Abstract
Duty hour regulations have been placed in residency programs to address mental health concerns and to improve wellness. Here, we elucidate the prevalence of depressive symptoms after implementing an overnight call shift system and the factors associated with burnout or depression among residents.
A sequential exploratory mixed methods study was conducted in a tertiary care pediatric and perinatal hospital in Tokyo, Japan. A total of 41 pediatric residents participated in the cross-sectional survey. We determined and compared the prevalence of depressive symptoms and the number of actual working hours before and after implementing the shift system. A follow-up focus-group interview with 4 residents was conducted to explore the factors that may trigger or prevent depression and burnout.
Mean working hours significantly decreased from 75.2 hours to 64.9 hours per week. Prevalence of depressive symptoms remained similar before and after implementation of the shift system. Emotional exhaustion and depersonalization from the burnout scale were markedly associated with depression. High workload, stress intolerance, interpersonal difficulties, and generation gaps regarding work–life balance could cause burnout. Stress tolerance, workload monitoring and balancing, appropriate supervision, and peer support could prevent burnout.
Although the overnight call shift system was effective in reducing working hours, its effectiveness in managing mental health issues among pediatric residents remains unclear. Resident wellness programs represent an additional strategy and they should be aimed at fostering peer support and improvement of resident–faculty interactions. Such an approach could be beneficial to the relationship between physicians of different generations with conflicting belief structures.
Keywords: burnout, depression, duty hours, pediatric residents, wellness
1. Introduction
Extended duty hours of resident physicians have been associated with negative consequences, including reduced patient safety and resident wellness.[1–2] Psychiatric disorders such as depression and burnout in overworked residents have been deemed as industrial accidents in recent years. In Japan, 23.3% of residents reportedly had depressive symptoms at the end of their training.[3] Furthermore, suicides among pediatricians as a result of overwork-related depression have been reported.[4]
According to the Japan Pediatric Society, the mean extra working hours of hospital pediatricians was approximately 80 hours per month, which is the certification criterion for karoshi (“death from overwork”).[5] In July 2003, the Accreditation Council for Graduate Medical Education (ACGME) enacted resident duty hour standards for all accredited programs to promote high-quality learning and safe care in teaching institutions in the United States.[6] Although a night-float (NF) system has been implemented to address duty hour limitations at many institutions in the United States, research has revealed contradictory results.
A systematic review investigating the impact of duty hour regulation on education for surgical residents showed a positive effect on their training. Conversely, another systematic review reported the negative impact of duty hour regulations for surgical residents on patient safety. A multi-institutional survey conducted on internal medicine residency programs in the United States found that job burnout and self-reported sleepiness in residents remained unchanged even after the implementation of duty hour regulations.[7,8,9] Furthermore, some researchers indicated that the NF system could disrupt basic biological functions, circadian rhythms, social relationships, and psychophysical health.[10]
There have been no debates regarding duty hour regulations for residents in Asian countries because of the lack of research into physician or resident wellness.[11] However, the need to improve the work–life balance of pediatricians by reducing duty hours is becoming a critical issue for the quality of medical care of children in Japan.[12] We implemented an overnight call shift (OCS) system in July 2011 to address the extended duty hours for pediatric residents in a pediatric hospital residency program in Japan. Compared with NF, the OCS system is considered to maintain physicians’ basic biological functions. In the traditional overnight call duty, residents are on-call after their usual day shift, resulting in some of them working for more than 30 consecutive hours. On the day of their OCS, residents get to take 8 hours off work after the morning round (Fig. 1).
Figure 1.
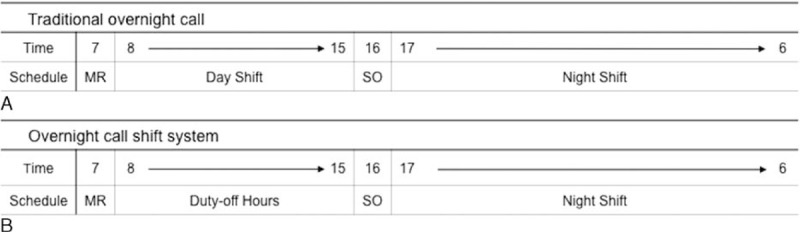
Time schedule of (A) traditional overnight call and (B) overnight call shift system. MR = morning round, SO = sign-out meeting.
2. Objectives
We conducted this study to describe and evaluate the mental health of our pediatric residents following the implementation of the OCS system. The primary outcome was to demonstrate the prevalence of depressive symptoms, the association between depression and burnout, and the change in working hours following the implementation of the OCS system. We also aimed to compare the prevalence of depressive symptoms and the number of working hours with the results of a preimplementation survey.[13] The secondary outcome was to explore the factors that could trigger or prevent burnout in residents, qualitatively.
3. Methods
3.1. Study setting and participants
The National Center for Child Health and Development (NCCHD) is a 490-bed tertiary care pediatric and perinatal hospital in Tokyo, Japan. The pediatric residency program is 3 years in duration and is approved by the Japan Pediatric Society. All applicants must have completed a mandatory 2-year rotation for postgraduate training under the supervision of the Ministry of Health, Labor, and Welfare.[14] The NCCHD pediatric residency program includes residents distributed across 3 postgraduate years with 10 to 15 residents per postgraduate year. Over the 3 years, residents have an overnight call duty once or twice a week during an 18-month pediatric ward rotation (8 months in the first year, 4 months in the second year, and 6 months in the third year).
3.2. Design
This was a sequential exploratory mixed methods study.[15] We started with a quantitative cross-sectional study to collect data on depression and burnout in pediatric residents, as well as their actual working hours after the implementation of the system, before conducting a qualitative focus-group interview of pediatric residents.
3.3. Quantitative data collection
We conducted a cross-sectional survey of pediatric residents at the NCCHD in October 2012. The anonymous survey included the questionnaires of the personal information, the Center for Epidemiologic Studies Depression Scale (CES-D), and the Maslach Burnout Inventory (MBI). We also investigated the actual working hours of pediatric residents. We did not assess prior mental health status of the participants because of the ethical aspect of it. The results were compared with those of a preimplementation survey conducted in October 2010, which also included results on the CES-D and working hours of pediatric residents. In that survey, 34 of the 36 (95% cooperation rate) pediatric residents at the NCCHD at that time completed their surveys.
3.4. Survey measurements
3.4.1. Center for epidemiologic studies depression scale (CES-D)
Residents were asked to complete the CES-D, a widely used self-report instrument designed to measure current depressive symptomatology in community populations. The 20-item CES-D assesses the frequency of symptoms during the past week on a 0–3 Likert-type scale (“rarely or never” to “most or all of the time”), with total scores ranging from 0 to 60. We used the Japanese version of the CES-D Scale. It has a sensitivity and specificity of 88.2% and 84.8%, respectively, at a cut-off level of 16 points.[16,17] An individual with a score of ≥16 was defined as positive for depressive symptoms.
3.4.2. Maslach burnout inventory (MBI)
We used the Japanese version of the MBI. Its reliability and validity have been confirmed previously.[18,19] The MBI comprises 17 items with 3 subscales, including emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA). The 5-point self-rated Likert scale includes responses for the magnitude of frequency (scored 1–5, ranging from “never” to “everyday”). Total scores per subscale were calculated by adding up the scores of each item.
3.4.3. Working hours of residents
The actual working hours of pediatric residents in September 2010 and September 2012 were determined through the self-enumeration working hours report. The actual working hours in a month of each resident was calculated as working hours per week.
3.5. Statistical analysis
We employed descriptive statistics to characterize participants by age, sex, marital status, and postgraduate year, calculating the frequencies and percentiles for variables. In tables, results are expressed as means ± SD and proportions for continuous and categorical variables, respectively. Continuous variables were compared by t-tests and categorical variables by χ2 and Fisher exact tests as appropriate. The significance level was set at P < 0.05. Data were analyzed using JMP 11 (SAS Institute Inc., Cary, NC).
3.6. Qualitative data collection
After completing an analysis of the quantitative study, a focus-group interview was conducted in September 2013 to obtain a qualitative perspective. Four pediatric residents (3 second-year residents and 1 third-year resident at the time of the interview; 2 men and 2 women) agreed to participate. We interviewed them in a private room at the hospital for approximately 60 minutes. The interview was audiotaped, and the tape was transcribed verbatim. Content analysis of the transcripts drew on grounded theory using a process of open, axial, and selective coding. The goal of the interview and of the analysis of the contents was to explore the contributory and protective factors for burnout in pediatric residents. In the open coding, 2 investigators independently read each transcript and identified themes, which were used to develop codes and analysis continued with each transcript, using a constant comparative approach. The codes were grouped into categories and the axial coding was used to examine the interrelationship of categories, including context, intervening conditions, and consequences.[20]
3.7. Ethical considerations
This study was approved by the ethics committee of the NCCHD. The cross-sectional quantitative survey was an anonymous questionnaire, and residents were informed that participation was not mandatory. To conduct the qualitative focus-group interview, consent from the participants was obtained in person by the interviewer.
4. Results
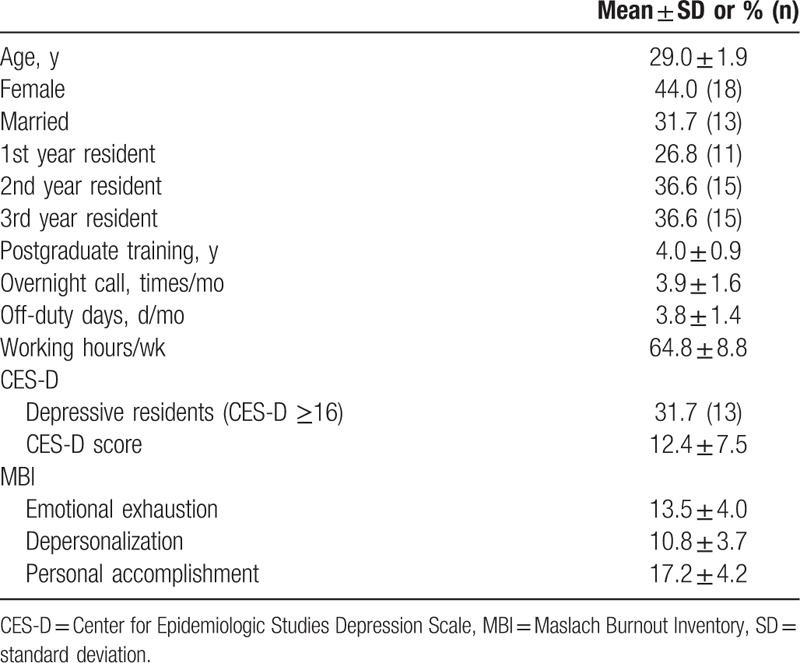
Of the 42 residents at the NCCHD who received an invitation to participate, 41 (98% cooperation rate) completed their surveys. Eleven (27%) were first-year residents, 15 (37%) were second-year residents, and 15 (37%) were third-year residents. The mean age of the study participants was 29 years; 32% were married and 44% were female. The mean frequencies of overnight call days and off-duty days were 3.9 times per month and 3.8 days per month, respectively. The mean working hours was 64.8 hours per week. The mean CES-D score was 12.4, and 16 residents (32%) had evidence of depressive symptoms with a score of 16 or more. In MBI, the mean EE score was 13.5, DP 10.8, and PA 17.2 (Table 1).
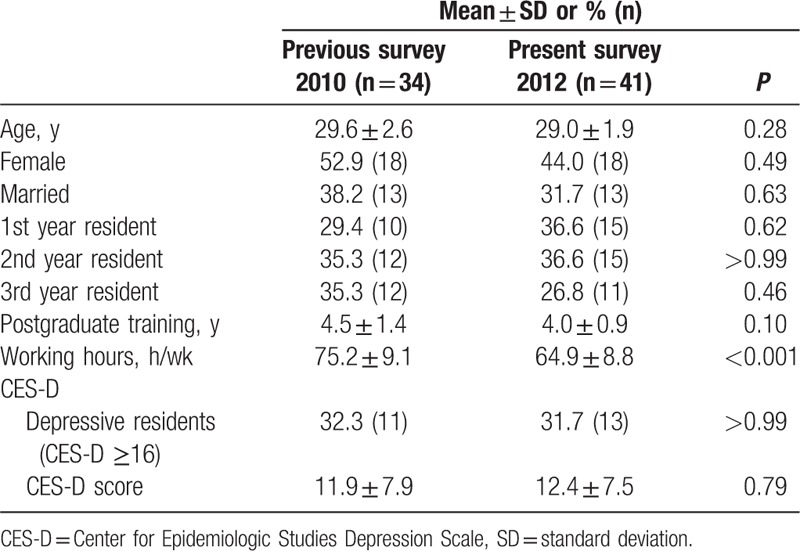
Table 1.
Participant characteristics (n = 41).
4.1. Depression
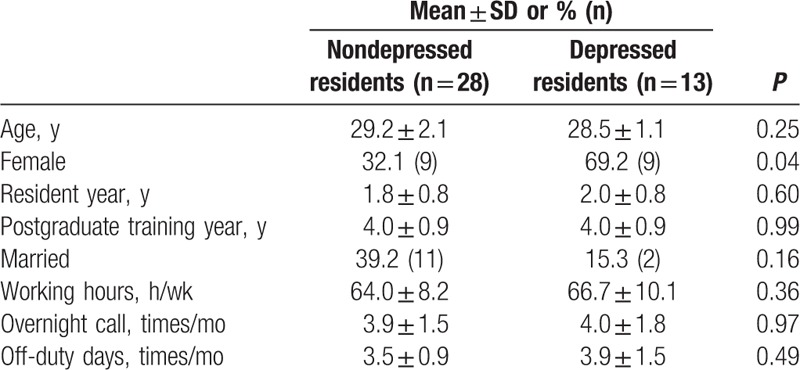
Table 2 describes the association of depressive symptoms with the demographic variables. The prevalence of depressive symptoms was significantly higher in female residents (62% vs 21%; P = .04). There was no statistical difference in age, resident year, postgraduate year, working hours, frequency of overnight call, and frequency of off-duty days between residents with depressive symptoms and those without depressive symptoms. Married residents were less likely to be depressed, although the difference was not statistically significant.
Table 2.
Comparison of characteristics between depressed and nondepressed residents.
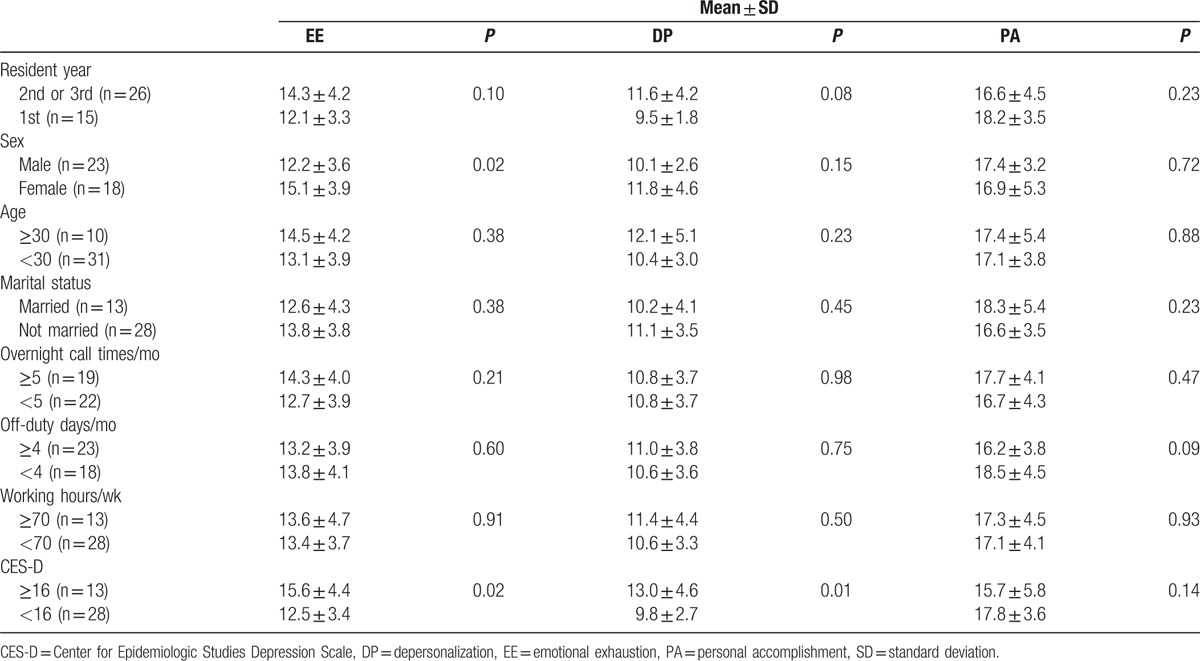
4.2. Burnout
Table 3 demonstrates the association of the MBI results with demographic variables. Women had significantly higher EE scores than men, but there were no differences for the DP and PA scores. In addition, after postgraduate year 5, residents had higher EE scores than those at 3 or 4 years. Both the EE and DP scores of residents with depressive symptoms (CES-D ≥16) were significantly higher than those without depressive symptoms (CES-D <16). No bivariate association was found between burnout subscales and other participants’ characteristics, including resident year, age, or marital status. Working conditions, such as frequency of overnight calls, frequency of off-duty days, and working hours, were not statistically associated with the MBI subscales.
Table 3.
Associations between participant characteristics, burnout scores, and depression scores.
4.3. Comparison survey
Table 4 shows a comparison of this survey with the results of our preimplementation study.[1] There were no significant differences in age, postgraduate year, sex, or marital status. Although mean working hours significantly decreased from 75.2 hours to 64.9 hours per week after the implementation of the OCS system, the prevalence of depressive symptoms was similar between the 2 study periods.
Table 4.
Comparison of the preimplementation survey with the present survey (preintervention to postintervention).
4.4. Focus-group interview
4.4.1. Identification of factors that could trigger burnout
We identified the following factors as having the potential to trigger burnout: a resident's stress tolerance, high workload, difficulty in interacting with patients’ parents and consultants, and generation gap on the perception of what constitutes an appropriate work–life balance for physicians.
4.4.2. Residents’ stress tolerance
Participants recognized that stress tolerance varied among individuals and that a person with low stress tolerance tended to burnout.
“It depends on the individual person whether a certain amount of workload exhausts them; that's what we call stress tolerance.”
4.4.3. High workload
Participants pointed out that shift working did not actually reduce their workload.
“We cannot eliminate our whole workload. We have to cover the work of duty-off residents. No doubt shift work allows us rest periods, but in reality we are always covering the work of duty-off residents.”
4.4.4. Difficulty in interacting with parents and consultants
Participants felt stressed when they had difficulty in interacting with patients’ parents and consultants.
“I tend to be stressed when having a difficult relationship with a patient's parents,”
and
“I sometimes feel stressed in paging consultants during the overnight call. Depending on who are the on-call consultants on the day, our stress varies a lot.”
4.4.5. Generation gap on the perception of what constitutes an appropriate work–life balance for physicians
Participants felt that there is a generation gap on the perception toward a physician's work–life balance between residents and attending physicians.
“Some attending physicians may not understand this kind of overnight call shift system and think that residents must work to exhaustion. They don’t say so to us directly, but might imply that ‘we work ourselves almost to death during residency’.”
4.4.6. Factors identified that could prevent burnout
We also identified the following factors that could prevent burnout: evaluation of each resident's stress tolerance, monitoring and balancing of each resident's workload, appropriate supervision of residents by attending physicians, and spontaneous peer support among residents.
4.4.7. Evaluation of each resident's stress tolerance
Participants noted that it was worth evaluating each resident's character and background that contributed to their stress tolerance.
“I think it is valuable to evaluate each resident's character or background at the beginning of residency.”
4.4.8. Monitoring and balancing of each resident's workload
Participants discussed the need to monitor and balance each resident's work to maintain equality.
“The overnight call shift system is not necessarily an adequate solution. In shift work, if a resident knocks off work leaving the work half done, the workload of other residents will increase. So, monitoring and balancing each resident's workload is essential.”
4.4.9. Appropriate supervision of residents by attending physicians
Participants expected attending physicians to provide appropriate supervision.
“I feel less stressed and more motivated to overcome challenges if we have attending physicians who provide advice for our troubles.”
4.4.10. Spontaneous peer support among residents
Participants became aware that spontaneous peer support among residents could prevent burnout.
“We care about each other and are sensitive to the possibility of a peer being burn out. Due to the circumstances, close bonds were spontaneously formed,”
and
“We heard that a few residents left our residency due to burnout several years ago. That's why we look after each other.”
5. Discussion
We conducted this study to assess the change of working hours and evaluate the mental health of our pediatric residents following the implementation of the OCS system. This study revealed that duty hour regulation was effective in reducing working hours of pediatric residents, but did not affect the prevalence of residents with depressive symptoms.
Our survey showed similar prevalence of certain depressive symptoms among pediatric residents compared with Western countries, where the prevalence was reported to be between 20% and 30%.[21] We also found an association between depressive symptoms and burnout, with the prevalence higher in female than male residents. These findings corroborate those of previous studies on medical trainees.[1]
Some reports revealed that depressive symptoms significantly decreased for men during residency, but remained high for women.[22] Goebert et al[23] noted that this might be related to the difficulties in succeeding in a traditionally male-dominated profession. Yasukawa et al[24] also suggested that women in Japanese medical schools and societies have historically been underrepresented in leadership positions, and that a significant proportion of Japanese women experienced gender-based discrimination. Moreover, the women themselves believed there were gender-based career obstacles compared with their male peers. Together with our results, these reports suggest that supporting female residents during their career development to ensure favorable work–life balance could be a feasible solution to their mental health issues.[25]
Although the OCS system was effective in reducing working hours (i.e., mean weekly working hours from 75.2 to 64.9 hours), this study did not show the evidence of the effectiveness of the OCS in preventing burnout and depression among pediatric residents.
Indeed, previous studies on the efficacy of duty hour limitations for maintaining resident wellness have reported conflicting results.[26,27] A large, multicenter, prospective, longitudinal study in the United States found no improvement in depressive symptoms after implementation of duty hour regulation, and concluded that additional strategies were necessary to improve resident education and patient care.[28] Our trial in Japan also confirmed previous findings in Western countries. We used a focus-group interview with residents to identify the contributory factors to depression and burnout during their training. Of note, these factors were unlikely to be solved by the introduction of duty hour regulations.
Among the contributory factors identified, individual stress tolerance, high workload, and interpersonal conflict have previously been identified as typical determinants of burnout.[29,30] The presence of a generational gap toward what constitutes an appropriate work–life balance for physicians is an emerging issue worldwide when considering the mental health of medical trainees.[31] In 2009, the Royal College of Physicians and Surgeons of Canada published a comprehensive guide on physician health. The guide describes how generational differences in the value systems at work can contribute to conflict, and emphasizes the need for careful mentoring by faculties and respectful interpersonal communication between generations.[32]
In the qualitative study, we identified several protective factors against burnout. These included the presence of peer support among residents, supervision by attending physicians, and the need to balance resident workloads in consideration of an individual's stress tolerance. Studies on industrial health have recognized the importance of such social support systems from supervisors, coworkers, and family, suggesting that they act as a buffer against burnout. Indeed, these findings corroborate with our quantitative results of the prevalence of depression being lower in married residents.[33] Thus, an alternative strategy of offering support for residents would be needed.[34] Some medical education researchers have reported that duty hour regulations are insufficient and have noted the need to incorporate formal wellness curricula into resident training programs. Evidence indicates that such programs can effectively address the issues of resident stress and burnout. Lefebvre[35] advocated that resident wellness programs should provide a safe place for residents to express their emotions or grievances, with the aim to foster peer support. In addition, tailored mentorship programs for individual residents would allow not only monitoring of stress tolerance and workload imbalance but also development of resident–faculty interactions that might help to bridge existing generation gaps.[36] In 2013, the ACGME and the American Academy of Pediatrics (AAP) presented the pediatric milestone project and identified a need to develop specific personal and professional development competencies.[37] A clinical report of physician health and wellness by the AAP highlighted the wellness program contents, including measuring and tracking burnout in residents, creating a lecture series on wellness topics, organizing resident retreats focused on health and wellness, and establishing online curriculum on self-care and wellness.[38] Such programs may also be applicable to other countries, including Japan.
Many Japanese physicians are influenced by the ancient samurai value system of Bushido, which perceives self-sacrifice as a positive attitude, described by Inazo Nitobe.[39] However, the professionalism of young physicians is changing in the past decade, which might be because of the national reform of medical education in Japan.[40] A qualitative study revealed that Japanese residents decreased their subjective workload when they felt that they could control their job and have a fulfilling personal life.[41] In addition, the Japan Society for Medical Education presented a draft version of the core competency of medical professionalism, which consisted of 7 subdomains, with “self-control and career development” included as one of the domains.
As outlined above, several studies and public statements imply the changing professionalism of modern physicians and highlight the need for bridging the generational gap on the value system. In other words, resident wellness programs could be an essential tool for improving mental health issues and work–life balance among residents in Japan.
6. Strengths and limitations
To our knowledge, this is the first mixed methods study that describes depression and burnout among pediatric residents. Previous studies have been limited to quantitative study using depression or burnout scales. We have objectively described the prevalence of depression and burnout in a residency program, and supplemented it with a qualitative study that explored the subjective factors contributing to those results.
The main limitation of this study is its poor generalizability due to the small sample size and its single-institute nature. Thus, it is unclear whether our findings are applicable to other institutions in Japan and elsewhere. Nonetheless, this is the first trial to evaluate the wellness of pediatric residents in an Asian country, and our results represent important preliminary data that can inform future studies in this area.
Another shortcoming is the limited impact of the duty hour regulations. In this study, we implemented the overnight call shift system to regulate duty hours to maintain residents’ biological functions that may be disrupted by NF. We found that the extent of the reduction was smaller than that of previous reports of duty hour regulations by NF in other medical specialties such as surgery.[7] Hence, we cannot rule out the possibility that a larger reduction in working hours of residents by NF might help in decreasing the prevalence of depression among residents. Nonetheless, we managed to achieve a statistically significant reduction in working hours and the magnitude of the change was similar to that of a survey of pediatric residency programs in the United States after the implementation of duty hour limitations.[42]
A third limitation can be seen in the participants included in the qualitative focus-group interview. We performed the interviews using a guide prepared according to the results of quantitative analysis, and had planned to conduct the interviews in the same season as the quantitative study had been conducted to minimize seasonal influence on mood. Therefore, the interviews were conducted one year after the quantitative analysis. As a result, the interview participants did not include third-year residents. Although there was a clear selection bias, it is unlikely that this had a major influence on our findings because the principal grounded theory of the qualitative study did not focus on participant selection. It might also be disputable that the time lag of one year between the quantitative and qualitative study might influence the results of the interview. However, each of the study components was conducted from different aspects and methods. Hence, we believe that time lag had little impact on the results. In addition, we conducted only one focus-group interview with 4 participants. Undoubtedly, we did not reach data saturation. Nonetheless, the qualitative interview explored the factors that could trigger or prevent burnout in residents, and we found adequate qualitative grounded data to explain our questions that arose from the results of the quantitative cross-sectional study. While we are aware that the sample size of this study is small both in the quantitative and qualitative aspects, we believe that the mixed methods design compensated for these restrictions, and produced satisfactory answers to our research questions on mental health issues of pediatric residents.
In conclusion, although duty hour regulations have been used as the first-line solution for the prevention of burnout and depression among residents, this study found no evidence of the effectiveness of this approach. Resident wellness programs represent an additional strategy and should be aimed at fostering peer support and improvement of resident–faculty interactions. Such an approach could create a confidential and mutually beneficial relationship between physicians of different generations with conflicting belief structures.
Acknowledgments
We would like to thank the data record reviewers for their cooperation in data collection. We would also like to thank Dr Julian Tang of the Department of Education for Clinical Research, National Center for Child Health and Development, for proofreading and editing this manuscript.
Footnotes
Abbreviation: CES-D = Center for Epidemiologic Studies Depression Scale, MBI = Maslach Burnout Inventory, NF = night-float, OCS = overnight call shift.
Funding/support: This research received no specific grant from any funding agency in public, commercial, or not-for-profit sectors.
The authors report no conflicts of interest.
References
- 1.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med 2004; 351:1829–1837. [DOI] [PubMed] [Google Scholar]
- 2.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med 2004; 351:1838–1848. [DOI] [PubMed] [Google Scholar]
- 3.Ito M, Seo E, Ogawa R, et al. Can we predict future depression in residents before the start of clinical training? Med Educ 2015; 49:215–223. [DOI] [PubMed] [Google Scholar]
- 4.Hiyama T, Yoshihara M. New occupational threats to Japanese physicians: karoshi (death due to overwork) and karojisatsu (suicide due to overwork). Occup Environ Med 2008; 65:428–429. [DOI] [PubMed] [Google Scholar]
- 5.Japan Pediatric Society. 2013. Survey of pediatricians working in hospitals. Available at: http://www.jpeds.or.jp/uploads/files/saisin_130219_1_1(1).pdf Accessed May 12, 2015. [Google Scholar]
- 6.Nasca TJ, Day SH, Amis ES., Jr ACGME Duty Hour Task Force. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med 2010; 363:e3. [DOI] [PubMed] [Google Scholar]
- 7.Jamal MH, Rousseau MC, Hanna WC, et al. Effect of the ACGME duty hours restrictions on surgical residents and faculty: a systematic review. Acad Med 2011; 86:34–42. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed N, Devitt KS, Keshet I, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 2014; 259:1041–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ripp JA, Bellini L, Fallar R, et al. The Impact of Duty Hours Restrictions on Job Burnout in Internal Medicine Residents: A Three-Institution Comparison Study. Acad Med 2015; 90:494–499. [DOI] [PubMed] [Google Scholar]
- 10.Gottlieb DJ, Peterson CA, Parenti CM, et al. Effects of a night float system on housestaff neuropsychologic function. J Gen Intern Med 1993; 8:146–148. [DOI] [PubMed] [Google Scholar]
- 11.Deshpande GA, Soejima K, Ishida Y, et al. A global template for reforming residency without work-hours restrictions: decrease caseloads, increase education. Findings of the Japan Resident Workload Study Group. Med Teach 2012; 34:232–239. [DOI] [PubMed] [Google Scholar]
- 12.Ehara A. Labor law violations in Japanese public hospitals from March 2002 to March 2011. Pediatr Int 2013; 55:90–95. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi Y, Takayama JI, Mishina H, et al. Depressive symptoms among pediatric residents in Japan. E-PAS 2011; 4515:236. [Google Scholar]
- 14.Onishi H, Yoshida I. Rapid change in Japanese medical education. Med Teach 2004; 26:403–408. [DOI] [PubMed] [Google Scholar]
- 15.Albright K, Gechter K, Kempe A. Importance of mixed methods in pragmatic trials and dissemination and implementation research. Acad Pediatr 2013; 13:400–407. [DOI] [PubMed] [Google Scholar]
- 16.Radloff L. The CES-D scale. A self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1:385–401. [Google Scholar]
- 17.Shima S, Shikano T, Kitamura T. New self-rating scales for depression. [In Japanese.]. Seisin Igaku 1985; 27:717–723. [Google Scholar]
- 18.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav 1981; 2:99–113. [Google Scholar]
- 19.Higashiguchi K, Morikawa Y, Miura K, et al. The development of the Japanese version of the Maslach Burnout Inventory and the examination of the factor structure. Nihon Eiseigaku Zasshi 1998; 53:447–455. [DOI] [PubMed] [Google Scholar]
- 20.Hanson JL, Balmer DF, Giardino AP. Qualitative research methods for medical educators. Acad Pediatr 2011; 11:375–386. [DOI] [PubMed] [Google Scholar]
- 21.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 2008; 336:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sen S, Kranzler HR, Krystal JH, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry 2010; 67:557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goebert D, Thompson D, Takeshita J, et al. Depressive symptoms in medical students and residents: a multischool study. Acad Med 2009; 84:236–241. [DOI] [PubMed] [Google Scholar]
- 24.Yasukawa K, Nomura K. The perception and experience of gender-based discrimination related to professional advancement among Japanese physicians. Tohoku J Exp Med 2014; 232:35–42. [DOI] [PubMed] [Google Scholar]
- 25.Nomura K, Yano E, Fukui T. Gender differences in clinical confidence: a nationwide survey of resident physicians in Japan. Acad Med 2010; 85:647–653. [DOI] [PubMed] [Google Scholar]
- 26.Moonesinghe SR, Lowery J, Shahi N, et al. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients’ outcomes: systematic review. BMJ 2011; 342:1580. [DOI] [PubMed] [Google Scholar]
- 27.Schumacher DJ, Frintner MP, Jain A, et al. The 2011 ACGME standards: impact reported by graduating residents on the working and learning environment. Academic Pediatrics 2014; 14:149–154. [DOI] [PubMed] [Google Scholar]
- 28.Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med 2013; 173:657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hurrell JJ, McLaney MA. Exposure to job stress: A new psychometric instrument. Scand J Work Env Health 1988; 14:27–28. [PubMed] [Google Scholar]
- 30.Pantaleoni JL, Augustine EM, Sourkes BM. Burnout in pediatric residents over a 2-year period: a longitudinal study. Acad Pediatr 2014; 14:167–172. [DOI] [PubMed] [Google Scholar]
- 31.Jovic E, Wallace JE, Lemaire J. The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res 2006; 6:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puddester D, Flynn L, Cohen J. CanMEDS Physician Health Guide: A Practical Handbook for Physician Health and Well- Being. Ottawa, Ontario, Canada: Royal College of Physicians and Surgeons of Canada; 2009. [Google Scholar]
- 33.Dyrbye LN, West CP, Satele D, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med 2014; 89:443–451. [DOI] [PubMed] [Google Scholar]
- 34.Haoka T, Sasahara S, Tomotsune Y, et al. The effect of stress-related factors on mental health status among resident doctors in Japan. Med Edu 2010; 44:826–834. [DOI] [PubMed] [Google Scholar]
- 35.Lefebvre D. Perspective: Resident physician wellness: a new hope. Acad Med 2012; 87:598–602. [DOI] [PubMed] [Google Scholar]
- 36.Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med 2009; 84:269–277. [DOI] [PubMed] [Google Scholar]
- 37.The Accreditation Council for Graduate Medical Education, the American Board of Pediatrics. Pediatrics Milestone Projects. 2013. Available at: http://www.acgme.org/acgmeweb/Portals/0/PDFs/Milestones/320_PedsMilestonesProject.pdf Accessed March 12, 2015. [Google Scholar]
- 38.McClafferty H, Brown OW, Vohra S, et al. Physician health and wellness. Pediatrics 2014; 134:830–835. [DOI] [PubMed] [Google Scholar]
- 39.Nishigori H, Harrison R, Busari J, et al. Bushido and medical professionalism in Japan. Acad Med 2014; 89:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kinoshita K, Tsugawa T, Barnett PB, et al. Challenging cases of professionalism in Japan: improvement in understanding of professional behaviors among Japanese residents between 2005 and 2013. BMC Med Edu 2015; 15:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishigori H, Deshpande GA, Obara H, et al. Beyond work-hour restrictions: a qualitative study of residents’ subjective workload. Perspect Med Educ 2015; 4:176–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cull WL, Mulvey HJ, Jewett EA, et al. Pediatric residency duty hours before and after limitations. Pediatrics 2006; 118:e1805–e1811. [DOI] [PubMed] [Google Scholar]


