Abstract
The incidence and prevalence of chronic obstructive pulmonary disease (COPD) is associated with increasing age. Osteoarthritis is also a growing problem in the aging population, and total knee replacement (TKR) is a common surgical procedure for this population. An increasing number of COPD patients are receiving TKR, but few studies have examined the complications and outcomes after TKR in COPD patients. The purpose of this study was to investigate the complications, including mortality, wound infections, hospitalization readmission, pneumonia (PN), and cerebrovascular accidents (CVAs) in patients with COPD after receiving TKR.
The National Health Insurance operated by the government is a nationwide health care program with universal coverage in Taiwan. It covers approximately 99% of the total Taiwanese population of 23 million people. In this case–control study, we analyzed the longitudinally linked National Health Insurance Research Database, which consists of a cohort of 1,000,000 randomly selected enrollees retrospectively followed from 1996 to 2010. This study analyzed patients who underwent TKR surgery between January 1, 2004 and December 31, 2009 by identifying the International Classification of Diseases, Ninth Revision, Clinical Modification code. We separated patients into COPD and non-COPD groups. Five study outcomes and complications were measured after TKR, including mortality for 1 and 3 years, wound infections for 1 and 2 years, hospitalization readmission for 30 and 90 days, PN for 30 and 90 days, and CVAs.
A total of 3431 patients who underwent TKR surgery were identified, including 358 patients with COPD and 3073 patients without COPD. The COPD group had a higher percentage of 90-day PN (3.7% vs. 1.1%), 30-day readmission (7.0% vs. 4.0%), 30-day CVA (1.7% vs. 0.6%), 90-day CVA (3.9% vs. 2.1%), and 3-year mortality (3.9% vs. 2.1%) than the non-COPD group. COPD was associated with 90-day PN (adjusted hazard ratio[HR)] = 2.12, P = 0.030) after adjusting for sex, cardiovascular disease, and CVA occurrence.
Patients with COPD had a higher risk of PN after TKR than patients without COPD, but no significant differences were found for CVAs and mortality.
Keywords: chronic obstructive pulmonary disease, total knee replacement
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic lung disease that produces airway obstruction and is not fully reversible after treatment with medication.[1] Patients with COPD have higher rates of complications after surgery than the general population.[2–4]
Osteoarthritis is also called degenerative arthritis and is a common form of arthritis that is commonly observed in older people. Osteoarthritis results from cartilage degeneration and the breakdown of joint cartilage and the underlying bone and exhibits associated symptoms of joint swelling, pain, and decreased range of motion; it causes a considerable socioeconomic burden worldwide.[5] The age-associated increase in the prevalence of COPD suggests that osteoarthritis is an increasing problem in this population.
Total knee replacement (TKR) is a common surgical procedure for osteoarthritis, rheumatoid arthritis (RA), systemic lupus erythematosus, and psoriatic arthritis.[6,7] TKR may produce a higher risk and more postoperative complications in patients with advanced diseases that involve severe joint destruction and deformity. Bozic et al[8] showed that the most significant independent risk factor for revision TKR within 12 months was COPD. Courtney et al[9] found that COPD is a risk factor that was predictive of critical care intervention after TKR. Courtney et al[10] also retrospectively reviewed 1012 consecutive patients undergoing elective primary hip and knee arthroplasties and found that COPD is a risk factor for developing late (>24 hours) complications after operation. An increasing number of COPD patients are undergoing TKR, and it is important to examine the complications and outcomes after TKR in COPD patients. The aim of our study was to investigate complications including mortality, wound infections, hospitalization readmission, pneumonia (PN), and cerebrovascular accidents (CVAs) in patients with and without COPD who undergo TKR by analyzing a nationwide database.
2. Methods
2.1. Ethics statement
This retrospective study was approved by the institutional review board (IRB) of the Chi Mei Medical Center, Taiwan (IRB no. 10504-E01). Consent was specifically waived by the approving IRB because all personal identifying information was removed from the dataset, and strict anonymity was maintained before further analysis.
2.2. Data sources
The National Health Insurance (NHI), operated by the government since 1995, is a nationwide health care program with universal coverage in Taiwan. The NHI is a single-payer insurance plan that covers approximately 99% of the total Taiwanese population of 23 million people and contracts with 97% of the healthcare providers.[11] The NHI Research Database (NHIRD), one of the largest administrative health care databases in the world, was released for research purposes. It contains all inpatient and outpatient registration and claims data of the NHI program, including demographic characteristics of patients, disease-diagnostic and surgery-operation codes (based on the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]), prescription records, and medical expenditures. In this study, we analyzed the longitudinally linked NHIRD data, which consisted of a cohort of 1,000,000 randomly selected enrollees retrospectively followed from 1996 to 2010.
2.3. Design and study participants
This study was designed as a population-based, longitudinal cohort study to retrospectively analyze patients who underwent TKR surgery by identifying cases in which the TKR was listed as the major procedure in the NHIRD database between January 1, 2004 and December 31, 2009 in Taiwan. In total, 3563 patients who underwent TKR surgery were preliminarily retrieved from 1,000,000 random samples of the NHIRD database (Fig. 1). We excluded patients who were younger than 40 years and those diagnosed with cancers before the TKR surgery. After exclusion filtering, total of 3431 patients remained in our study. To analyze the complications of TKR patients with a COPD history, the patients were separated into COPD and non-COPD groups (358 and 3073 patients separately) by using diagnostic codes ICD-9-CM to identify COPD patients 2 years before the TKR surgery according to their inpatient and outpatient records. The admission date for TKR surgery was designated as the index date.
Figure 1.
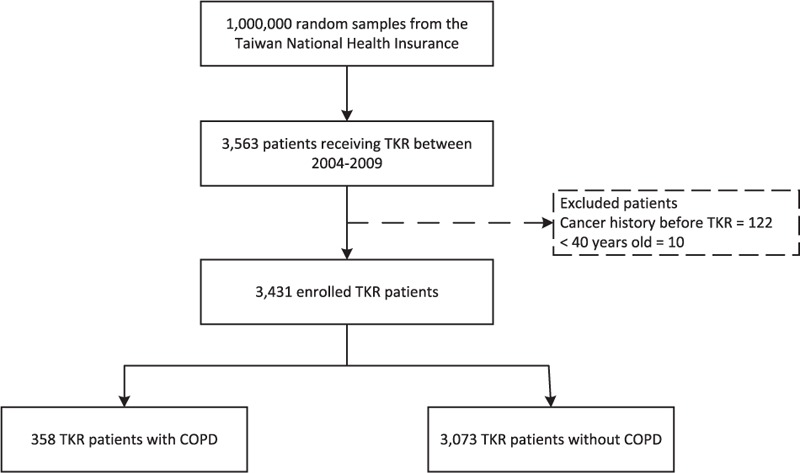
Flow chart of the patients included in the study. COPD = chronic obstructive pulmonary disease, TKR = total knee replacement.
2.4. Confounders
Patient characteristics and comorbidities were considered as confounders in our study. Characteristics included age, sex, and length of stay (LOS) in hospital for TKR surgery. To examining comorbidities, each patient was traced back from 2 years to the index date, which included cardiovascular disease (CVD), CVAs, chronic kidney disease (CKD), diabetes mellitus (DM), and RA.
2.5. Outcomes and complications
Five outcomes and complications were expected after TKR in COPD patients, including mortality for 1 and 3 years, wound infections for 1 and 2 years, hospitalization readmission for 30 and 90 days, PN for 30 and 90 days, and CVA for 30 and 90 days.
2.6. Statistical analysis
Continuous variables are presented as means (with standard deviations [SDs]), and discrete variables are expressed as frequencies and percentages. Demographic and comorbidity variables for the COPD and non-COPD groups were analyzed using χ2 tests and Student t test. Owing to the non-normal distribution of the LOS variable, a Mann–Whitney U test was performed to examine the significance. Statistical significance was indicated by a 2-sided P value of <0.05. Univariate analyses were performed using the Kaplan–Meier estimator with significance determined by the log-rank test to compare the survival function of complications and outcomes for patients who received TKR among variables such as COPD status, comorbidities, and demographic variables. To investigate the main effect of COPD that was associated with complications and outcomes, Cox proportional hazards regression analysis was conducted by controlling the significant characteristics identified in the univariate tests and estimating the hazard ratios (HRs) and 95% confidence intervals (CIs). In the sensitivity analysis, we conducted separate regression analysis among different age subgroups (using 65, 70, 75, and 80 years as cutoffs) to determine how ages affected our findings. All statistical analyses were performed by using SPSS software (version 15, SPSS Inc., Chicago, IL).
3. Results
3.1. Characteristics
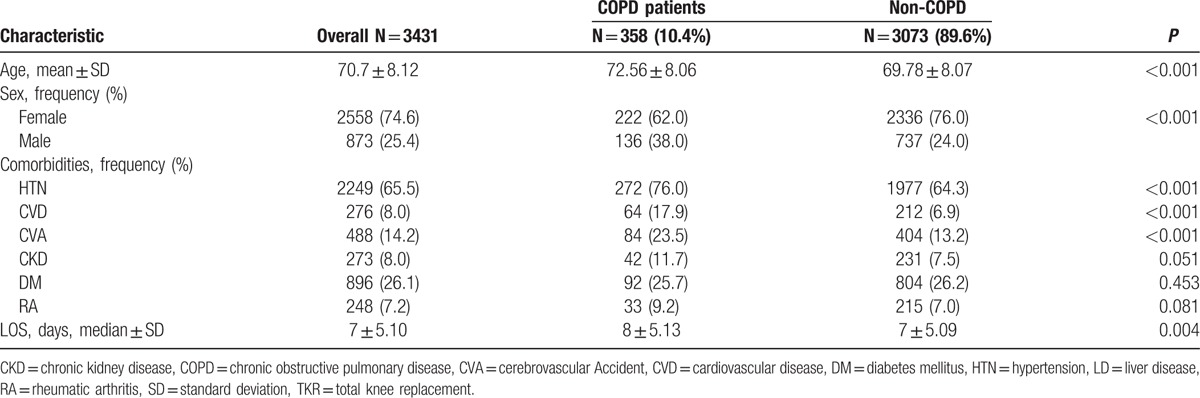
A total of 3431 qualified patients who underwent TKR surgery were identified in this study. The mean (SD) age was 70.1 ( ± 8.4) years and 74.6% were female. The average LOS was 8.4 ( ± 5.4) days. The study group consisted of 358 TKR patients with COPD, and the control group consisted of 3073 TKR patients without COPD. The comparisons of basic characteristics between these 2 groups (COPD vs. non-COPD) for patients who received TKR are shown in Table 1. Patients in the COPD group were significantly older than those in the non-COPD group (72.56 vs. 69.78 years). In addition, the COPD group had a smaller proportion of women (62.0% vs. 76.0%) and a higher prevalence of comorbidities (hypertension [HTN] [76.0% vs. 64.3%], CVD [17.9% vs. 6.9%], CVA [23.5% vs. 13.2%], CKD [11.7% vs. 7.5%]) than the non-COPD group. Patients in the COPD group also had a significantly longer LOS in hospitals (median 8 vs. 7 days).
Table 1.
Demographics of patients with/without COPD who underwent TKR.
3.2. Univariate analysis
To find complications in patients with and without COPD who undergo TKR, the comparisons among 2 groups are listed in Table 2. The COPD group had a higher percentage of 90-day PN (3.7% vs. 1.1%), 30-day readmission (7.0% vs. 4.0%), 30-day CVA (1.7% vs. 0.6%), 90-day CVA (3.9% vs. 2.1%), and 3-year mortality (3.9% vs. 2.1%) than the non-COPD group. In addition, possible risk factors for complications including age, sex, and 5 types of comorbidities were examined. Age was correlated with 90-day CVA incidence. Interestingly, sex was associated with most complications except for 1-year mortality. In terms of comorbidities, CVD exhibited a greater association with outcome variables including 90-day PN, 30-day readmission, 90-day readmission, 30-day CVA, 1-year mortality, and 3-year mortality. The cumulative incidence curves for the COPD and non-COPD groups are shown in Figure 2. The log-rank test for 90-day PN and 30-day readmission indicated significant differences in the complication risks between the COPD and non-COPD groups, and the cumulative incidence curves showed that the COPD group exhibited significantly higher incidence rates than the non-COPD group.
Table 2.
Univariate analysis for risk factors of complications following TKR.
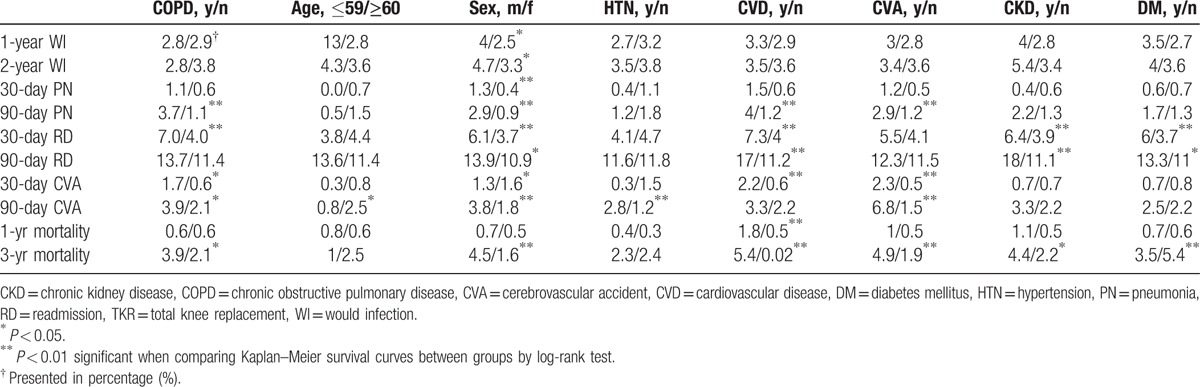
Figure 2.
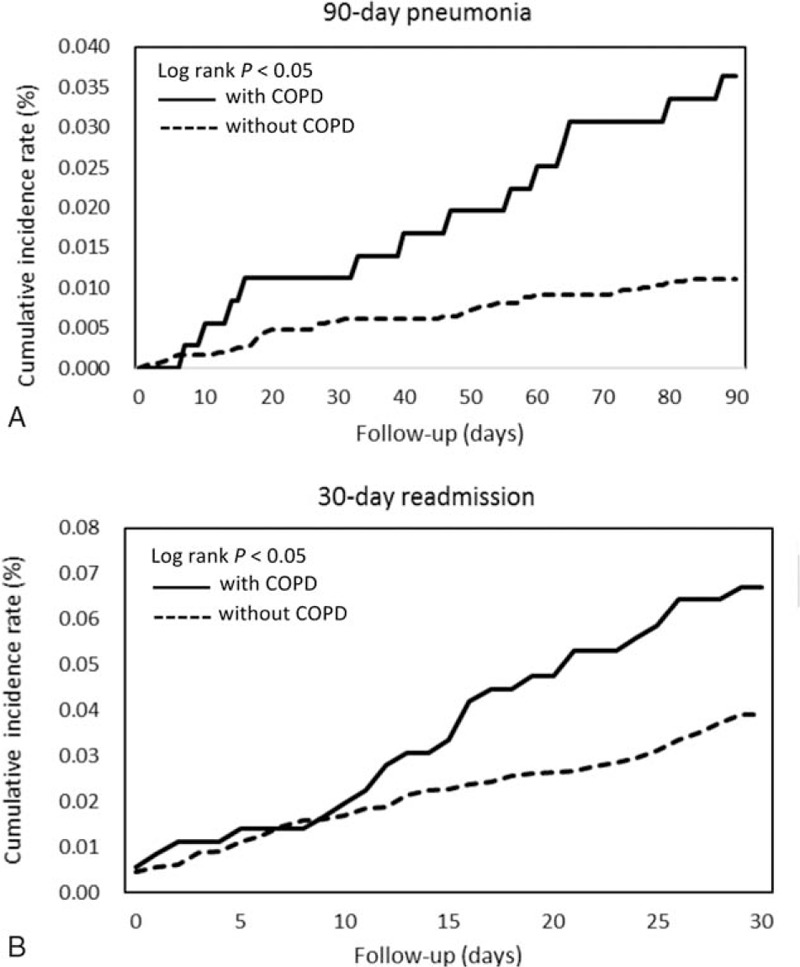
Cumulative incidence rates of complications including (A) 90-day pneumonia and (B) 30-day readmission in COPD patients and non-COPD patients after receiving total knee replacement. The log-rank test demonstrated significant differences in complication risks between the two groups. The cumulative incidence curves show that patients with COPD had a higher incidence rate than those without COPD. COPD = chronic obstructive pulmonary disease.
3.3. Multivariate analysis
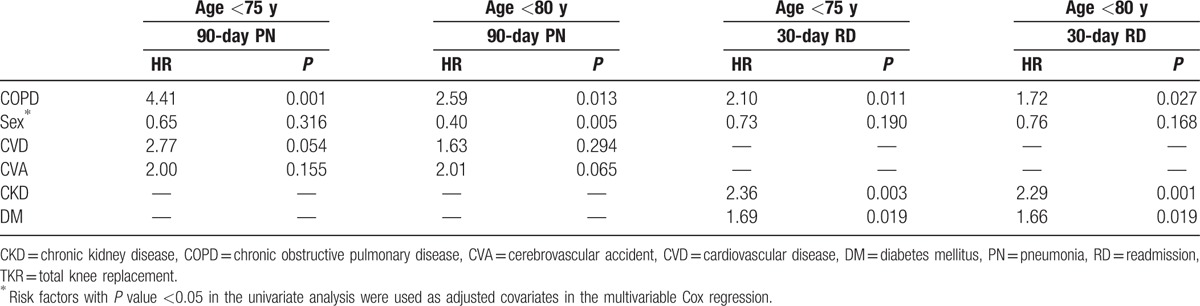
To estimate the unbiased complication risks associated with COPD in patients who received TKR, a multivariate Cox regression analysis was conducted by adjusting for the interference effects owing to the comorbidity and demographic variables that were found to be significant in the univariate analysis (Table 3). The analysis demonstrated that COPD was associated with 90-day PN (adjusted HR = 2.12, P = 0.030) after adjusting for sex, CVD, and CVA. The adjusted HR of 30-day readmission was 1.63 (P = 0.028) for the COPD group compared to the non-COPD group after adjusting for sex, CKD, and DM. Otherwise, no significant associations with COPD were found for 30-day CVA, 90-day CVA, and 3-year mortality after controlling for risk covariates. In the sensitivity analysis (Table 4), the Cox proportional hazard regression was conducted in different age subgroups. For patients’ age <75 years, the adjusted HR of 90-day PN was 4.41 (P = 0.001) and the adjusted HR of 30-day readmission was 2.10 (P = 0.011) indicated COPD patients in this subgroups were more associated with complication risks.
Table 3.
Multivariable analysis by Cox regression of complications following TKR.
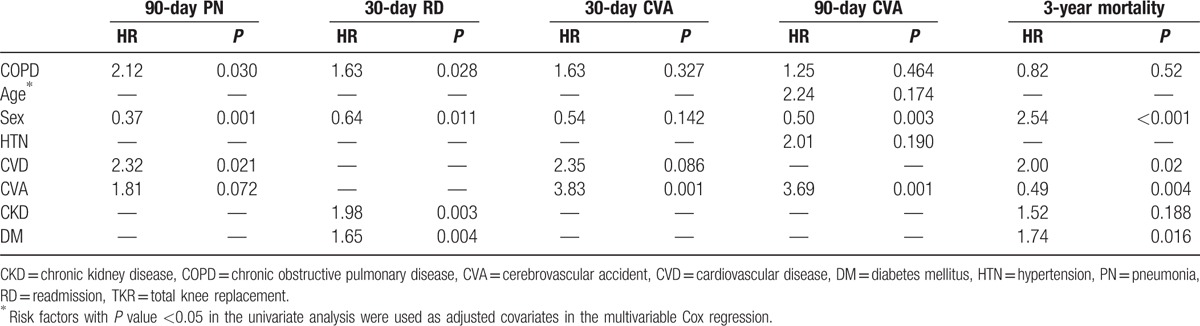
Table 4.
Sensitivity analysis by Cox regression of complications following TKR.
4. Discussion
The prevalence of COPD increases with age, along with a steadily increasing incidence of osteoarthritis. It is important to evaluate whether patients with COPD have an increased risk of complications after undergoing TKR. The complications in this study were measured after the index date and show the complications in patients with COPD after TKR. Our study demonstrated that patients with COPD who underwent TKR had increased risks of 30-day readmission and 30-day CVA, but no differences were found for 90-day readmission and 1-year mortality compared to patients without COPD.
In our study, the average age of COPD patients when they underwent TKR was 72.56 years, which is younger than the average age (75.88 years) at which COPD patients received total hip replacement (THR) in our previous study. Similar to previous studies, most patients who received TKR, regardless of COPD status, were older than 60 years and were predominantly women.[12,13] In our study, HTN was the most common comorbidity in both groups. Compared to patients without COPD, patients with COPD had a higher prevalence of HTN, CVD, and CVA. This phenomenon was also observed in patients with and without COPD who received THR in our previous study. According to previous studies, the common comorbidities in patients undergoing TKR include COPD, diabetes, CVD, and CVA, but few of these studies have considered their impact on the prognosis after TKR.[12–15] Our study focused on the impact of COPD on the prognosis of TKR. The effect of comorbid illness on mortality and prognosis needs to be further investigated.
A retrospective study in the Medicare Patient Safety Monitoring System showed a trend toward a decreased LOS after TKA from 4.1 days between 2002 and 2004 to 3.8 days between 2005 and 2007 in 4057 TKA patients.[14] Another study reviewed patients with TKR performed between April 2001 and December 2004 and excluded patients with an American Society of Anesthesiologists score of ≥3 or with perioperative complications and showed a LOS of 3.6 days.[16] Husted et al[17] surveyed 1731 patients who underwent TKR or total hip arthroplasty in a well-described, standardized, fast-track setup from 2004 to 2008 and found a LOS of 4.6 to 3.1 days. In our study, the LOS in COPD patients was 8 days, and that in non-COPD patients was 7 days. Some factors contributed to a longer LOS in our study than in other studies. First, the population of our study consisted of older adults with more comorbidities. Second, we included primary TKR and cases of revision, whereas previous studies only included primary TKR and excluded revision TKR. Third, previous studies excluded high-risk populations such as those with an American Society of Anesthesiologists score of ≥3 or those with perioperative complications. Fourth, implementation of a fast-track perioperative program that provides the best possible evidence-based treatment during hospitalization reduces the LOS in other countries. In Taiwan, no fast-track program exists,[18,19] and patients receive rehabilitation in the hospital rather than home-based rehabilitation.
In our study, the 30-day readmission rate was 4% in the non-COPD group and 7% in the COPD group. Bini et al[16] reviewed 90-day readmission rates for 9150 patients who underwent primary TKR or THR between April 2001 and December 2004 and excluded the high-risk population; the readmission rate was 3.5%. Vorhies et al[14] retrospectively reviewed 4057 Medicare TKA patients from 2002 to 2007 and found a 30-day readmission rate of 5.6%. Our non-COPD group had a similar readmission rate as in these studies, but the COPD group had a higher readmission rate than the general population. According to our previous study, patients with COPD also had a higher 30-day readmission rate after THR than the general population.[20] Patients with COPD were more likely to have comorbidities and multiple comorbidities than patients without COPD, and this may explain the higher rate of readmission. Our study findings are a reminder to clinicians and caregivers that patients with COPD have a high readmission rate after TKR and that additional close monitoring and follow-up may be important in this population.
Although the number of cases in the present study was small, it seemed that patients with COPD had a higher risk of CVA after TKR than the non-COPD patient group. An important risk factor for CVA is cigarette smoking, and this is also risk factor for COPD. Otherwise, COPD is a systemic inflammatory disease, and increased inflammation is a plausible explanation for CVAs.[21] COPD patients have a higher risk of developing neuronal damage because of hypoxia or associated comorbidities, and aging along with low brain perfusion contributes to cerebral damage.[22] The effects of inflammation, aging, and comorbidities such as diabetes, HTN, and hypoxia may be synergistic to CVAs, but the underlying mechanisms require further elucidation. It is necessary to pay attention to CVAs in COPD patients after TKR. Patients with COPD had a higher risk of developing PN after TKR than patients without COPD. COPD is a risk factor for the development of PN, and previous studies of PN have shown that COPD is a frequent comorbidity. Because PN is more common when the immunity of lung is already weakened and immune system does not work properly.[23]
There are some limitations of our study. First, no laboratory data, including pulmonary function, were present in the database, and the disease severity could not be evaluated in the COPD population. Because this was a nationwide study, our study group represents the distribution of COPD in an Asian population in clinical practice. The study showed complications after TKR in the general COPD population regardless of disease severity. Second, the accuracy of NHI claims data for COPD is debatable. Previous studies have validated the diagnosis accuracy in the NHIRD, and it appears to be a valid database for population research.[24,25] Third, this is a retrospective study, and TKR treatment was conducted by different surgeons and hospitals. Nuances in the surgical procedure and variations in the postoperative care plan were present. Fourth, the diagnoses of COPD were identified on the basis of ICD-9-CM codes and were not validated using pulmonary function test. Although COPD was defined by ≧3 outpatient or ≧1 discharge claims records with COPD, the possibility of misdiagnosis still exists. Otherwise, we described complications occur after surgery. There are many factors associated with these complications and other aspects of etiology cannot be ruled out in our retrospective study. Several factors might have affected the occurrence of complications, such as severity of COPD and osteoporosis, surgeon experience and surgeon volume, postoperative care, rehabilitation program, and level of hospital. A prospective study with a standardized treatment protocol for each TKR patient with COPD is warranted for further evaluation. An investigation of the relationship between COPD severity and complications after TKR is also needed.
5. Conclusion
This is a nationwide study of a large number of patients that compared complications after TKR in patients with and without COPD. Patients with COPD had a higher risk of PN after TKR than patients without COPD, but no significant differences were found for CVAs and mortality. We believe that the study provides valuable information about the complications of TKR in patients with COPD.
Acknowledgments
The authors express their sincere gratitude to Mr. Zhe-Wei Xu (Department of Industrial Engineering and Management, National Yunlin University of Science and Technology) for his effort in organizing data and assisting statistical analysis.
Footnotes
Abbreviations: CI = confidence interval, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVA = cerebrovascular accident, CVD = cardiovascular disease, DM = diabetes mellitus, HR = hazard ratio, LHID = Longitudinal Health Insurance Database, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, SD = standard deviation, TKR = total knee replacement.
The authors report no conflicts of interest.
References
- 1.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: gold executive summary. Am J Respir Crit Care Med 2013; 187:347–365. [DOI] [PubMed] [Google Scholar]
- 2.Arozullah AM, Khuri SF, Henderson WG, et al. Participants in the National Veterans Affairs Surgical Quality Improvement Program. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847–857. [DOI] [PubMed] [Google Scholar]
- 3.Smetana GW. Preoperative pulmonary evaluation. N Engl J Med 1999; 340:937–944. [DOI] [PubMed] [Google Scholar]
- 4.Trayner E, Jr, Celli BR. Postoperative pulmonary complications. Med Clin North Am 2001; 85:1129–1139. [DOI] [PubMed] [Google Scholar]
- 5.Glyn-Jones S, Palmer AJ, Agricola R, et al. Osteoarthritis. Lancet 2015; 386:376–387. [DOI] [PubMed] [Google Scholar]
- 6.Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. part 2: Treatment approaches. Ann Intern Med 2000; 133:726–737. [DOI] [PubMed] [Google Scholar]
- 7.Issa K, Pierce TP, Scillia AJ, et al. Midterm outcomes following total knee arthroplasty in Lupus patients. J Arthroplasty 2016; 31:655–657. [DOI] [PubMed] [Google Scholar]
- 8.Bozic KJ, Lau E, Ong K, et al. Risk factors for early revision after primary TKA in Medicare patients. Clin Orthop Relat Res 2014; 472:232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Courtney PM, Melnic CM, Gutsche J, et al. Which patients need critical care intervention after total joint arthroplasty? a prospective study of factors associated with the need for intensive care following surgery. Bone Joint J 2015; 97-B:1512–1518. [DOI] [PubMed] [Google Scholar]
- 10.Courtney PM, Rozell JC, Melnic CM, et al. Who should not undergo short stay hip and knee arthroplasty? Risk factors associated with major medical complications following primary total joint arthroplasty. J Arthroplasty 2015; 30 (9 Suppl):1–4. [DOI] [PubMed] [Google Scholar]
- 11.Wu CC, Hsu TW, Chang CM, et al. Age-adjusted Charlson comorbidity index scores as predictor of survival in colorectal cancer patients who underwent surgical resection and chemoradiation. Medicine (Baltimore) 2015; 94:e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meding JB, Klay M, Healy A, et al. The prescreening history and physical in elective total joint arthroplasty. J Arthroplasty 2007; 22 (6 Suppl. 2):21–23. [DOI] [PubMed] [Google Scholar]
- 13.Huddleston JI, Maloney WJ, Wang Y, et al. Adverse events after total knee arthroplasty: a national Medicare study. J Arthroplasty 2009; 24 (6 Suppl):95–100. [DOI] [PubMed] [Google Scholar]
- 14.Vorhies JS, Wang Y, Herndon JH, et al. Decreased length of stay after TKA is not associated with increased readmission rates in a national Medicare sample. Clin Orthop Relat Res 2012; 470:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vorhies JS, Wang Y, Herndon J, et al. Readmission and length of stay after total hip arthroplasty in a national Medicare sample. J Arthroplasty 2011; 26 (6 Suppl):119–123. [DOI] [PubMed] [Google Scholar]
- 16.Bini SA, Fithian DC, Paxton LW, et al. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty 2010; 25:114–117. [DOI] [PubMed] [Google Scholar]
- 17.Husted H1, Otte KS, Kristensen BB, et al. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 2010; 130:1185–1191. [DOI] [PubMed] [Google Scholar]
- 18.Jørgensen CC, Petersen MA, Kehlet H. Lundbeck Foundation Centre for Fast-Track Hip and Knee Replacement Collaborative Group. Preoperative prediction of potentially preventable morbidity after fast-track hip and knee arthroplasty: a detailed descriptive cohort study. BMJ Open 2016; 6:e009813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl 2012; 83:1–39. [DOI] [PubMed] [Google Scholar]
- 20.Liao KM, Lu HY. A National analysis of complications following total hip replacement in patients with chronic obstructive pulmonary disease. Medicine (Baltimore) 2016; 95:e3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donaldson GC, Hurst JR, Smith CJ, et al. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest 2010; 137:1091–1097. [DOI] [PubMed] [Google Scholar]
- 22.Liao KM, Ho CH, Ko SC, et al. Increased risk of dementia in patients with chronic obstructive pulmonary disease. Medicine (Baltimore) 2015; 94:e930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Restrepo MI, Mortensen EM, Pugh JA, et al. COPD is associated with increased mortality in patients with community-acquired pneumonia. Eur Respir J 2006; 28:346–351. [DOI] [PubMed] [Google Scholar]
- 24.Lin CC, Lai MS, Syu CY, et al. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc 2005; 104:157–163. [PubMed] [Google Scholar]
- 25.Cheng CL, Lee CH, Chen PS, et al. Validation of acute myocardial infarction cases in the national health insurance research database in Taiwan. J Epidemiol 2014; 24:500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]


