for deduction of 14 days was shown for 0.1 per year. For low incidence (0.1 per year), PE* and PE almost exactly formed a 45° line, indicating strong agreement. As incidence became higher, PE* became larger than PE. The deduction of 28 days generated bigger difference between PE* and PE than the deduction of 14 days did.
Fig. 2.
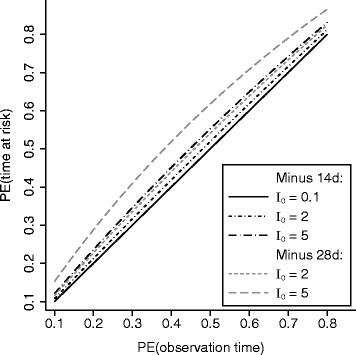
Differences in estimates of protective efficacy with and without the deduction of curative treatment time - PE(time at risk) and PE(observation time), respectively - depend on background incidence
We use two different malaria prevention studies to illustrate.
Study 1. Chemoprevention of malaria in Ugandan children
Three hundred and ninety three infants at 6 months of age were randomized to no chemoprevention, monthly sulfadoxine-pyrimethamine (SP), daily trimethoprim-sulfamethoxazole (TS), or monthly dihydroartemisinin-piperaquine (DP) [8]. Chemoprevention ended at the age of 24 months. Passive surveillance of malaria incidence was conducted. A malaria diagnosis was defined as temperature at least 38.0° Celsius or history of fever in the previous 24 h and a positive thick blood smear. Malaria was treated according to local clinical guidelines using either artemether-lumefantrine or quinine. The study deducted 14 days after each malaria attack from the denominator. Negative binomial regression was used to analyze the incidence data.
Pooling four groups, the overall incidence was 5.404 per person-year at risk (PYAR) after the deduction of curative treatment time from the observation time (Table 2). Using Eq. 3, the incidence based on observation time would be 4.477 per year. The former estimate of incidence was about 1 episode per time unit higher than the latter. DP was found to offer the highest protection: based on the “time at risk” definition this was 1–3.017/6.953 = 56.6%, but using Eq. 5, the PE based on observation time was lower: 0.566/[1 + 3.017 × (14/365.25)] = 0.507, or 50.7%.
Table 2.
Chemoprevention of malaria in Ugandan children, 2010–2013
| Trial arm | Sample size | Number of events | Person-year at riska | Event/PYAR | Event/observation timeb |
|---|---|---|---|---|---|
| Control | 98 | 760 | 109.3 | 6.953 | 5.490 |
| SP | 98 | 725 | 107.8 | 6.725 | 5.347 |
| TS | 99 | 609 | 116.8 | 5.214 | 4.346 |
| DP | 98 | 366 | 121.3 | 3.017 | 2.704 |
| Overall | 393 | 2460 | 455.2 | 5.404 | 4.477 |
aObservation time minus malaria curative treatment time
bEstimated using Eq. 3
Study 2. RTS,S malaria vaccine in Mozambican children
One thousand four hundred ninety three children aged 1 to 4 years were recruited and randomized to receive either control vaccines or RTS,S malaria vaccine [6, 7]. The surveillance period started at 14 days after the third dose of vaccine, which was 2.5 months post-enrollment. Surveillance continued to 21.0 months post-enrollment. Malaria was defined as temperature ≥ 37.5 °C or reporting fever in the last 24 h and malaria parasitemia ≥ 2500 per μL. After exclusion of 3 children from per-protocol analysis, 1490 were included in the main analysis. Several drugs were used in the treatment of malaria. In the analysis of multiple episode data, a child was considered not at risk for 28 days after the onset of the previous event due to treatment [6, 7].
The overall disease incidence was 0.351 events per PYAR according to the “time at risk” definition (Table 3). Using Eq. 3 to estimate the incidence based on observation time, the incidence was 0.342. The PE based on the definition with deduction of curative treatment time was 1–0.309/0.395 = 21.9%. Using Eq. 5, based on observation time, a similar PE of 21.4% was obtained. The PE in the trial report was adjusted for age, bednet use, and other covariates, and therefore was somewhat different [7].
Table 3.
RTS,S Malaria vaccine in Mozambican children, 2003–2005
| Trial arm | Sample size | Number of event | Person-year at riska | Events/PYAR | Events/observation timeb |
|---|---|---|---|---|---|
| Control | 745 | 384 | 972.1 | 0.395 | 0.383 |
| RTS,S | 745 | 310 | 1004.5 | 0.309 | 0.301 |
| Overall | 1490 | 694 | 1976.6 | 0.351 | 0.342 |
aObservation time minus malaria curative treatment time
bEstimated using Eq. 3
Discussion
Epidemiological studies and clinical trials typically are meticulous about case definitions and statistical analysis techniques. Less attention has been given to the denominator of an incidence rate. The definitions of the numerator and denominator are two distinct matters. We considered the denominator while taking the numerator definition as given. While some textbooks and references do use the phrase “at risk” in the definition, it is not clear what exactly “at risk” means. Some investigations, such as the malaria prevention trials we discussed, consider a person not at risk while they were receiving curative treatments because the curative treatments were supposed to temporarily make the person non-susceptible to the target disease. This definition appears to interpret “at risk” to mean “biologically susceptible”. However, it is possible to interpret “at risk” as being under observation. For example, in the RTS,S vaccine trial in Mozambique, children were also considered not at risk if they were absent from the study area for at least 2 weeks [6, 7]. Perhaps the children were biologically susceptible to malaria during their absence, but they were not under observation by the study team and this was the ground for excluding the duration of time from the statistical analysis. Interpreting this way, time at risk is equivalent to observation time.
In our opinion, both the definitions of incidence rate and protective efficacy with or without the deduction of treatment time are legitimate. However, they concern different research questions. We maintain that, from a real life and public health point of view, the observation time definition tends to be more appropriate, because a policy maker or programme manager is likely more concerned about what would occur in the community in a calendar year if an intervention is or is not implemented. In this context, time refers to observation time in the real life situation. The choice between the two denominators may or may not make a practically important difference. This depends on the disease incidence in the population. When disease incidence is high, from a real life perspective, disease incidence and protective efficacy can be substantially over-estimated by the common practice. When disease incidence is low, the difference may not be noticeable. These issues should be considered in study designs and in planning analyses.
It is good that many studies do present enough information that allows reconstruction of the incidence rate from one definition to another. The equations we presented should facilitate this. The equations do not directly provide confidence intervals because that would require individual level data instead of published estimates. But they can be applied to both the point estimates and the lower and upper limits of their confidence intervals in published reports to obtain the reconstructed point and interval estimates. However, this conversion based on published information is only possible for crude incidence. It is not possible for covariate (or random effects) adjusted analysis as the individual level data is typically not available to readers. As such, it is important for investigators to consider the appropriateness of the two analysis approaches in relation to the specific research context and accordingly provide the adjusted analysis to readers if needed. It is quite common that clinical trials present both intention-to-treat analysis and per protocol analysis results. Similarly, investigators may consider presenting both versions of incidence rate and protective efficacy. They are not mutually exclusive. In the derivation of the conversion formulae in the Methods we made an assumption of constant curative treatment time. The assumption was made primarily for brevity of exposition. It is not central to the conclusions we made. Similar to the paucity of discussion on the present topic, there is also a paucity of information about the constant curative treatment time assumption. It will be helpful if studies on disease prevention also provide information on curative treatments. The accuracy of the conversion formulae developed in the Methods section would be affected if the distribution of curative treatment time is neither constant nor random. We can imagine the possibility that curative treatment may depend on number of previous disease episodes or disease severity, possibly leading to unequal distribution of curative treatment times across intervention groups. If that occurs, the results based on the “time at risk” definition would be difficult to interpret, regardless of using the conversion formulae or not. In our opinion, that would strengthen the motivation for using the “observation time” definition.
If the “time at risk” definition is chosen, it is important to present the operational details, which have not been always clear in the literature. For example, it is quite common in vaccine studies to start observation when a participant is enrolled, but the analysis time starts only when the series of vaccination (e.g. three doses) is completed. If a disease episode is observed before the date of completion of vaccine series but the curative treatment time extends beyond this date, we believe the logic behind the choice of the “time at risk” definition should mandate deduction of the part of curative treatment time that is after this date. Insufficient description hinders understanding and reproducibility. An alternative approach, which avoids making specific assumptions about at-risk status during curative treatment, is to use a time-varying covariate [10, 11] for the preventive intervention variable so that the protective efficacy may change according to curative treatment history.
Conclusions
The practice of deducting treatment time from observation time is not wrong, but it is not always the best approach. It is important for investigators to consider the appropriateness of the two forms of analysis in relation to the specific research aims and the intended use of the results.
Acknowledgments
None.
Funding
This work was supported by the National Research Foundation, Singapore, under its Clinician Scientist Award (Award No. NMRC/CSA/0039/2012) administered by the Singapore Ministry of Health’s National Medical Research Council. The funding body played no role in any aspect of the conduct of this research.
Availability of data and materials
Not applicable; this is a statistical methodological study with illustration using information from publicly available publications (references [7, 8]).
Authors’ contribution
YBC, YX, MC and PM participated in the conceptualization and design of the work. YBC and PM developed the derivation of the formulae in the main text. YX developed the supplementary materials. YBC wrote the first draft of the manuscript. MC wrote the specific example about time on anti-malaria drug. YBC, YX, MC and PM participated in critical review and revision of the manuscript and approved the submission.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable; no human subjects.
Ethics approval and consent to participate
Not applicable; no human subjects or animal use.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- DP
Dihydroartemisinin-piperaquine
- PE
Protective efficacy
- PYAR
Person-year at risk
- SP
Sulfadoxine-pyrimethamine
- TS
Trimethoprim-sulfamethoxazole
Additional file
“Time not at risk” and its approximation. Derivation of the equations for approximating time not at risk. (DOCX 33 kb)
Contributor Information
Yin-Bun Cheung, Email: yinbun.cheung@duke-nus.edu.sg.
Ying Xu, Email: tinayxu@gmail.com.
Matthew Cairns, Email: matthew.cairns@lshtm.ac.uk.
Paul Milligan, Email: paul.milligan@lshtm.ac.uk.
References
- 1.Hennekens CH, Buring J. Epidemiology in medicine. Philadelphia: Lippincott Williams & Wilkins; 1987. [Google Scholar]
- 2.Smith P, Marrow RH. Field trials of health interventions in developing countries: a toolbox. London: Macmillan; 1996. [Google Scholar]
- 3.Greenland S, Rothman KJ. Measures of occurrence. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 32–50. [Google Scholar]
- 4.Porta M. A dictionary of epidemiology. Oxford: Oxford U.P; 2014. [Google Scholar]
- 5.Cameron AC, Trivedi PK. Regression analysis of count data. Cambridge: Cambridge U.P; 1998. [Google Scholar]
- 6.Alonso PL, Sacarlal J, Aponte JJ, et al. Efficacy of the RTS, S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet. 2004;364:1411–20. doi: 10.1016/S0140-6736(04)17223-1. [DOI] [PubMed] [Google Scholar]
- 7.Alonso PL, Sacarlal J, Aponte JJ, et al. Duration of protection with RTS, S/AS02A malaria vaccine in prevention of Plasmodium falciparum disease in Mozambican children: single-blind extended follow-up of a randomised controlled trial. Lancet. 2005;366:2012–18. doi: 10.1016/S0140-6736(05)67669-6. [DOI] [PubMed] [Google Scholar]
- 8.Bigira V, Kapisi J, Clark TD, et al. Protective efficacy and safety of three antimalarial regimens for the prevention of malaria in young ugandan children: a randomized controlled trial. PLoS Med. 2014;11:e1001689. doi: 10.1371/journal.pmed.1001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sagara I, Giorgi R, Doumbo OK, Piarroux R, Gaudrt J. Modelling recurrent events: comparison of statistical models with continuous and discontinuous risk intervals on recurrent malaria episodes data. Malar J. 2014;13:293. doi: 10.1186/1475-2875-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook RJ, Lawless JF. The statistical analysis of recurrent events. New York: Springer; 2007. [Google Scholar]
- 11.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer; 2000. [Google Scholar]
- 12.Enwere GC, Cheung YB, Zaman S, Akano A, Oluwalana C, Okoko B, Vaughan A, Adegbola R, Greenwood B, Cutts F. The epidemiology and clinical features of pneumonia according to radiographic findings in Gambian children. Trop Med Int Health. 2007;12:1377–85. doi: 10.1111/j.1365-3156.2007.01922.x. [DOI] [PubMed] [Google Scholar]
- 13.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319:670–4. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011;2:109–12. doi: 10.4103/2229-3485.83221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orenstein WA, Bernier RH, Hinman AR. Assessing vaccine efficacy in the field. Further observations. Epidemiol Rev. 1988;10:212–41. doi: 10.1093/oxfordjournals.epirev.a036023. [DOI] [PubMed] [Google Scholar]
- 16.Halloran ME, Longini IM, Struchiner CJ. Design and analysis of vaccine studies. New York: Springer; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable; this is a statistical methodological study with illustration using information from publicly available publications (references [7, 8]).


