Abstract
Accurate and timely diagnosis of severe acute respiratory syndrome coronavirus (SARS-CoV) infection is a critical step in preventing another global outbreak. In this study, 829 serum specimens were collected from 643 patients initially reported to be infected with SARS-CoV. The sera were tested for the N protein of SARS-CoV by using an antigen capture enzyme-linked immunosorbent assay (ELISA) based on monoclonal antibodies against the N protein of SARS-CoV and compared to 197 control serum samples from healthy donors and non-SARS febrile patients. The results of the N protein detection analysis were directly related to the serological analysis data. From 27 SARS patients who tested positive with the neutralization test, 100% of the 24 sera collected from 1 to 10 days after the onset of symptoms were positive for the N protein. N protein was not detected beyond day 11 in this group. The positive rates of N protein for sera collected at 1 to 5, 6 to 10, 11 to 15, and 16 to 20 days after the onset of symptoms for 414 samples from 298 serologically confirmed patients were 92.9, 69.8, 36.4, and 21.1%, respectively. For 294 sera from 248 serological test-negative patients, the rates were 25.6, 16.7, 9.3, and 0%, respectively. The N protein was not detected in 66 patients with cases of what was initially suspected to be SARS but serologically proven to be negative for SARS and in 197 serum samples from healthy donors and non-SARS febrile patients. The specificity of the assay was 100%. Furthermore, of 16 sera collected from four patients during the SARS recurrence in Guangzhou, 5 sera collected from 7 to 9 days after the onset of symptoms were positive for the N protein. N protein detection exhibited a high positive rate, 96 to 100%, between day 3 and day 5 after the onset of symptoms for 27 neutralization test-positive SARS patients and 298 serologically confirmed patients. The N protein detection rate continually decreased beginning with day 10, and N protein was not detected beyond day 19 after the onset of symptoms. In conclusion, an antigen capture ELISA reveals a high N protein detection rate in acute-phase sera of patients with SARS, which makes it useful for early diagnosis of SARS.
Severe acute respiratory syndrome (SARS) is an emerging infectious disease of significant public health concern. Due to the recurrence of SARS in Guangzhou and Beijing, China, we would like to stress the tremendous importance of sensitive, easy, and reliable early diagnosis of the SARS coronavirus (SARS-CoV) infection. The three major diagnostic methods currently available are (i) viral RNA detection using real-time reverse transcription (RT)-PCR (8, 15, 20), (ii) antibody detection using indirect immunofluorescence assay (2), or (iii) using both the recombinant N protein and culture extracts of SARS-CoV-based enzyme-linked immunosorbent assay (ELISA) (10, 16, 19). Although RT-PCR is a useful assay during the early phase of SARS-CoV infection with regard to sensitivity, it relies heavily on experienced technicians and specialized laboratory equipment and sometimes provides false-positive results due to contamination. Serological tests, however, do not provide early diagnosis, since the median time to seroconversion in patients with SARS is 17 to 20 days after the onset of symptoms (14). Since SARS-CoV appears in the blood much earlier than the antibodies (21), the identification of SARS-CoV antigen in sera may provide a possible method for early diagnosis of SARS. Since the nucleocapsid (N) proteins of known coronaviruses are relatively conserved, immunogenic, and abundantly expressed during infection (6, 9), we tried to determine whether the N protein is a potential early diagnostic marker for SARS. Recently, we reported the development of an antigen-capture ELISA based on monoclonal antibodies (MAbs) against the N protein of SARS-CoV (4). High levels of circulating N protein can be detected in the sera of patients with SARS (3). In this study, we further evaluate its early diagnostic value by using a large number of clinical samples collected between 2 February and 5 May 2003, during the SARS epidemic in Guangzhou, People's Republic of China. The serum specimens from the recurrence of SARS in Guangzhou are also analyzed (12).
MATERIALS AND METHODS
Clinical samples.
A total of 829 serum specimens were collected at 1 to 115 days after the onset of symptoms from 643 patients who were reported to have probable or suspicious symptoms of SARS between 2 February and 5 May 2003 during the SARS epidemic in Guangzhou. Of these patients, 204 had paired serum specimens available for serologic analysis, in which the acute-phase serum specimens were collected at day 1 to day 15 and the convalescent-phase serum specimens were subsequently obtained at day 28 or longer after the onset of illness. Sixteen serum specimens were collected from four patients during the recurrence of SARS in Guangzhou from 22 December 2003 to 30 January 2004. Another 197 serum specimens were used as controls. Of these samples, 30 sera were identified as positive for the influenza immunoglobulin G (IgG) antibody at a fourfold increase in antibody titer, 35 sera were identified as positive for the dengue IgM antibody, 32 sera were identified as positive for the measles IgM antibody, and 100 sera were from healthy blood donors. All of the serum specimens were stored at −20°C until tested.
MAb-based antigen capture ELISA for detection of SARS-CoV nucleocapsid protein.
Cloning and purification of the glutathione S-transferase-nucleocapsid fusion protein and development of monoclonal antibodies specific to the N protein of SARS-CoV have been reported previously (5). Evaluation of the MAb-based ELISA for detection of the N protein of SARS-CoV in sera and viral cell culture supernatant has been described previously (4). Briefly, Costar microtiter wells (Corning Incorporated) coated with a mixture of three different antinucleocapsid monoclonal antibodies, N10E4, N1E8, and N8E1, were vacuum dried and stored at 4°C before use. One hundred microliters of serum was added to the wells of the microtiter plate coated with the mixture of three anti-nucleocapsid protein MAbs, and the plates were incubated at 37°C for 60 min. After the wells were washed in phosphate-buffered saline with 0.05% Tween 20, antinucleocapsid rabbit serum was added at a 1:4,000 dilution and the plate contents were incubated at 37°C for 1 h. After the wells were washed, a 1:5,000 diluted horseradish peroxidase-conjugated goat anti-rabbit antibody (Zymed Laboratory Inc., South San Francisco, Calif.) was added. After three further washes, 100 μl of tetramethylbenzidine solution was added to each well. The reaction was stopped by adding 50 μl of 0.5 N sulfuric acid, and the plates were examined at 450 nm. Samples with an absorbance at 450 nm above the cutoff value (mean of negative control + [2.56 × standard deviation of 1,272 healthy blood donors]) (4) were considered positive.
Detection of SARS-CoV neutralizing activity with a neutralization test.
Serum specimens were tested for neutralizing activity according to the previously described procedures with modifications (22). Briefly, 56°C heated serum specimens were serially diluted from 1:20 to 1:1,280 and then mixed with 100 50% tissue culture infective doses of SARS-CoV. After incubation for 1 h at 37°C, the mixture was inoculated in triplicate into 96-well plates of Vero E6 cell cultures. Cultures were held at 37°C and 5% CO2, with daily observations for cytopathic effect (CPE). The results were determined after 3-day incubation at 37°C. A sample was considered positive if the neutralization antibody exhibited at least a fourfold increase in titers between the acute- and convalescent-phase serum specimens in the paired specimens group.
Detection of SARS-CoV-specific IgG antibody with indirect ELISA.
IgG antibody of SARS-CoV was tested by using the ELISA test kit manufactured by Beijing Huada GBI Biotechnology Co. Ltd., Beijing, People's Republic of China. The assay was performed according to the manufacturer's instructions. One hundred microliters of specimen diluent was added to each well, and 10 μl of sera was added, mixed, and incubated for 30 min at 37°C. The plates were washed six times with washing solution, and 100 μl of working conjugate (anti-human IgG horseradish peroxidase conjugate) was added and incubated for 30 min at 37°C. After the plates were washed, 100 μl of substrate was added and incubated for 10 min at 37°C. The reaction was stopped by adding 50 μl of stop solution, and the plates were examined at 450 nm. Samples with an absorbance at 450 nm above the cutoff value (mean of negative control + 0.13) were considered positive.
To ensure biosafety, the experiments using sera from patients for the ELISA were performed in a biosafety level 2 laboratory, and the neutralization test was performed in a biosafety level 3 laboratory.
RESULTS
Serum specimens (829 specimens) were tested for the N protein of SARS-CoV by using MAb-based antigen capture ELISA for 639 patients who were reported likely to be infected with the SARS-CoV. These 639 patients were divided into four groups by using confirmation through serological diagnosis. The results of N protein detection obtained were directly related to the serological analysis data.
Group I, comprising 27 patients who had paired or more than two serum specimens, were subsequently confirmed to have SARS-CoV infections on the basis of both being neutralization test positive and seroconversion. In these 27 patients, there were 41 serum specimens taken at day 2 to day 20 after the onset of illness, which were available for N protein analysis. Among the 41 samples, 100% of the 24 serum specimens collected from days 2 to 10 after the onset of symptoms were positive for N protein. However, the N protein was not detected beyond day 11 in this group (Table 1).
TABLE 1.
Results of the N protein of SARS-CoV assay for sera from patients with SARS in the neutralization test-positive group
| Days after onset of symptoms | No. of patients with positive sera/total no. of patients with SARS (%) |
|---|---|
| 1-5 | 19/19 (100) |
| 6-10 | 5/5 (100) |
| 11-15 | 0/11 (0) |
| 16-20 | 0/6 (0) |
Group II comprised 298 patients subsequently confirmed to be infected with SARS-CoV due to a positive serological analysis. Among these patients, 111 exhibited seroconversion (for those who had paired or more than two serum specimens), for which the acute- and convalescent-phase serum specimens were collected at day 1 to 15 and at 28 or more days after the onset of illness, respectively. For the other 187 patients in this group, only a single serum specimen was collected during the illness and a serological analysis showed IgG to be positive for SARS-CoV. For this group of 298 patients, 419 serum specimens were available for N protein analysis. The N protein positive rates for this group collected during days 1 to 5, 6 to 10, 11 to 15, 16 to 20, and 21 to 115 after the onset of symptoms were 92.9, 69.8, 36.4, 16.7, and 0%, respectively (Table 2).
TABLE 2.
Results of the N protein of SARS-CoV assay for sera from patients with SARS in the serological test-positive group
| Days after onset of symptoms | No. of patients with positive sera/total no. of patients with SARS (%) |
|---|---|
| 1-5 | 78/84 (92.9) |
| 6-10 | 44/63 (69.8) |
| 11-15 | 12/33 (36.4) |
| 16-20 | 4/19 (16.7) |
| 21-115 | 0/220 (0) |
Group III comprised 248 patients whose convalescent-phase sera taken beyond 28 days were not available. From these 248 patients, 294 serum specimens were collected between 1 and 27 days after symptom onset. Of these samples, 284 (96.5%) were collected between 1 and 20 days after symptom onset and 10 samples were collected between 21 and 27 days after symptom onset; serological tests were negative for all samples. Because of the lack of convalescent-phase serum obtained from these patients, we could not judge how many patients were truly infected with SARS-CoV. However, the N protein-positive rates for this group for samples collected during days 1 to 5, 6 to 10, 11 to 15, 16 to 20, and 21 to 27 after the onset of fever were 25.6, 16.7, 9.3, 0, and 0%, respectively (Table 3).
TABLE 3.
Results of the N protein of SARS-CoV assay for sera from patients with SARS in the serological test-negative group
| Days after onset of symptoms | No. of patients with positive sera/total no. of patients with SARS (%) |
|---|---|
| 1-5 | 34/133 (25.6) |
| 6-10 | 14/84 (16.7) |
| 11-15 | 4/43 (9.3) |
| 16-20 | 0/24 (0) |
| 21-27 | 0/10 (0) |
Group IV, comprising 66 patients who had paired serum specimens and who were subsequently excluded based on their convalescent-phase serum specimens collected beyond 28 days after symptom onset, were negative for SARS-CoV antibodies. There were 75 serum specimens from these 66 patients available for N protein analysis. The N protein was not detected in this group (Table 4).
TABLE 4.
Results of the N protein of SARS-CoV assay for sera from the excluded SARS patients
| Days after onset of symptoms | No. of patients with positive sera/total no. of patients with SARS (%) |
|---|---|
| 1-5 | 0/43 (0) |
| 6-10 | 0/12 (0) |
| 11-15 | 0/5 (0) |
| 16-20 | 0/1 (0) |
| 21-67 | 0/14 (0) |
In addition, 30 serum specimens collected from influenza patients, 35 specimens from dengue patients, and 32 specimens from measles patients, which were serologically confirmed, and 100 serum specimens from healthy donors were negative for N protein detection. The specificity was 100% (Table 5).
TABLE 5.
Results of the N protein of SARS-CoV assay for sera from non-SARS fever patients and healthy donors
| Donor condition | No. of samples with positive sera/total no. of samples (%) |
|---|---|
| Influenza | 0/30 (0) |
| Dengue | 0/35 (0) |
| Measles | 0/32 (0) |
| Healthy donors | 0/100 (0) |
The N protein capture ELISA was also used to test 16 serum specimens collected from four patients who exhibited SARS during a recurrence of the disease with laboratory-confirmed SARS-CoV infection in Guangzhou from 22 December 2003 to 30 January 2004. As shown in Table 6, the N protein was detected in the serial serum specimens of three patients taken within 7 to 9 days after the onset of symptoms. For patient 4, the first serum sample was taken at day 17 after the onset of symptoms and the N protein was not detectable in his serial serum specimens during his illness.
TABLE 6.
Results of the N protein and IgG antibody of SARS-CoV assays for sera from four patients during the recurrence of SARS in Guangzhou
| Patient no.a | Days after onset of symptoms | Results of N protein detection | Results of SARS-CoV IgG detection |
|---|---|---|---|
| 1 (12/16/2003) | 6 | + | + |
| 8 | − | + | |
| 10 | − | + | |
| 12 | − | + | |
| 2 (12/26/2003) | 6 | + | − |
| 7 | + | + | |
| 8 | + | + | |
| 19 | − | + | |
| 10 | − | + | |
| 11 | − | + | |
| 3 (12/30/2003) | 9 | + | + |
| 10 | − | + | |
| 11 | − | + | |
| 4 (1/8/2004) | 16 | − | + |
| 17 | − | + | |
| 22 | − | + |
The date of the onset of symptoms is given after the patient number in month/day/year format.
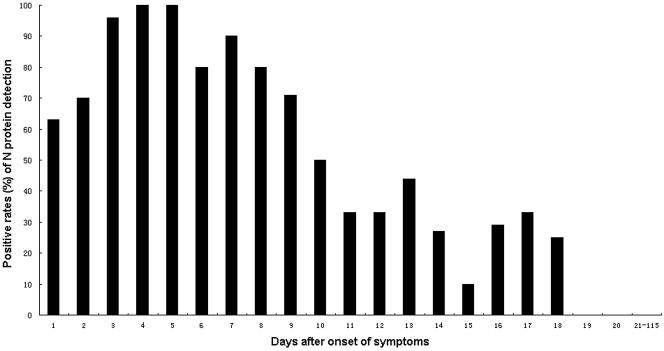
To further investigate the profile of N protein detection, a combination of 27 SARS patients who tested positive with the neutralization test and 298 SARS patients with serologically confirmed SARS-CoV infection were analyzed (Fig. 1). The highest positive rates (80 to 100%) were observed between day 3 and day 8 after the onset of symptoms, and nearly all sera were found to be positive for the N protein between day 3 and day 5 (96 to 100%). The detection rate of the N protein decreased after day 10 and was never detected beyond day 19 after the onset of symptoms.
FIG. 1.
The profile of the N protein of SARS-CoV in sera detected with MAb-based antigen capture ELISA from the onset of symptoms to the convalescent phase.
DISCUSSION
In a previous study, we demonstrated that SARS-CoV N protein could be detected by using MAb-based antigen capture ELISA in early acute phase serum specimens of patients with SARS (3, 4). In this study, we further confirmed these results using a large number of clinical samples as well as samples obtained during the recurrence of SARS in Guangzhou. Since SARS is a new and poorly understood disease, especially during the early breakout period, many non-SARS patients may be mislabeled as having SARS. Therefore, in order to evaluate the sensitivity and specificity of this assay accurately, data analysis was based on a serological diagnosis. Using samples from 325 patients with serologically confirmed SARS-CoV infection, N protein in 100% of the samples (19 of 19) from neutralization test-positive patients and 92.9% of the samples (78 of 84) from serologically confirmed patients taken from days 1 to 5 was detected with the assay. At days 6 to 10, 100% of the samples (5 of 5) from neutralization test-positive patients and 69.8% of the samples (44 of 63) from serologically confirmed patients were still positive for the N protein, and the detection rate of the N protein decreased in later samples. These results are consistent with those from our previous studies (3, 4). However, the N protein could be detected in 25.6% of the serum specimens (34 of 133) taken from days 1 to 5 and in 16.7% of the serum specimens (14 of 84) taken from days 6 to 10 after the onset of symptoms in patients exhibiting a negative result with SARS-CoV antibody detection (Group III). Since a few patients with SARS have had late seroconversion (11, 14), to rule out SARS, it is best to test a convalescent-phase serum collected beyond 28 days after the onset of symptoms (http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5228a4.htm). Although these patients were reported as likely to be infected with SARS-CoV according to the World Health Organization criteria, no convalescent-phase serum specimens collected beyond 28 days were available for those patients, and we do not know how many patients were truly infected with SARS-CoV. In addition, another 75 serum specimens from the “ruled-out” group and 197 control serum specimens from patients with influenza, dengue, and measles and healthy blood donors had been tested with the N protein capture ELISA, but no positive results were found. Based on serological diagnosis as the “gold standard, ” the results demonstrated that the antigen capture ELISA permitted a sensitive and specific detection of SARS-CoV N protein in clinical specimens.
Recent studies have shown that RT-PCR for SARS-CoV using nasopharyngeal aspirate samples appears to be the best supportive test for an early diagnosis. However, the variation in reported sensitivity and specificity makes it difficult for the RT-PCR to be considered the standard criterion for early diagnosis. Moreover, the best time for a high sensitivity for nasopharyngeal aspirate sampling was on days 8 to 10 after the onset of symptoms (18) or later (1). Waiting 8 to 10 days to make a firm diagnosis or to plan for appropriate therapy is not possible. Since it is important to diagnose and confirm SARS within the first few days of illness, we studied the N protein as an early diagnostic marker in 325 patients with serologically confirmed SARS-CoV infection. Using the antigen capture ELISA, we were able to demonstrate the presence of the N protein in some serum samples as early as day 1 and up to day 18 (Fig. 1), and nearly all sera were found positive for the N protein between days 3 and 5. The detection rates for the N protein of SARS-CoV in serum specimens showed a much higher percentage in blood during the first week of the illness than in subsequent weeks. The N protein in blood, therefore, is considered a good diagnostic marker during the early stage of the SARS-CoV infection. Since the N protein appears relatively stable to freezing and thawing and is stable for many months frozen at −20°C, detection of the N protein in serum samples retrospectively did not seem to affect the overall detection rate. In contrast, the storage of the specimens at −70°C, which is essential for RT-PCR in order to maintain viral RNA in optimal conditions, is not feasible in many nonresearch laboratories. In addition, the use of serum specimens for diagnosing SARS-CoV infection has the advantage of not requiring respiratory specimens, including sputum, nasopharyngeal aspiration, and endotracheal tube samples, which are regarded as a risk to health care workers.
Previous studies on coronaviruses have shown that the N protein is highly conserved, immunogenic, and abundantly expressed during infection (6, 9). Recent serological studies using the N protein-based ELISA have demonstrated that SARS patient sera contained a high level of antibodies against the N protein (16, 19). An immunohistochemical assay using a MAb specific for the N protein of SARS-CoV has demonstrated that the N protein was predominantly detected not only in the lung but also in many other organs and tissues in patients with SARS (7). The presence of N protein in the early acute-phase sera of patients with SARS in our findings suggests that the N protein of SARS-CoV may be a major viral target and released from the virus or infected cell into the blood at an early stage of infection. If so, these features make N protein a suitable candidate for early diagnostic application, and an N protein-based assay will provide good sensitivity. So far, it is still not clear whether SARS-CoV undergoes a high rate of genetic mutation, although some differences have been observed between the viral genomes sequenced (13).
To date, the correlation between virus loading and the clinical outcome remains unclear, although recent studies have demonstrated that the clinical outcomes for SARS patients with RT-PCR-positive serum or SARS patients with high viral loads are worse in general (17, 18). In our previous studies, the optical density of the N protein was highly variable from one individual to another on the same day (3). It is unclear from these data whether this variation predicts clinical outcome. However, based on the clinical data available, we were not able to find any significant differences associated with disease severity and levels of circulating N antigen in the patients with SARS. Previous studies of animal coronavirus have shown that the N protein plays an important role in viral pathogenesis and replication (9). Future experiments are planned to address the mechanism by which the N protein of SARS-CoV is presented in blood as a viral antigen and its role in viral pathogenesis and/or replication.
In conclusion, the high sensitivity of the capture ELISA in detecting SARS-CoV N protein in serum samples makes it a useful early laboratory diagnosis tool for SARS. This method overcomes several problems associated with the RT-PCR approach. For example, the problems due to contamination of RT-PCR products are not an issue in antigen detection assays. In addition, ELISA is rapid and easy to perform and can be carried out in less-well-equipped laboratory settings. Widely employing this assay will enhance our ability to provide a rapid response in the event of a return outbreak of SARS.
Acknowledgments
This work was supported by the special programs of SARS from the Ministry of Science and Technology of the People's Republic of China and the Research Project of Guangdong Province for SARS Prevention and Treatment.
We thank Rongchang Chen and Yuanda Xu (Guangzhou Institute of Respiratory Diseases, Guangzhou Medical College, Guangzhou, People's Republic of China) and Jin-lin Hou (Department of Infectious Diseases, Nanfang Hospital, Southern Medical University, Guangzhou, People's Republic of China) for providing the clinical data for analysis. We thank San Francisco Edit for their assistance in editing the manuscript.
REFERENCES
- 1.Chan, K. H., L. L. Poon, V. C. Cheng, Y. Guan, I. F. Hung, J. Kong, L. Y. Yam, W. H. Seto, K. Y. Yuen, and J. S. Peiris. 2004. Detection of SARS coronavirus in patients with suspected SARS. Emerg. Infect. Dis. 10:294-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan, P. K. S., K. C. Ng, R. C. W. Chan, R. K. Y. Lam, V. C. Y. Chow, M. Hui, A. Wu, N. Lee, F. H. Y. Yap, F. W. T. Cheng, J. J. Y. Sung, and J. S. Tam. 2004. Immunofluorescence assay for serologic diagnosis of SARS. Emerg. Infect. Dis. 10:530-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Che, X. Y., W. Hao, Y. D. Wang, B. Di, K. Yin, Y. C. Xu, C. G. Feng, Z. Y. Wan, V. C. Cheng, and K. Y. Yuen. 2004. Nucleocapsid protein as early diagnostic marker for SARS. Emerg. Infect. Dis. 10:1947-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Che, X. Y., L. W. Qiu, Y. X. Pan, K. Wen, W. Hao, L. Y. Zhang, Y. D. Wang, Z. Y. Liao, X. Hua, V. C. Cheng, and K. Y. Yuen. 2004. Sensitive and specific monoclonal antibody-based capture enzyme immunoassay for detection of nucleocapsid antigen in sera from patients with severe acute respiratory symdrome. J. Clin. Microbiol. 42:2629-2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Che, X. Y., L. W. Qiu, Y. X. Pan, X. Hua, W. Hao, Z. Y. Liao, Y. B. Mei, L. Y. Zhang, Z. Y. Wan, K. Y. Yuen, and Z. Huang. 2003. Rapid and efficient preparation of monoclonal antibodies against SARS-associated coronavirus nucleocapsid protein by immunizing mice. Di Yi Jun Yi Da Xue Xue Bao 23:640-642. (In Chinese.) [PubMed] [Google Scholar]
- 6.Daginakatte, G. C., C. Chard-Bergstrom, G. A. Andrews, and S. Kapil. 1991. Production, characterization, and uses of monoclonal antibodies against recombinant nucleoprotein of elk coronavirus. Clin. Diagn. Lab. Immunol. 6:341-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ding, Y. Q., L. He, Q. L. Zhang, Z. X. Huang, X. Y. Che, J. L. Hou, H. J. Wang, H. Shen, L. W. Qiu, Z. G. Li, J. Geng, J. J. Cai, H. X. Han, X. Li, W. Kang, D. S. Weng, P. Liang, and S. B. Jiang. 2004. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J. Pathol. 203:622-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang, S. S., T. C. Chen, J. Y. Yang, C. A. Hsiung, I. J. Su, Y. L. Liu, et al. 2004. Sensitive and quantitative detection of severe acute respiratory syndrome coronavirus infection by real-time nested polymerase chain reaction. Clin. Infect. Dis. 38:293-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King, B., and D. A. Brian. 1982. Bovine coronavirus structural proteins. J. Virol. 42:700-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ksiazek, T. G., D. Erdman, C. S. Goldsmith, S. R. Zaki, T. Peret, S. Emery, S. Tong, C. Urbani, J. A. Comer, W. Lim, P. E. Rollin, S. F. Dowell, A. E. Ling, C. D. Humphrey, W. J. Shieh, J. Guarner, C. D. Paddock, P. Rota, B. Fields, J. DeRisi, J. Y. Yang, N. Cox, J. M. Hughes, J. W. LeDuc, W. J. Bellini, L. J. Anderson, et al. 2003. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 348:1953-1966. [DOI] [PubMed] [Google Scholar]
- 11.Leong, H. N., K. W. Chan, A. S. Khan, L. Oon, S. Y. Se-Thoe, X. L. Bai, D. Yeo, Y. S. Leo, B. Ang, T. G. Ksiazek, and A. E. Ling. 2004. Virus-specific RNA and antibody from convalescent-phase SARS patients discharged from hospital. Emerg. Infect. Dis. 10:1745-1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liang, G. D., Q. X. Chen, J. G. Xu, Y. F. Liu, W. L. Lim, J. S. M. Peiris, L. J. Anderson, L. Ruan, H. Li, B. Kan, B. Di, P. Cheng, K. H. Chan, D. D. Erdman, S. Y. Gu, X. G. Yan, W. L. Liang, D. H. Zhou, L. Haynes, S. M. Duan, X. Zhang, H. Zheng, Y. Gao, S. X. Tong, D. X. Li, L. Fang, P. Z. Qin, W. B. Xu, and SARS Diagnosis Working Group. 2004. Laboratory diagnosis of four recent sporadic cases of community-acquired SARS, Guangdong Province, China. Emerg. Infect. Dis. 10:1774-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marra, M. A., S. J. Jones, C. R. Astell, R. A. Holt, A. Brooks-Wilson, Y. S. Butterfield, J. Khattra, J. K. Asano, S. A. Barber, S. Y. Chan, A. Cloutier, S. M. Coughlin, D. Freeman, N. Girn, O. L. Griffith, S. R. Leach, M. Mayo, H. McDonald, S. B. Montgomery, P. K. Pandoh, A. S. Petrescu, A. G. Robertson, J. E. Schein, A. Siddiqui, D. E. Smailus, J. M. Stott, G. S. Yang, F. Plummer, A. Andonov, H. Artsob, N. Bastien, K. Bernard, T. F. Booth, D. Bowness, M. Czub, M. Drebot, L. Fernando, R. Flick, M. Garbutt, M. Gray, A. Grolla, S. Jones, H. Feldmann, A. Meyers, A. Kabani, Y. Li, S. Normand, U. Stroher, G. A. Tipples, S. Tyler, R. Vogrig, D. Ward, B. Watson, R. C. Brunham, M. Krajden, M. Petric, D. M. Skowronski, C. Upton, and R. L. Roper. 2003. The genome sequence of the SARS-associated coronavirus. Science 300:1399-1404. [DOI] [PubMed] [Google Scholar]
- 14.Peiris, J. S. M., C. M. Chu, V. C. C. Cheng, K. S. Chan, I. F. N. Hung, L. L. M. Poon, K. I. Law, B. S. F. Tang, T. Y. W. Hon, C. S. Chan, K. H. Chan, J. S. C. Ng, B. J. Zheng, W. L. Ng, R. W. M. Lai, Y. Guan, K. Y. Yuen, et al. 2003. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia—a prospective study. Lancet 361:1767-1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poon, L. L., K. H. Chan, O. K. Wong, T. K. Cheung, I. Ng, B. Zheng, et al. 2004. Detection of SARS coronavirus in patients with severe acute respiratory syndrome by conventional and real-time quantitative reverse transcription-PCR assays. Clin. Chem. 50:67-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi, Y. L., Y. P. Yi, P. Li, T. Kuang, L. H. Li, M. Dong, Q. J. Ma, and C. Cao. 2003. Diagnosis of severe acute respiratory syndrome (SARS) by detection of SARS coronavirus nucleocapsid antibodies in an antigen-capturing enzyme-linked immunosorbent assay. J. Clin. Microbiol. 41:5781-5782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tony, M., G. A. Farcas, S. M. Poutanen, B. M. Willey, D. E. Low, J. Butany, S. L. Asa, and K. C. Kain. 2004. Severe acute respiratory syndrome-associated coronavirus in lung tissue. Emerg. Infect. Dis. 10:20-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsang, O. T. Y., T. N. Chau, K. W. Choi, E. Y. K. Tso, W. Lim, M. C. Chiu, W. L. Tong, P. O. Lee, B. H. S. Lam, T. K. Ng, J. Y. Lai, W. C. Yu, and S. T. Lai. 2003. Coronavirus-positive nasopharyngeal aspirate as predictor for severe acute respiratory syndrome mortality. Emerg. Infect. Dis. 11:1381-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woo, P. C. Y., S. K. P. Lau, B. H. L. Wong, H. W. Tsoi, A. M. Y. Fung, K. H. Chan, V. K. P. Tam, J. S. M. Peiris, and K. Y. Yuen. 2004. Detection of specific antibodies to severe acute respiratory syndrome (SARS) coronavirus nucleocapsid protein for serodiagnosis of SARS coronavirus pneumonia. J. Clin. Microbiol. 42:2306-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yam, W. C., K. H. Chan, L. L. Poon, Y. Guan, K. Y. Yuen, W. H. Seto, and J. S. M. Peiris. 2003. Evaluation of reverse transcription-PCR assays for rapid diagnosis of severe acute respiratory syndrome associated with a novel coronavirus. J. Clin. Microbiol. 41:4521-4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhai, J. H., T. Briese, E. Dai, X. Y. Wang, X. Pang, Z. G. Du, et al. 2004. Real-time polymerase chain reaction for detecting SARS coronavirus, Beijing, 2003. Emerg. Infect. Dis. 10:300-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng, B. J., Y. Guan, K. H. Wong, J. Zhou, K. L. Wong, B. W. Y. Yong, L. W. Lu, and S. S. Lee. 2004. SARS-related virus predating SARS outbreak, Hong Kong. Emerg. Infect. Dis. 10:176-178. [DOI] [PMC free article] [PubMed] [Google Scholar]