Abstract
Objective
to determine the effect of 900 mg/day of dried garlic powder (standardised to 1.3% allicin) in reducing total cholesterol. Design: double-blind, randomised six-month parallel trial.
Subjects
115 individuals with a repeat total cholesterol concentration of 6.0—8.5 mmol/l and low-density lipoprotein (LDL) cholesterol of 3.5 mmol/l or above after six weeks of dietary advice.
Intervention
the active treatment group received dried garlic tablets (standardised to 1.3% allicin) at a dosage of 300 mg three times daily. The control group received a matching placebo.
Outcome measures
primary end-point: total cholesterol concentration; secondary end-points: concentrations of LDL and high-density lipoprotein cholesterol, apolipoproteins (apo) A1 and B, and triglycerides.
Results
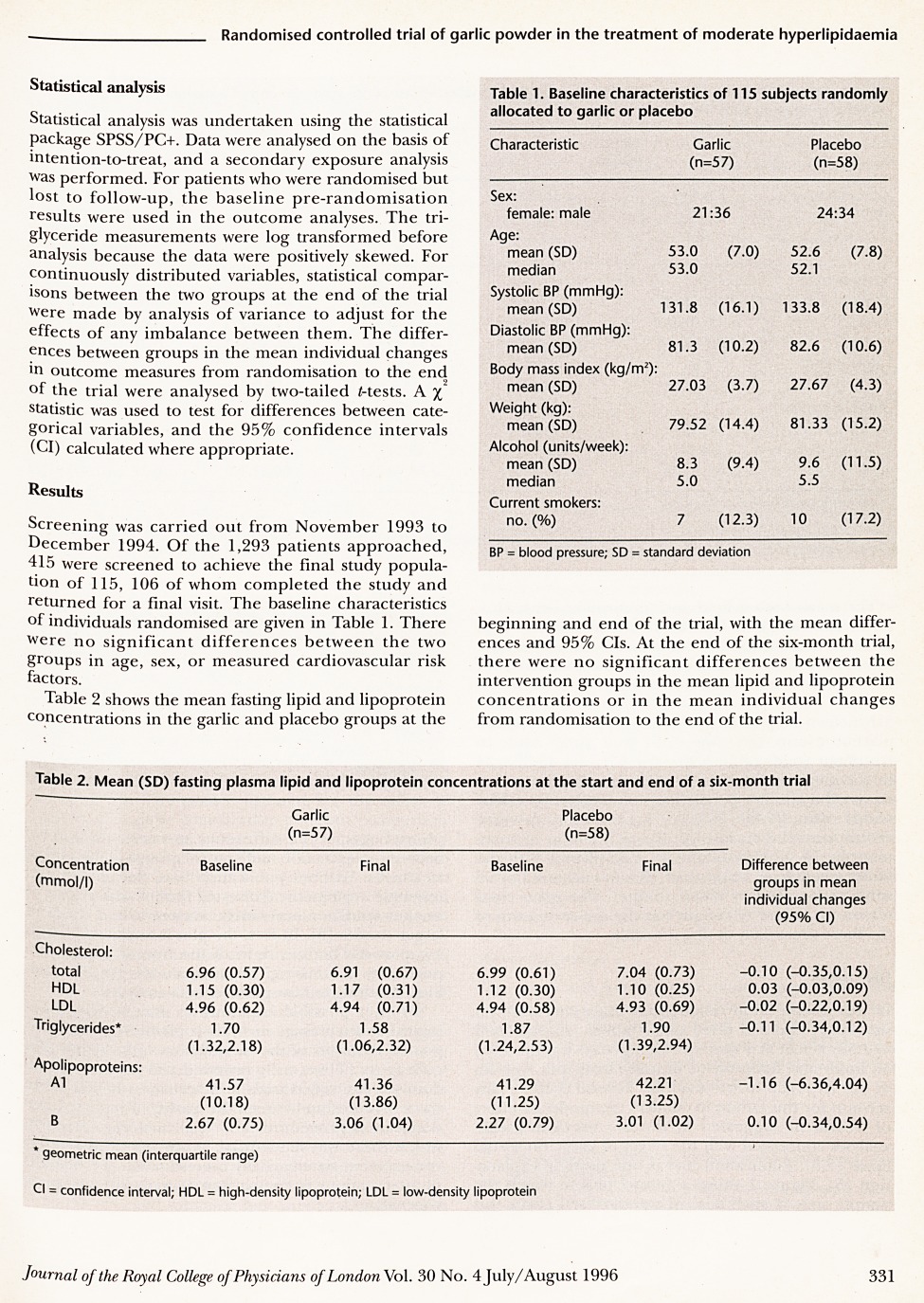
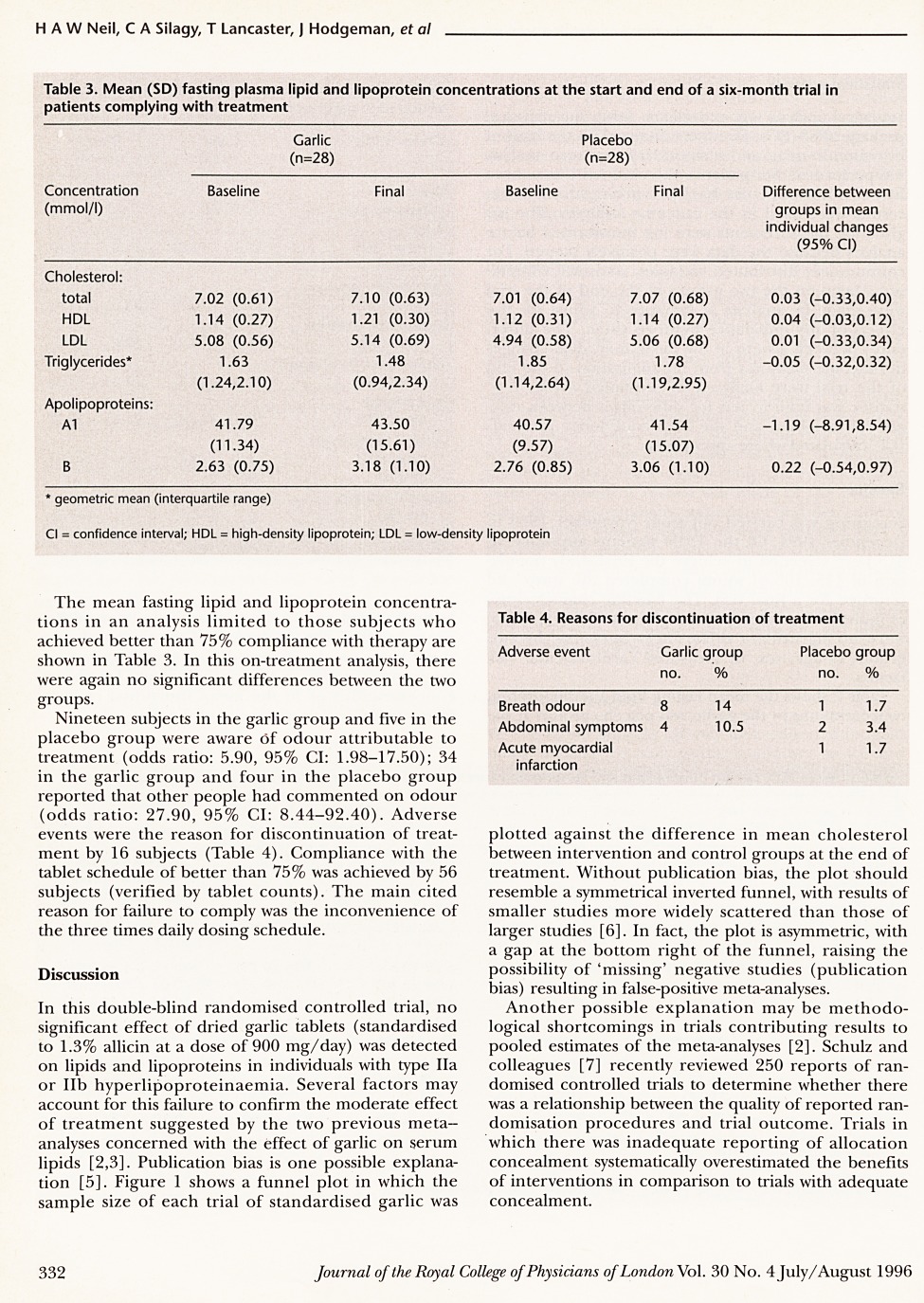
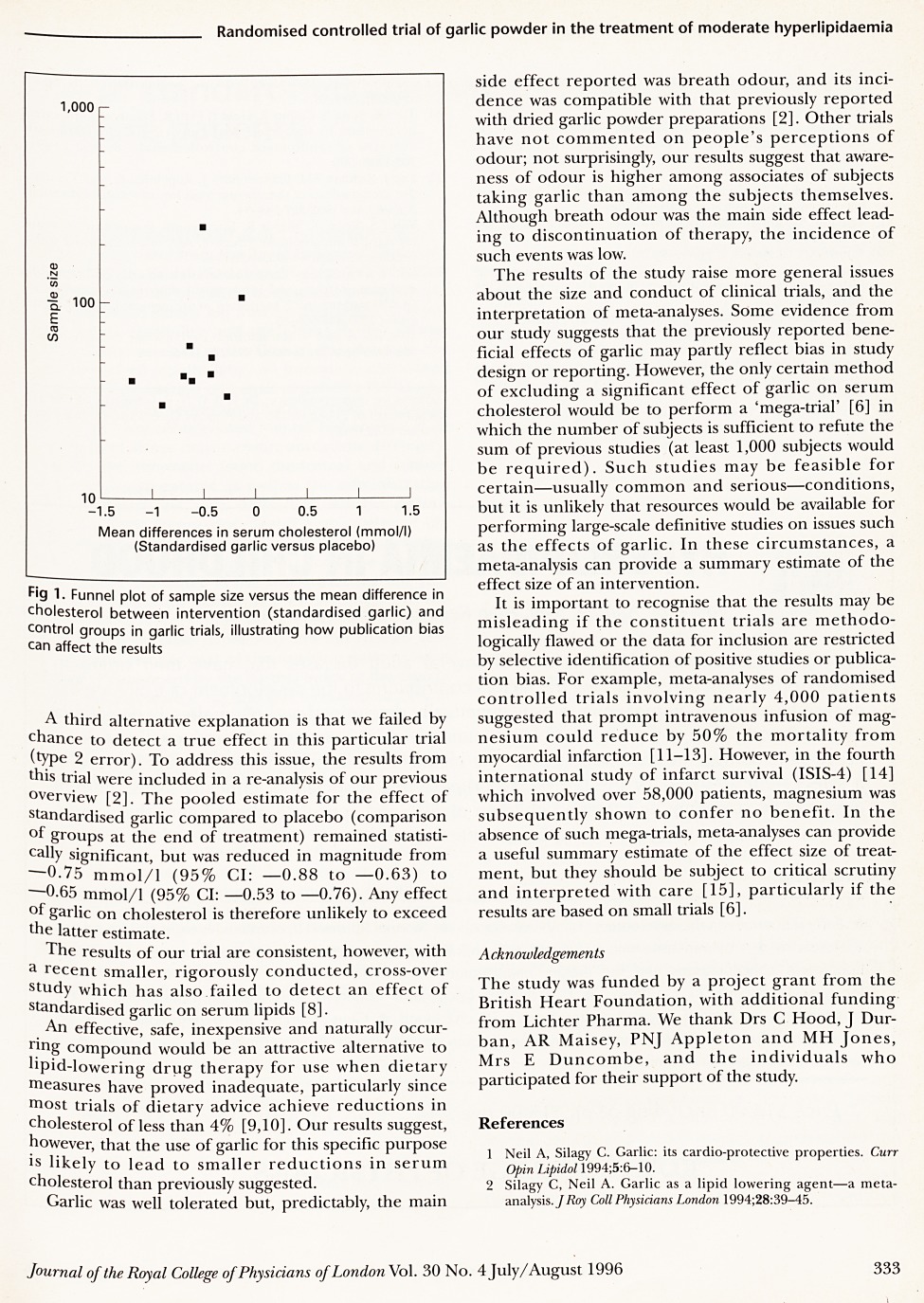
there were no significant differences between the groups receiving garlic and placebo in the mean concentrations of serum lipids, lipoproteins or apo A1 or B, by analysis either on intention-to-treat or treatment received. In a meta-analysis which included the results from this trial, garlic was associated with a mean reduction in total cholesterol of -0.65 mmol/l (95% confidence intervals: -0.53 to -0.76).
Conclusions
in this trial, garlic was less effective in reducing total cholesterol than suggested by previous meta-analyses. Possible explanations are publication bias, overestimation of treatment effects in trials with inadequate concealment of treatment allocation, or a type 2 error. We conclude that meta-analyses should be interpreted critically and with particular caution if the constituent trials are small.
Full text
PDF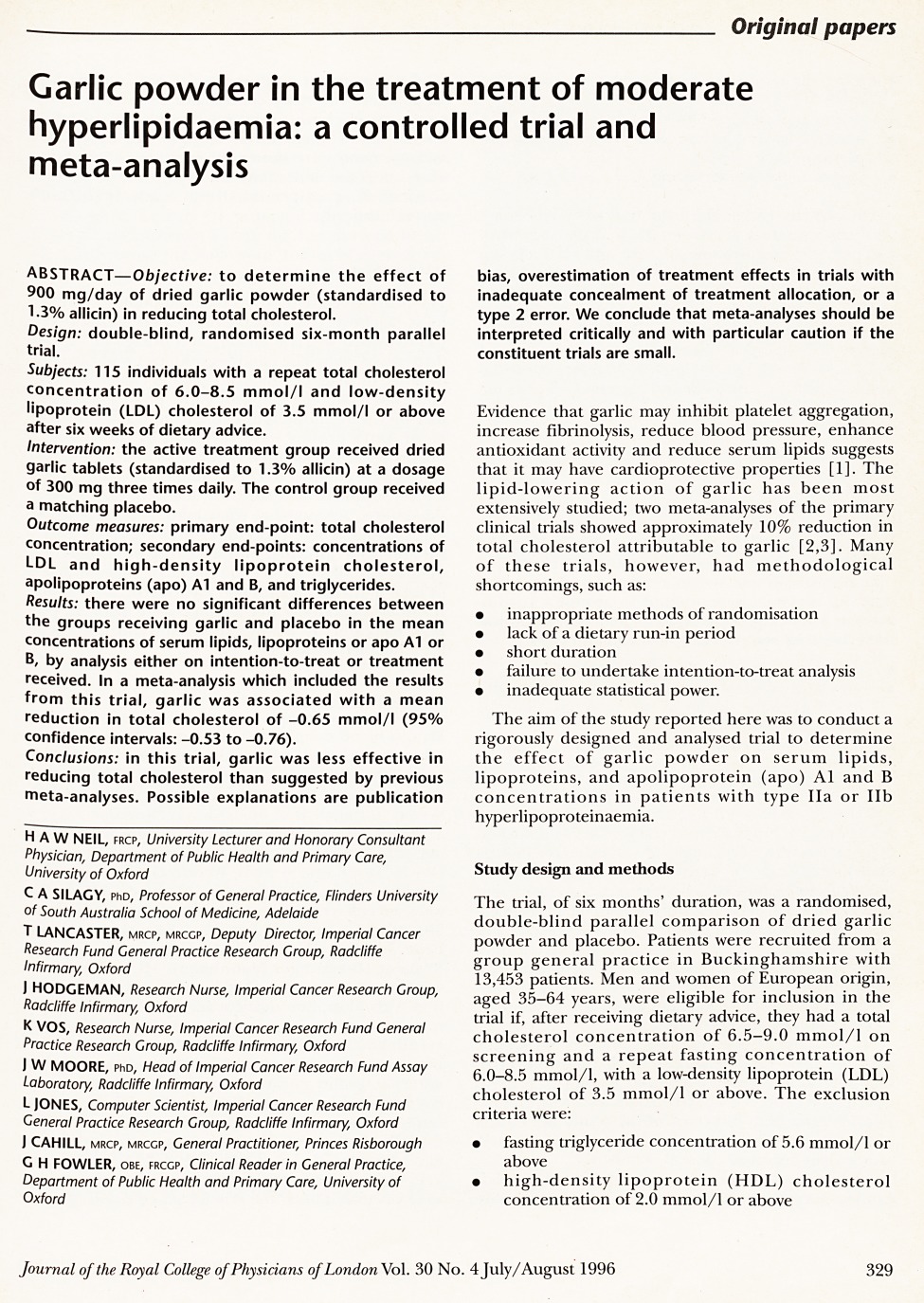
Contributor Information
H A W Neil, University Lecturer and Honorary Consultant Physician, Department of Public Health and Primary Care, University of Oxford.
C A Silagy, Professor of General Practice, Flinders University of South Australia School of Medicine, Adelaide.
T Lancaster, Deputy Director, Imperial Cancer Research Fund General Practice Research Group, Radcliffe Infirmary, Oxford.
J Hodgeman, Research Nurse, Imperial Cancer Research Group, Radcliffe Infirmary, Oxford.
K Vos, Research Nurse, Imperial Cancer Research Fund General Practice Research Group, Radcliffe Infirmary, Oxford.
J W Moore, Head of Imperial Cancer Research Fund Assay Laboratory, Radcliffe Infirmary, Oxford.
L Jones, Computer Scientist, Imperial Cancer Research Fund General Practice Research Group, Radcliffe Infirmary, Oxford.
J Cahill, General Practitioner, Princes Risborough.
G H Fowler, OBE; Clinical Reader in General Practice, Department of Public Health and Primary Care, University of Oxford.



