Abstract
Purpose
Young women of color in the United States are disproportionately affected by sexually transmitted infections (STIs). We characterize the protective behaviors used by young women to reduce their vulnerability to STI acquisition, and examine how STI prevention strategies differ by race/ethnicity.
Methods
From 2015–2016, women ages 13–24 presenting to five Northern California family planning clinics were surveyed about their STI prevention strategies. Chi-squared tests and multivariable logistic regression identified associations between race/ethnicity and use of sexual health-promoting strategies.
Results
Among 790 women, the most common strategies included condom use (67%), asking partners about STIs (47%), limiting sexual partners (35%), frequent STI screening (35%), and asking partners about other sexual partners (33%). Black, Hispanic, and Asian women had decreased odds of utilizing strategies prior to intercourse compared to White women (aORBlack 0.25 CI [0.14–0.47]; aORHispanic 0.36 CI [0.20–0.65]; aORAsian 0.44 CI [0.23–0.84]). Black women had decreased odds of using strategies requiring partner involvement (aORBlack 0.35 CI [0.13–0.92]). White women were more likely to report that providers discussed condoms (aOR 2.53 CI [1.04–6.15]) and asking partners about STIs (aOR 2.56 CI [1.52–4.32]) compared to non-White women. Black and Hispanic women were more likely to feel very uncomfortable discussing lifetime sexual partners (aORBlack 4.26 CI [1.36–13.30], aORHispanic 5.35 CI [1.79–15.99]) and condom use (aORBlack 3.05 CI [1.14–8.15], aORHispanic 2.86 CI [1.11–7.35]) with providers.
Conclusions
Young women use diverse strategies to prevent STIs that vary by race/ethnicity. Providers can use these findings to improve sexual health counseling and promote equitable education and services.
Keywords: sexually transmitted infections, adolescents, disparities, reproductive health, sexual behavior
Half of all sexually transmitted infections (STIs) in the United States occur in young adults age 15–24 years old, with striking racial/ethnic disparities in STI prevalence [1,2]. Young Black women have nearly four times the odds of having an STI compared to young White women [3]. Comparatively, rates of chlamydia, gonorrhea, and syphilis are nearly twice as high for young Hispanic women compared to White women [1,4]. Asian adolescents have comparatively lower rates of STIs, but are especially understudied in evaluations of sexual health outcomes [1,4].
Reasons for disparities in STIs are multifactorial, including structural and community factors. For example, studies suggest Black women are more likely to encounter a partner with an infection due to racially segregated partnerships. High incarceration rates among Black men result in a smaller pool of male partners. Monogamous Black women are therefore more likely to encounter a male partner who has an STI and/or has had multiple sexual partners in the past year [5–7]. For Hispanic women, relationship power differentials and desires for relationship intimacy have been described, which impact adolescents’ ability to negotiate condom use [8–9]. Furthermore, healthcare providers’ patterns of STI testing have been shown to vary by patient race/ethnicity, which may further propagate disparities in STIs [10]. Variable screening and treatment decisions may reflect provider bias and consequently contribute to minority patients’ disparate experiences with family planning care [11–12].
Individual factors may also contribute to disparities in STIs, and research to date has focused primarily on risk-taking behaviors in young women. While various behaviors are associated with STIs, sexual practices alone have not accounted for racial/ethnic disparities [13]. In fact, young Black women have higher rates of STIs despite having fewer partners, higher condom use, and being less likely to engage in oral and anal sex compared to young White and Hispanic women [13,14].
Limited studies explore how women use sexual health-promoting behaviors. Evidence suggests that young adults assess and manage their infection risks in a purposeful manner [15]. However, studies focus primarily on abstinence and condom use as STI prevention efforts, neglecting other health-promoting strategies used by young women [16–18]. Furthermore, no studies explore how these protective behaviors vary by race/ethnicity. This study aims to characterize health-promoting strategies used by young women to reduce their vulnerability to STIs, and to examine how these strategies differ by race/ethnicity. Secondarily, we identify differences in provider-patient discussions about STI prevention, young women’s comfort with discussing sexual health topics with providers, and young women’s preferences for characteristics of infection prevention methods.
Methods
This study is a sub-analysis of data collected as part of a larger cross-sectional study to evaluate patient perspectives on integration of pre-exposure prophylaxis for HIV prevention into family planning care. Participants were recruited from September 2015 to April 2016 from waiting rooms of five family planning clinics in the San Francisco Bay Area. Eligible participants in the overall study were English or Spanish-speaking, 13–45 year old women whose HIV status was negative or unknown, and were presenting for family planning services. Participants eligible for sub-analysis were 13–24 year-old women who were sexually active with men. Verbal informed consent was obtained from all participants, and parental consent was waived due to the confidential nature of the clinic services and low-risk nature of the study. The University of California San Francisco Institutional Review Board approved this study.
Participants completed a tablet-administered 15-minute anonymous survey including demographic information, sexual and reproductive health history, sexual practices, perceived STI risk, and worry about acquiring an STI. Women self-identified their race/ethnicity by selecting all that applied from a pre-specified list. Participants who indicated multiple racial/ethnic identities were first categorized as Hispanic ethnicity if they identified as Latina/Hispanic, while remaining multiracial individuals were assigned to their non-white racial identities for analysis [19]. Due to the small number of participants identifying as Native Hawaiian/Pacific Islander, these respondents were included in the Asian subgroup for analysis.
Participants were presented with a list of strategies to reduce vulnerability to STIs and were asked to identify which strategies they had used in the past six months. For analysis, health-promoting strategies were grouped into preparatory versus event-driven actions, and partner-independent versus partner-dependent actions. Preparatory actions used in advance of intercourse included limiting the number of partners or frequency of sex, having partners tested for STIs, asking partners about other sexual partners and STIs, and HIV pre-exposure prophylaxis. Event-driven actions were defined as strategies used during or after sex including condom use, changing the type of sex (vaginal, anal or oral), getting tested for STIs, and using HIV post-exposure prophylaxis. Partner-dependent actions necessitated discussion with or cooperation by a partner to carry out the strategy, including condoms, changing the type of sex, asking partner about other sexual partners or STIs, and requesting partners to test for STIs. Having sex exclusively with “safe” partners presumed to not have an STI was also categorized as partner-dependent, since this assumption is often shaped by partners’ disclosure or non-disclosure of risk factors or STI status.
Descriptive statistics were calculated, with differences assessed by Pearson’s chi-squared test for analysis of categorical variables and student’s t test for continuous variables. Covariates associated with race/ethnicity in bivariate analysis (p < 0.10) were included in logistic regression analysis of the primary outcome. Based on previously reported association with STIs, age, income, insurance, marital status, and having a prior STI were a priori determined to be included in adjusted analyses [20–24]. Multivariable analysis was performed to assess for association between race/ethnicity and use of any protective behaviors, preparatory actions, and partner-dependent actions, while adjusting for associated factors. Consistent with prior research on sexual health disparities, non-Hispanic White women were used as the reference group to permit comparison of results with other studies [3, 11].
We also use descriptive statistics to analyze young women’s report of discussions with providers about health-promoting strategies, comfort during sexual health conversations, and preferences for STI prevention methods by race/ethnicity. To assess comfort during sexual health discussions, participants responded on a 4-point Likert-type scale ranging from very uncomfortable to very comfortable with regards to how they felt about conversations with providers about condom use and lifetime sexual partners.
Results
In the parent study, 2,389 women were approached; 271 declined and 149 were ineligible, leaving 1,969 surveys for analysis. Seven hundred and ninety respondents met the age and eligibility requirements for this sub-analysis, of whom 15% were White, 24% were Black, 42% were Hispanic, and 19% were Asian. The majority of young women reported a household income of less than $60,000 a year and received public insurance (Table 1).
Table 1.
Characteristics of sample stratified by race/ethnicity (N=790)
| Total | White (n=115) | Black (n=193) | Hispanic (n=329) | Asian (n=153) | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| N (%) | n (%) | n (%) | n (%) | n (%) | ||
| Sociodemographics | ||||||
| Age, years | 0.04 | |||||
| 13–19 | 264 (33) | 29 (25) | 60 (31) | 127 (39) | 48 (31) | |
| 20–24 | 526 (67) | 86 (75) | 133 (69) | 202 (61) | 105 (69) | |
| Gender minoritya | 6 (1) | 1 (1) | 1 (1) | 0 (0) | 4 (3) | 0.08 |
| Completed high school/GED or less | 488 (62) | 59 (51) | 138 (72) | 217 (66) | 74 (48) | < 0.001 |
| Household income < $60,000 | 659 (83) | 94 (82) | 165 (86) | 279 (85) | 121 (79) | < 0.001 |
| Public Insurance | 401 (51) | 41 (36) | 134 (70) | 172 (52) | 54 (35) | < 0.001 |
| Ever married | 39 (5) | 4 (4) | 9 (5) | 24 (7) | 2 (1) | 0.08 |
| English is primary language | 589 (75) | 111 (97) | 186 (96) | 188 (57) | 104 (68) | < 0.001 |
| Only access reproductive healthcareb | 214 (27) | 22 (19) | 42 (22) | 111 (34) | 39 (26) | 0.001 |
| Reproductive Health | ||||||
| Ever pregnant | 337 (43) | 41 (36) | 120 (62) | 137 (42) | 39 (26) | < 0.001 |
| Current birth control method | ||||||
| None | 91 (12) | 8 (7) | 28 (15) | 39 (12) | 16 (11) | 0.24 |
| Emergency contraception | 4 (1) | 2 (2) | 0 (0) | 2 (1) | 0 (0) | 0.15 |
| Withdrawal/rhythm method | 31 (4) | 8 (7) | 6 (3) | 12 (4) | 5 (3) | 0.34 |
| Condoms/diaphragm | 230 (29) | 25 (22) | 62 (32) | 98 (30) | 45 (29) | 0.27 |
| Hormonal contraceptionc or intrauterine device | 425 (54) | 70 (61) | 94 (49) | 175 (53) | 86 (56) | 0.19 |
| Permanent method | 2 (1) | 0 (0) | 0 (0) | 1 (1) | 1 (1) | 0.62 |
Gender minority refers to individuals defined at birth as female, who identified their gender as male, transgender, genderqueer, or other than female.
Participants stated they only see a doctor when they are pregnant or for birth control visits.
Hormonal contraception includes pill, patch, ring, injection, implant, intrauterine contraception
p-values for overall racial/ethnic comparisons were calculated using chi-squared test.
Almost all (95%) young women reported having condomless sex in the past six months. Nearly one-third (29%) had been diagnosed with an STI in the past, and one in five (22%) had ever experienced intimate partner violence (Table 2). On a Likert-type scale, over half (54%) were at least somewhat worried about STIs and most (71%) believed someone in their age group is at least somewhat likely to acquire an STI, although few (10%) perceived themselves as at least somewhat likely to acquire an STI. In bivariate analysis, women aged 20–24 had decreased odds of being worried about STIs (OR 0.83 CI [0.62–1.12]) despite being more likely to perceive themselves (OR 1.76 CI [1.02–3.05]) and others their age (OR 1.72 CI [1.25–2.38]) as at increased risk of acquiring an STI. The majority (69%) reported having an STI prevention plan, with Black and White women being most likely to have a plan in bivariate analyses (p<0.001). Three quarters of women (72%) were very or somewhat satisfied with their STI prevention plan, and no racial/ethnic differences were found in satisfaction levels.
Table 2.
Sexual health characteristics, concerns about sexual health, and infection prevention plans by race/ethnicity (N=790)
| Total | White (n=115) | Black (n=193) | Hispanic (n=329) | Asian (n=153) | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| N (%) | n (%) | n (%) | n (%) | n (%) | ||
| Sexual Health | ||||||
| Lifetime # of sexual partners (median, IQR) | 4 (2–7) | 7 (4–14) | 4 (2–7) | 3 (2–6) | 3 (1–6) | < 0.001 |
| Ever had anal sex | 277 (35) | 57 (50) | 44 (23) | 119 (36) | 57 (37) | < 0.001 |
| Ever had an STI | 231 (29) | 29 (25) | 86 (45) | 81 (25) | 35 (23) | < 0.001 |
| Ever experienced interpersonal violence | 173 (22) | 35 (30) | 33 (17) | 81 (25) | 24 (16) | 0.006 |
| Ever threatened over condom negotiationa | 51 (6) | 8 (7) | 9 (5) | 24 (7) | 10 (7) | 0.69 |
| Ever exchanged sexb | 22 (3) | 2 (2) | 8 (4) | 7 (2) | 5 (3) | 0.49 |
| Sexual Health Concerns & Plans | ||||||
| Worried about STIsc | 424 (54) | 57 (50) | 93 (48) | 179 (54) | 95 (62) | 0.10 |
| Think they are likely to get an STId | 78 (10) | 14 (12) | 19 (10) | 28 (9) | 17 (11) | 0.68 |
| Think average person their age is likely to get an STIe | 560 (71) | 100 (87) | 123 (64) | 211 (64) | 126 (82) | < 0.001 |
| Have an STI prevention plan | 548 (69) | 87 (76) | 158 (82) | 210 (64) | 93 (61) | < 0.001 |
STI = sexually transmitted infection; refers to chlamydia, gonorrhea, syphilis, trichomonas, herpes, molluscum, genital warts/Human papilloma virus, and pelvic inflammatory disease
Refers to ever being threatened physically or emotionally when wanting to use a condom, or having sex without a condom due to fear of partner not having sex with them or breaking off relationship.
Exchanged sex for money, drugs, a place to stay, food, transportation, or something else.
In response to question: “How worried are you that you will get an STI in the next 5 years?”
In response to question: “How likely is it that you will get an STI in the next 5 years?”
In response to question: “How likely is it that an average person your age will get an STI in the next 5 years?”
p-values for overall racial/ethnic comparisons were calculated using chi-squared test and student’s t test
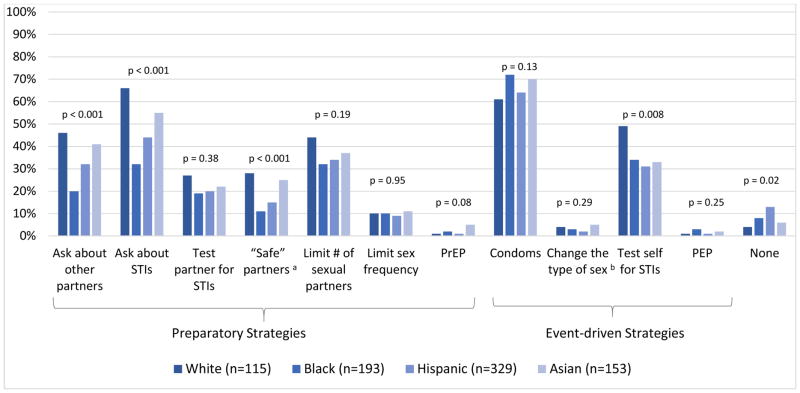
The majority of young women (91%) reported using at least one strategy to reduce their vulnerability to STIs, and over half (56%) used more than one strategy. The most commonly reported strategies included using condoms (67%), asking partners about STIs (47%), limiting sexual partners (35%), testing themselves for STIs (35%), and asking their partner about other sexual partners (33%) (Figure 1).
Figure 1. Prevalence of specific health-promoting behaviors used by young women to reduce vulnerability to STIs by race/ethnicity (N=790).
STI = sexually transmitted infection, PrEP = pre-exposure prophylaxis, PEP = post-exposure prophylaxis
a“Safe” partners refer to those whom subjects believed would not have HIV or other STIs
bChanging type of sex refers to engaging in less risky behaviors (for example, having oral sex instead of vaginal or anal sex)
p-values for overall racial/ethnic comparisons were calculated using chi-squared test.
Young women’s report of protective strategies varied by race/ethnicity for several methods. Adjusting for age, education, household income, insurance, marital status, English as a primary language, number of lifetime sexual partners, and history of an STI, multivariable logistic regression revealed that compared to White women, Black and Hispanic women were less likely to report having sex exclusively with “safe” partners who they perceived to not have an STI (aORBlack 0.28 CI [0.14–0.57], aORHispanic 0.45 CI [0.25–0.81]) and asking their partners about STIs (aORBlack 0.21 CI [0.12–0.37], aORHispanic 0.43 CI [0.26–0.72]). Black women were also less likely to ask their partners about other sexual partners (aORBlack 0.32 CI [0.18–0.58]). Furthermore, Black and Asian women had decreased odds of using frequent STI testing as a protective strategy (aORBlack 0.43 CI [0.25–0.75], aORAsian 0.53 CI [0.30–0.92]) compared to White women.
Adjusted multivariable regression of protective behavior categories revealed that Black, Hispanic, and Asian women were significantly less likely to use risk-reducing strategies in advance of intercourse compared to White women. In addition, Black women were also less likely to use partner-dependent protective strategies compared to White women, with Hispanic women approaching significance. There were no statistically significant racial/ethnic differences in use of any strategy versus no strategies to reduce vulnerability to infection (Table 3).
Table 3.
Associations between young women’s race/ethnicity and use of health-promoting behaviors (N=790)
| Any strategy vs. no strategy | Any preparatory actiona vs. no preparatory action | Any partner-dependent actionb vs. no partner-dependent action | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| aOR (95% CI) | p-value | aOR (95% CI) | p-value | aOR (95% CI) | p-value | |
| White | Reference | Reference | Reference | |||
| Black | 0.39 (0.12–1.27) | 0.12 | 0.25 (0.14–0.47) | < 0.001 | 0.35 (0.13–0.92) | 0.03 |
| Hispanic | 0.35 (0.11–1.08) | 0.07 | 0.36 (0.20–0.65) | 0.001 | 0.40 (0.16–1.01) | 0.05 |
| Asian | 0.76 (0.21–2.73) | 0.68 | 0.44 (0.23–0.84) | 0.01 | 0.61 (0.22–1.7) | 0.35 |
aOR = Adjusted odds ratio, CI = confidence interval
Multivariable logistic regression adjusted for age, income, education, insurance, marital status, primary language, lifetime sexual partners, and history of STI
Includes women using any of the following strategies before intercourse: using pre-exposure prophylaxis for HIV prevention, asking partners about other sexual partners or STIs, having partners tested for STIs, limiting number of sexual partners, limiting frequency of sex, only having sex with partners they think would not have an STI
Includes women using any of the following strategies that involve their partner: using condoms, changing type of sex they have, asking partners about other sexual partners or STIs, having partners tested for STIs, only having sex with partners they think would not have an STI
Young women reported many features were very important to them when choosing a health-promoting strategy. The most frequently reported characteristics were efficacy (84%), safety (83%), having few or no side effects (72%), preventing pregnancy in addition to STIs (67%), convenience (65%), and being able to control the method without relying on their partner for use (61%). Importance of these factors varied by race/ethnicity. Compared to White women, a higher proportion of Black, Hispanic, and Asian women valued a method that prevents pregnancy, offers privacy, does not require a clinic appointment, is preferred by a partner, and is recommended by a friend. Black and Hispanic women were also more likely to report that feeling comfortable discussing the method with a partner and the method not detracting from sexual enjoyment were very important considerations compared to White women’s responses (Table 4).
Table 4.
Young women’s preferences for STI prevention methods by race/ethnicity (N=790)
| Total | White (n=115) | Black (n=193) | Hispanic (n=329) | Asian (n=153) | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Very important features | N (%) | n (%) | n (%) | n (%) | n (%) | |
| Efficacy | 647 (84) | 100 (87) | 147 (76) | 266 (81) | 134 (88) | 0.06 |
| Safety | 633 (83) | 94 (82) | 147 (76) | 259 (79) | 133 (87) | 0.25 |
| Has few or no side effects | 552 (72) | 76 (66) | 139 (72) | 229 (70) | 108 (71) | 0.22 |
| Also prevents pregnancy | 512 (67) | 52 (45) | 130 (67) | 228 (69) | 102 (67) | < 0.001 |
| Convenience | 498 (65) | 69 (60) | 120 (62) | 203 (62) | 106 (69) | 0.12 |
| Able to control use (do not have to rely on partner for use) | 456 (61) | 72 (63) | 106 (55) | 185 (56) | 93 (61) | 0.08 |
| Privacy (no one can tell I’m using the method) | 401 (54) | 34 (30) | 112 (58) | 179 (54) | 76 (50) | < 0.001 |
| Comfortable discussing method with partner | 396 (53) | 42 (37) | 106 (55) | 173 (53) | 75 (49) | 0.001 |
| Recommended by a doctor | 401 (53) | 50 (44) | 97 (50) | 172 (52) | 82 (54) | 0.01 |
| Cost | 372 (49) | 50 (44) | 84 (44) | 157 (48) | 81 (53) | 0.21 |
| Can use method without seeing a provider (does not require a clinic appointment) | 339 (45) | 30 (26) | 97 (50) | 147 (45) | 65 (43) | < 0.001 |
| Does not detract from sexual enjoyment | 296 (40) | 26 (23) | 93 (48) | 125 (38) | 52 (34) | < 0.001 |
| Partner’s preference | 230 (31) | 13 (11) | 77 (40) | 100 (30) | 40 (26) | < 0.001 |
| Recommended by a friend | 226 (30) | 17 (15) | 67 (35) | 101 (31) | 41 (27) | < 0.001 |
STI = sexually transmitted infections
p-values for overall racial/ethnic comparisons were calculated using chi-squared test
Women reported discussing with healthcare providers the following STI prevention methods: condoms (83%), talking to partners about STIs (57%), testing themselves for STIs (55%), testing partners for STIs (37%), limiting number of sexual partners (30%), how different types of sex affect STI risk (12%), and pre- or post-exposure prophylaxis (12%). Compared to Black, Hispanic and Asian women, White women had nearly three times the odds of reporting that a healthcare provider spoke to them about condoms (aOR 2.53 CI [1.04–6.15]) and talking to their partners about STIs (aOR 2.56 CI [1.52–4.32]). This finding was consistent between unadjusted and adjusted analyses for age, education, household income, insurance, marital status, English as a primary language, number of lifetime sexual partners, and history of an STI. There were no racial/ethnic differences among other provider discussions about STI prevention methods.
Though the majority of young women felt very comfortable discussing condom use (65%) and the number of sexual partners (56%) with healthcare providers, 11% felt very uncomfortable with each of these conversations as measured by a Likert-type scale. Compared to young White women, young Black and Hispanic women were significantly more likely to feel very uncomfortable discussing condom use (aORBlack 3.05 CI [1.14–8.15], aORHispanic 2.86 CI [1.11–7.35]) and lifetime sexual partners (aORBlack 4.26 CI [1.36–13.30], aORHispanic 5.35 CI [1.79–15.99]) with providers. This held true in univariate and multivariate analyses adjusting for age, education, household income, insurance, marital status, English as a primary language, number of lifetime sexual partners, history of an STI, history of intimate partner violence, threats over condom negotiation, and history of exchange sex and lifetime sexual partners.
Discussion
In this diverse sample of young women, the majority of participants reported using at least one health-promoting strategy to reduce their vulnerability to STIs. Which method(s) women used to promote sexual health, as well as their preferences for method characteristics, varied by race/ethnicity. While women discussed a variety of health-promoting strategies with healthcare providers, Black and Hispanic women were more likely to feel very uncomfortable during sexual health conversations compared to White women.
Differences in use of protective behaviors may partially contribute to higher rates of STIs among Black and Hispanic young women. Reasons for differences in health-promoting behaviors cannot be determined by this study. While the higher proportion of White women utilizing testing services may be due to their increased number of sexual partners, these findings also raise the possibility of disparities in healthcare access, comfort seeking sexual health care, or knowledge about how STI testing and treatment reduce risk of new infections [25–26]. Considering that a positive STI test also increases the likelihood of partner treatment, interventions to improve patient knowledge and use of STI screening may facilitate curtailing reinfection rates and reducing community STI prevalence [27].
Differences in use of partner-dependent strategies by race/ethnicity were striking, and may relate to power inequities in sexual partnerships [28–29]. While White and Hispanic women were more likely to report any history of intimate partner violence, there were no racial/ethnic differences in experiencing threats over condom negotiation. These are likely inadequate markers of the complex factors impacting use of a partner-dependent method or not; future research should explore the role of partners of health-promoting strategies, and how to incorporate partners to promote young women’s and men’s sexual health.
The majority of young women in this study believed their risk of STI acquisition was lower than the risk posed to other women their age. While this may be a reflection of women being more aware of their own efforts to decrease vulnerability to infection compared to others’, this optimism bias may hinder efforts to promote protective behaviors [30]. The high incidence of condomless sex and prior STI diagnoses in this sample suggests a need for comprehensive counseling to assist young women in accurately estimating their vulnerability to STIs so they can make informed decisions about adopting protective strategies. Furthermore, qualitative research is needed to understand why young women may become less worried about STIs with increasing age despite increased perceived STI vulnerability. This apparent contradiction may influence sexual behaviors and the adoption of health-promoting strategies.
Although women use diverse strategies to prevent STIs, providers discuss a limited number of prevention strategies with young women. High rates of condomless sex in the past six months highlight the importance of additional protective behaviors, as inconsistent condom use has been implicated as having equivalent or higher risk of infection compared with no condom use [31]. Qualitative research suggests that adolescents and young adults associate condom use with a lack of trust in their partner, which may serve to decrease condom use [32]. If providers only discuss STI prevention in the context of condom use, they may inadvertently miss opportunities to discuss other ways in which women actively mediate vulnerabilities to STIs.
Young women may be unaware of the diversity of strategies available to promote their sexual health. This study identifies opportunities for clinicians and educators to both reinforce health-promoting strategies used by young women and increase awareness of other protective behaviors, in turn facilitating development of strategies that align with young women’s needs and values.
Strengths-based counseling that focuses on what women already do and can do, rather than what they should not do, may help empower adolescents and young women to promote their own sexual health, especially among young women in higher-risk sexual networks [33]. Positive youth asset-development programs have shown long-term reductions in STI risk factors by supporting young people in developing their own strengths such as decision-making skills, communicating expectations, self-determination, and planning for the future [34–35]. By eliciting strategies used by young women, providers can use a strengths-based approach to encourage and support young women’s preferences, abilities, and values.
Emerging evidence also demonstrates how providers can use shared decision-making to incorporate an adolescent’s context and preferences into these discussions [36]. Using this framework, a provider develops trust; elicits patient preferences, values and abilities; provides evidence-based information; facilitates decision-making; and emphasizes opportunity for continued conversations [37]. Literature on shared decision-making for STI prevention is limited, but research in similar populations demonstrates women prefer shared decision-making in contraceptive counseling [38]. Considering young women’s broad range of preferences regarding STI prevention methods, clinicians have the opportunity to provide patient-centered care that elicits young women’s individual values and preferences when discussing STI prevention. Providers can help young women weigh competing priorities, match preferences to methods, and collaboratively decide on the best strategies for each woman.
Shared decision-making is founded on providers and patients having a trusting relationship, and limited data suggest trust is related to clinical outcomes [39]. In our study, Black and Hispanic young women were significantly more likely to feel very uncomfortable in discussions of lifetime sexual partners and condom use. This lack of comfort may be due to prior experiences of discrimination or distrust in family planning or other healthcare visits, and has critical implications for young Black and Hispanic women’s healthcare [11–12]. Using a shared decision-making approach can help providers focus on developing trust and cultural humility, which may be important to not only reduce disparities in STIs, but improve women’s long-term health.
Limitations of this study include its being a cross-sectional, convenience sample of young women presenting to family planning care in the San Francisco Bay Area, limiting generalizability. Due to the cross-sectional design, the study does not address how sexual behaviors and protective strategies change over time nor what specific strategy or combination of strategies improve STI protection. In addition, we were unable to quantify in what proportion of sexual acts each strategy was used. All data were based on self-report, and social desirability and recall bias may be present. While the choices of strategies offered to participants may not capture the full spectrum of what methods women are using, women were given the option of indicating additional strategies if needed.
This study recruited a large, racially and ethnically diverse group of young women presenting for family planning services. Candid responses were enhanced by the anonymous nature of the study, and the high response rate decreased risk of selection bias. This study adds to the existing literature by including information on a wide range of protective behaviors, rather than limiting inquiry to condoms and abstinence.
The U.S. Preventative Services Task Force and Centers for Disease Control recommend high-intensity behavioral counseling for all sexually-active adolescents and for adults at increased risk of STIs [40]. Brief, individualized counseling in the clinical setting has been shown to significantly reduce sexual risk behaviors and STI reinfection rates, especially among adolescents with a history of STIs [33]. Identifying what methods young women use to promote their sexual health is essential to not only gain women’s trust, but to guide counseling sessions that are contextualized by young women’s preferences, abilities and values. Our findings suggest that though many young women utilize methods to reduce their vulnerability to STIs, racial/ethnic differences in these protective behaviors may contribute to disparities in STI rates. Further exploration is needed to understand why young women choose certain sexual health-promoting strategies over others and how providers can best partner with patients in determining an optimal health promotion strategy. Furthermore, we must ensure equal access to sexual health education and services in order to promote positive sexual health outcomes and reduce disparities in young women’s sexual health.
Implications and Contribution.
Young women use diverse strategies to reduce their vulnerability to sexually transmitted infections (STIs). Racial/ethnic differences in protective behaviors may contribute to disparities in STIs. Further research should explore the reasons driving variable protective practices, and interventions to promote the sexual health of all young women.
Acknowledgments
This research was supported by grants through the Society of Family Planning Research Fund and the UCSF PROF-PATH program funded by the National Institute on Minority Health and Health Disparities (R25MD006832). This publication was made possible in part by the Clinical and Translational Research Fellowship Program (TL1 TR000144). The findings and conclusions in this article are those of the authors and do not necessarily represent the views of Planned Parenthood Federation of America, Inc.
Footnotes
Conflict of interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2014. Atlanta: U.S. Department of Health and Human Services; 2015. [Google Scholar]
- 2.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sexually transmitted diseases. 2013;40(3):187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 3.Forhan SE, Gottlieb SL, Sternberg MR, et al. Prevalence of Sexually Transmitted Infections Among Female Adolescents Aged 14 to 19 in the United States. Pediatrics. 2009;124(6) doi: 10.1542/peds.2009-0674. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control (CDC) NCHHSTP Atlas. [Accessed May 10, 2016]; Available at: http://gis.cdc.gov/grasp/nchhstpatlas/main.html?value=AQT.
- 5.Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis. 1999;26(5):250–61. doi: 10.1097/00007435-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Morris M, Kurth AE, Hamilton DT, et al. Concurrent Partnerships and HIV Prevalence Disparities by Race: Linking Science and Public Health Practice. American Journal of Public Health. 2009;99(6):1023–31. doi: 10.2105/AJPH.2008.147835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barry PM, Kent CK, Klausner JD. Risk factors for gonorrhea among heterosexuals—San Francisco, 2006. Sex Transm Dis. 2009;36(Suppl 2):S62–6. doi: 10.1097/OLQ.0b013e31815faab8. [DOI] [PubMed] [Google Scholar]
- 8.Brady SS, Tschann JM, Ellen JM, et al. Infidelity, trust, and condom use among Latino youth in dating relationships. Sex Transm Dis. 2009;36(4):227–31. doi: 10.1097/OLQ.0b013e3181901cba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arteaga S, Gomez AM. “Is that a method of birth control?” A qualitative exploration of young women’s use of withdrawal. The Journal of Sex Research. 2015;53(4–5):626–32. doi: 10.1080/00224499.2015.1079296. [DOI] [PubMed] [Google Scholar]
- 10.Wiehe SE, Rosenman MB, Wang J, Fortenberry JD. Disparities in chlamydia testing among young women with sexually transmitted infection symptoms. Sex Transm Dis. 2010;37(12):751–5. doi: 10.1097/OLQ.0b013e3181e50044. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 12.Dehlendorf C, Rodriguez MI, Levy K, Borrero S, et al. Disparities in family planning. Am J Obstet Gynecol. 2010;202(3):214–20. doi: 10.1016/j.ajog.2009.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pflieger JC, Cook EC, Niccolai LM, Connell CM. Racial/ethnic differences in patterns of sexual risk behavior and rates of sexually transmitted infections among female young adults. Am J Public Health. 2012;103(5):903–9. doi: 10.2105/AJPH.2012.301005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buhi ER, Marhefka SL, Hoban MT. The State of the union: sexual health disparities in a national sample of US college students. J Am Coll Health. 2010;58(4):337–46. doi: 10.1080/07448480903501780. [DOI] [PubMed] [Google Scholar]
- 15.Hock-Long L, Henry-Moss D, Hatfield-Timajchy K, et al. Condom use with serious and casual heterosexual partners: findings from a community venue-based survey of young adults. AIDS Behav. 2013;17(3):900–13. doi: 10.1007/s10461-012-0177-2. [DOI] [PubMed] [Google Scholar]
- 16.Hensel DJ, Fortenberry JD. A multidimensional model of sexual health and sexual and prevention behavior among adolescent women. J Adolesc Health. 2013;52(2):219–27. doi: 10.1016/j.jadohealth.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beadnell B, Morrison DM, Wilsdon A, et al. Condom use, frequency of sex, and number of partners: multi-dimensional characterization of adolescent sexual risk-taking. J Sex Res. 2005;42(3):192–202. doi: 10.1080/00224490509552274. [DOI] [PubMed] [Google Scholar]
- 18.Gielen AC, Faden RR, O’Campo P, et al. Women’s protective sexual behaviors: a test of the health belief model. AIDS Educ Prev. 1994;6(1):1–11. [PubMed] [Google Scholar]
- 19.Office of Management and Budget (OMB) [Accessed April 28, 2016];Statistical policy directive No. 1, race and ethnic standards for federal statistics and administrative reporting. 2000 OMB Bulletin No. 00-02. Accessed at: http://wonder.cdc.gov/wonder/help/populations/bridged-race/Directive15.html. [PubMed]
- 20.Hogben M, Leichliter JS. Social Determinants and Sexually Transmitted Disease Disparities. Sexually Transmitted Diseases. 2008 Dec;35(12 Suppl):S13–8. doi: 10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 21.Harling G, Subramanian S, Barnighausen T, Kawachi I. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sexually transmitted diseases. 2013;40(7):575–81. doi: 10.1097/OLQ.0b013e31829529cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sales JM, Smearman EL, Swartzendruber A, et al. Socioeconomic-related risk and sexually transmitted infection among African-American adolescent females. J Adolesc Health. 2014;55(5):698–704. doi: 10.1016/j.jadohealth.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fortenberry JD, Brizendine EJ, Katz BP, Orr DP. Post-treatment sexual and prevention behaviours of adolescents with sexually transmitted infections. Sex Transm Infect. 2002;78(5):365–8. doi: 10.1136/sti.78.5.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Campo P, Deboer M, Faden RR, et al. Prior episode of sexually transmitted disease and subsequent sexual risk-reduction practices. A need for improved risk-reduction interventions. Sex Transm Dis. 1992;19(6):326–30. [PubMed] [Google Scholar]
- 25.Mayer KH, Venkatesh KK. Interactions of HIV, other sexually transmitted diseases, and genital tract inflammation facilitating local pathogen transmission and acquisition. American Journal of Reproductive Immunology. 2011;65(3):308–16. doi: 10.1111/j.1600-0897.2010.00942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004;2(1):33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Expedited partner therapy in the management of sexually transmitted diseases. Atlanta, GA: US Department of Health and Human Services; 2006. [Google Scholar]
- 28.Matson PA, Chung SE, Huettner S, Ellen JM. Understanding variability in adolescent women’s sexually transmitted infection-related perceptions and behaviors associated with main sex partners. Sex Transm Dis. 2014;41(8):475–9. doi: 10.1097/OLQ.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 29.Peipert JF, Lapane KL, Allsworth JE, et al. Women at risk for sexually transmitted diseases: correlates of intercourse without barrier contraception. Am J Obstet Gynecol. 2007;197(5):474e47–478. doi: 10.1016/j.ajog.2007.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinstein ND. Optimistic biases about personal risks. Science. 1989;246(4935):1232–3. doi: 10.1126/science.2686031. [DOI] [PubMed] [Google Scholar]
- 31.Ahmed S, Lutalo T, Wawer M, et al. HIV incidence and STD prevalence associated with condom use in Rakai, Uganda. AIDS. 2001;15(16):2171–9. doi: 10.1097/00002030-200111090-00013. [DOI] [PubMed] [Google Scholar]
- 32.Marston C, King E. Factors that shape young people’s sexual behaviour: a systematic review. The Lancet. 2006;368(9547):1581–6. doi: 10.1016/S0140-6736(06)69662-1. [DOI] [PubMed] [Google Scholar]
- 33.Diclemente RJ, Wingood GM, Sionean C, et al. Association of Adolescents’ History of Sexually Transmitted Disease (STD) and Their Current High-Risk Behavior and STD Status: A Case for Intensifying Clinic-Based Prevention Efforts. Sexually Transmitted Diseases. 2002;29(9):503–9. doi: 10.1097/00007435-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Gavin LE, Catalano RF, David-Ferdon C, et al. A review of positive youth development programs that promote adolescent sexual and reproductive health. J Adolesc Health. 2010;46(3 Suppl):S75–91. doi: 10.1016/j.jadohealth.2009.11.215. [DOI] [PubMed] [Google Scholar]
- 35.Svanemyr J, Amin A, Robles OJ, Greene ME. Creating an Enabling Environment for Adolescent Sexual and Reproductive Health: A Framework and Promising Approaches. Journal of Adolescent Health. 2015;56(1 Suppl):S7–14. doi: 10.1016/j.jadohealth.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 36.Knapp C, Madden V, Feeg V, et al. Decision making experiences of adolescents enrolled in children’s medical services network. Institute for Child Health Policy University of Florida; 2008. [Google Scholar]
- 37.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17:285–94. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 38.Dehlendorf C, Levy K, Kelley A, et al. Women’s preferences for contraceptive counseling and decision making. Contraception. 2013;88(2):250–6. doi: 10.1016/j.contraception.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dehlendorf C, Henderson JT, Vittinghoff E, et al. Association of the Quality of Interpersonal Care During Family Planning Counseling with Contraceptive Use. American Journal of Obstetrics and Gynecology. 2016 doi: 10.1016/j.ajog.2016.01.173. pii: S0002-9378(16)00223-4. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 40.Lin JS, Whitlock E, O’Connor E, Bauer V. Behavioral Counseling to Prevent Sexually Transmitted Infections: A Systematic Review for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2008;149:497–508. doi: 10.7326/0003-4819-149-7-200810070-00011. [DOI] [PubMed] [Google Scholar]