Abstract
Purpose
To determine the effect of multifocal contact lenses on accommodation and phoria in children.
Methods
This was a prospective, non-dispensing, randomized, crossover, single visit study. Myopic children with normal accommodation and binocularity and no history of myopia control treatment were enrolled and fitted with Coopervision Biofinity single vision (SV) and multifocal (MF, +2.50D center distance add) contact lenses. Accommodative responses (photorefraction) and phorias (Modified Thorington) were measured at 4 distances (>3m, 100cm, 40cm, 25cm). Secondary measures included high and low contrast logMAR acuity, accommodative amplitude and facility. Differences between contact lens designs were analyzed using repeated measures regression and paired t-tests.
Results
A total of 16 subjects, aged 10-15 years, completed the study. There was a small decrease in high (SV: -0.08, MF: +0.01) and low illumination (SV:-0.03, MF: +0.08) (both p<0.01) visual acuity, and contrast sensitivity (SV: 2.0, MF: 1.9 log units, p=0.015) with multifocals. Subjects were more exophoric at 40 cm (SV: -0.41, MF: -2.06 Δ) and 25cm (SV: -0.83, MF: -4.30 Δ) (both p<0.01). With multifocals, subjects had decreased accommodative responses at distance (SV: -0.04; MF: -0.37 D, p=0.02), 100 cm (SV: +0.37; MF: -0.35 D, p<0.01), 40 cm (SV: +1.82; MF: +0.62 D, p<0.01), and 25 cm (SV: +3.38; MF: +1.75 D, p<0.01). There were no significant differences in accommodative amplitude (p=0.66) or facility (p=0.54).
Conclusions
Children wearing multifocal contact lenses exhibited reduced accommodative responses and more exophoria at increasingly higher accommodative demands than with single vision contact lenses. This suggests that children may be relaxing their accommodation and using the positive addition or increased depth of focus from added spherical aberration of the multifocals. Further studies are needed to evaluate other lens designs, different amounts of positive addition and aberrations, and long-term adaptation to lenses.
Keywords: myopia control, multifocal soft contact lenses, children, accommodation, phoria
The prevalence of myopia increased from 24% to 34% in children 12-17 years between 1972 and 2008.1 In Taiwan, the prevalence of myopia in children 16-18 years increased from 74% to 84% over less than 20 years.2 While the increase in prevalence of higher myopia (at least -6.00 D) is not as great, the progression in myopia is concerning due to its association with glaucoma,3 retinal detachment,4 choroidal neovascularization,5 and other serious ocular pathologies.6,7
Several promising options to slow down the rate of myopia progression and potentially minimize associated complications include progressive additional spectacle lenses,8 anticholinergic agents,9, 10 and orthokeratology.11 This study focused on the growing popularity of soft multifocal contact lenses. Previous studies have used spherical or aspheric distance-center multifocal lenses, where refractive error is corrected centrally, and positive defocus is presented peripherally.12-14 While multiple studies have demonstrated efficacy in myopia control using multifocal lenses,13-16 only a few studies have evaluated accommodative and binocular outcomes with multifocal contact lenses in non-presbyopic subjects, and with mixed results. One study of young adults (mean age: 22.8 ± 2.5 years) showed that myopes wearing +1.50 D multifocal lenses exhibited leads of accommodation,17 while another study on adults (age 25 to 35 years) showed no statistically significant differences in accommodative response between single vision and multifocal contact lenses.18 In a recent study, Kang et al found accommodative lags of 0.63 D, 1.12 D and 0.82 D for a target at 33 cm with single vision distance, +1.50 D, and +3.00 D multifocal contact lenses, respectively, in a cohort of 18 to 28 year olds.19 To our knowledge, there has been only one study that examined accommodative response through multifocal lenses in a pediatric population (age 11 to 14).14 In that study, the authors suggested that children accommodated normally through the multifocal using the distance portion of the correction. However, accommodation was measured with one eye wearing a multifocal and one wearing a single vision contact lens, so it is unclear which eye/lens combination was used by the child to focus on the target.14 A recent publication by Aller et al reported that children (age 8 to 18 years) fitted with Acuvue Bifocal contact lenses were more exophoric than those wearing single vision Acuvue 2 lenses.16 This study selected an add power to neutralize the subject's near phoria but did not report the average or range of add powers of the multifocal contact lenses.
Since myopia control lenses are intended to be worn by children, who have very different accommodative and binocular systems than adults,20, 21 it is critical to understand if accommodation and binocular function is affected by multifocal contact lenses in children. The aim of the current study was to examine the effect of a commercial distance-center multifocal contact lens designed for presbyopia on accommodation, heterophoria, and other visual functions in a pediatric, myopic population.
Methods
Subjects
This prospective, randomized, single-visit, cross-over study was conducted in pediatric subjects at the State University of New York College of Optometry. The study was approved by the local Institutional Review Board, registered on ClinicalTrials.gov (NCT #02180347), and adhered to the tenets established by the Declaration of Helsinki. All subjects and their parents/guardians gave their written assent and consent to participate in the study.
Patients were recruited from the University Eye Center at the State University of New York College of Optometry. Inclusion criteria were age between 7 and 15 years, best corrected visual acuity of 20/25 or better, refractive error between -1.00 and -8.00 D with less than or equal to 1.00 D of astigmatism, and no history of any ocular condition, binocular vision disorder, prior participation in myopia control, or use of any pharmaceutical agent that is known to affect accommodation. Medical records were reviewed to ensure eligibility. Subjects did not need to have previous experience with contact lens wear.
Study Design
Baseline Testing
Snellen visual acuity, non-cycloplegic autorefraction, and slit lamp examination were performed to verify eligibility. Autorefraction was taken as the average spherical equivalent of three measurements with the Grand Seiko WAM-5500 Binocular Autorefractor (Grand Seiko Ltd., Hiroshima, Japan).
Contact Lenses & Fitting
The study used Biofinity brand sphere and distance-center design multifocal contact lenses with an add power of +2.50 D (comfilcon A, 48% water content, CooperVision; USA). This add power was chosen based on previous research indicating that +2.00 to +2.50 was the maximum visually acceptable add power for children.22 Both lenses have a base curve of 8.6 mm and a diameter of 14.0 mm. The multifocal lenses are designed with a central distance zone of 3 mm, with a gradually increasing positive power towards the periphery of the optic zone.
Subjects underwent testing with both types of contact lenses, but were randomized to begin with either the spherical single vision distance contact lens, or multifocal contact lens. Contact lenses were worn binocularly throughout all tests except for photorefraction in the multifocal contact lens condition. Under the multifocal condition during photorefraction, the multifocal contact lens on the right eye was switched to a single vision contact lens to allow accurate measurement of accommodative response (see details below). The distance prescription for both lenses was selected as the average spherical equivalent measure obtained from auto-refraction. The contact lenses were allowed to settle for ten minutes before evaluation of fit. During this time, the lighting was dimmed in the examination room and subjects were instructed to refrain from near work. Acceptable contact lens fit was evaluated based on adequate coverage, centration, and movement on the eye. Inadequate corneal coverage, decentration of more than 1 mm, or movement on blink greater than 1 mm would have disqualified the subject from the study. After adequate fitting was determined, a series of visual functions testing was conducted.
Outcome Measures
Accommodation
Accommodative responses were measured monocularly through the right eye using a custom built infrared (IR) photorefractor (Camera DMK 22 AUC03 and Cosmica Pentax 50 mm lens, Tubingen, Germany) based on the design of the PowerRefractor used in several studies of human refractive state and accommodation.23-27 The photorefractor was positioned 100 cm from the subject and recorded measurements at a sampling rate of 76 Hz. Room illumination was adjusted to ensure pupil size was at least 4 mm at all times. The system was calibrated for each subject's right eye while wearing the single vision distance contact lens. The system gain was determined using ± 3 D lenses to alter the subject's refraction by a fixed amount and any offset in the infrared reading during calibration was corrected to zero as each subject was distance corrected. Subjects viewed the target through the left eye, which wore either the single vision or the multifocal correction. Consensual accommodative response, refractive state in the vertical meridian, and pupil diameter were measured in the subjects' right eye, which was corrected for the distance with a single vision contact lens and occluded by an infrared filter. Accommodative responses were measured at four stimulus distances: distance (>3 m), 100 cm, 40 cm, and 25 cm, giving accommodative demands at 0 D, 1 D, 2.5 D and 4 D, respectively. The near targets consisted of three lines of words in which the letter height of each line subtended 0.31°, 0.36° (roughly a 20/50 letter at 40 cm), and 0.41° of visual angle at each target distance so that the letter sizes were maintained to give the same visual angle at all distances. Subjects were instructed to keep the center word clear at each target distance for 10-15 seconds and close their eyes for 10 seconds between each target. Photorefraction data were collected continuously over the time period at which the subjects viewed the target. The data were filtered offline to remove artifacts created by off-axis fixation, blinks, or glare from the infrared filter using KaleidaGraph (Synergy Software, Reading, PA) and then averaged. This process was repeated at each test distance three times and averaged to provide the final measurement.
Binocular push-up accommodation was measured using a Royal Air Force near point rule (Haag-Streit England, Essex, United Kingdom). The target was the same as the 40 cm target used for the photorefraction. The subject was instructed to keep the center word clear and report first blur. Three measurements were taken to the nearest half-centimeter, averaged, and converted to diopters.
Binocular accommodative facility was tested with +2.00/-2.00 D flippers to assess the dynamics and stamina of the accommodative system. The test was administered at 40 cm and measured in cycles per minute (cpm), using the same target as was used for photorefraction at 40 cm.
Lateral Phoria
Phoria was measured using the Modified Thorington method at four distances: distance (3 m), 100 cm, 40 cm, and 25 cm (Bernell Muscle Imbalance Card, Bernell Corp, South Bend, IN). The modified Thorington card calibrated for 40 cm was used to measure phoria at 100 cm. 40 cm, and 25 cm. A conversion factor using the definition of a prism diopter was used to adjust for the different test distances to calculate the subjects' true phorias at 100 cm and 25 cm.28
High and Low Illumination Visual Acuity
High and low illumination visual acuities were measured binocularly with an electronic logMAR chart using an iPad with Retina display (Apple Inc., Cupertino, CA) at a viewing distance of 3 m (Ridgevue Vision, Denver, CO) using a screen luminance of 150 cd/m2. Low illumination logMAR acuity was measured with the subjects holding 2.0 neutral density filters over their eyes, to counter the backlight illumination from the screen and to reduce luminance by a factor of 100 to approximately 1.5 cd/m2.
Contrast Sensitivity
Contrast sensitivity was measured binocularly at 10 cycles per degree with the validated Ridgevue Contrast Sensitivity Test run on an iPad with Retina display. The scoring system of the Ridgevue Contrast Sensitivity test is based on the scoring system of the Pelli-Robson Chart and has been shown to have good repeatability and similar results as the Freiburg acuity and contrast test.29 Following instrument protocol, a test distance of 1 m was used.
Data Analysis
Descriptive statistics were calculated for demographic and baseline data. Repeated measures analysis of variance (ANOVA) was used to assess changes in accommodative response and phoria by test distance and lens type. Post-hoc testing with Bonferroni corrections for multiple comparisons were done, as appropriate. Paired t-tests were used to compare differences between multifocal and single vision lens conditions in high and low illumination logMAR acuity, contrast sensitivity, amplitude of accommodation, and accommodative facility. A p-value of <0.05 was considered to be statistically significant. All statistical analyses were conducted using SPSS version 19 (SPSS, Chicago, IL).
Results
Seventeen subjects were enrolled in the study, but one subject did not complete the study due to failure to be able to insert contact lenses. No subjects were disqualified from inadequate fitting of contact lenses. Eleven subjects (69%) were female and the average age was 13.3 ± 1.7 years (mean ± standard deviation; range: 10 to 15 years). The demographic distribution was black, 41%; white, 23.5%; Asian, 12%; other, 23.5%. The mean spherical equivalent refractive error by non-cycloplegic autorefraction was -2.42 ± 0.83 D in the right eye and -2.44 ± 0.73 D in the left eye (range for all eyes: -1.75 to -4.00 D). The pupil size while subjects viewed the distance target under room illumination (6.5 to 7.5 lux) was 6.6 ± 0.31 mm.
Accommodation
Photorefractor data were only available for 15 of the 16 subjects because we did not obtain sufficient data for one subject. Individual accommodative responses for all subjects are shown in the single vision and multifocal contact lens conditions (Figure 1a). The gains of the accommodative stimulus-response functions were estimated by the slopes of linear regressions fit to each individual's data. The slope of the stimulus response function flattened under multifocal compared to single vision condition (multifocal: 0.55 ± 0.20, single vision: 0.82 ± 0.17, p < 0.01). The inset figure shows the relative accommodative gain with multifocal compared to single vision contact lens wear (Figure 1A). The gains were reduced for all eyes wearing the multifocal compared to the single vision contact lens. As expected, the mean accommodative response decreased with increasing target demand (Figure 1B). Post-hoc testing showed reduced refractive states with multifocal contact lenses at distance (single vision: -0.04 ± 0.43 D; multifocal: -0.37 ± 0.72 D, p = 0.02), 100 cm (single vision: +0.37 ± 0.44 D; multifocal: -0.35 ± 0.70 D, p < 0.01), 40 cm (single vision: +1.82 ± 0.53 D; multifocal: +0.62 ± 0.63 D, p < 0.01), and 25 cm (single vision: +3.38 ± 0.52 D; multifocal: +1.75 ± 0.62 D, p < 0.01) (Figure 1B).
Figure 1.
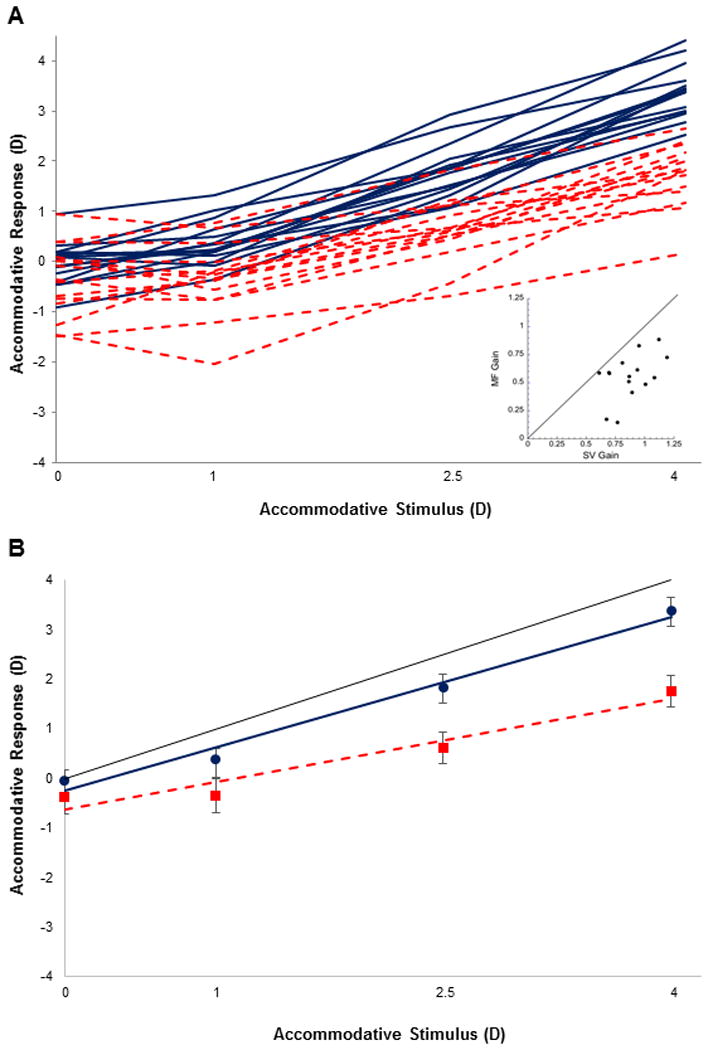
(A) Accommodative responses for subjects wearing single vision (blue solid) and multifocal (red dashed) contact lenses. Inset shows the gain of the accommodative stimulus response function for each subject while wearing either single vision or multifocal contact lenses (n=15). (B) Mean (± standard deviation) accommodative response at each stimulus demand and mean accommodative stimulus response function for single vision (blue) and multifocal (red) contact lens conditions. The black solid line shows the 1:1 line.
Binocular push-up amplitude of accommodation was normal for the subject age.30 There was no significant difference in binocular accommodative amplitude (single vision: 13.1 ± 2.2 D; multifocal: 13.2 ± 2.5 D, p = 0.66) or accommodative facility (single vision: 8.9 ± 3.7 cpm; multifocal: 8.6 ± 2.7 cpm, p = 0.54).
Phoria
As expected, most subjects exhibited more exophoria with greater near demands. Mean phorias were significantly more exophoric with multifocal contact lenses at 40 cm (single vision: -0.41 ± 2.91 Δ; multifocal: -2.06 ± 2.49 Δ, p < 0.01), and 25 cm (single vision: -0.83 ± 3.23 Δ; multifocal: -4.30 ± 4.32 Δ, p < 0.01) (Figure 2B). Phorias were not significantly different at distance (p = 0.19) or 100 cm (p = 0.06).
Figure 2.
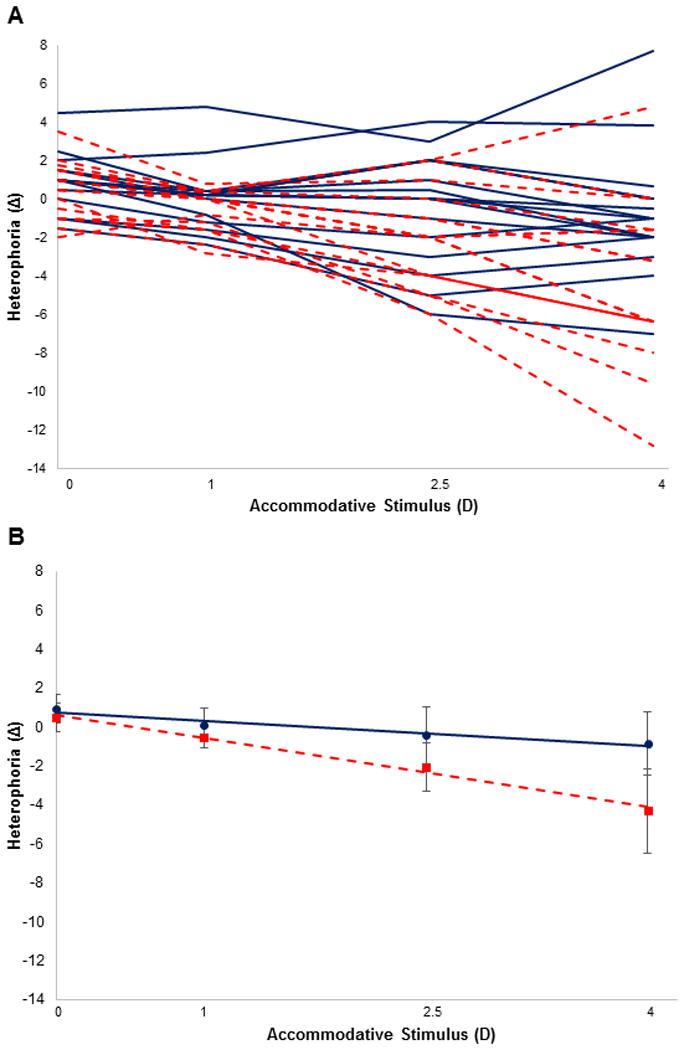
(A) Lateral phoria for subjects wearing single vision (blue solid) and multifocal (red dashed) contact lenses (n=16). (B) Mean (± standard deviation) phoria at each stimulus demand with single vision (blue) and multifocal (red) contact lens conditions. Esophoria indicated as positive and exophoria as negative.
Visual Acuity and Contrast Sensitivity
Visual acuity measured under high and low illumination is shown in Figure 3. Multifocal lenses reduced visual acuity under both high (single vision: -0.08 ± 0.08, multifocal: +0.01 ± 0.09, p < 0.01) and low illumination (single vision: -0.03 ± 0.08, multifocal: +0.08 ± 0.09, p < 0.01) compared to single vision lenses. Quantitatively, this shows that subjects lost about a line (4-5 letters) of acuity under high or low illumination, but average acuity was always better than about 20/25 Snellen equivalent. Across the same type of contact lens, visual acuity decreased under low illumination (single vision: p < 0.01, multifocal: p < 0.01).
Figure 3.
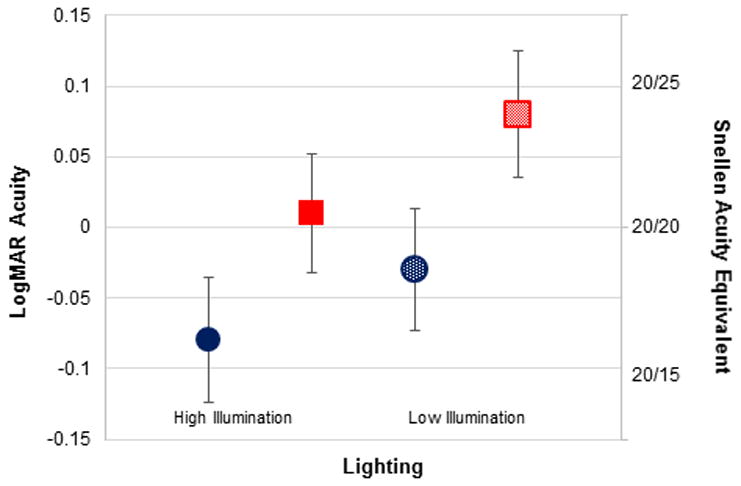
Mean and standard deviation LogMAR visual acuity and Snellen equivalent measured under high (solid fill) and low (pattern fill) illumination with single vision (blue circles) and multifocal (red squares) contact lenses.
A statistically significant, but clinically small, difference in contrast sensitivity between multifocal and single vision was found. Mean contrast sensitivity decreased from 2.0 ± 0.1 log units with single vision lenses to 1.9 ± 0.1 log units with multifocal contact lenses (p = 0.015).
Discussion
The purpose of this study was to evaluate the effect of multifocal contact lenses on accommodation, phoria, and visual function in a normal population of myopic children. The results of this study showed that the multifocal contact lenses used in this study alter binocular posture and some aspects of accommodation when compared to single vision contact lenses. Specifically, when viewing through the multifocal lenses accommodative response was reduced, the eyes were more exophoric, and visual acuity was reduced.
As seen in other studies of presbyopia31 and myopia control32 contact lenses, both visual acuity and contrast sensitivity were slightly degraded with the multifocal contact lenses used in this study. Decreased visual acuity and contrast sensitivity were also consistent with previous findings on young adults wearing multifocal lenses.19, 22 Our findings and those of others,22 showed that contrast sensitivity is reduced in children wearing multifocal contact lenses compared to single vision lenses. However, these results are generally limited to a few spatial frequencies and further research is needed to understand the effect of multifocal contact lenses across all spatial frequencies in children.
A recent study of adults by Kang et al. 19 also reported increased accommodative lag of 1.12 D and 0.82 D at near (33 cm) with multifocal contact lenses (+1.50 and +3.00 D Proclear multifocal, respectively) compared to 0.63 D of lag with single vision (Proclear sphere). The present study found similar but slightly larger lags of accommodation in children wearing +2.50 D Biofinity multifocal lenses. Two possible reasons may explain the decrease in accommodative response with multifocals. Non-presbyopic wearers may be utilizing the positive addition of the lens to relax their accommodation, and the positive spherical aberration induced by the aspheric design of the multifocals may increase their depth of focus. Children typically exhibit little to no spherical aberration (+0.018 μm),33 compared to the average adult who has about +0.18 μm for a 6 mm pupil.34 Multifocal lenses induce additional spherical aberration of up to about +0.20 μm.35-37 Specifically, the distance-center +2.00 D Proclear multifocal lenses (similar in design to Biofinity) induced an average of +0.11 μm of spherical aberration.35 Adaptive optics simulations in adults demonstrated that the depth of focus reached a maximum at about 2 D with about 0.6 μm of spherical aberration.38 The combination of ocular and multifocal contact lens induced spherical aberration creates an enlarged depth of focus. This effect would be expected to be less in children than adults based on spherical aberration population averages. Nevertheless, a larger range of clear vision would lessen the need to accommodate for any non-presbyopic wearer.
Children seemed to relax accommodation through the multifocal at distance (-0.37 D), which was not found with single vision contact lenses (-0.04 D, Figure 1b). This discrepancy is likely explained by the power profile of the Biofinity multifocal. For a plano labeled multifocal lens, the central 3 mm zone shows a positive power of +0.67 D.39 Due to the fact that the non-cyclopleged spherical equivalent refractive error from auto-refraction was used to select the distance power, it is possible that children may have been slightly over-corrected in both lenses. This is also supported by the three subjects who had gains larger than 1.0 (Figure 1a). Children may have accommodated though the single vision contact lenses to keep the target clear but, due to the inherent distortion of aspheric multifocal contact lenses, they may have more readily relaxed their accommodation with multifocals. While performing a cycloplegic refraction may have provided some additional insight into refractive state in the distance, any difference in refractive error following cycloplegia would likely be small and clinically insignificant in this myopic population with normal binocularity and accommodation.
Pupil size has an effect on higher order aberrations of the eye and the amount of plus power and aberrations experienced from multifocal contact lenses.39 One of the limitations of photorefraction, is that it measures over the entire pupil and does not allow analysis of higher order aberrations at various pupil diameters as can be achieved with aberrometry. While we are unable to quantify the changes in higher order aberrations in this study, the power profile of the Biofinity +2.50 D lens, suggests that the children would be experiencing the majority of the plus power and asphericity (spherical aberration) in the lens with pupil sizes as small as about 4 mm.39
Accommodative amplitude and facility were taken binocularly to assess “real-world” testing conditions. Accommodative facility through single vision and multifocal contact lenses for our subjects (8 cpm) was found to be higher than the expected norms (5 cpm) in 8 to 12 year old children.21 The higher values found in our study may be due to using a 20/50 Snellen acuity target, larger than the traditional 20/30 target used to measure accommodative facility in adults or that we did not require the subjects to read the words aloud.21 A suppression check was not utilized and may also be a potential explanation for the above average performance on this test. Our accommodative amplitude results were consistent with previous studies in normal children.30 While the binocular push-up amplitude of accommodation was greater in children wearing multifocal contact lenses, the difference between amplitudes in multifocal and single vision lenses was not statistically significant, likely due to the poor repeatability of this measurement and the subjective nature of these tests where children have to appreciate and respond quickly to clinical endpoints.40
The modified Thorington card provides a quick and simple method of measuring horizontal phoria that has shown to be repeatable within and across examiners.28 The distance and near lateral phoria with single vision contact lenses showed good agreement with previous studies in children.41 Because the modified Thorington method is performed in free space and provides peripheral cues to accommodation, it is possible that more esophoric posture may be measured compared to an in-instrument method such as Von Graefe.42 While normative data for adults typically show range between orthophoria and 6 PD exophoria at near, Jimenez et al found in 1,016 pediatric subjects that children showed exophoria of about 0.4 ± 3.1 PD at near, consistent with what we found in our study.41 The increase in exophoria induced by multifocal contact lenses at near is in agreement with previous studies and supports the hypothesis that the children are utilizing the positive addition or increased depth of focus provided by the multifocal design to relax their accommodation.16, 19
Myopia control using multifocal contact lenses is becoming an acceptable option for reducing myopia progression and more clinical trials are underway.12-14 This study demonstrated that children wearing multifocals exhibited decreased accommodative response and more exophoria than when wearing single vision contact lenses. They also experienced a slight reduction in visual acuity, particularly under low lighting and contrast. When fitting children in multifocal contact lenses, it is important to consider these expected changes in order to properly evaluate and manage patients. For example, children with high exophoria or who experience double vision at near with multifocal contact lenses may have their myopia better managed with other forms of myopia control such as orthokeratology or atropine. Our findings of reduced accommodative stimulus-response slopes and greater exophoria at near are consistent with the notion that children are using the positive addition at near. This potentially reduces the therapeutic effect of myopia control during near viewing. We speculate that the benefit of the near addition may be achieved mainly when viewing at distance.
Kang et al.19 measured accommodation and visual function in young adults wearing +1.50 D and +3.00 D distance-center multifocal lenses over a two week period and found no statistically significant difference in accommodative response and phoria between the first visit and after two weeks of daily contact lens wear. Further studies are needed to evaluate long-term adaptation to multifocal contact lenses, other multifocal lens designs, and different amounts of positive addition and spherical aberration in children. These findings also suggest that multifocal contact lenses may be useful for children with accommodative insufficiency or vergence disorders and further research in this area is also warranted.
Acknowledgments
This study was partially supported by an NIH/NEI T35 grant (EY020481). We would like to acknowledge Dr. Frank Schaeffel for providing the photorefractor system. We also like to thank Dr. Alexandra Benavente-Perez, Dr. Mark Bullimore, Ann Nour, Christine Yoo, Kim Duong and Jinyoung Choe for their support of this project. Results of the study have been previously reported as an abstract at the American Academy of Optometry meeting in New Orleans, LA, October 7, 2015.
References
- 1.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632–9. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 2.Lin LL, Shih YF, Hsiao CK, et al. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 2004;33:27–33. [PubMed] [Google Scholar]
- 3.Mitchell P, Hourihan F, Sandb, et al. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106:2010–5. doi: 10.1016/s0161-6420(99)90416-5. [DOI] [PubMed] [Google Scholar]
- 4.Saw SM, Gazzard G, Shih-Yen EC, et al. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381–91. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida T, Ohno-Matsui K, Yasuzumi K, et al. Myopic choroidal neovascularization: a 10-year follow-up. Ophthalmology. 2003;110:1297–305. doi: 10.1016/S0161-6420(03)00461-5. [DOI] [PubMed] [Google Scholar]
- 6.Celorio JM, Pruett RC. Prevalence of lattice degeneration and its relation to axial length in severe myopia. Am J Ophthalmol. 1991;111:20–3. doi: 10.1016/s0002-9394(14)76891-6. [DOI] [PubMed] [Google Scholar]
- 7.Wang NK, Chen YP, Lai CC, et al. Paediatric retinal detachment: comparison of high myopia and extreme myopia. Br J Ophthalmol. 2009;93:650–5. doi: 10.1136/bjo.2008.145920. [DOI] [PubMed] [Google Scholar]
- 8.Hyman L, Gwiazda J, Marsh-Tootle WL, et al. The Correction of Myopia Evaluation Trial (COMET): design and general baseline characteristics. Control Clin Trials. 2001;22:573–92. doi: 10.1016/s0197-2456(01)00156-8. [DOI] [PubMed] [Google Scholar]
- 9.Song YY, Wang H, Wang BS, et al. Atropine in ameliorating the progression of myopia in children with mild to moderate myopia: a meta-analysis of controlled clinical trials. J Ocul Pharmacol Ther. 2011;27:361–8. doi: 10.1089/jop.2011.0017. [DOI] [PubMed] [Google Scholar]
- 10.Siatkowski RM, Cotter SA, Crockett RS, et al. Two-year multicenter, randomized, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. J J AAPOS. 2008;12:332–9. doi: 10.1016/j.jaapos.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 11.Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–85. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 12.Lam CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98:40–5. doi: 10.1136/bjophthalmol-2013-303914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207–14. doi: 10.1097/OPX.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 14.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152–61. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 15.Sankaridurg P, Holden B, Smith E, 3rd, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52:9362–7. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 16.Aller TA, Liu M, Wildsoet CF. Myopia control with bifocal contact lenses: a randomized clinical trial. Optom Vis Sci. 2016;93:344–52. doi: 10.1097/OPX.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 17.Tarrant J, Severson H, Wildsoet CF. Accommodation in emmetropic and myopic young adults wearing bifocal soft contact lenses. Ophthalmic Physiol Opt. 2008;28:62–72. doi: 10.1111/j.1475-1313.2007.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madrid-Costa D, Ruiz-Alcocer J, Radhakrishnan H, et al. Changes in accommodative responses with multifocal contact lenses: a pilot study. Optom Vis Sci. 2011;88:1309–16. doi: 10.1097/OPX.0b013e31822be35a. [DOI] [PubMed] [Google Scholar]
- 19.Kang P, Wildsoet CF. Acute and short-term changes in visual function with multifocal soft contact lens wear in young adults. Cont Lens Anterior Eye. 2016;39:133–40. doi: 10.1016/j.clae.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Jimenez JR, Durban JJ, Anera RG. Maximum disparity with acuvue bifocal contact lenses with changes in illumination. Optom Vis Sci. 2002;79:170–4. doi: 10.1097/00006324-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Scheiman M, Wick B. Clinical Management of Binocular Vision: Heterophoric, Accommodative, and Eye Movement Disorders. 3. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 22.Bickle KM. Master's thesis. Columbus, OH: The Ohio State University; 2013. Bifocal lenses in nearsighted kids (BLINK) Study. [Google Scholar]
- 23.Choi M, Weiss S, Schaeffel F, et al. Laboratory, clinical, and kindergarten test of a new eccentric infrared photorefractor (PowerRefractor) Optom Vis Sci. 2000;77:537–48. doi: 10.1097/00006324-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Allen PM, Radhakrishnan H, O'Leary DJ. Repeatability and validity of the PowerRefractor and the Nidek AR600-A in an adult population with healthy eyes. Optom Vis Sci. 2003;80:245–51. doi: 10.1097/00006324-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Hunt OA, Wolffsohn JS, Gilmartin B. Evaluation of the measurement of refractive error by the PowerRefractor: a remote, continuous and binocular measurement system of oculomotor function. Br J Ophthalmol. 2003;87:1504–8. doi: 10.1136/bjo.87.12.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harb E, Thorn F, Troilo D. Characteristics of accommodative behavior during sustained reading in emmetropes and myopes. Vision Res. 2006;46:2581–92. doi: 10.1016/j.visres.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schaeffel F, Mathis U, Bruggemann G. Noncycloplegic photorefractive screening in pre-school children with the “PowerRefractor” in a pediatric practice. Optom Vis Sci. 2007;84:630–9. doi: 10.1097/OPX.0b013e3180dc99ea. [DOI] [PubMed] [Google Scholar]
- 28.Cebrian JL, Antona B, Barrio A, et al. Repeatability of the modified Thorington card used to measure far heterophoria. Optom Vis Sci. 2014;91:786–92. doi: 10.1097/OPX.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 29.Kollbaum PS, Jansen ME, Kollbaum EJ, et al. Validation of an iPad test of letter contrast sensitivity. Optom Vis Sci. 2014;91:291–6. doi: 10.1097/OPX.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 30.Larsson E, Holmstrom G, Rydberg A. Ophthalmological findings in 10-year-old full-term children--a population-based study. Acta Ophthalmol. 2015;93:192–8. doi: 10.1111/aos.12476. [DOI] [PubMed] [Google Scholar]
- 31.Madrid-Costa D, Garcia-Lazaro S, Albarran-Diego C, et al. Visual performance of two simultaneous vision multifocal contact lenses. Ophthalmic Physiol Opt. 2013;33:51–6. doi: 10.1111/opo.12008. [DOI] [PubMed] [Google Scholar]
- 32.Kollbaum PS, Jansen ME, Tan J, et al. Vision performance with a contact lens designed to slow myopia progression. Optom Vis Sci. 2013;90:205–14. doi: 10.1097/OPX.0b013e3182812205. [DOI] [PubMed] [Google Scholar]
- 33.Papamastorakis G, Panagopoulou S, Tsilimbaris MK, et al. Ocular higher-order aberrations in a school children population. J Optom. 2015;8:93–100. doi: 10.1016/j.optom.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kingston AC, Cox IG. Population spherical aberration: associations with ametropia, age, corneal curvature, and image quality. Clin Ophthalmol. 2013;7:933–8. doi: 10.2147/OPTH.S44056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Legras R, Benard Y, Rouger H. Through-focus visual performance measurements and predictions with multifocal contact lenses. Vision Res. 2010;50:1185–93. doi: 10.1016/j.visres.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 36.Bakaraju RC, Ehrmann K, Ho A, Papas E. Inherent ocular spherical aberration and multifocal contact lens optical performance. Optom Vis Sci. 2010;87:1009–22. doi: 10.1097/OPX.0b013e3181fbad60. [DOI] [PubMed] [Google Scholar]
- 37.Gifford P, Cannon T, Lee C, et al. Ocular aberrations and visual function with multifocal versus single vision soft contact lenses. Cont Lens Anterior Eye. 2013;36:66–73. doi: 10.1016/j.clae.2012.10.078. [DOI] [PubMed] [Google Scholar]
- 38.Rocha KM, Vabre L, Chateau N, et al. Expanding depth of focus by modifying higher-order aberrations induced by an adaptive optics visual simulator. J Cataract Refract Surg. 2009;35:1885–92. doi: 10.1016/j.jcrs.2009.05.059. [DOI] [PubMed] [Google Scholar]
- 39.Plainis S, Atchison DA, Charman WN. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013;90:1066–77. doi: 10.1097/OPX.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 40.Anderson HA, Hentz G, Glasser A, et al. Minus-lens-stimulated accommodative amplitude decreases sigmoidally with age: a study of objectively measured accommodative amplitudes from age 3. Invest Ophthalmol Vis Sci. 2008;49:2919–26. doi: 10.1167/iovs.07-1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jimenez R, Perez MA, Garcia JA, et al. Statistical normal values of visual parameters that characterize binocular function in children. Ophthalmic Physiol Opt. 2004;24:528–42. doi: 10.1111/j.1475-1313.2004.00234.x. [DOI] [PubMed] [Google Scholar]
- 42.Maples WC, Savoy RS, Harville BJ, et al. Comparison of distance and near heterophoria by two clinical methods. Optom Vis Devel. 2009;40:100–6. [Google Scholar]


