Few measures in public health can compare with the impact of vaccines. Vaccinations have reduced disease, disability, and death from a variety of infectious diseases. For example, in the United States, children are recommended to be vaccinated against 16 diseases (1). Table 1 highlights the impact in the United States of immunization against nine vaccine-preventable diseases, including smallpox and a complication of one of those diseases, congenital rubella syndrome, showing representative annual numbers of cases in the 20th century compared with 2016 reported cases (2, 3). All of the diseases have been reduced by more than 90% and many have either been eliminated or reductions of 99% or more have been achieved. A recent analysis of vaccines to protect against 13 diseases estimated that for a single birth cohort nearly 20 million cases of diseases were prevented, including over 40,000 deaths (4). In addition to saving the lives of our children, vaccination has resulted in net economic benefits to society amounting to almost $69 billion in the United States alone. A recent economic analysis of 10 vaccines for 94 low- and middle-income countries estimated that an investment of $34 billion for the immunization programs resulted in savings of $586 billion in reducing costs of illness and $1.53 trillion when broader economic benefits were included (5). The only human disease ever eradicated, smallpox, was eradicated using a vaccine, and a second, polio, is near eradication, also using vaccines (6, 7).
Table 1.
Comparison of 20th century annual morbidity and current estimates vaccine-preventable diseases
| Disease | 20th Century annual morbidity (2) | 2016 Reported cases (3) | Percent decrease (%) |
| Smallpox | 29,005 | 0 | 100 |
| Diphtheria | 21,053 | 0 | 100 |
| Measles | 530,217 | 69 | >99 |
| Mumps | 162,344 | 5,311 | 97 |
| Pertussis | 200,752 | 15,737 | 92 |
| Polio (paralytic) | 16,316 | 0 | 100 |
| Rubella | 47,745 | 5 | >99 |
| Congenital rubella syndrome | 152 | 1 | 99 |
| Tetanus | 580 | 33 | 94 |
| Haemophilus influenzae | 20,000 | 22* | >99 |
Haemophilus influenzae type b (Hib) < 5 y of age.
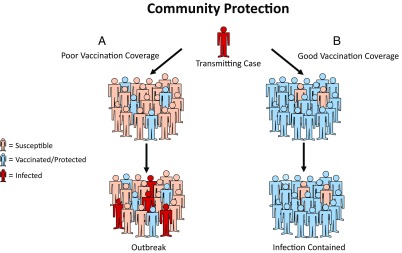
Vaccines not only provide individual protection for those persons who are vaccinated, they can also provide community protection by reducing the spread of disease within a population (Fig. 1). Person-to-person infection is spread when a transmitting case comes in contact with a susceptible person. If the transmitting case only comes in contact with immune individuals, then the infection does not spread beyond the index case and is rapidly controlled within the population. Interestingly, this chain of human-to-human transmission can be interrupted, even if there is not 100% immunity, because transmitting cases do not have infinite contacts; this is referred to as “herd immunity” or “community protection,” and is an important benefit of vaccination.
Fig. 1.
(A) A highly susceptible population in which a transmitting case is likely to come in contact with a susceptible person leading to a chain of person-to-person transmission. (B) A highly immune population in which a transmitting case is unlikely to come in contact with a susceptible person, thereby breaking the chain of transmission and achieving indirect protection of remaining susceptibles because they are not exposed.
Mathematical modelers can estimate on average how many persons the typical transmitting case is capable of infecting if all of the contacts were susceptible (i.e., a population of 100% susceptibility). This number is known as R0, or the basic reproductive number. The immunity threshold needed within the population for terminating transmission can be calculated in percent as (R0 − 1)/R0 × 100 and is a guide to setting immunity levels and vaccination coverage targets for various diseases (8). For example, measles is one of the most contagious of vaccine-preventable diseases, with an estimated immunity threshold of 92–94%. In contrast, the protection threshold for rubella is estimated at 83–85%. Thus, eliminating rubella transmission is easier than measles, and when there are gaps in immunization coverage leading to accumulation of susceptibles, measles is often the first vaccine-preventable disease identified. Because of community protection induced by vaccines, persons who cannot be vaccinated (e.g., have contraindications or are younger than the age for whom vaccines are recommended), as well as persons who fail to make an adequate immune response to the vaccine (although most vaccines are highly effective, they are not 100% effective), can be protected indirectly because they are not exposed (Fig. 1). Thus, for most vaccines, achieving high levels of coverage is important not only for individual protection but in preventing disease in vulnerable populations that cannot be directly protected by vaccination. This provides the rationale for interventions to achieve high population immunity, such as removing barriers that may prevent access to vaccines (e.g., providing recommended vaccines without cost), as well as mandates for immunization requirements for attending school (9). There are many reasons why vaccinations may not be received as recommended. One extreme is outright opposition to vaccines. Probably even more common may be that making the effort to receive vaccines (e.g., making the healthcare visits at the appropriate time so vaccines can be administered) may be a low priority compared with other issues, so in the absence of having a mandate for vaccination, other things take priority. Thus, appropriate mandates could help in making vaccination a priority for all (10).
It’s often said that vaccines save lives, but this is not strictly true; it is vaccination that saves lives. A vaccine that remains in the vial is 0% effective even if it is the best vaccine in the world. Thus, it is imperative that we all work together to assure that a high level of coverage is obtained among populations for whom vaccines are recommended. In some sense, vaccines have become victims of their own success. Diseases that once induced fear and sparked desire for vaccines are now rare, and there is a false and dangerous sense of complacency among the public.
In addition, in recent years, growing numbers of persons have become hesitant about vaccines, fearing side effects and not appreciative of the enormous health and economic benefits that vaccines provide. A CDC report on 159 measles cases reported between January 4 and April 2, 2015, showed that 68 United States residents with measles were unvaccinated, and of these 29 (43%) cited philosophical or religious objections to vaccination (11). A 2014 national web-based poll of parents in the United States estimated that 90.8% (89.3–92.1%) reported accepting or planning to accept all recommended noninfluenza childhood vaccines, 5.6% (4.6–6.9%) reported intentionally delaying one or more, and 3.6% (2.8–4.5%) reported refusing one or more vaccines (12). A national survey of pediatricians in the United States reported that the proportion of pediatricians reporting parental vaccine refusals increased from 74.5% in 2006 to 87.0% in 2013 (13). A 67-country survey on the state of vaccine confidence reported an average of 5.8% of respondents globally were skeptical about the importance of vaccines, with that proportion rising to more than 15% in some countries (14). One of the major concerns in recent years has been the allegations that vaccines can cause autism. There are three major theories advanced on the role of vaccines in causing autism: (i) measles, mumps, rubella vaccine (MMR); (ii) thimerosal, an ethyl mercury containing preservative in many vaccines in the United States in the past, now mostly out of vaccines recommended for children; and (iii) too many vaccines (15). There have been multiple well-conducted studies and independent reviews of those studies by the Institute of Medicine (now the National Academy of Medicine) that do not support a role for vaccines in causing autism (16). Independent evaluation of the safety of the immunization schedule has found it to be extremely safe (17). However, translating the science into information capable of influencing vaccine skeptics has been difficult.
The National Vaccine Advisory Committee (NVAC) in the United States issued a report in 2015, with 23 recommendations to assure high levels of vaccine confidence (18). The recommendations have five focus areas: (i) measuring and tracking vaccine confidence, (ii) communication and community strategies to increase vaccine confidence, (iii) healthcare provider strategies to increase vaccine confidence, (iv) policy strategies to increase vaccine confidence, and (v) continued support and monitoring of the state of vaccine confidence. Critical to assuring confidence is evidence-based research to evaluate which interventions are most effective. The NVAC recommended that a repository of evidence-based best practices for informing, educating, and communicating with parents and others in ways that foster or increase vaccine confidence be created. And while we have focused on children, vaccine preventable diseases exact a substantial health burden in adults and immunization coverage rates for most recommended vaccines are substantially lower for adults than those achieved for recommended vaccines in children. Thus, there is need not only in enhancing immunization rates in children but also in adults.
In summary, vaccines are some of the most effective and also cost-effective prevention tools we have. But vaccines that are not administered to persons for whom they are recommended are not useful. It is incumbent upon all of us who work in the healthcare setting, as well as community leaders, to stress to our friends and colleagues the importance of vaccination both for the individual vaccinated as well as for the communities in which the individuals live. Also critically important, there remains an urgent need for greater emphasis on research to develop vaccines for global diseases for which vaccines either do not exist or need improvement.
Acknowledgments
The authors thank Dianne Miller, Ali Ellebedy, and Sandra Roush for their assistance in preparation of the manuscript.
Footnotes
See Perspective on page 4055.
References
- 1.Centers for Disease Control and Prevention 2017 Recommended immunization schedule for children and adolescents 18 years or younger, United States 2017. Available at https://www.cdc.gov/vaccines/schedules/downloads/child/0-18yrs-child-combined-schedule.pdf. Accessed March 13, 2017.
- 2.Centers for Disease Control and Prevention Notifiable Diseases and Mortality Tables. MMWR Morb Mortal Wkly Rep. 2016;65:ND-924-ND-941. [PubMed] [Google Scholar]
- 3.Roush SW, Murphy TV. Vaccine-Preventable Disease Table Working Group Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298:2155–2163. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 4.Zhou F, et al. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133:577–585. doi: 10.1542/peds.2013-0698. [DOI] [PubMed] [Google Scholar]
- 5.Ozawa S, et al. Return on investment from childhood immunization in low- and middle-income countries, 2011-20. Health Aff (Millwood) 2016;35:199–207. doi: 10.1377/hlthaff.2015.1086. [DOI] [PubMed] [Google Scholar]
- 6.Fenner F, Henderson DA, Arita I, Jezek AZ, Ladnyi ID. Smallpox and its Eradication. World Health Organization; Geneva: 1988. [Google Scholar]
- 7.Morales M, Tangermann RH, Wassilak SG. Progress toward polio eradication—Worldwide, 2015-2016. MMWR Morb Mortal Wkly Rep. 2016;65:470–473. doi: 10.15585/mmwr.mm6518a4. [DOI] [PubMed] [Google Scholar]
- 8.Fine PEM, Mulholland K. Community immunity. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 6th Ed. Elsevier; Philadelphia: 2013. pp. 1395–1412. [Google Scholar]
- 9.Rodewald LE, Orenstein WA, Hinman AR, Schuchat A. Immunization in the United States. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 6th Ed. Elsevier; Philadelphia: 2013. pp. 1310–1333. [Google Scholar]
- 10.Orenstein WA, Hinman AR. The immunization system in the United States—The role of school immunization laws. Vaccine. 1999;17:S19–S24. doi: 10.1016/s0264-410x(99)00290-x. [DOI] [PubMed] [Google Scholar]
- 11.Clemmons NS, Gastanaduy PA, Fiebelkorn AP, Redd SB, Wallace GS. Centers for Disease Control and Prevention (CDC) Measles—United States, January 4–April 2, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:373–376. [PMC free article] [PubMed] [Google Scholar]
- 12.Frew PM, et al. Changes in childhood immunization decisions in the United States: Results from 2012 & 2014 National Parental Surveys. Vaccine. 2016;34:5689–5696. doi: 10.1016/j.vaccine.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hough-Telford C, et al. Vaccine delays, refusals, and patient dismissals: A survey of pediatricians. Pediatrics. 2016;138:e20162127. doi: 10.1542/peds.2016-2127. [DOI] [PubMed] [Google Scholar]
- 14.Larson HJ, et al. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerber JS, Offit PA. Vaccines and autism: A tale of shifting hypotheses. Clin Infect Dis. 2009;48:456–461. doi: 10.1086/596476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute of Medicine . Adverse Effects of Vaccines: Evidence and Causality. The National Academy Press; Washington, DC: 2012. [PubMed] [Google Scholar]
- 17.Maglione MA, et al. Safety of vaccines used for routine immunization of U.S. children: A systematic review. Pediatrics. 2014;134:325–337. doi: 10.1542/peds.2014-1079. [DOI] [PubMed] [Google Scholar]
- 18.National Vaccine Advisory Committee 2015 Assessing the state of vaccine confidence in the United States: Recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 9, 2015 [corrected]. Public Health Rep 130:573–595; erratum in Public Health Rep 2016. [Google Scholar]