Abstract
The Finnish HPV Family Study is a prospective cohort study assessing the dynamics of human papillomavirus (HPV) transmission between parents and infant. Serial genital and oral scrapings from 76 families, including mother, father, and infant, and semen samples were collected over 2 years of follow-up, analyzed by nested PCR, and confirmed by hybridization with 12 high-risk (HR) HPV types. The most common HPV profile was HR HPV in all family members (29%), followed by HPV-positive mother-infant pairs (26%). HPV-positive father-infant pairs were less frequent (11%), and in six (8%) families, only the infant was HR HPV positive. The prevalence of genital HR HPV in the parents ranged from 13 to 25%, and that of oral HPV ranged from 8 to 34%. In the infants, HPV DNA was detected in 15% of the genital and 10% of the oral samples at birth, reaching peaks of 18 and 21%, respectively, at 6 months, and declining to 10% at 24 months. Persistent HPV in the mother was a risk factor for oral HPV in the infant (odds ratio [OR], 5.69; 95% confidence interval [95% CI], 1.5 to 21.3), while oral HPV in the mother at 6 months was a risk factor for genital HR HPV (OR, 6.38; 95% CI, 1.15 to 35.32). No such independent risk could be attributed to subclinical HPV in the father. Persistent maternal cervical HPV and subclinical oral HPV affect the risk of infant HPV. The age of 6 months is a critical point for the infant to acquire or be free of HR HPV DNA.
Several studies have confirmed the detection of human papillomavirus (HPV) in children, but the transmission modes are still partly unknown. Sexual abuse has been claimed to be the source of genital infections in some cases (21), but nonsexual modes of HPV transmission also have to be considered. These include vertical transmission from parents to infants, horizontal transmission from other family members and those in close contact with the child, autoinoculation from one site to another, and possibly indirect transmission via fomites (23).
In utero transmission could be caused either by ascending infection from an infected birth canal or hematogenously, via the placenta. HPV DNA has been detected in amniotic fluid (18, 30), fetal membranes (27), placental trophoblastic cells (4), and infants born by cesarean section (4, 16, 25, 27, 30), as well as in spontaneously aborted material (7). Vertical transmission from mother to infant is well documented (4, 14, 16, 24-27). The concordance between HPV types detected in infants and their mothers ranges from 57 to 69%, suggesting that HPV infections in infants may be acquired from sources other than the mother (23).
The possible role of the father as a vertical transmitter of HPV has not been systematically evaluated before. However, HPV reservoirs may exist in men's genitalia, mostly in intraurethral epithelia (6, 15), and in the vas deferens (17). A possible vehicle of HPV transmission from father to infant is the sperm, via fertilization. HPV DNA has been detected in 8 to 64% of semen samples from asymptomatic men (2, 6, 13, 19), both in the seminal plasma and in spermatozoa (11). Furthermore, HPV is actively transcribed in sperm cells (10, 11).
Most of the previous studies on transmission have focused on genital HPV, while the role of oral HPV has not been studied. However, oral HPV DNA has been detected in 40% of infants (14, 16, 25) and in 10 to 67% of adults (22). The aim of the present study was to evaluate the frequency and persistence of high-risk (HR) HPV in infants and their parents. In addition, the infant's risk of acquiring HPV from the parents was studied. This is the first prospective study of HPV detection at multiple sites within families.
MATERIALS AND METHODS
Patients.
The Finnish HPV Family Study is a prospective follow-up cohort study performed at the Department of Obstetrics and Gynecology, Turku University Central Hospital (TUCH) and Institute of Dentistry, Faculty of Medicine, University of Turku. The Joint Commission on Ethics of Turku University and TUCH has approved the study protocol (#3/1998). Written informed consent was obtained from the participants. Young pregnant women in the third trimester, fathers-to-be, and infants participated in the study. Voluntary enrollment of families was started in September 1998, and at the moment 76 families, including 1 family with twins, have completed the 2-year follow-up.
Samples.
The types of samples (2,522 in all) taken for HR HPV DNA testing and the times of sampling (from before delivery to 2 years after delivery) are given in Table 1. A routine Pap smear was taken by using the conventional three-sample technique (vagina, exocervix, endocervix) with two wooden spatulas and a cytobrush (MedScand, Malmö, Sweden). The slide was fixed with a preservative (Spray-Cyte; Becton Dickinson and Company, Sparks, Md.).
TABLE 1.
Samples taken from the mother, father and infant during follow-up
| Sample taken | Before deliverya | At delivery | 2-3 days | 1 mo | 2 mo | 6 mo | 12 mo | 24 mo |
|---|---|---|---|---|---|---|---|---|
| Mother | ||||||||
| Pap smear | X | X | X | |||||
| Cervical mucosa | X | X | X | X | ||||
| Oral mucosa | X | X | X | X | X | |||
| Father | ||||||||
| Semen | X | |||||||
| Urethra | X | |||||||
| Oral mucosa | X | X | X | X | X | |||
| Infant | ||||||||
| Genital mucosa | X | X | X | X | X | X | X | |
| Oral mucosa | X | X | X | X | X | X | X |
At the time of enrollment.
Scrapings for HPV DNA testing were taken from the cervical mucosa of the mother, the distal part of the urethral mucosa of the father, the labias or preputium and scrotum of the infant, and the oral mucosae (without touching the tongue) of all subjects by using a small brush (Cytobrush; MedScand). The brushes were placed in a tube containing 70% ethanol except for the cervical sample, which was placed in a tube with 0.05 M phosphate-buffered saline (PBS) with 100 μg of gentamicin. The samples were immediately frozen (−20°C) and then stored at −70°C.
A semen sample from the father was taken into a plastic container by masturbation after at least 2 days of abstinence. If taken at home, the sample was transferred to the laboratory within 2 h after ejaculation. Samples were centrifuged in a Sorval MC12V (Zurich, Switzerland) at 3,500 rpm for 15 min. Seminal plasma and semen cells were stored separately, first at −20°C and afterwards at −70°C.
HPV DNA testing.
DNA was extracted by the high-salt method (12) from all samples except semen samples, for which the High Pure PCR template preparation kit (Boehringer, Mannheim, Germany) was used according to the manufacturer's instructions. HPV DNA was detected by nested PCR using MY09-MY11 and GP05+-GP06+ as external and internal primers, respectively (17). For cervical scrapings, only GP05+-GP06+ was used. The specificity of all PCR products was confirmed by hybridization with digoxigenin-labeled HR HPV (types 16, 18, 31, 33, 35, 39, 45, 51, 52, 54, 56, and 58) oligoprobes (17). All PCR products for the infants were also hybridized with HPV type 6 (HPV6) and HPV11 oligoprobes to detect the most prevalent low-risk HPV types.
The sensitivity of the PCR method is at least 20 copies of HPV; 20 SiHa cells mixed with 300 ng of human fibroblast DNA become strongly positive by this method.
Controls for PCR.
For evaluation of the possible contamination during DNA extraction, DNA was simultaneously extracted from cultured human fibroblasts. Only eight study samples were processed at the same time. For each set of eight samples, we had one fibroblast control. Additionally, every eighth sample for PCR contained no DNA. DNA dilution of SiHa cells was used as a positive control for HPV DNA detection. DNA extraction, the making of the master mix for PCR, and the adding of target DNA to the reaction mixture were all done in separate rooms.
Statistical analyses.
Statistical analyses were performed with the SPSS computer software package (version 11.5 for Windows). Frequency tables were analyzed by using the chi-square test, with Pearson and likelihood ratio (LR) tests for the significance of differences between the categorical variables. Odds ratios (ORs) and 95% confidence interval (95% CI) were calculated where appropriate. Differences in the means of continuous variables between the groups were analyzed by using nonparametric tests or analysis of variance, when applicable. Concordance between the paired samples (mother-infant, father-infant, etc.) was analyzed by using the two-sample or K-related sample t test (Wilcoxon, McNemar, or Friedman test).
Multiple logistic regression models were used to analyze the power of different variables as predictors of HPV positivity of the infant by using the stepwise backward approach with LR statistics. Variables were entered into the model with a P value of 0.10 being the probability for stepwise removal and a P value of 0.05 being the probability for stepwise entry. Both crude and adjusted ORs are given, where indicated. In all analyses, probability values of <0.05 were regarded as significant.
RESULTS
This study includes 76 consecutive families, 1 of which has twins, of the Finnish HPV Family Study. The mean ages of mothers and fathers were 25.0 years (range, 18 to 35 years) and 28.1 years (range, 19 to 43 years), respectively. The mean gestational age at delivery was 40 weeks (range, 36 to 42 weeks). Sixty-three (82%) mothers had a vaginal birth, and 14 (18%) had a caesarean section. Overall, 25 and 16% of the mothers and the fathers, respectively, reported previous genital warts, and 4 and 10%, respectively, reported previous oral warts. The prevalence of current HPV infections as reported by the parents ranged from 1 to 7%. Ten (27%) mothers and 10 (29%) fathers reported previous Chlamydia infections. The high proportion of parents with reported allergies (42 to 43%) might be a consequence of the possibility of an allergy nurse consultation in connection with the present study.
HPV detection in the families.
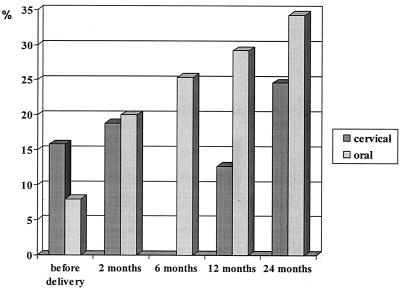
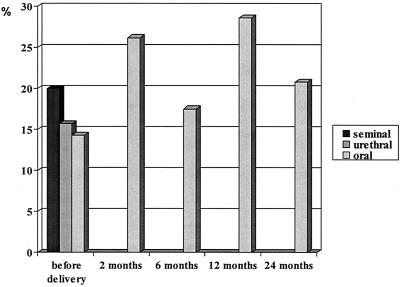
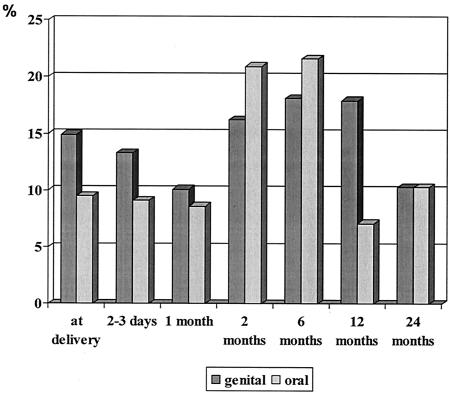
Figures 1, 2, and 3 summarize the rates of detection of HPV DNA in the oral and genital samples of the parents and infant. HPV DNA positivity of the maternal oral and cervical samples ranged from 8 to 34% and from 13 to 25%, respectively (Fig. 1). Nine (12%) pregnant mothers were diagnosed with Pap smear class II upon enrollment in the study. Only two out of nine Pap smear class II samples were shown to contain HPV DNA. At months 12 and 24, Pap smear class II was diagnosed only in 8 and 6% of the mothers, respectively. Of the paternal samples taken at enrollment, HPV was found most frequently in semen samples (20%), followed by urethral (16%) and oral (14%) samples. The rate of detection of HPV DNA in oral samples ranged from 14 to 29% during the follow-up (Fig. 2). In infants, the highest rates of detection of HPV were found at the age of 6 months, both in the oral (22%) and in the genital (18%) samples (Fig. 3). Altogether, five oral and five genital samples of the infants tested positive for low-risk HPV types 6 and 11. One infant had HPV6 and HPV11 DNA detectable in the genital sample at day 3 and month 12 and in the oral sample at month 6. An additional infant had HPV6- and HPV11-positive oral and genital samples at month 6.
FIG. 1.
Rates of detection of cervical and oral high-risk HPV DNA in mothers during the 2-year follow-up.
FIG. 2.
Rates of detection of seminal, urethral, and oral high-risk HPV DNA in fathers during the 2-year follow-up.
FIG. 3.
Rates of detection of genital and oral high-risk HPV DNA in infants during the 2-year follow-up.
HPV dynamics in the families are shown in Table 2. Only 2.6% of the families were totally HPV DNA negative. In 22 families (29%), HPV DNA was detected in all family members. HPV DNA was more frequent in mother-infant than in father-infant pairs (26 versus 11%). However, in six (8%) families, only the infant was HPV positive, as determined by any sample positive for HPV.
TABLE 2.
Detection of HPV DNA in the members of the 76 families
| HPV DNA detectiona
|
No. (%) of families | ||
|---|---|---|---|
| Infant | Mother | Father | |
| + | + | + | 22 (29.0) |
| + | + | − | 20 (26.3) |
| + | − | + | 8 (10.5) |
| + | − | − | 6 (7.9) |
| − | + | − | 4 (5.3) |
| − | − | + | 3 (3.9) |
| − | + | + | 11 (11.4) |
| − | − | − | 2 (2.6) |
+, at least one positive HR HPV DNA sample; −, HR HPV DNA negative.
HPV status of the parents related to genital and oral HPV of the infant.
The acquisition of HR HPV DNA by the infant in his or her oral or genital mucosa was related to the HPV status of the parents (Table 3). Only the infant's genital HPV at discharge was significantly related to oral HR HPV detected in the mother before delivery; only the infant's oral HPV at the age of 6 months was significantly related to oral HR HPV detected in the father before delivery. In addition to the data presented in the table, there was also a borderline association between the infant's genital HR HPV at discharge and 1 month after delivery and the urethral and oral HR HPV of the father detected before delivery.
TABLE 3.
HPV status of the mother and the father associated with the infant's acquisition of HR HPV in the genital tract and oral mucosa by univariate analysis
| Infant's acquisition of HR HPV (dependent variable) | HPV status in mother and/or father | OR | 95% CI | Significance |
|---|---|---|---|---|
| Genital HPV, at discharge | Oral HPV in mothera | NCb | NC | 0.001c |
| Oral HPV in fathera | 4.714 | 0.921-24.139 | 0.081 | |
| Oral HPV | ||||
| 2 mo | Cervical HPV at 2 monthsd | 3.056 | 0.811-11.526 | 0.097 |
| 6 mo | Oral HPV in father-to-be-e | NC | NC | 0.047c |
| Oral HPV in father at 6 monthse | NC | NC | 0.090c | |
| 24 mo | Cervical HPV before deliveryf | 4.875 | 0.916-25.943 | 0.81 |
Factors included in the analysis were the mother's and father's HPV status before delivery.
NC, not computable.
By Pearson's test.
Factors included in the analysis were the mother's and father's HPV status before delivery and at 2 months.
Factors included in the analysis were the mother's and father's HPV status before delivery and at 6 months.
Factors included in the analysis were the mother's and father's HPV status before delivery and at 24 months.
Logistic regression analysis was used to reveal the factors in the maternal and paternal HPV status (as covariates) predisposing the infant to acquisition of oral HR HPV, genital HR HPV, or any HR HPV sample positive during the 24-month follow-up (dependent variable). Both crude and adjusted ORs were calculated, as indicated in Table 4. The OR for an infant to have oral HPV DNA (any sample positive) was nearly sixfold if the mother's genital sample was HR HPV DNA positive at month 24 (i.e., if she was a chronic HPV carrier) (adjusted OR, 5.695; 95% CI, 1.521 to 21.323; P < 0.010). The infant's risk of acquiring genital DNA was associated with the mother's oral HPV positivity at month 6 (OR, 6.385; 95% CI, 1.154 to 35.323; P = 0.034). Interestingly, maternal oral HPV at 2 months (OR, 0.115; 95% CI, 0.015 to 0.864; P = 0.036) and 12 months (OR, 0.127; 95% CI, 0.025 to 0.635; P = 0.012) showed an inverse correlation.
TABLE 4.
Maternal and paternal HPV status as determinants of infant positivity for genital, oral, or any HPV in logistic regression analysis
| HPV status of Infant | Covariate | Crude OR (95% CI) | Adjusted ORa (95% CI) |
|---|---|---|---|
| Oral HPV in any sample | Cervical HPV at 24 mo | 4.432 (1.272-15.444) | 5.695 (1.521-21.323) |
| Genital HPV in any sample | Oral HPV of mother at 2 mo | 0.278 (0.079-0.974) | 0.115 (0.015-0.864) |
| Genital HPV in any sample | Oral HPV of mother at 6 mo | 0.893 (0.306-2.603) | 6.385 (1.154-35.323) |
| Genital HPV in any sample | Oral HPV of mother at 12 mo | 0.350 (0.121-1.015) | 0.127 (0.025-0.635) |
| HPV in any sample | Oral HPV of mother at 12 mo | 0.396 (0.129-1.214) | 0.233 (0.055-0.983) |
Adjusted for all other HPV samples of the mother and father.
DISCUSSION
The Finnish HPV Family Study was designed to evaluate the natural history of HPV infections of the infant, as well as the transmission of HPV between the parents and the infant. The present report is focused on the dynamics and risk factors associated with the acquisition of HR HPV by infants.
HPV DNA is frequently found in at least one sample from both the oral and the genital mucosae of both parents, as well as in the infant (9, 16, 17, 23). The rate of detection of cervical HR HPV DNA during pregnancy has been reported to range from 1 to 32% (3, 14, 24-26). The peak incidence of genital HPV infections is encountered in women between the ages of 20 and 24 years (20, 22). The present rate of detection of HR HPV DNA (16%) in these young pregnant women (mean age, 25 years) falls well within this frame. On the other hand, HPV DNA was detected in 16% of the urethral samples of the fathers-to-be, a finding in agreement with data reported previously (29), including those of our previous study, where the rate of detection of penile HPV DNA among young military conscripts was 17% (8). The concept of asymptomatic males as transmitters of HPV to their sexual partners is generally accepted and is supported by these observations, among others (17, 22, 23). However, no earlier data are available on the eventual modes of HPV spread from the father to his infant.
That such a spread exists is clearly favored by the present study. The rate of detection of genital HR HPV DNA in infants was not negligible. Altogether, 15% of the genital samples taken from the infants immediately after delivery were positive for HR HPV DNA, and 13% of the infants were HR HPV positive at discharge. Even significantly higher detection rates have been reported in three studies, where HR HPV DNA was found in 19 to 61% of genital samples at 24 h (1, 14) and at 3 to 4 days (25) after delivery. The frequency and methods of sampling, as well as differences in the sensitivity of the HPV assays used, may explain the divergent results (22, 23). In our study, HPV DNA was measured by sensitive nested PCR, and the results were confirmed by Southern blot hybridization, precluding the false HPV positive samples inherent in studies relying on PCR alone (22).
Also, the rates of detection of oral HR HPV in neonates vary within a broad range, from 0 to 79% (1, 24, 28). These divergent figures are explained by the factors mentioned above. The rates of detection of HR HPV DNA in the oral swab samples from the neonates in the present study are at the lower end of this range: 10% immediately after delivery and 9% at discharge. However, these figures are in line with our previous results on HPV DNA detection in the nasopharyngeal aspirates of neonates (16), as well as with those of two additional reports, where the rates of HPV DNA detection in buccal swab samples from infants were analyzed (14, 25).
When individual families (with a mother, father, and infant) are considered as study subjects, eight distinct profiles of HPV detection are established. The most common HPV profile (29%) is that in which all three family members demonstrate at least one HR HPV-positive sample during the 24 months of follow-up. This is one indication that HR HPV infections spread among families. For further studies, the most interesting HPV profiles are those of families in which all members are infected persistently and totally HPV negative families.
The dynamics of subclinical HR HPV infections in neonates can be established only by prospective follow-up and repeated sampling. The present data suggest that these infections are subject to fluctuation over time. Rates of detection of oral and genital HPV DNA decreased during the first month of neonatal life. This “regression” could easily be explained by the neutralizing antibodies derived transplacentally from the mother and still functionally active in the neonatal circulation. Interestingly, however, at the age of 6 months, 18% of genital and 22% of oral samples were HR HPV DNA positive. This coincides with the period when the infant's own immune system is at its weakest and circulating maternal antibodies have disappeared. At the age of 12 months, rates of detection of oral HPV DNA dropped to 7%, which could be due to maternal antibodies received from breast feeding. Our figures are lower than those reported in two studies, where HR HPV DNA was detected in 20 to 23% of the oral samples at least 6 weeks after delivery (5, 14) and persistent HPV16 DNA was detected in 83% of oral or genital samples after 6 months of follow-up (1). We have previously reported the persistence of oral HPV DNA for as long as 3 years (16). However, persistence of oral HPV DNA has not been detectable in all follow-up studies (24, 28). Such a fluctuation in oral samples stresses the importance of repeated sampling.
In this study only HR HPVs were detected in parents and infants. Thus, at this stage, we do not know the overall concordance between the HPV types in parents and infants. However, we have shown previously that there is 69% concordance between HPV types in mothers and their infants (16).
The mechanisms of HPV transmission between family members are of great interest but until now have been poorly understood (22, 23). The HPV Family Study in Finland attempts to address the problem of intrafamily transmission by evaluating HR HPV DNA status at multiple sites over 2 years of follow-up. In adults, the rates of detection of low-risk and HR HPV in clinically normal oral mucosae have ranged from 10 to 67% (22). In the present study, the prevalence of HR HPV DNA in the mothers' oral mucosae increased from 8 to 34% over 2 years of follow-up and fluctuated between 14 and 29% in the fathers. These oral reservoirs of HR HPV might be potential sources of virus transmission to the neonates, as well as of genital infections.
By the univariate approach, as seen in Table 3, the presence of HR HPV in the oral mucosa of the mother prior to delivery seemed to be associated with detection of genital HR HPV in the infant at discharge. The other significant association was found between oral HR HPV of the father-to-be and oral HR HPV of the infant at 6 months. These findings indicate that the risk of HPV transmission to the infant cannot be based on a simple temporal association with the parents' HPV status.
Finally, an effort was made using multiple logistic regression analysis to disclose the dynamics of the parents' HPV status (used as covariates) as determinants of the HPV exposure of the infant, with (i) any oral HR HPV-positive, (ii) any genital HR HPV-positive, or (iii) any HR HPV-positive sample as the dependent variable. Cervical HR HPV during the pregnancy was not a risk factor for acquisition of either oral or genital HPV by the infant at any stage during follow-up. However, a persistent cervical HR HPV infection of the mother detected at 24 months after delivery was the strongest risk factor for acquisition of oral HPV DNA by the infant. This finding indicates that persistent HR HPV infections, in addition to being a significant risk factor for cervical cancer (22), also predispose an infant to contracting this virus. Interestingly, no such risk could be attributed to any of the “paternal factors,” i.e., the urethral, seminal, or oral HPV of the fathers in this study.
Another significant observation was the high adjusted OR for infant genital HPV if the mother had HR HPV in her oral sample at 6 months after delivery. This is a period of maximal immunological vulnerability of the infant, because of the immature immune system and the limited protection provided by the maternal antibodies. It coincides with the period when the prevalence of both oral and genital HR HPV in the infant has reached its peak, followed by a rapid decline by the age of 12 months. Of interest in this respect also is the association of the infant's oral HPV at 6 months with the detection of oral HR HPV in the father-to-be. The protective effect of the mother's oral HPV at 2 and 12 months could also be explained by immunological mechanisms, i.e., by neutralizing antibodies from the mother at 2 months and those of the infant at 12 months. Taken together, these observations suggest that the age of 6 months seems to be critical for the infant to acquire or be free of HR HPV infections.
To conclude, the Finnish HPV Family Study indicates that families with different HPV profiles exist, with those in which all members have HR HPV and those completely negative for the virus as the two extremes. As in adults, detection of HR HPV in infants is a dynamic process, with substantial fluctuation over time. Persistent cervical HR HPV was shown to be a significant risk factor for infant oral HPV, while maternal oral HR HPV at 6 months was a risk factor for infant genital HPV. However, the mechanisms of HPV transmission are highly complex and are associated with the development of the infant's own immune system during the first months of life.
Acknowledgments
This work was supported by The Päivikki and Sakari Sohlberg Foundation, Helsinki, Finland; The Government Special Foundation for the Turku University Central Hospital, Turku, Finland; The Medical Research Council of the Academy of Finland, Helsinki, Finland; The South-Western Division of the Finnish Cancer Society, Turku, Finland; and The Turku University Foundation, Turku, Finland.
Special thanks are due to Elisa Hovinmäki, Johanna Järvi, Ulla-Maija Ericsson, and Satu Sivula for taking all the samples. The technical assistance of Sarita Järvinen, Sari Mäki, Ulla Mikkola, Niina Niemi, and Tatjana Peskova in the HPV laboratory is gratefully acknowledged. We also thank Ville Jussila and Julia Ruotsi for entry of these data into SPSS files and Kari Syrjänen for help with the statistical analysis. Most of all, we express our gratitude to the collaborating parents who made this study possible.
REFERENCES
- 1.Cason, J., J. N. Kaye, R. J. Jewers, P. K. Kambo, J. M. Bible, B. Kell, B. Shergill, F. Pakarian, K. S. Raju, and J. Best. 1995. Perinatal infection and persistence of human papillomavirus types 16 and 18 in infants. J. Med. Virol. 47:209-218. [DOI] [PubMed] [Google Scholar]
- 2.Chan, P. J., B. C. Su, T. Kalugdan, I. M. Seraj, D. R. Tredway, and A. King. 1994. Human papillomavirus gene sequences in washed human sperm deoxyribonucleic acid. Fertil. Steril. 61:982-985. [DOI] [PubMed] [Google Scholar]
- 3.Eppel, W., C. Worda, P. Frigo, M. Ulm, E. Kucera, and K. Czerwenka. 2000. Human papillomavirus in the cervix and placenta. Obstet. Gynecol. 96:337-341. [DOI] [PubMed] [Google Scholar]
- 4.Favre, M., S. Majewski, N. De Jesus, M. Malejczyk, G. Orth, and S. Jablonska. 1998. A possible vertical transmission of human papillomavirus genotypes associated with epidermodysplasia verruciformis. J. Investig. Dermatol. 111:333-336. [DOI] [PubMed] [Google Scholar]
- 5.Fredericks, B. D., A. Balkin, H. W. Daniel, J. Schonrock, B. Ward, and I. H. Frazer. 1993. Transmission of human papillomaviruses from mother to child. Aust. N. Z. J. Obstet. Gynaecol. 33:30-32. [DOI] [PubMed] [Google Scholar]
- 6.Green, J., E. Monteiro, V. N. Bolton, P. Sanders, and P. E. Gibson. 1991. Detection of human papillomavirus DNA by PCR in semen from patients with and without penile warts. Genitourin. Med. 67:207-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hermonat, P. L., L. Han, P. J. Wendel, J. G. Quirk, S. Stern, C. L. Lowery, and T. M. Rechtin. 1997. Human papillomavirus is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes 14:13-17. [DOI] [PubMed] [Google Scholar]
- 8.Hippeläinen, M., S. Syrjänen, M. Hippeläinen, H. Koskela, J. Pulkkinen, S. Saarikoski, and K. Syrjänen. 1993. Prevalence and risk factors of genital human papillomavirus (HPV) infections in healthy males: a study on Finnish conscripts. Sex. Transm. Dis. 20:321-328. [PubMed] [Google Scholar]
- 9.Kellokoski, J. K., S. M. Syrjänen, F. Chang, M. Yliskoski, and K. J. Syrjänen. 1992. Southern blot hybridization and PCR in detection of oral human papillomavirus (HPV) infections in women with genital HPV infections. J. Oral Pathol. Med. 21:459-464. [DOI] [PubMed] [Google Scholar]
- 10.Lai, Y. M., J. F. Lee, H. Y. Huang, Y. K. Soong, F.-P. Yang, and C. C. Pao. 1997. The effect of human papillomavirus infection on sperm cell motility. Fertil. Steril. 67:1152-1155. [DOI] [PubMed] [Google Scholar]
- 11.Lai, Y. M., F.-P. Yang, and C. C. Pao. 1996. Human papillomavirus deoxyribonucleic acid and ribonucleic acid in seminal plasma and sperm cells. Fertil. Steril. 65:1026-1030. [PubMed] [Google Scholar]
- 12.Miller, S. A., D. D. Dykes, and H. F. Polesky. 1988. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 16:1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olatunbosun, O., H. Deneer, and R. Pierson. 2001. Human papillomavirus DNA detection in sperm using polymerase chain reaction. Obstet. Gynecol. 97:357-360. [DOI] [PubMed] [Google Scholar]
- 14.Pakarian, F., J. Kaye, J. Cason, B. Kell, R. Jewers, N. Derias, K. S. Raju, and J. M. Best. 1994. Cancer associated human papillomaviruses: perinatal transmission and persistence. Br. J. Obstet. Gynecol. 101:514-517. [DOI] [PubMed] [Google Scholar]
- 15.Pakendorf, U. W., M. S. Bornman, and D. J. Du Plessis. 1998. Prevalence of human papillomavirus in men attending the infertility clinic. Andrologia 30:11-14. [DOI] [PubMed] [Google Scholar]
- 16.Puranen, M. H., M. H. Yliskoski, S. V. Saarikoski, K. J. Syrjänen, and S. M. Syrjänen. 1997. Exposure of an infant to cervical human papillomavirus infection of the mother is common. Am. J. Obstet. Gynecol. 176:1039-1045. [DOI] [PubMed] [Google Scholar]
- 17.Rintala, M., P. Pöllänen, V. Nikkanen, S. Grénman, and S. Syrjänen. 2000. Human papillomavirus DNA is found in the vas deferens. J. Infect. Dis. 185:1664-1667. [DOI] [PubMed] [Google Scholar]
- 18.Rogo, K. O., and P. N. Nyansera. 1989. Congenital condylomata acuminata with meconium staining of amniotic fluid and fetal hydrocephalus. East Afr. Med. J. 66:411-413. [PubMed] [Google Scholar]
- 19.Rohde, V., K. Erles, H. P. Sattler, H. Derouet, B. Wullich, and J. R. Schlehofer. 1999. Detection of adeno-associated virus in human semen: does viral infection play a role in the pathogenesis of male infertility? Fertil. Steril. 72:814-816. [DOI] [PubMed] [Google Scholar]
- 20.Sellors, J. W., J. B. Mahony, J. Kaczorowski, A. Lytwyn, H. Bangura, S. Chong, A. Lorincz, D. M. Dalby, V. Janjusevic, J. L. Keller, et al. 2000. Prevalence and predictors of human papillomavirus infection in women in Ontario, Canada. CMAJ 165:503-508. [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens-Simmon, C., D. Nelligan, P. Breese, C. Jenny, and J. Douglas. 2000. The prevalence of genital human papillomavirus infections in abused and nonabused preadolescent girls. Pediatrics 106:645-649. [DOI] [PubMed] [Google Scholar]
- 22.Syrjänen, K., and S. Syrjänen. 2000. Papillomavirus infections in human pathology, 1st ed. Wiley, New York, N.Y.
- 23.Syrjänen, S., and M. Puranen. 2000. Human papillomavirus infections in children: the potential role of maternal transmission. Crit. Rev. Oral Biol. Med. 11:259-274. [DOI] [PubMed] [Google Scholar]
- 24.Tenti, P., R. Zappatore, P. Migliora, A. Spinillo, C. Belloni, and L. Carnevali. 1999. Perinatal transmission of human papillomavirus from gravidas with latent infections. Obstet. Gynecol. 93:475-479. [DOI] [PubMed] [Google Scholar]
- 25.Tseng, C.-J., C.-C. Liang, Y.-K. Soong, and C.-C. Pao. 1998. Perinatal transmission of human papillomavirus in infants: relationship between infection rate and mode of delivery. Obstet. Gynecol. 91:92-96. [DOI] [PubMed] [Google Scholar]
- 26.Tseng, C.-J., C.-Y. Lin, R.-L. Wang, L.-J. Chen, Y.-J. Chan, T.-T. Hsien, and C. C. Pao. 1992. Possible transplacental transmission of human papillomaviruses. Am. J. Obstet. Gynecol. 166:35-40. [DOI] [PubMed] [Google Scholar]
- 27.Wang, X., Q. Zhu, and H. Rao. 1998. Maternal-fetal transmission of human papillomavirus. Chin. Med. J. 111:726-727. [PubMed] [Google Scholar]
- 28.Watts, D. H., L. A. Koutsky, K. K. Holmes, D. Goldman, J. Kuypers, N. B. Kiviat, and D. A. Galloway. 1998. Low risk of perinatal transmission of human papillomavirus: results from a prospective cohort study. Am. J. Obstet. Gynecol. 178:365-373. [DOI] [PubMed] [Google Scholar]
- 29.Wikström, A., C. Popescu, and O. Forslund. 2000. Asymptomatic penile HPV infection: a prospective study. Int. J. STD AIDS 11:80-84. [DOI] [PubMed] [Google Scholar]
- 30.Xu, S., L. Liu, S. Lu, and S. Ren. 1998. Clinical observation on vertical transmission of human papillomavirus. Chin. Med. Sci. J. 13:29-31. [PubMed] [Google Scholar]