Abstract
Introduction
A diet high in fruits and vegetables (FV) is associated with reduced risk of chronic disease. One strategy to incentivize FV consumption among low-income households is to make them more affordable through the Supplemental Nutrition Assistance Program (SNAP). This study aims to identify the cost effectiveness of subsidizing FV purchases among the one in seven Americans who participate in SNAP.
Methods
A cost-effectiveness analysis was conducted from a societal perspective to estimate lifetime costs and health gains associated with subsidizing FV purchases. A stochastic microsimulation model of obesity, Type 2 diabetes, myocardial infarction, and stroke in the 2015 U.S. population was used. Model parameters were based on nationally representative SNAP participation and dietary consumption data from the National Health and Nutrition Examination Survey (2003–2012), and data from a randomized trial of FV subsidies among SNAP users.
Results
Despite cycling of participants in and out of SNAP, expanding a FV subsidy nationwide through SNAP would be expected to reduce incidence of Type 2 diabetes by 1.7% (95% CI=1.2, 2.2), myocardial infarction by 1.4% (95% CI=0.9, 1.9), stroke by 1.2% (95% CI=0.8, 1.6), and obesity by 0.2% (95% CI=0.1, 0.3), and be cost saving from a societal perspective. The saved costs would be largely attributable to long-term reductions in Type 2 diabetes and cardiovascular diseases.
Conclusions
The model suggests nationwide SNAP FV subsidies would reduce chronic disease morbidity, mortality, and costs over long time horizons that are unlikely to be observed in short-term community-based trials.
Introduction
The U.S. Federal government's Healthy People 2020 objectives include increasing fruit and vegetable (FV) consumption by at least 50% among all Americans.1 Although a diet high in FVs is associated with reduced risk of chronic diseases,2 adults in the U.S., particularly those in low-income households, consume far less than the recommended quantity of FVs—likely contributing to socioeconomic disparities in chronic disease.3
One strategy to incentivize FV consumption among low-income households is to make them more affordable to purchase through the Supplemental Nutrition Assistance Program (SNAP) (formerly the Food Stamp Program), the country's largest nutrition assistance program with approximately 46 million enrolled low-income Americans.4 The Healthy Incentive Pilot (HIP) study recently randomized SNAP-participating households in Hamden County, Massachusetts to either receive standard SNAP benefits (a monthly deposit, averaging approximately $4 per person per day) or standard SNAP benefits plus an additional incentive for FV purchases.5 In the incentive arm, for every $1 of SNAP benefits spent on approved FVs, participants received a 30-cent additional benefit. Approved FVs included fresh, canned, frozen, or dried FVs without added sugars, fats, oils or salt, excluding white potatoes and 100% fruit juices. The program increased daily consumption of targeted FVs by 0.24 cup equivalents per person per day, an approximately 26% increase from pre-incentive consumption, while participating in the program.6,7
Given the financial cost of targeted FV subsidy to consumers,8 a key question is whether the long-term health and healthcare cost savings potentially resulting from increasing FV consumption might offset the cost of incentives. Prior work suggests that subsidizing FV purchases may be cost effective, assuming increased FV intake would be sustained for a lifetime.9 This prior work focuses on average quality-adjusted life years (QALYs) gained from reducing all-cause mortality, and not the differential QALYs and costs of specific diseases.9 Several questions remain unanswered, including whether the targeted subsidy would remain cost effective if FV intake increases only occurred during the period of SNAP enrollment, how differences between the national population and the SNAP-participating population in food consumption patterns and chronic disease risks may critically affect costs and effectiveness, and how complex patterns of substitution between food groups could alter the long-term effectiveness of the program in reducing cardiovascular diseases and obesity. In addition, participants in the HIP trial significantly reduced their refined grain intake as they increased FV intake, which may have other secondary health and healthcare cost benefits.
This study sought to identify the circumstances under which expanding a FV subsidy in SNAP nationwide would be cost effective from a societal perspective, particularly given observed SNAP participation rates and durations in the country, food consumption patterns among SNAP users, and differences in diseases risks and costs within the SNAP population as compared with the general U.S. population.
Methods
A model of four health outcomes significantly associated with FV intake was constructed using data from a recent comprehensive meta-analysis2: obesity, Type 2 diabetes, myocardial infarction (MI), and stroke. This model incorporated detailed SNAP participation rates and durations, as well as food prices and dietary consumption data for a representative U.S. population (Figure 1). The model structure was based on a previously published microsimulation model,10,11 which simulates individuals rather than aggregate population averages (i.e., a Markov cohort model), because microsimulation allows us to account for complex co-variations in key traits that may critically impact the cost effectiveness of a FV subsidy program. Table 1 summarizes the key model parameters and data sources, further detailed in the Appendix.
Figure 1.
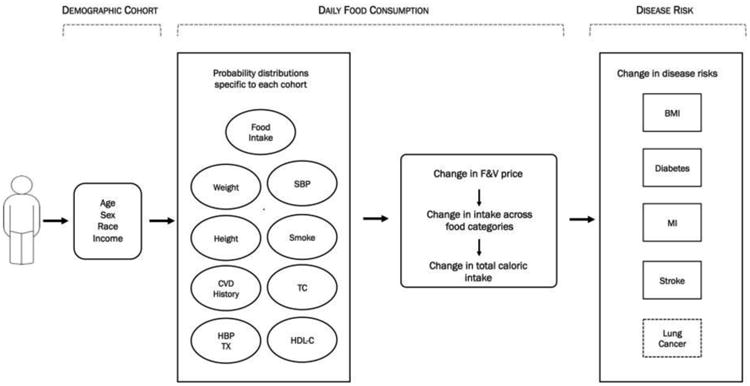
Model schematic.
SBP, systolic blood pressure; TC, total cholesterol; HBP TX, hypertension treatment status; HDL-C, high-density lipoprotein cholesterol; MI, myocardial infarction; CVD, cardiovascular disease; FV, fruit and vegetable
Table 1. Model Parameters and Sources.
| Parameters | Source |
|---|---|
| Population size of demographic cohorts | NHANES 2003-2012 |
| Weight changes associated with caloric intake (Appendix Text 1) | NIH model of body mass change a |
| Risk of MI or stroke by demographic group (Appendix Text 2) | Model-based estimates from meta-analysis data b |
| Risk of type II diabetes (Appendix Table 5) | CDC |
| Risk of lung cancer (Appendix Table 6) | SEER |
| Baseline MI history prevalence (Appendix Table 7) | NHANES 2003-2012 |
| Baseline stroke history prevalence (Appendix Table 8) | NHANES 2003-2012 |
| Baseline hypertension treatment prevalence (Appendix Table 9) | NHANES 2003-2012 |
| Baseline systolic blood pressure (Appendix Table 10) | NHANES 2003-2012 |
| Baseline total cholesterol (Appendix Table 11) | NHANES 2003-2012 |
| Baseline HDL cholesterol (Appendix Table 12) | NHANES 2003-2012 |
| Baseline weight and height (Appendix Tables 13 and 14) | NHANES 2003-2012 |
| MI or stroke mortality rate (Appendix Text 3) | Model calibration to national data c |
| Hazard ratio of Type II diabetes on all-cause mortality (Appendix Table 2) | Meta-analysis data d |
| All-cause mortality rate | CDC |
| Food cost (Appendix Table 3A) | QFHPD |
| Food consumption elasticity (Appendix Table 3B) | HIP findings e |
Risk of MI or stroke by demographic group - Model-based estimates from meta-analysis data. 25,58,59
Hazard ratio of type II diabetes on all-cause mortality - Meta-analysis data.35
Food consumption elasticity - HIP findings.6
NHANES, National Health and Nutrition Examination Survey; MI, myocardial infarction; CDC, Center for Disease Control and Prevention; SEER, Surveillance, Epidemiology, and End Results; HDL, High-density lipoprotein; QFHPD, Quarterly Food-at-home Price Database; HIP, Healthy Incentive Pilot
Modeling Framework
A nationally representative sample of 10,000 Americans aged 0–85 years was simulated, starting in 2015, to estimate the impact of a FV subsidy on costs and QALYs over their remaining life courses, as recommended by current cost-effectiveness analysis guidelines.12-14 Based on the National Health and Nutrition Examination Survey ([NHANES], 2003–2012, N=34,294),15 the simulated individuals were stratified by SNAP participation status (based on demographics and income eligibility, federal poverty level <130%; Appendix Table 3B),16,17 age (0–9, 10–19, 20–39, 40–59, 60–85 years), sex, race/ethnicity (NHANES categories of non-Hispanic white, non-Hispanic black, Mexican-American, or other), and income (relative to the federal poverty level, adjusted for household size).
Health-related risk factors for the four diet-related diseases of interest (obesity, Type 2 diabetes, MI, and stroke) were assigned to each simulated individual according to NHANES (Table 1, Figure 1, Appendix Tables S4–S14, and Text 1) and daily food intake in each U.S. Department of Agriculture food category per 24-hour dietary recalls adjusted for within-person variations in consumption to estimate usual daily intake.15,18 Risk factors were updated annually to reflect age and time trends, as well as changes in risk factors including dietary consumption patterns accounting for SNAP participation status. Survey sample weights were used to correct for differential sampling and non-response in the NHANES survey.19
Heath Benefit Measures
The risk of each of the four major FV-related outcomes was estimated for each individual, before versus after a 30% SNAP subsidy on approved FV purchases using HIP rules.20 Disease incidence was estimated based on previously validated risk equations incorporating individual risk factors (Appendix Text 1–2; Appendix Tables 5–14).21–29 Deaths attributable to these risk factors and other causes were taken into account as a function of age and sex.25,26 To ensure face validity, Type 2 diabetes incidence rates were compared to Center for Disease Control and Prevention estimates17; and MI and stroke incidence rates were compared to estimates from the Atherosclerosis Risk in Communities study, the Greater Cincinnati/Northern Kentucky Stroke Study, and independent cohort studies from National Heart, Lung, and Blood Institute.23,30,31
Because the HIP Trial reported an increase of 26.2% in FV consumption in the incentive arm, a base case was simulated in which this percentage increase in FV consumption was adopted by current SNAP participants given a 30% FV price subsidy (Appendix Table 3C), with the subsidy amount limited to $60 per person per month. Because HIP also reported significantly lower refined grain consumption (8.8%) among HIP subsidy participants, this change in refined grain intake and resulting change in weight were incorporated into the base case. In addition to computing total calorie changes and associated changes in body weight (using NIH body weight models),27,29 published meta-analytic risk reduction estimates were used for the reduction in Type 2 diabetes, MI, and stroke associated with reduced BMI and with increases in FV net of BMI changes, to compute the change in morbidity and mortality anticipated from the subsidy (Appendix Tables 2A–2D).2,32–35
Costs and Utilities
Following current cost-effectiveness guidelines,13,14 costs and QALY estimates were integrated over the life course for all simulated individuals from a societal perspective. Costs associated with the incentive program included the subsidy amount and, in the base case, an estimated 30% overhead expenditure rate,36 incurred for the years of participation, which was varied in sensitivity analyses. Food price data were obtained from the U.S. Department of Agriculture Quarterly Food-at-Home Price Database linked to NHANES (Appendix Table 3A).37 Annual disease-specific healthcare costs and the disutility of disease states to calculate QALYs were based on large-scale survey data (Appendix Table 4).38,39 Costs were expressed in 2015 U.S. dollars using the Consumer Price Index,40 and QALYs were discounted at a 3% annual discount rate.
Sensitivity and Uncertainty Analyses
First, the percentage of the U.S. population enrolled in SNAP was varied, as a new incentive may impact enrollment, or SNAP participation may be currently inflated by the recent economic recession. In the base case, the 2014 estimate was used in which 14.6% of the U.S. population was enrolled in SNAP.41 The participation rate was varied from 5% to 25%, the lowest and highest rates of participation over the last 3 decades, with participation within each demographic group proportional to the rate of participation during those prior years.
In the base case, both single-spell (people with <2 years of SNAP participation, with one episode in their life) and multi-spell SNAP participants (people frequently on and off SNAP) were included. In a second sensitivity analysis, the length of multi-spell participation durations was adjusted from the current typical spell length of 96 months to a spell length varying from 48 months to 160 months (Appendix Table 3B), which spanned the durations observed in available data.16
Third, different levels of FV subsidy were considered to examine what levels of subsidy would be most cost effective. The incentive percentages SNAP participants receive from purchasing targeted FVs were varied from 10% to 30%, assuming proportionate responses to the HIP trial result. In addition, the effects of habit formation and maintaining higher FV consumption without a subsidy were assessed by simulating half the amount of FV increase observed during participation among individuals with a prior history of SNAP participation.
Fourth, lung cancer was included as one of the health outcomes in the model, given meta-analytic data indicating that increased FV intake is associated with significantly lower lung cancer risk.2 It was omitted from the base case because the biological mechanism for the relationship was uninformed.
Fifth, potential changes in consumption of non-targeted FVs, those that do not qualify for the incentive, were simulated.6 A portion of the HIP intervention group consumed significantly more 100% fruit juice than non-participants, potentially due to confusion. This increase in 100% fruit juice was included to account for its caloric effects.
Finally, program overhead costs were varied from as low as 20% to as high as 50%, compared with the base case of 30%.
All analyses were performed in R, version 3.2.1. In each scenario, the model was re-run 10,000 times while repeated Monte Carlo sampling from the probability distributions of all input parameters to capture uncertainties in the estimates, generating 95% CIs around all outcomes as per International Society For Pharmacoeconomics and Outcomes Research guidelines.42 The Appendix details all input data, equations, and complete technical details,43 along with a link to program code for replication.
Results
If there were no change to current SNAP participation and food consumption profiles, the model estimated that the U.S. population aged 18–85 years would be expected to experience annual incidence rates of approximately 70.0 Type 2 diabetes cases (95% CI=60.2, 79.8), 40.0 new MIs (95% CI=39.8, 40.2), and 34.3 strokes (95% CI=34.0, 34.5) per 10,000 people. Consistent with the model, independent Centers for Disease Control and Prevention and National Heart, Lung, and Blood Institute data estimated a current incidence of 69.0 new Type 2 diabetes cases, 40.0 new MIs, and 34.5 new strokes per 10,000 people.44–47 Further age- and sex-specific validation is given in Appendix Figures 1–2.
If a 30% subsidy of FV purchases produced the same increase in FV consumption as found in the HIP trial (a 26.2% increase) and resulted in the same decrease in refined grain consumption (an 8.8% decrease), Type 2 diabetes, MI, and stroke incidence would be expected to decline substantially due to the impact of increasing FVs. Relatively smaller declines in obesity would be expected, given the relatively small impact of the subsidy on overall caloric intake (Figure 2).32 On average, Type 2 diabetes incidence would be expected to decrease by 10.3% (95% CI=9.4, 11.2) among SNAP participants; this decline would be expected to translate into a 1.7% (95% CI=1.2, 2.2) decline among the overall U.S. population, assuming no positive spillover effects from SNAP participant behavior to non-participant behavior. MI and stroke incidence would be expected to decline by 8.5% (95% CI=7.2, 9.8) and 7.4% (95% CI=6.3, 8.5), respectively, among SNAP participants, which would be 1.4% (95% CI=0.9, 1.9) and 1.2% (95% CI=0.8, 1.6) for the overall U.S. population. By contrast, obesity incidence would not be expected to decline substantially; the incidence would be expected to decline by 1.3% (95% CI=0.7, 1.9) among SNAP participants—a reduction of 0.2% (95% CI=0.1, 0.3) in the U.S. population (Appendix Table 1).
Figure 2.
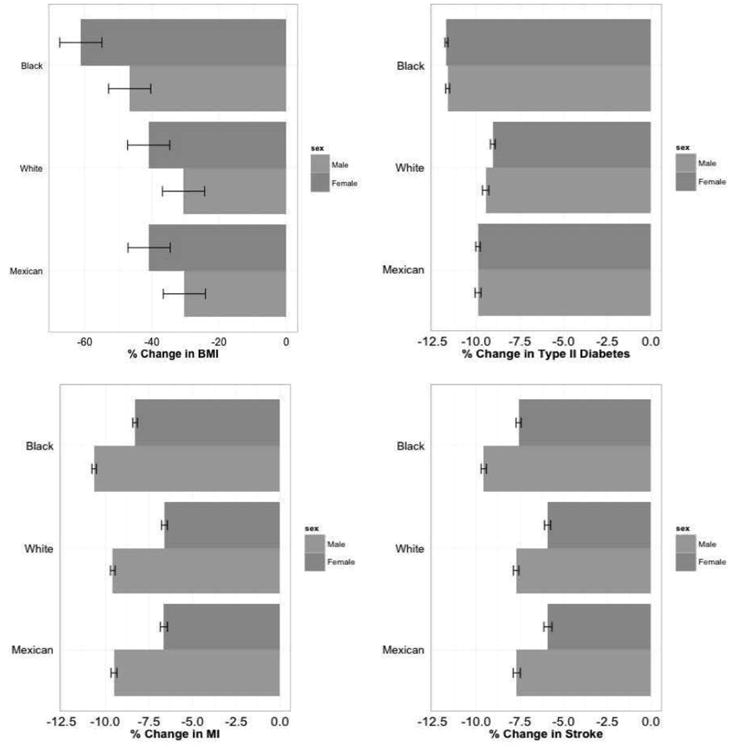
Projected reduction in incidence of diseases by gender and race/ethnicity due to a 30% subsidy on SNAP purchases of fruits and vegetables in the SNAP population.
MI, myocardial infarction; SNAP, Supplemental Nutrition Assistance Program
Although individuals in most demographic cohorts would be expected to benefit from a 30% subsidy of FV purchases, the projected benefits varied by demographic group (Figure 2). The largest relative declines in incidence of Type 2 diabetes, MI, and stroke were observed among blacks, as were the largest declines in BMI; these were due to high SNAP participation rates, low baseline FV consumption, and high baseline refined grain consumption among blacks, which produced the largest absolute disease reductions for this group.
The intervention produced an estimated gain of 0.52 (95% CI=0.51, 0.53) QALYs per SNAP user, which amounts to 0.24 (95% CI=0.23, 0.25) QALYs per capita for the general U.S. population over the life course.
The largest expected cost-savings from future averted disease was from averted Type 2 diabetes, followed by averted MI and stroke. The dollars saved from averted Type 2 diabetes amounted to $952 (95% CI=941, 963) per SNAP user over a simulated life course. The cost of the intervention (incentives and overhead costs) was $1,324 (95% CI=1,319, 1,330) per SNAP user, which amounted to $202 (95% CI=199, 204) per capita for the general U.S. population, approximately $857 million dollars total annually. From a societal perspective, the intervention was cost saving at a net savings of $824 (95% CI=821, 827) per capita, and had an incremental cost-effectiveness ratio (ICER) of $3,432 (95% CI=2,837, 4,027) per QALY gained (Table 2 and Appendix Figure 4). The net cost savings was produced by summing overall disease costs with the intervention minus costs without the intervention, including all disease treatment, subsidy, and overhead costs, discounted at a 3% annual rate.
Table 2. Cost-effectiveness Analysis.
| Scenario | Total QALYs (per capita) | Total cost (USD) | Incremental QALYs gained | Incremental cost | ICER |
|---|---|---|---|---|---|
| Status quo | 22.31 (0.01) | 8,580.21 (146.65) | |||
| 30% subsidy a | 22.55 (0.01) | 7,756.47(148.20) | 0.24 (0.02) | -823.74 (1.55) | -3,432.32 (304.91) |
| Sensitivity analyses | |||||
| SNAP participation rate | |||||
| 5% b | 22.52 (0.01) | 7,943.09 (143.35) | 0.21 (0.02) | -637.12 (3.30) | -3,033.33 (302.56) |
| 25% c | 22.59 (0.01) | 7,568.07 (138.89) | 0.28 (0.02) | -1,012.14 (7.76) | -3,614.28 (248.71) |
| Duration of subsidy | |||||
| 6 years d | 22.54 (0.01) | 7,935.08 (136.11) | 0.23 (0.02) | -645.13 (10.54) | -2,804.35 (217.51) |
| 16 years e | 22.58 (0.01) | 7,700.06 (138.90) | 0.27 (0.02) | -880.15 (7.75) | -3,259.25 (230.34) |
| Additional health outcomes | |||||
| Including LC f | 22.55 (0.02) | 8,450.08 (148.99) | 0.24 (0.02) | -919.92 (2.34) | -3,898.31 (272.51) |
| Implementation cost | |||||
| 20% overhead cost g | 22.55 (0.02) | 7,665.05 (150.05) | 0.24 (0.02) | -915.16 (3.40) | -3,813.17 (331.19) |
| 40% overhead cost h | 22.55 (0.02) | 7,782.11 (142.22) | 0.24 (0.02) | -798.10 (4.43) | -3,325.42 (282.17) |
| 60% overhead cost i | 22.55 (0.02) | 7,810.07 (148.67) | 0.24 (0.02) | -770.14 (2.02) | -3,208.92 (282.54) |
| Substitution HIP trial – including changes in fruit juice j | 22.54 (0.02) | 7,782.12 (142.19) | 0.24 (0.02) | -798.00 (4.46) | -3,395.74 (211.26) |
| Subsidy level | |||||
| 10% subsidy k | 22.53 (0.02) | 7,855.14 (152.56) | 0.22 (0.02) | -725.07 (5.91) | -3,295.45 (300.35) |
| 20% subsidy l | 22.54 (0.02) | 7,815.12 (155.32) | 0.23 (0.02) | -765.09 (8.67) | -3,326.09 (275.91) |
| Habit formation | |||||
| 50% maintainm | 22.94 (0.02) | 6,687.21 (149.06) | 0.63 (0.02) | -1,893.00 (2.41) | -3,004.76 (94.57) |
Notes: The reference category for all rows is the status quo, except for the “including LC” scenario for which the reference category is the status quo with LC included.
30% subsidy: base case analysis on subsidizing 30% of FV purchases among SNAP users in the U.S.
5% enrolled: 5% of the U.S. population enrolled in SNAP.
25% enrolled: 25% of the U.S. population enrolled in SNAP
48 months SNAP: 48 months completed length of SNAP participation.
160 months SNAP: 160 months completed length of SNAP participation.
LC added: lung cancer included as one of the health outcomes.
20% overhead cost: 20% overhead expenditure rate.
40% overhead cost: 40% overhead expenditure rate.
50% overhead cost: 50% overhead expenditure rate.
Fruit juice included: 100% fruit juice included in consumption changes in addition to refined grain and targeted FV.
0% subsidy: subsidizing 10% of FV purchases.
20% subsidy: subsidizing 20% of FV purchase.
50% maintain: Habit formation and maintaining half the amount of FV increase observed during participation among individuals with a prior history of SNAP participation.
ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life years; LC, lung cancer; FV, fruits and vegetables; SNAP, Supplemental Nutrition Assistance Program; HIP, Healthy Incentive Pilot
The healthcare cost reductions and intervention costs accumulated most among blacks, who experienced an estimated healthcare cost reduction of $3,829 (95% CI=3,672, 3,985) given a FV subsidy cost of $1,367 (95% CI=1,359, 1,675) per SNAP user (Appendix Figure 5).
None of the sensitivity analyses substantially changed the fundamental finding of cost savings from the FV subsidy (Appendix Figure 6).
When SNAP enrollment rates were varied from 5% to 25%, the lowest and highest rates of participation over the last 3 decades, the FV subsidy was cost saving with an ICER varying from $3,033 saved (95% CI=2,441, 3,625) to $3,614 saved (95% CI=3,128, 4,100) per QALY gained (Table 2).
Next, the effects of lower SNAP participation duration and subsidy levels were evaluated. Participants having completed the spell length of 48 months would be expected to experience more QALYs at less cost, with an ICER of $2,804 (95% CI=2,382, 3,225) saved per QALY gained. Decreasing subsidy levels to 10% would still be cost saving at an ICER of $3,295 (95% CI=2,707, 3,883) saved per QALY gained.
Habit formation and maintaining higher FV consumption without a subsidy (half the amount of FV increase observed during participation) among individuals with a prior history of SNAP participation resulted in significantly higher QALYs gained, 0.63 (95% CI=0.62, 0.64) with an ICER of $3,005 (95% CI=2,597, 3,412).
In addition to the four primary health outcomes, if lung cancer is included as one of the health outcomes, a FV subsidy would be expected to produce 0.24 (95% CI=0.22-0.26) QALYs gained per person, an ICER of $3,898 (95% CI=3,364, 4,431) saved per QALY gained. Moreover, when increases in 100% fruit juice consumption from a FV subsidy were incorporated, as per the HIP trial, participants would not be expected to receive benefits in obesity due to higher caloric intake from 100% fruit juice (Appendix Figure 6). However, the overall intervention was still cost saving from other averted diseases with an ICER of $3,395 (95% CI=2,981, 3,808) saved per QALY gained.
Lastly, varying overhead costs of implementation from 20% to 50% of incentives paid to participants did not substantially change the results. The FV subsidy was expected to be cost saving within the simulated range of the overhead costs with the smallest savings of $3,208 (95% CI=2,655, 3,760) per QALY gained (Table 2).
Discussion
A 30% subsidy on SNAP FV purchases would likely have large, meaningful public health benefits. Substantial reductions in morbidity and mortality would most likely be observed from reduced incidences of three long-term chronic diseases (Type 2 diabetes, MI, and stroke), consistent with findings from prior meta-analytic studies.48–50 SNAP demonstrations typically focus on short-term outcomes such as net caloric intake, and hence may fail to capture the much larger and meaningful long-term chronic disease prevention benefits of increased FV consumption. These benefits would likely persist even if the incentive is imperfectly implemented, as in the HIP trial where participants were confused about approved FVs included in the incentive.
These findings are particularly relevant for federal policymakers because the incentive would be cost saving from a societal perspective. This study accounted for the fact that increased FV intake may only occur during periods of SNAP participation among people who cycle in and out of SNAP. Accounting for complex variations in SNAP participation among different demographic groups and correlated risk factors among SNAP participants, the subsidy would be expected to particularly benefit non-Hispanic blacks—the group for whom healthcare interventions alone have not been sufficient to reduce large disparities in cardiovascular disease incidence that have been attributed in part to poor nutrition.51
Limitations
The effects of a FV subsidy on disease risks were modeled based on the most rigorous available meta-analytic data.2,32–34 Therefore, findings are likely to be conservative and potentially robust to the concern that several associations in the nutrition literature may be false-positive associations.12,52–54 Additional studies estimating the degree of heterogeneous treatment effects, including kilocalorie effect size of FV intake,55 are needed, but would likely strengthen the authors' conclusions. Second, data from NHANES are subject to the limitations of survey studies, including recall biases, acceptability biases, and under-reporting, which may lead to underestimation of SNAP participation.56 This bias would also lead the impact estimates to be conservative. Finally, although uncertainty analyses were performed by sampling from distributions around the input parameter data sources, all possible uncertainties in a simulation model cannot be captured. Hence, results are inevitably subject to the assumptions inherent in modeling. Among these is the use of risk factor equations to estimate risk, which may overestimate disease when clinical treatment of risk factors improves over time; however, such improvements in treatment are historically observed disproportionately among higher-socioeconomic groups.57
Conclusions
Nationwide expansion of the HIP financial incentive program for FV purchases would be expected to lower obesity, Type 2 diabetes, and cardiovascular disease in the U.S and would be cost saving under a wide range of scenarios. The benefits would likely accumulate among demographic groups who have been traditionally missed by healthcare-based interventions, thus addressing social and economic determinants of nutritional and health disparities.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of NIH under Award Numbers R01HL132814, DP2MD010478, and K08HL121056. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
Author contributions: SEC: study conception and design, statistical analysis, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript; HS: study conception and design, analysis and interpretation of data, critical revision of the manuscript; SB: study conception and design, statistical analysis, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, obtained funding.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Office of Disease Prevention and Health Promotion; [Accessed February 2, 2016]. Healthy People 2020 Objectives- Nutrition and Weight Status. www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives. [Google Scholar]
- 2.Lock K, Pomerleau J, Causer L, McKee M. WHO; [Accessed May 1, 2016]. Chapter 9 Low fruit and vegetable consumption. www.who.int/publications/cra/chapters/volume1/0597-0728.pdf. [Google Scholar]
- 3.U.S. Department of Agriculture. Dietary Guidelines for Americans. 2010 http://health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf.
- 4.Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. USDA ERS; [Accessed February 22, 2016]. Household Food Security in the United States in 2014. http://www.ers.usda.gov/publications/pub-details/?pubid=79760. [Google Scholar]
- 5.U.S. Department of Agriculture. Healthy Incentives Pilot (HIP) Early Implementation Report. [Accessed May 2, 2016];2013 www.fns.usda.gov/healthy-incentives-pilot-hip-early-implementation-report.
- 6.Bartlett S, Klerman J, Olsho L, et al. U.S. Department of Agriculture; 2014. [Accessed May 2, 2016]. Evaluation of the Healthy Incentives Pilot (HIP): Final Report. www.fns.usda.gov/sites/default/files/HIP-Final.pdf. [Google Scholar]
- 7.Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot. Am J Clin Nutr. 2016;104(2):423–435. doi: 10.3945/ajcn.115.129320. http://dx.doi.org/10.3945/ajcn.115.129320. [DOI] [PubMed] [Google Scholar]
- 8.Herman DR, Harrison GG, Afifi AA, Jenks E. Effect of a targeted subsidy on intake of fruits and vegetables among low-income women in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am J Public Health. 2008;98(1):98–105. doi: 10.2105/AJPH.2005.079418. http://dx.doi.org/10.2105/AJPH.2005.079418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.An R. Nationwide expansion of a financial incentive program on fruit and vegetable purchases among Supplemental Nutrition Assistance Program participants: A cost-effectiveness analysis. Soc Sci Med. 2015;147:80–88. doi: 10.1016/j.socscimed.2015.09.032. http://dx.doi.org/10.1016/j.socscimed.2015.09.032. [DOI] [PubMed] [Google Scholar]
- 10.Choi SE, Brandeau ML, Basu S. Expansion of the National Salt Reduction Initiative: A Mathematical Model of Benefits and Risks of Population-Level Sodium Reduction. Med Decis Making. 2016;36(1):72–85. doi: 10.1177/0272989X15583846. http://dx.doi.org/10.1177/0272989X15583846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basu S, Seligman HK, Gardner C, Bhattacharya J. Ending SNAP Subsidies For Sugar-Sweetened Beverages Could Reduce Obesity And Type 2 Diabetes. Health Aff (Millwood) 2014;33(6):1032–1039. doi: 10.1377/hlthaff.2013.1246. http://dx.doi.org/10.1377/hlthaff.2013.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramsey S, Willke R, Briggs A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health. 2005;8(5):521–533. doi: 10.1111/j.1524-4733.2005.00045.x. http://dx.doi.org/10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996;276(15):1253–1258. http://dx.doi.org/10.1001/jama.1996.03540150055031. [PubMed] [Google Scholar]
- 14.WHO. WHO Guide to Cost-effectiveness Analysis. [Accessed February 2, 2016];2003 www.who.int/choice/publications/p_2003_generalised_cea.pdf?ua=1.
- 15.CDC. Atlanta, GA: 2014. [Accessed February 22, 2016]. National Health and Nutrition Examination Survey, 2008-2012. www.cdc.gov/nchs/nhanes.htm. [Google Scholar]
- 16.U.S. Department of Agriculture. Dynamics of Supplemental Nutrition Assistance Program Participation from 2008 to 2012. [Accessed May 1, 2016]; www.fns.usda.gov/sites/default/files/ops/Dynamics2008-2012.pdf.
- 17.National Center for Health Statistics. National Center for Health Statistics Data Access. [Accessed February 28, 2016];2015 www.cdc.gov/nchs/data_access.htm.
- 18.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98. http://dx.doi.org/10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. Atlanta, GA: 2013. [Accessed February 2, 2016]. Continuous NHANES Web Tutorial. www.cdc.gov/nchs/tutorials/Nhanes/index_continuous.htm. [Google Scholar]
- 20.U.S. Department of Agriculture. Requirements and Specifications for SNAP HIP Fruit and Vegetable Purchases. [Accessed May 1, 2016]; www.fns.usda.gov/sites/default/files/purchase_list.pdf.
- 21.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1 Pt 2):293–298. doi: 10.1016/0002-8703(91)90861-b. http://dx.doi.org/10.1016/0002-8703(91)90861-B. [DOI] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. http://dx.doi.org/10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 23.National Heart Lung and Blood Institute. Incidence and prevalence: Chart book on cardiovascular and lung diseases, 2006. [Accessed May 1, 2016];2009 www.nhlbi.nih.gov/resources/docs/cht-book_ip.htm.
- 24.CDC. Incidence of diagnosed diabetes per 1,000 population aged 18–79 years, 1980–2011. [Accessed April 30, 2016];2012 www.cdc.gov/diabetes/statistics/incidence/fig3.htm.
- 25.Smith-Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med. 2010;152(8):481–487. doi: 10.7326/0003-4819-152-8-201004200-00212. http://dx.doi.org/10.7326/0003-4819-152-8-201004200-00212. [DOI] [PubMed] [Google Scholar]
- 26.CDC. National Center for Health Statistics; United States Life Tables. www.cdc.gov/nchs/products/life_tables.htm. [Google Scholar]
- 27.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol. 2013;1(2):97–105. doi: 10.1016/s2213-8587(13)70051-2. http://dx.doi.org/10.1016/S2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hall KD, Jordan PN. Modeling weight-loss maintenance to help prevent body weight regain. Am J Clin Nutr. 2008;88(6):1495–1503. doi: 10.3945/ajcn.2008.26333. http://dx.doi.org/10.3945/ajcn.2008.26333. [DOI] [PubMed] [Google Scholar]
- 29.Hall KD, Sacks G, Chandramohan D, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378(9793):826–837. doi: 10.1016/S0140-6736(11)60812-X. http://dx.doi.org/10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702. http://dx.doi.org/10.1093/oxfordjournals.aje.a115184. [PubMed] [Google Scholar]
- 31.Broderick J, Brott T, Kothari R, et al. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29(2):415–421. doi: 10.1161/01.str.29.2.415. http://dx.doi.org/10.1161/01.STR.29.2.415. [DOI] [PubMed] [Google Scholar]
- 32.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. http://dx.doi.org/10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011;108(1):56–62. doi: 10.1016/j.amjcard.2011.03.004. http://dx.doi.org/10.1016/j.amjcard.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li M, Fan Y, Zhang X, Hou W, Tang Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: meta-analysis of prospective cohort studies. BMJ Open. 2014;4(11):e005497. doi: 10.1136/bmjopen-2014-005497. http://dx.doi.org/10.1136/bmjopen-2014-005497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nwaneri C, Cooper H, Bowen-Jones D. Mortality in Type 2 Diabetes Mellitus: Magnitude of the Evidence From a Systematic Review and Meta-analysis. Br J Diabetes Vasc Dis. 13(4):192–207. [Google Scholar]
- 36.U.S. Department of Agriculture. Food and Nutrition Service, 2013 Explanatory Notes. 2013 www.obpa.usda.gov/30fns2013notes.pdf.
- 37.U.S. Department of Agriculture. Quarterly Food-at-Home Price Database. [Accessed May 1, 2016]; www.ers.usda.gov/data-products/quarterly-food-at-home-price-database.aspx.
- 38.Agency for Healthcare Research and Quality. Disparities in Health Care Quality Among Racial and Ethnic Minority Groups. 2010 www.ahrq.gov/research/findings/nhqrdr/nhqrdr10/minority.pdf.
- 39.Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2010 (GBD 2010) Disability Weights. [Accessed February 22, 2016];2010 http://ghdx.healthdata.org/record/global-burden-disease-study-2010-gbd-2010-disability-weights.
- 40.Bureau of Labor Statistics. Consumer Price Index (CPI) Inflation Calculator. [Accessed January 5, 2016]; www.bls.gov/data/inflation_calculator.htm.
- 41.U.S. Department of Agriculture. Supplemental Nutrition Assitance Program (SNAP): National Level Annual Summary. 2015 www.fns.usda.gov/sites/default/files/pd/SNAPsummary.pdf.
- 42.Briggs AH, Weinstein MC, Fenwick EA, et al. Model parameter estimation and uncertainty analysis: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group-6. Med Decis Making. 2012;32(5):722–732. doi: 10.1177/0272989X12458348. http://dx.doi.org/10.1177/0272989X12458348. [DOI] [PubMed] [Google Scholar]
- 43.Rahmandad H, Sterman JD. Reporting guidelines for simulation-based research in social sciences. Syst Dyn Rev. 2012;28(4):396–411. http://dx.doi.org/10.1002/sdr.1481. [Google Scholar]
- 44.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. http://dx.doi.org/10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Center for Health Statistics. Heart disease facts. [Accessed May 1, 2016];2014 www.cdc.gov/heartdisease/facts.htm.
- 46.National Center for Health Statistics. Stroke facts. [Accessed May 1, 2016];2014 www.cdc.gov/stroke/facts.htm.
- 47.National Center for Health Statistics. Crude and Age-Adjusted Incidence of Diagnosed Diabetes per 1,000 Population Aged 18-79 Years, United States, 1980-2014. 2014 www.cdc.gov/diabetes/statistics/incidence/fig2.htm.
- 48.Lewis KH, Basu S. Epidemiology of Obesity in the United States. In: Ahima RS, editor. Metabolic Syndrome: A Comprehensive Textbook. Cham: Springer International Publishing; 2016. pp. 13–31. http://dx.doi.org/10.1007/978-3-319-11251-0_2. [Google Scholar]
- 49.Hung HC, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96(21):1577–1584. doi: 10.1093/jnci/djh296. http://dx.doi.org/10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 50.Wang X, Ouyang Y, Liu J, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. doi: 10.1136/bmj.g4490. http://dx.doi.org/10.1136/bmj.g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Howard VJ. Reasons underlying racial differences in stroke incidence and mortality. Stroke. 2013;44(6 Suppl 1):S126–128. doi: 10.1161/STROKEAHA.111.000691. http://dx.doi.org/10.1161/STROKEAHA.111.000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ioannidis JP. Implausible results in human nutrition research. BMJ. 2013;347:f6698. doi: 10.1136/bmj.f6698. http://dx.doi.org/10.1136/bmj.f6698. [DOI] [PubMed] [Google Scholar]
- 53.Nwaneri CC, H, Bowen-Jones D. Mortality in Type 2 Diabetes Mellitus. Br J Diabetes Vasc Dis. 2013;13(4):192–207. http://dx.doi.org/10.1177/1474651413495703. [Google Scholar]
- 54.Schoenfeld JD, Ioannidis JPA. Is everything we eat associated with cancer? A systematic cookbook review. Am J Clin Nutr. 2013;97(1):127–134. doi: 10.3945/ajcn.112.047142. http://dx.doi.org/10.3945/ajcn.112.047142. [DOI] [PubMed] [Google Scholar]
- 55.Bertoia ML, Mukamal KJ, Cahill LE, et al. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015;12(9):e1001878. doi: 10.1371/journal.pmed.1001878. http://dx.doi.org/10.1371/journal.pmed.1001878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kreider B, Pepper JV, Gundersen C, Jolliffe D. Identifying the Effects of SNAP (Food Stamps) on Child Health Outcomes When Participation Is Endogenous and Misreported. J Am Stat Assoc. 2012;107(499):958–975. http://dx.doi.org/10.1080/01621459.2012.682828. [Google Scholar]
- 57.Cook NR, Ridker PM. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women's Health Study. JAMA Intern Med. 2014;174(12):1964–1971. doi: 10.1001/jamainternmed.2014.5336. http://dx.doi.org/10.1001/jamainternmed.2014.5336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. http://dx.doi.org/10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 59.NHLBI. Incidence and Prevalence Chart Book on Cardiovascular and Lung Diseases, 2006. 2009 www.nhlbi.nih.gov/resources/docs/cht-book_ip.htm.
- 60.National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program: Cancer Statistics Review (CSR) 1975-2011. [Accessed January 20, 2016]; http://seer.cancer.gov/archive/csr/1975_2011/browse_csr.php?sectionSEL=15&pageSEL=sect_15_table.19.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


