Supplemental Digital Content is available in the text
Keywords: diabetes, Islander, obesity, Pacific, pediatric
Abstract
Estimate prevalence of obesity and acanthosis nigricans (AN) among children in United States Affiliated Pacific (USAP) jurisdictions.
Cross-sectional measurement of weight, height, and AN in 5775, 2 to 8 years old in 51 communities—Hawai‘i, Alaska, Commonwealth of the Northern Mariana Islands, Guam, American Samoa, Palau, Republic of the Marshall Islands (RMI), 4 Federated States of Micronesia (Pohnpei, Yap, Kosrae, Chuuk). Analyses weighted to jurisdiction-specific sex and age distributions accounting for clustering of communities within jurisdictions.
Prevalence of obesity was 14.0%, overweight 14.4%, healthy weight 68.9%, and underweight 2.6%, higher in males (16.3%) than females (11.6%), higher among 6 to 8 years old (16.3%) than 2 to 5 years old (12.9%), highest in American Samoa (21.7%), and absent in RMI. In total, 4.7% of children had AN, with no sex difference, higher in 6 to 8 years old (6.8%) than 2 to 5 years old (3.5%) and highest in Pohnpei (11.9%), and absent in Alaska. Obesity was highly associated with AN (odds ratio = 9.25, 95% confidence interval = 6.69–12.80), with the strongest relationships among Asians, followed by Native Hawaiians and Pacific Islanders (NHPI).
Obesity, age, and Asian and NHPI race were positively associated with AN.
1. Introduction
Rates of obesity in preschool children in the United States have plateaued, and declined by 4% in non-Hispanic Whites,[1] thought to be related to decreases in intake of sugar-sweetened beverages and fast food, and decreased caloric content of common foods in the food supply. However, the decline among non-Hispanic Whites will intensify the disparity of obesity among race/ethnic groups. Further, the proportion of the obese people that are extremely obese is increasing, forecasting a rise in metabolic disease and diabetes.[2]
Pacific Islanders are the predominant racial/ethnic groups of the United States Affiliated Pacific Region (USAP) yet are not described in the National Health and Nutrition Examination Survey reports.[3] Other survey data sets are available in some of the USAP but only provide information on self-reported obesity for adolescent children, such as the Youth Behavioral Risk Factor Survey and the National Health Information Survey.[4]
A meta-analysis of the limited published data on measured body size of children in the USAP—including Alaska, American Samoa, Commonwealth of the Northern Marianas (CNMI), Guam, Hawai‘i, Palau, Pohnpei, Yap, and the Republic of the Marshall Islands (RMI)—showed high rates of obesity.[5] Higher prevalence of obesity was found in the older ages (6–8 years), with a high degree of variability throughout the region, whereas overweight was constant across the age groups.
Screening for chronic conditions is not generally performed in young children. However, obesity in childhood is associated with adult noncommunicable diseases (NCD), of which there is an epidemic in the Pacific Islands resulting in declaration of an NCD Regional State of Emergency.[6] Acanthosis nigricans (AN) is a condition that is found on the skin in the presence of hyperinsulinemia, which is correlated with obesity,[7] and is an indication of metabolic disease.
The objective of this paper is to describe the prevalence of obesity and AN, and differences by race/ethnicity among young children in the US Affiliated Pacific (USAP). Data were collected by the Children's Healthy Living (CHL) Program using rigorous selection, measurement, and analytic methodology[8,9] in all of the USAP jurisdictions.
2. Methods
2.1. Study population
Cross-sectional survey data were collected on 2 to 8 years old children that were recruited from 51 communities in the 11 USAP jurisdictions (Hawai‘i, Alaska, CNMI, Guam, American Samoa, Palau, RMI, and the 4 Federated States of Micronesia—Pohnpei, Yap, Kosrae, and Chuuk). Communities were selected for CHL based on census data for population size >1000, relative accessibility and representativeness, having >25% of the population of indigenous/native descent (15% in Alaska due to focus on accessible communities), and having >10% of the population under age 10. Sample size was powered on BMI for the CHL intervention trial.[9]
Of 51 communities selected, 27 communities were selected in 2011 from 5 CHL Intervention study jurisdictions using 2000 US census data[9] and 24 communities were selected in 2013, from 6 CHL Prevalence study jurisdictions, using regional 2010 data[10–12]; 5775 children participated from the 51 communities; 4488 children were from the jurisdictions participating in the CHL randomized controlled trial (Intervention Study), for which baseline data were used[9] (Table 1). The other 1287 children were from jurisdictions participating in the CHL prevalence study. Sample size was powered for BMI prevalence. The same methods were used for data collection in both CHL studies.
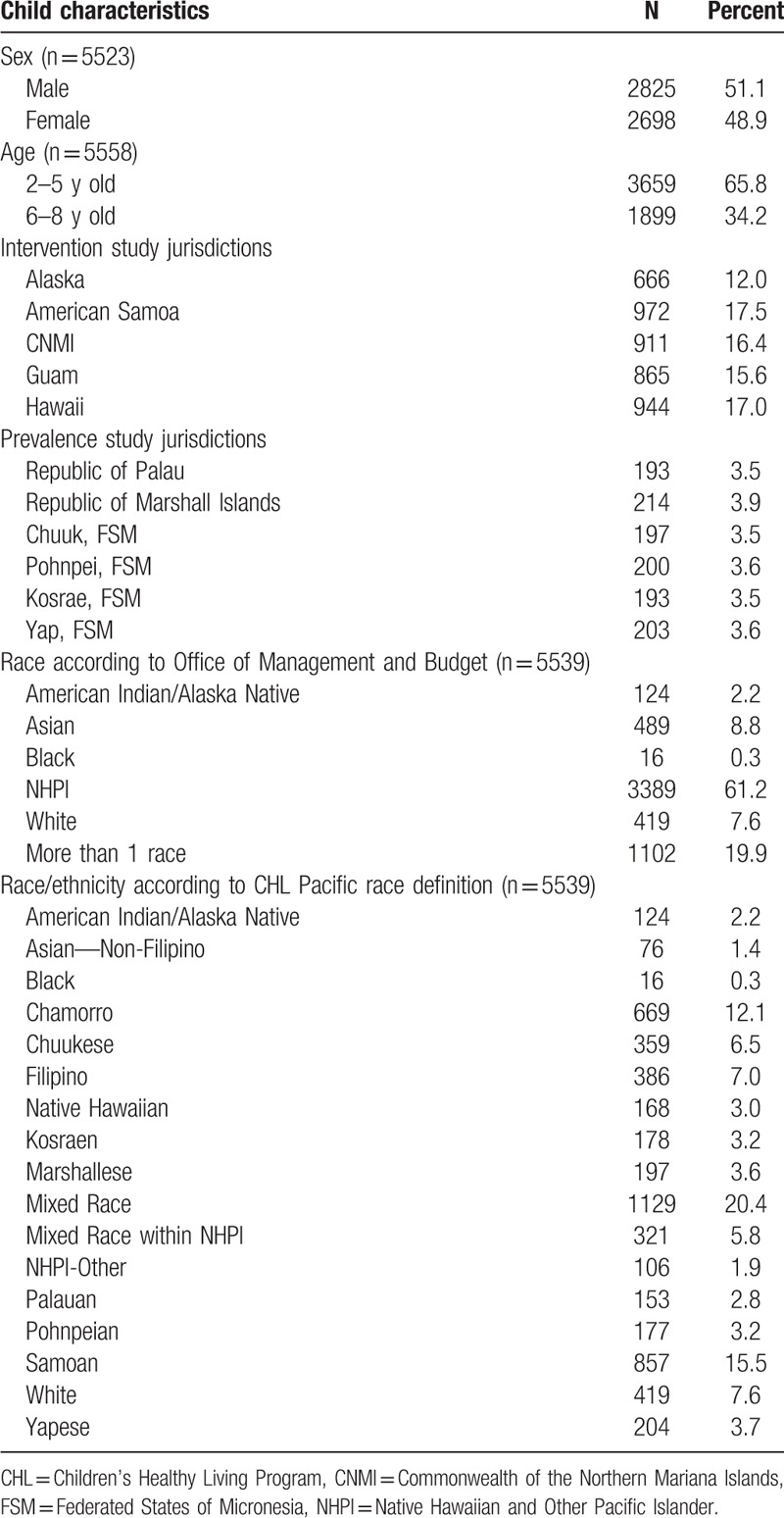
Table 1.
Characteristics of study participants with anthropometric measurements in the Children's Healthy Living program (n = 5558).
Of the 5775 children, 217 children were excluded because their age as reported by the caregiver was out of the study age range. Of the remaining 5558, 5463 children (51.1% male) were measured for anthropometry and 4625 (50.8% male) were screened for AN. The AN number is smaller because, by design, some communities in the Intervention study were only measured for anthropometry.
2.2. Outcome measures
Anthropometry: Weight and height were measured according to standard procedures[13] and equipment (Perspective Enterprises Stadiometer model PE-AIM-101, Seca scale Model 876) throughout the USAP region. All anthropometric measurers were standardized to 1 expert with intra-measurer reliability of 0.999 for both weight and height.[8] Three measurements of height and of weight were taken; if 2 of the 3 were not within 0.2 units, the first 3 measurements were crossed out and an additional set of 3 measurements was taken (Supplemental Table 1). All measurements were averaged for analysis. Body mass index (BMI) was calculated as weight (kg)/(height (m)[2]. Categories were defined using Centers for Disease Control reference BMI percentile data according to age and sex where obese was greater than the 95th; overweight was 85th to the 94th; healthy weight was 5th to the 84th; and underweight was less than the 5th.[14]
Acanthosis nigricans (AN): AN was measured by the Burke method[15] on a 0 to 4 scale and analyzed as present (1–4) or absent (0) in regression models (Supplemental Table 2).
Race/ethnicity: Parents or caregivers reported the race/ethnicity of children by completing a questionnaire that provided check boxes according to Office of Management and Budget (OMB) categories[16] with additional categories of common ethnic groups of the region, as well as write-in space, listed under the races of Asian (ASIAN), Native Hawaiian and Pacific Islanders (NHPI), and American Indian/Alaska Native (AIAN) (Supplemental Table 3). A “Pacific race” variable with 17 categories was developed from these data: more than one race, AIAN, Asian Other Than Filipino, Black, White, Chamorro, Chuukese, Filipino, Kosraen, Marshallese, Native Hawaiian, Palauan, Pohnpeian, Samoan, Yapese, more than one NHPI ethnicity, and other NHPI Group. Other NHPI groups included Carolinian, Tongan, Kiribati, Tokelauan, and Tahitian.
2.3. Statistical procedures
All analyses used survey sampling techniques[17] that weighted the sample to the young child population size in each community, based on census data, and that accounted for the clustering of participants in communities within jurisdictions. The weighting resulted in representative estimates for the jurisdictions and the region, with 2 caveats. In Hawaii, the communities represented the non-Honolulu population and, in Alaska, the communities represented the most populous areas. Prevalence was estimated with 95% confidence intervals (CI) overall and by sex, age group, race/ethnicity, and jurisdiction. Prevalence was compared between groups by chi-square test. Logistic regression models of AN assessed its relationship with obesity, adjusted for age group (2–5 years or 6–8 years), sex, and race/ethnicity according to either the OMB or Pacific definitions. Odds ratios and 95% CI were the primary statistics reported from the models. Since Pacific Islanders were the focus of the study and the White population did not have Acanthosis Nigricans, Asians (who were predominantly Filipino) were selected as the reference group for regression models. Underweight and overweight children were excluded from the models, and obese children were compared to healthy weight children. An interaction term was included to determine if race/ethnicity modified the obesity–AN relationship. Statistical analysis was done using SAS (SAS Institute Inc., Cary, NC).
2.4. Human studies
Human studies approval was obtained from the Committee on Human Studies at the University of Hawaii at Manoa and the Institutional Review Board (IRB) at the University of Guam. All other participating jurisdictions ceded IRB approval to the University of Hawaii at Manoa. Parents consented and children assented to participate. Participants received $20 for participation in most locations. In Guam and Alaska, remuneration was increased to $40 and $50, respectively.
3. Results
Demographic characteristics of participants by child's sex, age, race/ethnicity and jurisdictions are given in Table 1.
3.1. Overall prevalence
The USAP regional prevalence of obesity was 14.0% (standard error [SE] = 0.9%), overweight was 14.4% (SE 1.0%), healthy weight was 68.9% (SE 1.4%), and underweight was 2.6% (SE 0.3%). Significant differences were observed between males and females (P < 0.001), with prevalence of obesity of 16.3% (SE 1.2%) for males children and 1.6% (SE 0.8%) for females. Obesity prevalence also differed significantly by age group (P = 0.009), with 12.9% (SE 0.9%) in the 2 to 5 years old and 16.3% (SE 1.3%) in the 6 to 8 years old.
The prevalence of AN was 4.7% overall (SE 0.9%), and did not vary by sex (P = 0.98) but varied by age (P = 0.001). 2 to 5 years old children had an AN prevalence of 3.5% (SE 0.8%) and 6 to 8 years children 6.8% (SE 1.1%). Of the 217 children with AN, 60.3% (SE 3.1%) had an AN score of 1, 20.8% (SE 2.7%) a score of 2, 12.2% (SE 2.2%) a score of 3, and 6.8% (SE 2.2%) a score of 4. There was a significant difference in the distribution of AN scores between the Prevalence study jurisdictions and Intervention study jurisdictions (6.4% [SE 0.8] and 4.0% [SE 1.1], P = 0.01, respectively). Seventy-four percent (SE 4.1%) of children with AN from the Prevalence Study Jurisdictions had scores of 1, or were less severe cases, whereas in Intervention study jurisdictions, only 51% (SE 5.3%) had a score of 1.
3.2. Prevalence of Obesity and AN by Jurisdiction
Significant differences were observed in both the prevalence of obesity (P < 0.0001) and AN by jurisdiction (P < 0.0001, Fig. 1). Prevalence of obesity was highest in American Samoa (21.7%; SE 1.4%) and absent in the RMI. Prevalence of AN was highest in Pohnpei (11.9%; SE 4.1%) and absent in Alaska.
Figure 1.
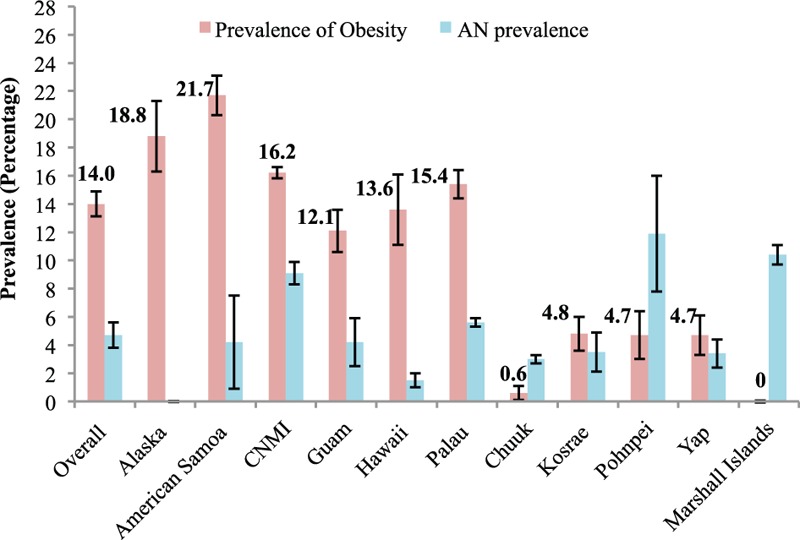
Weighted prevalence of obesity and acanthosis nigricans (AN) in the United States Affiliated Pacific Jurisdictions. AN = acanthosis nigricans.
3.3. Prevalence of Obesity and AN by Race/Ethnicity
Among OMB race categories, there was a significant difference in the prevalence of AN (P = 0.0004) but not obesity (P = 0.18). The prevalence of obesity by OMB race was 26.4% (SE 2.1%) among AIANs, 16.6% (SE 1.1) among Asians, 13.4% (SE 5.6%) among Blacks, 13.9% (SE 1.5%) among those of >1 race, 13.6% (SE 1.0%) among NHPIs, and 9.3% (SE 2.5%) among Whites. The prevalence of AN by OMB race was 9.4% (SE 0.9%) among Asians, 5.6% (SE 1.3%) among NHPIs, 2.6% (SE 0.7%) among those of >1 race, and 0% among AIANs, Blacks, and Whites (Fig. 2).
Figure 2.
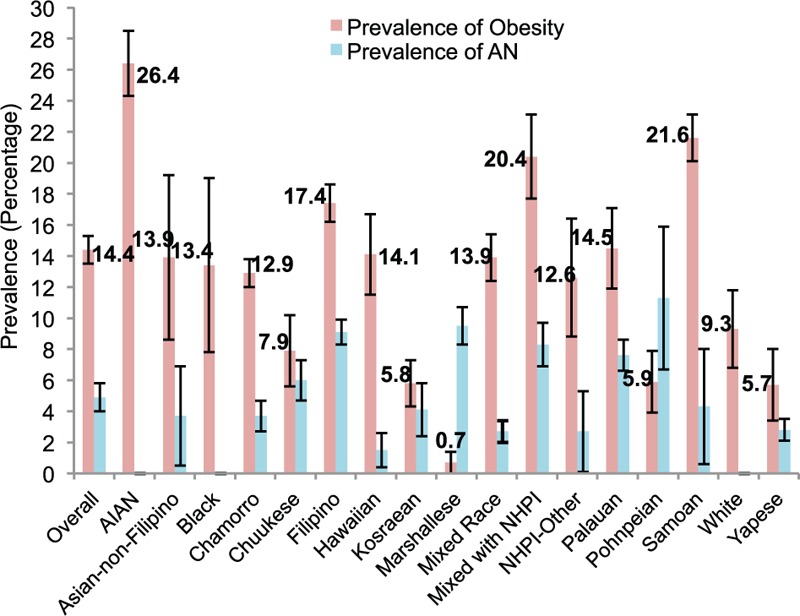
Weighted prevalence of obesity and acanthosis nigricans (AN) by Pacific Race. AN = acanthosis nigricans.
Significant differences were observed in the prevalence of obesity (P < 0.0001) and AN (P < 0.0001) among Pacific race/ethnic groups. Prevalence of obesity was highest among AIANs (26.4%, SE 2.1%), followed by Samoans (21.6%, SE 1.5%), >1 NHPI ethnicity (20.4%, SE 2.7%), and Filipino (17.4%, SE 1.2%). Obesity was lowest among Marshallese (0.7%, SE 0.7%), Yapese (5.7%, SE 2.3%), Kosraean (5.8%, SE 1.5%), and Pohnpeian (5.9%, SE 2.0%). Prevalence of AN was highest among Pohnpeian (11.3%, SE 4.6%), Marshallese (9.5%, SE 1.2%), Filipino (9.1%, SE 0.8%), and >1 NHPI ethnicity (8.3%, SE 1.4%). AN was absent among AIANs, Blacks, and Whites.
3.4. Obesity—AN Relationship
Figure 3 compared prevalence of AN between obese and healthy weight children, overall, and by race/ethnic groups, using the Pacific definition. The prevalence of AN among all healthy weight children was 2.2% (SE 0.05%) and among all obese children was 7.8% (1.9% SE) (Fig. 3). With 1 exception (Marshallese), all race/ethnic groups where AN occurred exhibited a higher prevalence of AN among the obese compared to the healthy weight children. The obese were 3.5-fold more likely to have AN than the healthy weight children overall; however, AN was 10-fold more likely among the obese than healthy weight children for the following race/ethnic groups: Chuukese (11-fold); Palauan (18-fold); Kosraean (25-fold); Filipino (30-fold); Chamorro (214-fold); and among Native Hawaiian, NHPI-Other and Yapese AN only occurred in obese, making the ratio infinity. The highest prevalence of AN among obese children was observed for Pohnpeians at 46.2% (SE 16.2%), followed by Filipinos at 44.7% (SE 3.3%), Chuukese at 39.4% (SE 5.7%), Kosraen at 38.9% (SE 5.3%), Yapese at 38.2% (SE 12.0%), Palauan at 34.7% (SE 0.5%), and Chamorro at 27.9% (SE 9.6%). Among Marshallese, the healthy weight children had a high prevalence of AN, at 9.4% (SE 2.0%), although the 1 obese child (who did not live in the Marshall Islands) did not have AN.
Figure 3.
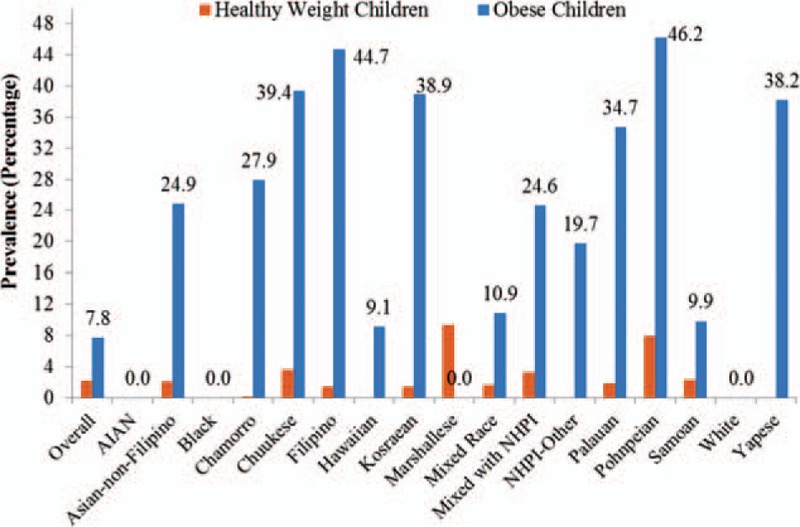
Weighted unadjusted prevalence of acanthosis nigricans (AN) comparing obese to healthy weight children. AN = acanthosis nigricans.
Logistic regression models of AN were fit with the following independent variables: sex, age group (6–8 vs 2–5), obesity (obese vs healthy weight), race/ethnicity, and an interaction between obesity and race/ethnicity (Supplemental Tables 4 and 5). Two models were run: one used the OMB race classification and another used the Pacific race/ethnicity classification. Race/ethnicity, using either definition, was a significant moderator of the relationship between obesity and AN (P's for interaction < 0.001). The older age group (6–8 years) was more likely to have AN than the younger age group (2–5 years) (ORs of 1.5 to 2.0, P's < 0.05). There was no difference in AN risk between males and females (P = 0.34). Obese Asian, NHPI, and >1 race group children were at significantly higher risk of AN compared to healthy weight children. There was a positive association between obesity and AN for Asian and most NHPI race/ethnic groups, and null associations between obesity and AN for other race/ethnic groups.
4. Discussion
Prevalence of obesity based on CHL standardized measurements was similar to that found in meta-analysis of published data (CHL vs meta-analysis, respectively: 14.0% vs 14.1% for 2 to 8 years old; 9.2% vs 10.0% at 2 years old, and 24.4% vs 23.2% at 8 years old).[5] An increase occurred between ages 4 to 5 years and 6 to 11 years. Obesity and older age were positively associated with acanthosis nigricans. AN among 6 to 8 years old was twice that of 2 to 5 years old, foretelling an even higher prevalence of AN in adolescence.
The USAP is characterized by many Asian and Pacific race/ethnicities, race/ethnic mixtures, and migration among the islands, confounding race/ethnic, and jurisdiction differences in obesity and AN. Race/ethnicity modified the relationship between obesity and AN. Methods for studying race/ethnic mixtures will continue to require attention as populations become increasingly mixed.
Obesity was highest among children in the American Samoa jurisdiction (21.7%), the highest among nonmixed Pacific Islander race/ethnic groups, and consistent with results of the meta-analysis[5] and those of Shabbir et al[18] that reported that Samoans had the highest prevalence of obesity among Asian/Pacific Islander (API) racial groups in the 5th, 7th, and 9th grades in Los Angeles County, CA. AN was lower than expected given the high rate of obesity.
In total 18.8% of 2 to 8 years old children in Alaska were classified as obese, lower than surveillance data from the Pregnancy Risk Assessment Monitoring System (PRAMS) and Childhood Understanding Behaviors Survey (CUBS) where 24.9% of Alaskan 3 year olds were obese and 42.2% of Alaska Native children were obese,[19] respectively. CHL recruited from 4 of the largest urban centers in Alaska, whereas PRAMS and CUBS were statewide and included smaller, remote communities that have limited access to healthy foods and where intake of sugar-sweetened beverage is higher. The CHL Alaska sample was largely White, whereas Alaska Native children have a higher prevalence of obesity.[19] However, PRAMS and CUBS rely on self-report data that may underestimate height and may therefore overestimate obesity status.[20] Although the prevalence of obesity in Alaska was among the highest in the USAP, AN was absent.
CNMI was the third highest in the rate of obesity and AN in the study. A 2005 nutrition survey conducted on 420 children 0–10 years old found that 45% of 7–10 years old, 26% of 4 to 6 years old, and 25% of 2 to 3 years old were obese[21] and 9 cases of AN, which were only present in obese 8 to 10 years old.[22]
The prevalence of obesity in Hawaii (13.6%) was lower than other studies conducted in earlier years. In 2003, Stark et al[23] documented obesity prevalence was 7% for 2 to 3 years old, 20% for 4 to 5 years old, and 29% for 6 – 10 years old. In 2010, obesity prevalence among 5 to 8 years old was 19.7% in the same population.[24] Pobutsky et al[25] documented obesity in 4 to 5 years old public school children during school year 2002–2003 at 14.4%, lower than a smaller study conducted the same year that found obesity prevalence at 21.5% in 4 to 5 years old public school children.[26] These findings suggest that obesity prevalence is decreasing in young children in Hawaii, including among Native Hawaiians, or that measurement methodology influenced the height results.[20]
The prevalence of obesity among children on Guam was the lowest among CHL Intervention Study jurisdictions at 12.1% and lower than a recently published report by Paulino and colleagues[27] where prevalence of obesity was 14% among children ages 4 to 5 years and 23% among children ages 6 to 11 years. The higher rates from the Department of Education may also be due in part to less standard height measurements that tend to underestimate height.[20]
Obesity prevalence for the 4 states of the Federated States of Micronesia (FSM) were at least 4-fold lower than obesity rates found in American Samoa and >2-fold lower than those found in Hawaii. Prevalence of obesity was similar in Yap, Pohnpei, and Kosrae States (4.7–4.8%), but was especially low in Chuuk State (<1.0%). Palau showed obesity prevalence similar to Hawaii and CNMI. In the Marshall Islands, there were no obese children. The higher obesity rates in Palau may be related to higher income and a higher degree of acculturation to western lifestyle as reflected in a higher World Bank classification.[28] Although the prevalence of obesity of Palauan children living in Palau was similar to that of Palauan children living in other jurisdictions, the prevalence of obesity was higher for Chuukese, Yapese, Pohnpeian, and Kosreans living outside their home jurisdiction. The increase was especially prominent for the Chuukese children where the prevalence of obesity was < 1.0% for Chuukese children measured in Chuuk compared to almost 8% for Chuukese in all jurisdictions. Obesity for children in Yap, Pohnpei, and Kosrae States was slightly higher than what was reported in a 2010 report on the Maternal and Child Health Program in the FSM, where obesity prevalence ranged from 2% to 3%,[29] implying an increasing rate.
A limitation of this study is the measurement of AN across race/ethnic groups with differing skin color. The higher proportions of AN in the level 1 category in the Prevalence jurisdictions could be due to those populations having darker skin color or, alternatively, could reflect the emerging problem of AN despite lower obesity levels due to nutrition transition, reporting on racial/ethnic mixtures, or to other factors.
4.1. Interpretation
Despite the strong association of obesity and AN, the relatively high AN prevalence among Prevalence jurisdictions, despite lower but emerging rates of obesity, and the lower AN where obesity has been prevalent for a longer time suggests that AN may represent an important early indicator of nutrition transition and metabolic change. Given that rates of obesity and AN increase with age, the data foretell high rate of future diabetes, as is already found in the adult populations in the region. Further study is needed to determine which of the factors such as race/ethnicity, socio-economic status, diet, physical activity, skin color, or other, are contributing to AN in the USAP.
Supplementary Material
Footnotes
Abbreviations: AIAN = American Indian/Alaska Native, AN = acanthosis nigricans, API = Asian/Pacific Islander, BMI = body mass index, CHL = Children's Healthy Living Program, CNMI = Commonwealth of the Northern Mariana Islands, CUBS = Childhood Understanding Behaviors Survey, FSM = Federated States of Micronesia, NCD = noncommunicable diseases, NHPI = Native Hawaiians and Pacific Islanders, OMB = Office of Management and Budget, PRAMS = Pregnancy Risk Assessment Monitoring System, RMI = Republic of the Marshall Islands, SE = standard error, USAP = United States Affiliated Pacific.
Authorship: Fenfang Li had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. FL and LW conducted data analysis and are responsible for it.
Funding: The study was funded by the United States Department of Agriculture, National Institute of Food and Agriculture, Grant 2011-68001-30335. The authors would like to acknowledge and thank the CHL Team throughout the Pacific.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- 1.Dietz WH, Economos CD. Progress in the control of childhood obesity. Pediatrics 2015; 135:e559.originally published online. February 2015; DOI: 10. 1542/peds. 2014-2972. [DOI] [PubMed] [Google Scholar]
- 2.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr 2014; 168:561–566.doi:10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014; 311:806–814.doi:10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willett W. Nutritional Epidemiology. 3rd ednNew York, NY: Oxford University Press; 2013. [Google Scholar]
- 5.Novotny R, Fialkowski MK, Li F, et al. Prevalence of young child overweight and obesity in the United States Affiliated Pacific Region as compared to the 48 contiguous States: a systematic review and meta-regression by the children's healthy living program. Am J Public Health 2015; 105:e22–e35.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pacific Islands Health Officers Association Board Resolution #48-01. “Declaring a Regional State of Health Emergency Due to the Epidemic of Non-Communicable Diseases in the United States-Affiliated Pacific Islands” The Burden of NCDs. May 24, 2010. [Google Scholar]
- 7.Kutlubay Z, Burhan E. Acanthosis nigricans: a fold (intertriginous) dermatosis. Clin Derm 2015; 33:466–470.doi.org/10.1016/j.clindermatol.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Li F, Novotny R, Wilkens LW, et al. Anthropometric measurement standardization in the US-Affiliated Pacific: a Report from the Children's Healthy Living Program. Am J Hum Bio 2015; 28:364–371.DOI: 10.1002/ajhb.22796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilken[s] LR, Novotny R, Fialkowski MK, et al. Children's Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health 2013; 13:944.doi: 10.1186/1471-2458-13-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Economic Policy, Planning, and Statistics Office of the Republic of the Marshall Islands, 2012. Available at: http://www.eppso.org/#!other-links/c1b3i (accessed December 26, 2016). [Google Scholar]
- 11.Federated States of Micronesia, Division of Statistics, 2010. Available at: http://www.sboc.fm/index.php?id0=Vm0xMFlWbFdTbkpQVm1SU1lrVndVbFpyVWtKUFVUMDk (accessed December 26, 2015). [Google Scholar]
- 12.Republic of Palau, Office of Planning and Statistics, 2005. http://palaugov.org/executive-branch/ministries/finance/budgetandplanning/rop-statistical-yearbooks/ (accessed December 26, 2015). [Google Scholar]
- 13.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 14.A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years). Available at: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm (accessed January 30, 2016). [Google Scholar]
- 15.Burke JP, Hale DE, Hazuda HP, et al. A quantitative scale of acanthosis nigricans. Diabetes Care 1999; 22:1655–1659. [DOI] [PubMed] [Google Scholar]
- 16.Office of Management and Budget, Standards for the Classification of Federal Data on Race and Ethnicity, Directive 15, 1997. Available at: https://www.whitehouse.gov/omb/fedreg_notice_15/ (accessed December 26, 2015). [Google Scholar]
- 17.Kish L. Survey Sampling. New York: Wiley-Interscience; 1995. [Google Scholar]
- 18.Shabbir S, Kwan D, Wang MC, et al. Asians and Pacific Islanders and the growing childhood obesity epidemic. Ethn Dis 2010; 20:129–135. [PubMed] [Google Scholar]
- 19.Wojcicki JM, Young MB, Perham-Hester KA, et al. Risk factors for obesity at age 3 in Alaskan children, including the role of beverage consumption: results from Alaska PRAMS 2005-2006 and its three-year follow-up survey, CUBS, 2008–2009. PLoS One 2015; 10: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Esquivel M, Wellness Policy Implementation for child obesity prevention in Hawaii. UHM dissertation, 2014. [Google Scholar]
- 21.Paulino YC, Coleman P, Davison NH, et al. Nutritional characteristics and body mass index of children in the Commonwealth of the Northern Mariana Islands. J Am Dietet Assoc 2008; 108:2100–2104. [DOI] [PubMed] [Google Scholar]
- 22.Novotny R. Dietary Characteristics of Children in the CNMI: Final Report August 31, 2007. [Google Scholar]
- 23.Stark MJ, Niederhauser VP, Camacho JM, et al. The prevalence of overweight and obesity in children at a Health Maintenance Organization in Hawai’i. Hawaii Med J 2011; 70 Suppl 1:27–31. [PMC free article] [PubMed] [Google Scholar]
- 24.Novotny R, Oshiro C, Wilkens LR. Prevalence of childhood obesity among young multiethnic children from a health maintenance organization in Hawaii. Child Obes 2013; 9:35–42.doi: 10.1089/chi.2012.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pobutsky A, Bradbury E, Reyes-Salvail F, et al. Overweight and obesity among Hawai‘i children aged 4 to 5 years enrolled in public schools in 2007–2008 and comparison with a similar 2002–2003 cohort. Haw J Med Pub Health 2013; 72:7. [PMC free article] [PubMed] [Google Scholar]
- 26.Manea SJ. Overweight among Kauai first-graders. Hawaii Med J 2015; 64:244–245. [PubMed] [Google Scholar]
- 27.Paulino YC, Guerrero RT, Uncangco AA, et al. Overweight and obesity prevalence among public school children in Guam. J Health Care Poor Underserved 2015; 26 (2 suppl):53–62.doi: 10.1353/hpu.2015.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Bank. Available at: http://chartsbin.com/view/2438 (accessed July 16, 2016). [Google Scholar]
- 29.Federated States of Micronesia Maternal and Child Health Programs. MCH Program needs assessment for 2010–2015; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


