Abstract
Introduction:
Obesity is one of the greatest health problems in the world. The World Health Organization (WHO) defined obesity as a disease in which the excess of adipose tissue accumulates in such a degree that is endangers health. Obesity is a very complex multifactor disease that is developed under the influence of genetic and metabolic factors, environment, social and cultural environment as well as bad habits. The causes of obesity can be numerous. The most common source of obesity is the development of energetic imbalance.
Material and methods:
A retrospective study of medical records in the Department of Obstetrics and Gynecology, University Clinical Hospital in Mostar was conducted. It included 1300 pregnant women and their children that were delivered in the time period from January 1st 2015 to December 31st 2015. It was conducted a retrospective study which involved 1300 pregnant women who gave births in the Department of Obstetrics and Gynecology of University Clinical Hospital in Mostar in the period from January 1st 2015 to December 31st 2015 and their newborns.
Results:
The difference in age of pregnant women with different body mass index was not statistically relevant. The average age of pregnant women with normal body mass was 29.52 ± 5.48, overweight pregnant women 30.30 ± 5.138, and obese pregnant women 30.00 ± 5.103 (F = 2.730; p = 0.066). The youngest was 24, and the oldest was 49 years old. The average gestational age at delivery was 39.23 ± 1.556 (min 28; max. 42 weeks of gestation). The majority of pregnant women; 660 of them (50.8 %), were overweight in the early stages of their pregnancy, there were 322 (24.8 %) obese women, and there were 318 (24.5 %) normal weight women.
At the end of the pregnancy, the highest number was that of obese pregnant women 925 (71.2 %), while 328 (25.2 %) pregnant women were overweight, and only 47 (3.6 %) pregnant women had normal weight.
Conclusion:
Nutritive status and weight gain of a mother during pregnancy are an important indication of her health and of the foetus growth. Overweightness and obesity of a mother before pregnancy and during pregnancy has a negative influence on the health of the mother and infant. Moreover, it is linked with risk and a negative pregnancy outcome. BMI was associated with an increased risk of adverse perinatal outcome.
Keywords: obesity, pregnant woman, body mass index
1. INTRODUCTION
Obesity is one of the greatest health problems in the world. The World Health Organization (WHO) defined obesity as a disease in which the excess of adipose tissue accumulates in such a degree that is endangers health (1). Obesity is a very complex multifactor disease that is developed under the influence of genetic and metabolic factors, environment, social and cultural environment as well as bad habits. The causes of obesity can be numerous. The most common source of obesity is the development of energetic imbalance. When there is an increased intake of high calorie food rich in fat and refined sugar combined with low physical activity, that extra energy is stored in the body in the form of fat. Moreover, research shows a significant genetic factor in the development of obesity (2). Resistance to leptin is also considered to be one of the causes of obesity. Leptin is a hormone that is mostly produced by adipose tissue. Leptin acts as a signal molecule and by biding itself to its receptors in hypothalamus it maintains a homeostasis of an organism. With a range of regulative mechanism it leads to a lower storage and better usage of fat. In states of reduction of energy supplies and starvation, leptin levels in blood get lower. It is believed that in obese people a resistance to leptin was developed because their levels of leptin are high (3). Obesity has become one of the leading threats to health in the world. The prevalence of obesity is increasing on almost all of the continents and in all of the developed countries (4). The prevalence of obesity in the United Kingdom was 20 %, which places it behind United States where the prevalence of obesity is 34%. Despite the alarming results, the prevalence of obesity shows growth tendency in both countries. According to some prognosis, without a systematic intervention and with the current growth rate, the prevalence of obesity will grow up to 50% in adult population until year 2050 therefore causing great expenses to health system (5). To diagnose obesity certain anthropogenic measurements are used, more specifically, measurement of body mass index (BMI), waist line, waist and hips ratio and skinfold measurement (6). Body mass index (BMI) is an internationally accepted index to define obesity. Body mass index (BMI) is a simple index of weight-for-height that is commonly used to classify overweight and obesity in adults. It is defined as a person’s weight in kilograms divided by the square of his height in meters (kg/m2). It is a simple, safe, non-invasive and cheap way of estimating body mass and health (7). The American Institute of Medicine defined normal body weight as BMI 18.5-24.9 kg/m2, overweight as BMI 25- 29.9 kg/m2 and obese as BMI of 30 kg/m2 and more (8). The fertility of obese and overweight woman is significantly reduced in comparison to women with normal body weight. Mother’s overweightness before pregnancy has a negative effect on the health of the mother and the newborn. Pregnant women with BMI over 24.9 kg/m2 have a higher risk of complications during pregnancy, such as gestational diabetes mellitus (GDM), hypertension, preeclampsia and caesarian section. The fetuses of pregnant women with BMI higher than 24.9 kg/m2 have a higher risk of premature birth, congenital anomalities, fetal macrosomia with possible injuries during birth and overweightness. Higher body mass and high BMI in the first trimester and a higher increase in body weight during pregnancy, as well as increased concentration of insulin, glucose, triglyceride, cholesterol and leptin in the serum of mothers significantly influence the body weight of infants. Women with BMI<25 kg/m2 in the first trimester give birth to children with a lower birth mass that those women with BMI≥ 25 kg/m2, women with a lower increase of body weight during pregnancy give birth to children with lower birth weight than those women with a higher increase. Women with BMI≥ 25 kg/m2 and higher give birth to largest children, while women with BMI< 19 kg/m2 give birth to smaller children than women with normal weight. Overweight women with BMI> 30 kg/m2 have the lowest weight increase (9-19).
2. AIM
The goal of this study was investigated the associations between pre-pregnant body mass index (BMI1) and gestational weight gain (GWG) with term perinatal outcomes of mothers and their newborns.
3. MATERIAL AND METHODS
A retrospective study of medical records in the Department of Obstetrics and Gynecology, University Clinical Hospital in Mostar was conducted. It included 1300 pregnant women and their children that were delivered in the time period from January 1st 2015 to December 31st 2015.
Parameters for the inclusion of pregnant woman in the study were: body mass index in the early (BMI 1) and in the end stages of the pregnancy (BMI 2), weight gain, parity, age, method of delivery (spontaneous delivery, cesarean section, vacuum extraction), gestational age, complications during pregnancy (gestational diabetes mellitus - GDM, pregnancy induced hypertension- HTA, preeclamsia, bleeding). Parameters for inclusion of newborn infants were: birth weight, gender, vitality (Apgar score), complications (birth trauma, intrauterine growth restricrition–IUGR, asphyxia, perinatal infections). The criteria to exclude pregnant women from the study were: pregnant women with incomplete documentation, those who were diagnosed with diabetes prior to pregnancy, women with multiple pregnancies, women who gave birth to newborns with congenital malformations, mors fetus in utero, stillborns.
BMI of pregnant women was measured at the beginning and at the end of the pregnancy. In addition, the weight gain during pregnancy was measured. BMI was put into categories: 1. lower body mass (<18.5 kg/m2), 2. normal body weight (18.5–24.9 kg/m2), 3. overweight (25–29.9 kg/m2) and 4. obese (≥30 kg/m2). Weight gain was marked as: 1. small (< 8 kg), 2. normal (8-16 kg) and 3. excessive (>16 kg).
Depending on the body mass index, pregnant women were divided into three groups: 1. those who had a regular body mass index, 2. overweight and 3. obese. Risk factors were observed during the pregnancy, delivery and in early neonatal period. BMI was calculated as a ratio of body mass in kilograms and square meters of height in meters. Height and weight were measured by Seca mechanical scale with a hight scale.
Data was collected in MS Excel (version Microsoft Excel 11, Microsoft Corporation, Redmond, WA, USA). To conduct a statistic analysis of obtained data a software system was used (version 17.0, SPSS Inc., Chicago, Illinois, USA) SPSS for Windows (version 17.0, SPSS Inc., Chicago, Illinois, USA). Nominal variables are shown as frequency and percentage, while continuous variables are shown as arithmetic average. To research the difference between categorical variables, a Chi square test was used, while Fisher’s exact test was used when there was a lack of expected frequency. To test differences between parametric variables a one side analysis of variance was used, while to test multiple comparisons a Scheffe post hoc test was used. Probability of p< 0.05 was taken into consideration as statistically significant.
4. RESULTS
It was conducted a retrospective study which involved 1300 pregnant women who gave births in the Department of Obstetrics and Gynecology of University Clinical Hospital in Mostar in the period from January 1st 2015 to December 31st 2015 and their newborns.
The difference in age of pregnant women with different body mass index was not statistically relevant. The average age of pregnant women with normal body mass was 29.52 ± 5.48, overweight pregnant women 30.30 ± 5.138, and obese pregnant women 30.00 ± 5.103 (F = 2.730; p = 0.066). The youngest was 24, and the oldest was 49 years old. The average gestational age at delivery was 39.23 ± 1.556 (min 28; max. 42 weeks of gestation). The majority of pregnant women; 660 of them (50.8 %), were overweight in the early stages of their pregnancy, there were 322 (24.8 %) obese women, and there were 318 (24.5 %) normal weight women. At the end of the pregnancy, the highest number was that of obese pregnant women 925 (71.2 %), while 328 (25.2 %) pregnant women were overweight, and only 47 (3.6 %) pregnant women had normal weight.
As far as weight gain is concerned, the majority of pregnant women, that is 800 (61.5 %) of them, had normal weight gain, while 434 (33.4 %) pregnant women had excessive weight gain and 66 (5 %) pregnant women had low weight gain. The majority of pregnant women were obese at the end of their pregnancy. Spontaneous deliveries occurred most often that is 818 (62.9 %), while caesarean sections occurred 274 (21.1 %), induced labour 181 (13.9 %) and vacuum extraction 27 (2.1 %).
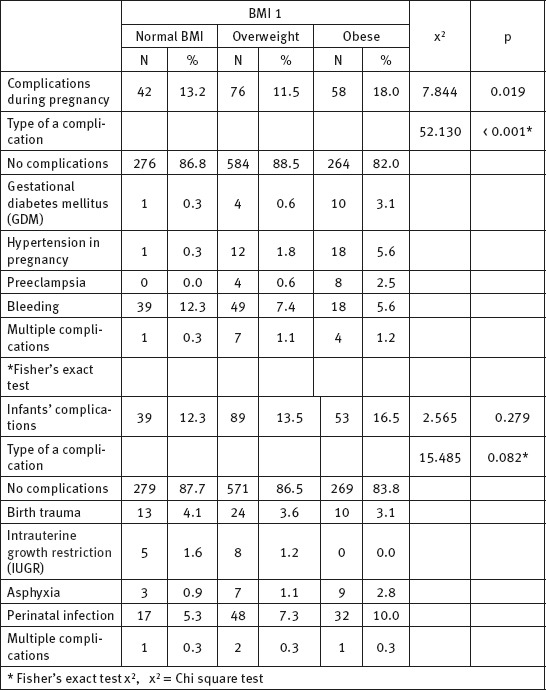
The majority of woman, 1124 (86.5 %), didn’t experience any complications during pregnancy, while 176 (13.5 %) pregnant women experienced certain complications in pregnancy. The most common complication during pregnancy was bleeding (8.2 %), pregnancy induced hypertension (2.4 %), preeclampsia (1.8 %), gestational diabetes mellitus (1.2 %). As far as infants are concerned, the majority of them, 1119 (86.1 %), were without complications, while 181 (13.9 %) of them had complications. The most common complication in infants was perinatal infection 97 (7.5 %) and birth trauma (3.6 %). Body mass index at the beginning of pregnancy has proved itself as significant statistic element in determining the mode of delivery (Table 1). The caesarean section, as a method of delivery, occurred most often in the group of overweight and in the group of obese pregnant woman (p< 0.001). Body mass index of pregnant women at the beginning of their pregnancy (BMI 1) and body mass index of pregnant women at the end of their pregnancy (BMI 2) proved to be a significant statistic element in the development of complications during pregnancy; the largest number of complications was in the group of obese pregnant women (hypertension 5.6 %, preeclampsia 2.5 %, bleeding (5.6 %), GDM 3.1 % (χ2 = 52,130; p< 0.001*) (Table 2). On the other hand, the body mass index of pregnant women in the early stages of pregnancy was not an important statistical element of development of complications for infants (χ2 = 15.485; p = 0,082*). Statistically, there is no notable difference in gestational age considering the body mass index before pregnancy (F = 0.221; p = 0.802).
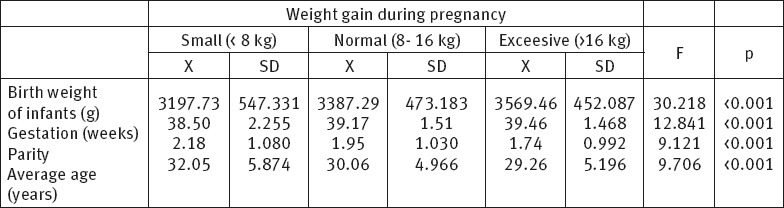
Table 1.
The distribution of pregnant women according to body mass index at the beginning of pregnancy and the method of delivery
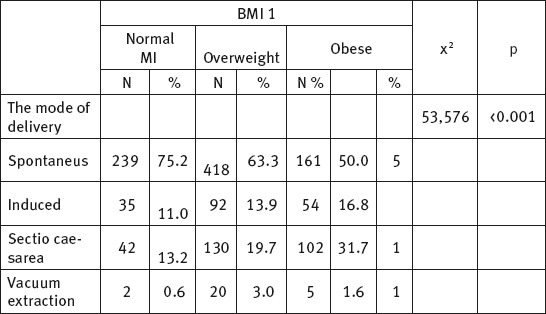
Table 2.
The distribution of pregnant women according to their body mass index at the beginning of their pregnancy and by complications in mother and infants
There is a statistically significant difference in the weight of infants in reference to pregnant women with different body mass index (F = 21.509; p< 0.001). The average birth weight of infants of obese pregnant women was significantly larger in comparison to infants of normal or overweight woman. Body mass index at the end of the pregnancy (BMI 2) has proven to be a significant statistical elements in determining the method of delivery (χ2 = 22.751; p< 0.001). In the group of obese women there was a higher percentage of births with caesarean section (23.9 %) in comparison to those with normal (10.6 %) or higher than normal body mass i.e. overweight (14.6 %). Body mass index at the end of the pregnancy (BMI 2) proved to be statistically significant element in the development of complications during pregnancy (χ2 = 22.152; p = 0.007*), nor as a significant element of development of complications in newborns (χ2 = 13.603; p = 0.139*) (Table 3). The difference in gestational age in pregnant women of different body mass is statistically significant (F = 3.048; p = 0.048) (Table 4). The difference in the body mass of infants of pregnant women with different body mass index at the beginning and at the end of pregnancy is statistically significant. Obese pregnant women gave birth to heavier children (3501.55 ± 475.483 g) than women with normal body mass (3070.85 ± 527.421g) or overweight (3313.31 ± 440.204 g) (F = 34.512; p< 0.001) (Table 4). The difference in vitality of infants in reference to different body mass of pregnant women was not statistically significant (F = 1.79; p = 0.167) (Table 4). Weight gain of pregnant women did not show itself to be statistically significant element in the development of complications during pregnancy (χ2 = 16.928; p = 0.055*), nor as a significant element of determining the mode of delivery (χ2 = 7.250; p = 0.298*), nor as a significant element of development of complications in newborn infants (χ2 = 2.958; p = 0.982*). However, the difference in parity of pregnant women of different body mass index was statistically relevant (F = 9.121; p< 0.001) (Table 5). Pregnant women with an excessive weight gain have a lower parity in comparison to pregnant women with small or normal weight gain. The difference in gestational age of pregnant women with different body weight is statistically significant (F = 12.841; p< 0.001). Pregnant women with excessive weight gain have a higher gestational age (39.4 ± 1.468), that is they gave birth later in life in comparison to those with a small (38.50 ± 2.255) or normal weight gain (39.46 ± 1.468) (Table 5). The difference in weight gain of infants delivered by mothers with different body mass is statistically significant (F = 30.218; p< 0.001). Pregnant women with excessive weight gain gave birth to heavier infants (3569.46 ± 452.087 g) in comparison to those with lower (3197.73 ± 547.331 g) or normal weight gain (3387.29 ± 473.183 g) (Table 5). Difference in age of pregnant women is statistically relevant (F = 9.706; p< 0.001). The results have shown that a lower weight gain is present in older pregnant women (32.05 ± 5.874), and that normal (30.06 ± 4.966) and excessive weight gain (29.26 ± 5.196) is present in younger pregnant women (p< 0.001) (Table 5). Difference in vitality of infants according to body weight gain is not statistically significant (F = 0.152; p = 0.859).
Table 3.
The distribution of pregnant women according to their body mass index at the end of their pregnancy and by complications found in mother and infants. BMI = body mass index; GDM = Gestational diabetes mellitus; HTA = Hypertension in pregnancy; IUGR = Intrauterine Grouth Restriction (IUGR)
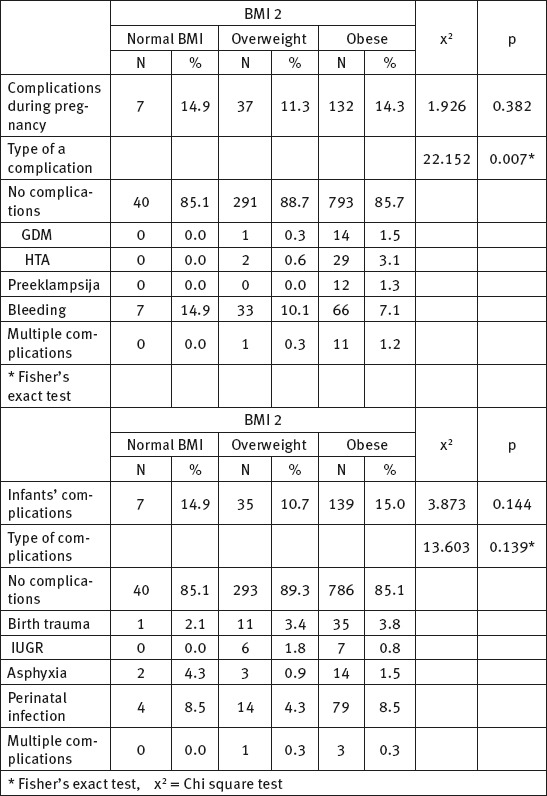
Table 4.
The distribution of pregnant women according to their body mass index at the end of pregnancy (BMI 2), by average age, gestation, parity, birth weight and Apgar scor of newborns. * Fisher’s exact test. BMI = body mass index
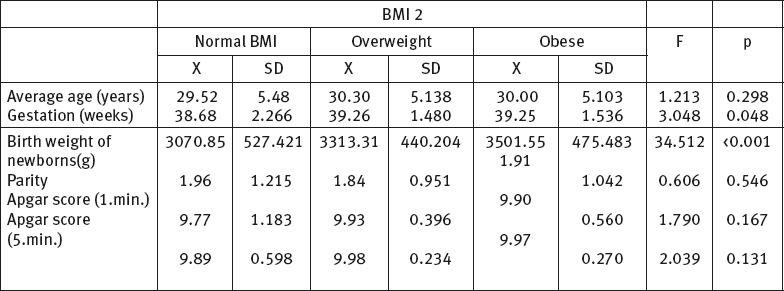
Table 5.
The distribution of birth weight of infants, gestation, parity and average age of pregnant women according to their weight gain during pregnancy
5. DISCUSSION
Obesity and increasing of obesity in young women is a major public health problem in the entire world and the same is in Bosnia and Herzegovina. We are facing pregnant women with high body mass index or obesity in clinical practice more and more often. Obesity and overweightness can result in adverse pregnancy, childbirth, and neonatal outcomes (20). Furthermore, the results of this study have shown that to be the case.
In early stages of pregnancy, the majority of pregnant women were overweight 50.8 %, there were 24.8 % obese women and 24.5 % had normal weight. At the end of the pregnancy, the highest number was obese pregnant women 71.2 %, while 25.2 % pregnant women were overweight, and only 3.6 % pregnant women had normal weight.
As far as weight gain is concerned, the majority of pregnant women, that is 61.5 % of them, had normal weight gain, 33.4 % pregnant women had excessive weight gain and 5 % pregnant women had low weight gain. The average weight gain of a healthy pregnant woman is 11.5 kg, and about 2.5–3.5 kg of that is in body fat supplies. A higher weight gain, in absence of pathological conditions such as preeclampsia and related edema, is mostly a result of a larger amount of body fat. Adipose tissue (body fat) as an active endocrine organ can lead to endothelial dysfunction of blood vessels in mother and placenta, which can lead to expectation of a bad perinatal result (2, 3, 4).
In the study conducted by Reylonds and Inder 2014, the frequency of obese pregnant women at the end of their pregnancy was 35 %, which is twice less than in our research (14). In the study from Dale Country, Wisconsin year 2011, 50.6 % of pregnant women were overweight which is twice as much as in our study (15).
In our study, it was shown that the body mass index in the early stages of pregnancy (BMI 1) and in the late stages of pregnancy (BMI 2) has a significant influence on the method of giving birth. When it comes to overweight and obese pregnant women, it was proved that there is a higher frequency of caesarean sections and vacuum extraction deliveries in comparison to pregnant women with normal body weight (p< 0.001). Within the group of obese pregnant women there is a higher percentage of caesarean sections (23.9 %) in comparison to those with normal (10.6 %) and excessive body weight (14.6 %). Numerous studies have shown a higher frequency of caesarean sections in overweight and obese pregnant women (18-25).
A study conducted in Germany from 1990 to 2012 revealed that the frequency of caesarean section in case of overweight pregnant women was 38.8 % and in case of obese women it was 45 %, which is a higher frequency than in our study (16). A study conducted in Brazil in 2012 shows an increased frequency of caesarean sections as well as proportional increase in the frequency of caesarean sections in relation to increased weight gain (17, 31, 32).
Body mass index in the early stages of pregnancy (BMI 1) and body mass index of pregnant women at the end of their pregnancy (BMI 2) proved to be a significant element in the development of complications during pregnancy; the highest amount of complications during pregnancy occurred in the group of obese pregnant women. The following complications occurred: hypertension (5.6 %), GDM (3.1 %), preeclampsia (2.5%) (p < 0.001*). In addition, weight gain did not prove itself to a significant factor for the development of complications during pregnancy (p = 0,055*), nor as a significant factor in determining the method of childbirth (p = 0.298*). Pregnant women that were overweight or obese had a higher frequency of GDM, hypertension during pregnancy and preeclampsia, while women with normal body mass index had a higher rate of bleeding.
A number of significant studies have shown that larger BMI, that is the when a women is overweight or obese, influences the development of gestational diabetes, pregnancy hypertension and preeclampsia. It has been estimated that compared to women with a normal BMI, the risk of pregnancy diabetes is 2 and 4 times higher in overweight and obese women, respectively (18-25, 31, 32).
The body mass index in the beginning of pregnancy (BMI 1), as well as weight gain during pregnancy were not significant factors in the development of complications in newborns (p = 0.082*; p = 0.928*), while newborns of pregnant women with excessive body weight gain and obesity at the end of the pregnancy had a higher frequency of perinatal infections (8.5 %) and trauma (3.8 %) in comparison with pregnant women with normal body mass (2.1 %). A study by Cresswell JA et al. conducted in Sub-Saharan Africa showed a higher frequency of perinatal infections in obese women (22). According to a study conducted in Sweden in 2014, a high mothers BMI equals a higher risk for development of asphyxia and bad clinical presentation of a newborn (23).
Our study revealed that a higher body mass index of mothers at the start and the end of the pregnancy as well as a higher weight gain during pregnancy, cause higher body mass of infants (p< 0.001). The same results were obtained in some other studies (19-24) while a study conducted in Washington showed opposing results according to which women with a higher BMI gave birth to underdeveloped children more often (25).
In addition, the results have shown that older pregnant women and women who gave birth more than once have a lower weight gain during pregnancy and that with the increase of parity pregnant women have a higher body mass index at the beginning of the pregnancy (p< 0.001). The results conducted by Kashanian et al. (2008) showed that mother’s weight gain during pregnancy was considerably lower in obese women, which is consistent with the results of our study (20).
The results have shown that the pregnancy lasts longer with pregnant women with a higher body mass index and a higher gain (p< 0.001). A retrospective study of 9336 births at the University of California, San Francisco showed that a higher BMI is associated with prolonged gestation at term. Authors concluded that achieving an optimal BMI before conception may reduce the risk of post-term pregnancy and its associated complications (26).
In addition, numerous studies have shown a lower sum of Apgar scale in infants of obese mothers, while our study did not show that there are statistically significant differences in the vitality of newborns according to body mass index of mothers at the beginning and the end of their pregnancies or depending on weight gain of mothers during pregnancy, one of the possible reasons being the small sample size (Table 4) (9,20,28). Abnormal BMI was not associated with poor pregnancy outcomes in cohort of Cameroonian women (33).
It is not clear whether obesity is a direct cause of adverse pregnancy outcome or whether the association between obesity and adverse outcome is due to factors or characteristics that are shared by both entities, such as advanced maternal age, higher gravidity and associated complications in pregnancy. Women who were obese or overweight before pregnancy have a higher risk for complications during pregnancy and delivery and they can also expect more health problems occurring to their children, both in infant age and later in life. Therefore, women with a high BMI need more care during pregnancy and childbirth which requires high expenses (29, 30, 34).
The health of the mother and children in most societies is protected by law and considered important for numerous reasons. Mother and children are biologically more sensitive and more subject to influences from environment. The reproductive ability and health of the next generation of adults depends (besides on the gene factor) directly on preconception, prenatal and perinatal period as well as the environmental risk factors (9, 31).
Finally, we acknowledge the small sample size as being a weakness of the present study, but this was due to it being a retrospective study carried out in hospital over a period of one year only. It is certain that there is a need for preconception advisement that would cover the topic of reduction of body mass and exercise, as well as a need for multidiscipline approach before the planned pregnancy. It is our belief that the results of this study can direct attention to the importance of determining body mass index and body mass gain in antenatal care of pregnant women which would surely lead to better perinatal results.
6. CONCLUSION
Nutritive status and weight gain of a mother during pregnancy are an important indication of her health and of the foetus growth. Overweightness and obesity of a mother before pregnancy and during pregnancy has a negative influence on the health of the mother and infant. Moreover, it is linked with a negative pregnancy outcome. BMI was associated with a increased risk of adverse perinatal outcome.
Footnotes
• Author’s contributions: IB collected the data, TB analyzed them and wrote the text. VM and TB assisted in writing the text including final editing and critical revision of the scientific content. All authors have read the text and approved the final manuscript.
• Conflict of interest: None declared.
REFERENCES
- 1.WHO. Obesity and overweight. Fact sheet N°311. 2015 [Google Scholar]
- 2.Münzberg H, Björnholm M, Bates HS, Myers Jr MG. Leptin receptor action and mechanisms of leptin resistance. CMLS Cell Mol Life Sci. 2005;62:642–52. doi: 10.1007/s00018-004-4432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 4.Gesink Law DC, Maclehose RF, Longnecker MP. Obesity and time to pregnancy. Hum Reprod. 2007;22:414–20. doi: 10.1093/humrep/del400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368:1136–8. doi: 10.1016/S0140-6736(06)69473-7. [DOI] [PubMed] [Google Scholar]
- 6.Beaten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436–40. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175–82. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 8.Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH, et al. Obesity, obstetric complications and cesarean delivery rate-a population-based screening study. FASTER Research Consortium. Am J Obstet Gynecol. 2004;190:1091–7. doi: 10.1016/j.ajog.2003.09.058. [DOI] [PubMed] [Google Scholar]
- 9.Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA. 2009;301:635–50. doi: 10.1001/jama.2009.113. [DOI] [PubMed] [Google Scholar]
- 10.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MV. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196:322–8. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clausen T, Burski TK, Oyen N, Godang K, Bollerslev J, Henriksen T. Maternal anthropometric and metabolic factors in the first half of pregnancy and risk of neonatal macrosomia in term pregnancies. A Prospective study. Eur J Endocrinol. 2005;153:887–94. doi: 10.1530/eje.1.02034. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro C, Sutija VG, Bush J. Effect of maternal weight gain on infant birth weight. J Perinat Med. 2000;28:428–31. doi: 10.1515/JPM.2000.056. [DOI] [PubMed] [Google Scholar]
- 13.Challier JC, Basu S, Bintein T, et al. Obesity in pregnancy stimulates macrophage accumulation and inflammation in the placenta. Placenta. 2008;29(3):274. doi: 10.1016/j.placenta.2007.12.010. doi:10.1016/j.placenta.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reynolds LC, Inder TE, Neil JJ, Pineda RG, Rogers CE. Maternal obesity and increased risk for autism and developmental delay among very preterm infants. J Perinatol. 2014 doi: 10.1038/jp.2014.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeal C, Remington P, Ndiaye M, Stewart K, Stattelman-Scanlan D. The epidemiology of maternal overweight in Dane County, Wisconsin. 2014;113:24–7. [PubMed] [Google Scholar]
- 16.Kyvernitakis I, Köhler C, Schmidt S, Misselwitz B, Großmann J, Hadji P, Kalder M. Impact of maternal body mass index on the cesarean delivery rate in Germany from 1990 to 2012. J Perinat Med. 2014 doi: 10.1515/jpm-2014-0126. [DOI] [PubMed] [Google Scholar]
- 17.Gonçalves CV, Mendoza-Sassi RA, Cesar JA, de Castro NB, Bortolomedi AP. Body mass index and gestational weight gain as factors predicting complications and pregnancy outcome. Rev Bras Ginecol Obstet. 2012;34:304–9. doi: 10.1590/s0100-72032012000700003. [DOI] [PubMed] [Google Scholar]
- 18.Sahu MT, Agarwal A, Das V, Pandey A. Impact of maternal body mass indeks on obstetric outcome. J Obstet Gynaecol Res. 2007;33:655–9. doi: 10.1111/j.1447-0756.2007.00646.x. [DOI] [PubMed] [Google Scholar]
- 19.Raatikainen K, Heiskanen N, Heinonen S. Transition from Overweight to Obesity Worsens Pregnancy Outcome in a BMI-dependent Manner. Obesity. 2006;14:165–71. doi: 10.1038/oby.2006.20. [DOI] [PubMed] [Google Scholar]
- 20.Kashanian M, Dadkhah F, Baradaran HR, Bakoui F. Evaluation of the relationship between high maternal weight and the duration of different stages of labor, delivery rout, neonatal weight and apgar score. Obesity research and clinical practice. 2008;2:225–30. doi: 10.1016/j.orcp.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Kiel DW, Dodson EA, Artal R, Boehmer TK, Leet TL. Gestational weight gain pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110:752–8. doi: 10.1097/01.AOG.0000278819.17190.87. [DOI] [PubMed] [Google Scholar]
- 22.Cresswell JA, Campbell OM, De Silva MJ, Filippi V. Effect of maternal obesity on neonatal death in sub-Saharan Africa: multivariable analysis of 27 national datasets. Lancet. 2012;380:1325–30. doi: 10.1016/S0140-6736(12)60869-1. [DOI] [PubMed] [Google Scholar]
- 23.Persson M, Johansson S, Villamor E, Cnattingius S. Maternal overweight and obesity and risks of severe birth-asphyxia-related complications in term infants: a population-based cohort study in Sweden. PLoS Med. 2014;20:11, e1001648. doi: 10.1371/journal.pmed.1001648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nohr EA, Vaeth M, Bech BH, et al. Maternal Obesity and Neonatal Mortality According to Subtypes of Preterm Birth. Obstet Gynecol. 2007;110(5):1083–90. doi: 10.1097/01.AOG.0000286760.46679.f8. [DOI] [PubMed] [Google Scholar]
- 25.Jared M, Baeten BA, Elizabeth A. Bukusi i sur. Pregnancy Complications and Outcomes Among Overweight and Obese Nulliparous Women. Am J Public Health. 2001;91:436–40. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stotland NE, Washington AE, Caughey AB. Prepregnancy body mass index and the length of gestation at term. Am J Obstet Gynecol. 2007;197(4):378. doi: 10.1016/j.ajog.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 27.Graves B, DeJoy S, Pekow P. Maternal Body Mass Indeks, Delivery Route, and Induction in a Midwifery Caseload. J Midwifery Womens Health. 2006;51:254–9. doi: 10.1016/j.jmwh.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 28.Chen M, McNiff C, Madan J, Goodman E, Davis JM, Dammann O. Maternal obesity and neonatal Apgar scores. J Matern Fetal Neonatal Med. 2010;23:89–95. doi: 10.3109/14767050903168440. [DOI] [PubMed] [Google Scholar]
- 29.Guo L, Liu J, Ye R, Liu J, Zhuang Z, Ren A. Gestational Weight Gain and Overweight in Children Aged 3-6 Years. J Epidemiol. 2015;25(8):536–43. doi: 10.2188/jea.JE20140149. doi:10.2188/jea.JE20140149. Epub 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mamun AA, Mannan M, Doi SA. Gestational weight gain in relation to offspring obesity over the life course: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2014;15(4):338–47. doi: 10.1111/obr.12132. doi:10.1111/obr.12132. [DOI] [PubMed] [Google Scholar]
- 31.Abenhaim HA, Kinch RA, Morin L, Benjamin A, Usher R. Effect of prepregnancy body mass index categories on obstetrical and neonatal outcomes. Archives of Gynecology and Obstetrics. 2007;275(1):39–43. doi: 10.1007/s00404-006-0219-y. [DOI] [PubMed] [Google Scholar]
- 32.Liu X, Du J, Wang G, Chen Z, Wang W, Xi O. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China. Archives of Gynecology and Obstetrics. 2012;283(1):65–70. doi: 10.1007/s00404-009-1288-5. [DOI] [PubMed] [Google Scholar]
- 33.Fouelifack FY, Fouedjio JH, Fouogue JT, Sando Z, Fouelifa LD, Mbu RE. Associations of body mass index and gestational weight gain with term pregnancy outcomes in urban Cameroon: a retrospective cohort study in a tertiary hospital. BMC Res Notes. 2015;8:806. doi: 10.1186/s13104-015-1765-9. doi:10.1186/s13104-015-1765-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moll U, Olsson H, Landin-Olsson M. Impact of Pregestational Weight and Weight Gain during Pregnancy on Long-Term Risk for Diseases. PLoS One. 2017;12(1):e0168543. doi: 10.1371/journal.pone.0168543. doi:10.1371/journal.pone.0168543.eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agrawal S, Singh A. Obesity or Underweight–What is Worse in Pregnancy? J Obstet Gynaecol India. 2016;66(6):448–452. doi: 10.1007/s13224-015-0735-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


