Abstract
Background:
The shoulder area is mainly innervated with the C5 and C6 nerve roots, and interscalene brachial plexus block (ISB) is widely used for postoperative analgesia after shoulder surgery. However, it is associated with adverse effects, such as numbness and weakness in the blocked arm due to an unwanted block of the lower brachial plexus (C7-T1). We hypothesized that the C5 approach during ISB would provide postoperative analgesia while minimizing adverse events after arthroscopic shoulder surgery.
Methods:
A total of 92 patients scheduled for arthroscopic shoulder surgery were enrolled and randomly assigned to 1 of the 3 groups: The control (no ISB, n = 31), conventional ISB (ISB with the conventional approach, n = 31), or C5 ISB (ISB with the C5 approach, n = 30) group. ISB was performed before the induction of anesthesia, and a subacromial catheter was placed in all patients at the end of the surgery. Postoperative pain scores, numbness, and weakness were recorded at 2, 8, and 24 hours after surgery. Oxygen saturation and overall patient satisfaction scores were also assessed at 1 and 48 hour after surgery, respectively.
Results:
The pain scores were lower in the conventional ISB group and the C5 ISB group than in the control group at postoperative 2 and 8 hours (P < 0.05). The incidence and degree of numbness and weakness of the blocked arm were significantly lower in the C5 ISB group than in the conventional ISB group (P < 0.05). Oxygen saturation were lower in the conventional ISB group and C5 ISB group than in the control group (P = 0.01). Overall patient satisfaction scores were higher in the C5 ISB group than in the control or conventional ISB group (P < 0.01).
Conclusion:
The C5 approach for ISB provides analgesia as effectively as the conventional approach following arthroscopic shoulder surgery, with the advantages of minimal numbness and weakness.
Keywords: interscalene brachial plexus block, rotator cuff tear, shoulder arthroscopy
1. Introduction
Various regional blocks have been used as adjunctive treatments to control postoperative pain after arthroscopic shoulder surgery for rotator cuff tears.[1–5] Interscalene brachial plexus block (ISB)—even with a single injection of a low dose of local anesthetic—is the most commonly used regional block in providing significant analgesia after shoulder surgery. However, ISB has also been associated with adverse effects, including numbness and weakness due to a temporary blockade of the lower brachial plexus.[6,7]
The C5 and C6 nerve roots primarily innervate the shoulders, and the authors presumed that the C5 approach for ISB may clinically be the appropriate management of postoperative pain after arthroscopic shoulder surgery for rotator cuff tears in minimizing lower brachial plexus (C7, C8 and T1) blockade. Dobie et al[8] showed that the C5 targeted nerve root block was effective for pain control after ambulatory shoulder surgery through prospective case series. Another previous investigation reported that the use of an ultrasound-guided C5–6 root perineural catheter with 0.2% ropivacaine provided adequate analgesia after major shoulder surgery.[9] However, to the best of our knowledge, there have not been any randomized and controlled studies that made a comparison of the efficacy and safety between ISB with the C5 approach and that with the conventional approach after shoulder surgery. We tested the hypothesis that an ultrasound-guided C5 approach for ISB is an adequate postoperative analgesia—while minimizing adverse events in the blocked arm—following arthroscopic shoulder surgery for a rotator cuff tear.
The present study compared the C5 approach with the conventional approach in using ISB with respect to analgesic efficacy and postoperative adverse effects following arthroscopic shoulder surgery for rotator cuff tear. The primary outcome measure was postoperative pain, and the secondary outcome measures included the incidence and degree of numbness and weakness in the blocked arm, postoperative oxygen saturation, and overall patient satisfaction.
2. Materials and methods
This prospective, randomized, and controlled study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1009/112–006). Written informed consent was obtained from each patient during a preoperative visit. The clinical trial was registered with the Clinical Research Information Service (No. KCT0000204).
In total, 92 ASA class I-III patients, aged 18–70 years, scheduled for elective arthroscopic shoulder surgery for rotator cuff repair were included. Exclusion criteria were known allergies to study medications, history of chronic opioid use, preoperative peripheral neuropathy, and refusal to undergo regional anesthesia. Patients were educated on the use of a numerical rating scale (NRS) at a preoperative visit.
Randomization was performed using a computer-generated random number table. Allocation numbers were sealed in opaque envelopes, which were opened in sequence by an independent anesthesiologist who was not involved in the assessment of outcomes. Patients who fulfilled the inclusion criteria were randomly allocated to 1 of the 3 groups: control group (no ISB); conventional ISB group (ISB with a conventional approach); or C5 ISB group (ISB with a C5 approach). Patients in conventional ISB and C5 ISB group were blinded to which method of ISB was performed. Outcome assessors were blinded to the treatment allocation.
Patients were premedicated with 30 μg/kg of midazolam for anxiolysis and transferred to the operating room. Each patient was monitored using standard protocols (noninvasive blood pressure monitoring, electrocardiography, and pulse oximetry). The skin was then disinfected with a povidone-iodine solution. No regional block was performed for the patients in the control group. The patients in conventional or C5 ISB group were placed in a lateral decubitus position and an ISB was performed by a single physician using an S-Nerve ultrasound machine with a 6–13-MHz linear transducer (SonoSite Inc., Bothell, WA). The success of the block was confirmed by checking the cold sensation of the shoulder area.
In the conventional ISB group, an ultrasound transducer was initially placed on the supraclavicular fossa to locate the supraclavicular brachial plexus, which was shown as a hypoechoic bundle lateral and superficial to the subclavian artery. By moving the transducer cranially, the brachial plexus was revealed between the anterior and middle scalene muscle (Fig. 1). An ultrasound reflector-coated nerve block needle (50-mm, 22-gauge Stimuplex A; B. Braun Melsungen AG, Melsungen, Germany) connected to a peripheral nerve stimulator (Stimuplex DIG RC; B. Braun Melsungen AG) was introduced into the plexus sheath under ultrasound guidance and placed between the C5 and C6 nerve roots. Its position was confirmed by activation of the deltoid motor reflex with a current output of 0.5 mA, after which 20 mL of 0.375% ropivacaine containing 1:200,000 epinephrine was administered incrementally.
Figure 1.
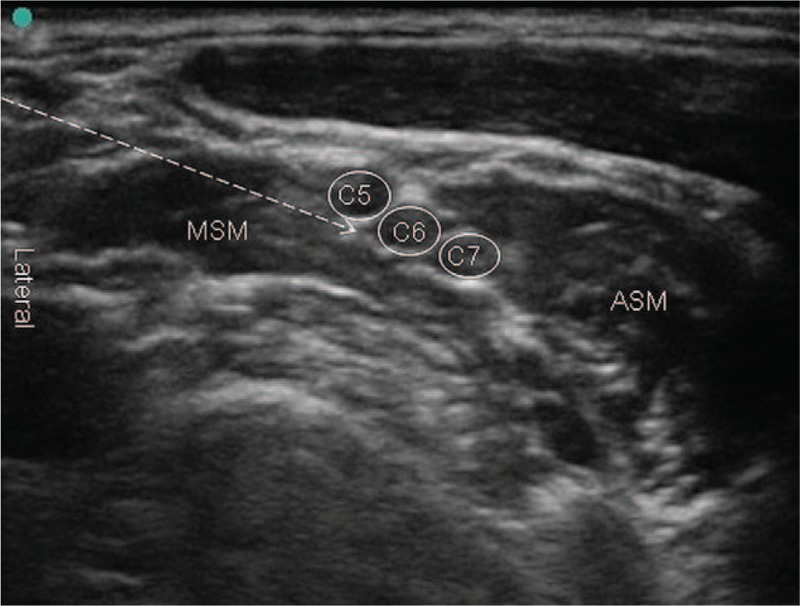
Sonographic view of interscalene brachial plexus block with conventional approach. ASM = anterior scalene muscle, MSM = middle scalene muscle.
In the C5 ISB group, the anterior and posterior tubercles of the C6 transverse process and the C6 nerve root were located at the level of the cricoid cartilage, which was confirmed by locating the posterior tubercle of the C7 transverse process. The distal C5 root could be observed at the anterior lateral side of the C6 root at the C6 transverse process level.[10,11] An ultrasound reflector-coated nerve block needle was inserted via a posterior approach under ultrasound guidance; the needle tip was placed just above the distal part of the C5 root at the level of the C6 transverse process (Fig. 2). After confirming negative aspiration, the same volume was injected around the C5 root incrementally.
Figure 2.
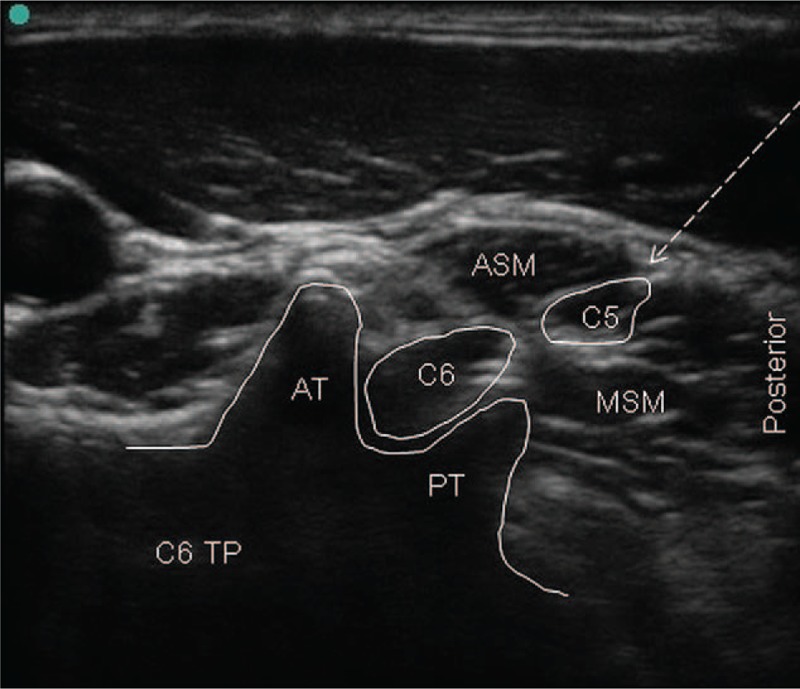
Sonographic view of interscalene brachial plexus block with C5 approach. ASM = anterior scalene muscle, AT = anterior tubercle, MSM = middle scalene muscle, PT = posterior tubercle, TP = transverse process.
After ISB, anesthesia was induced with intravenous propofol (2 mg/kg), sevoflurane, remifentanil (1 μg/kg), and rocuronium (0.6 mg/kg). After tracheal intubation, mechanical ventilation was controlled to maintain end-tidal CO2 at 35–40 mm Hg. Anesthesia was maintained with continuous infusion of remifentanil and sevoflurane (in oxygen mixed with medical air, FiO2 0.5).
Arthroscopic shoulder procedures for rotator cuff repair were performed by a single surgeon. All surgeries were performed in the lateral decubitus position with general anesthesia. In all patients, subacromial catheters were placed into the subacromial space under direct visualization at the end of surgery and a patient-controlled analgesia (PCA) device was connected to the subacromial catheter at the end of anesthesia. The PCA included 110 mL of 0.5% ropivacaine and was programmed to run at 2 mL/h as a background infusion with a 2-mL bolus dose and a 30-min lockout time. Subacromial catheters were removed after consumption of the PCA solution, in the ward. Patients were transferred to a post-anesthesia care unit (PACU) after surgery.
The primary outcome was the pain scores after surgery and these were evaluated at 2, 8, and 24 hours using a numerical rating scale (NRS; 0 = no pain, 10 = worst imaginable pain). Secondary outcomes were numbness and weakness in the blocked arm, postoperative oxygen saturation, and overall patient satisfaction. Numbness and weakness were recorded at 2, 8, and 24 hours after surgery. Oxygen saturation was recorded at 1 hour postoperatively and the patient global satisfaction score was also assessed with an NRS (0 = not satisfied, 10 = entirely satisfied) at 48 hours after surgery.
The sample size of 30 patients was based on a previous study,[5] in which the postoperative pain score (visual rating scale) in patients with a subacromial catheter (control group) was 5.22 (2.33) and a reduction of 2 (mean) was considered to be clinically important (α = 0.05, power = 0.9). The sample size analysis showed that 30 patients per group would be sufficient to detect a difference among the groups.
Statistical analyses were performed using the SPSS software (ver. 15.0 for Windows; SPSS, Chicago, IL). Continuous variables (age, weight, height, anesthesia time, operation time, intraoperative remifentanil infusion, pain NRS, postoperative oxygen saturation, and satisfaction NRS) were compared using analysis of variance (ANOVA) with a post hoc comparison using Bonferroni's correction. For comparisons of differences among groups in incidence variables (gender, ASA class, the incidences and degree of numbness and weakness), the chi-squared test or Fisher's exact test was used, as appropriate. Data are expressed as numbers of patients (%) or means (standard deviation). P values < 0.05 were considered to indicate statistical significance.
3. Results
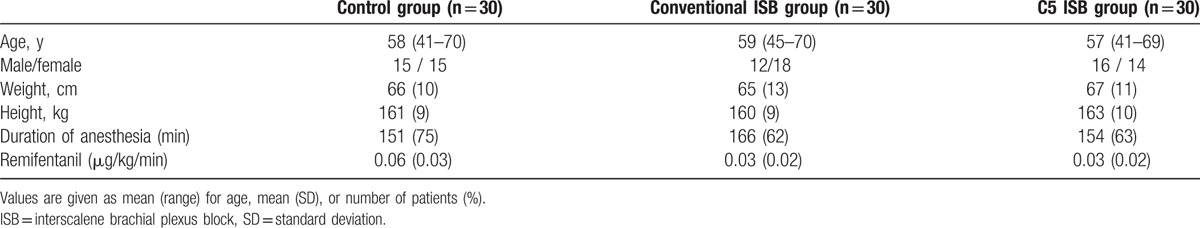
In total, 92 patients were recruited and 2 were excluded from the statistical analysis (due to subacromial catheter disconnection during the study period). Thus, data from 90 patients were analyzed (Fig. 3). The characteristics of patients are presented in Table 1 and there were no statistically significant differences among the groups.
Figure 3.
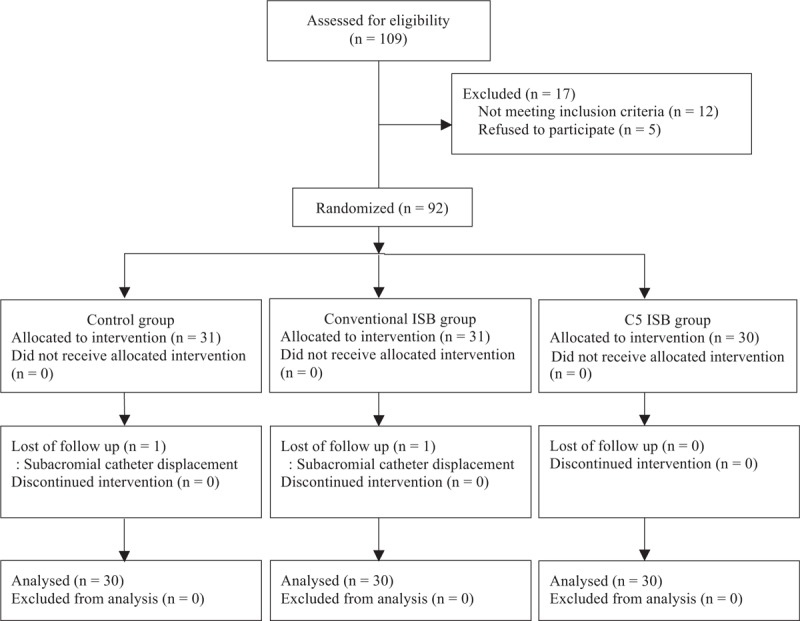
CONSORT flowchart. Ninety-two subjects were randomized; 2 subjects were eliminated due to subacromial catheter displacement during the study period. ISB = interscalene brachial plexus block.
Table 1.
Patients characteristics.
The postoperative pain scores were lower in conventional ISB group and C5 ISB group than in control group until 8 hours postoperatively; 7.6 (1.8) for control group vs. 1.1 (1.6) for conventional ISB group and 0.6 (1.1) for C5 ISB group at 2 hour postoperatively, P < 0.05; 4.1 (1.4) for control group vs. 3.2 (1.0) for conventional ISB group and 2.5 (1.5) for C5 ISB group at 8 hours postoperatively (P < 0.05, Fig. 4). There was no statistical significance in the 24 hours postoperative pain scores among the 3 groups (Fig. 4).
Figure 4.
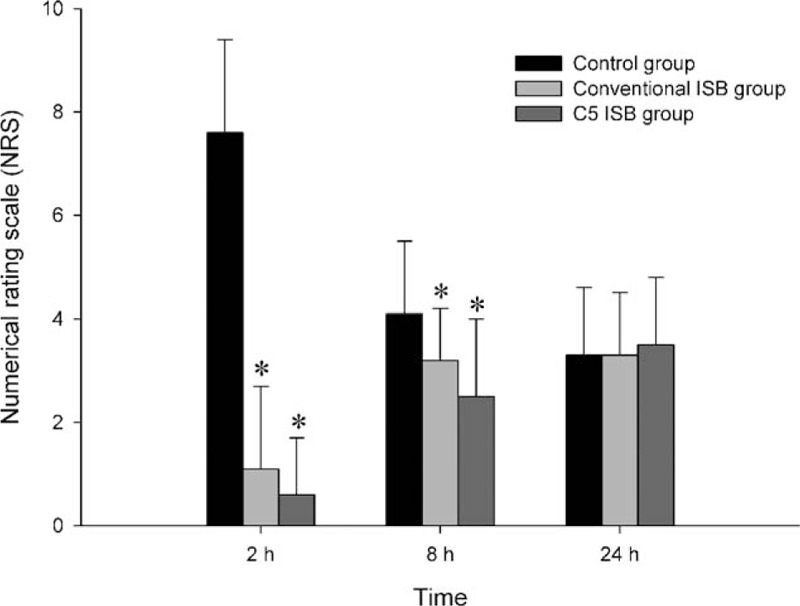
Postoperative pain scores. ISB = interscalene block. ∗P < 0.05 compared with control group.
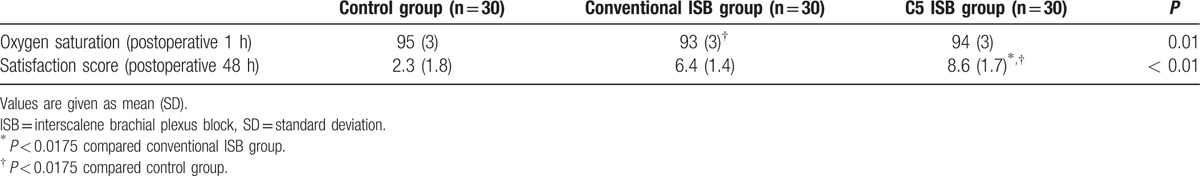
The incidence of numbness (57% vs 93%, P < 0.01) and of weakness (13% vs 70%, P < 0.01) in the blocked arm was lower in the C5 ISB group than in the conventional ISB group. Additionally, the degree of numbness and weakness was less in the C5 ISB group compared to the conventional ISB group (Table 2). The postoperative oxygen saturation value at postoperative 1 hour was significantly lower in the conventional ISB group and C5 ISB group than in the control group (93 [3] and [94] [3] vs 95 [3], respectively; P = 0.01). The overall patient satisfaction score at postoperative 48 hours was significantly higher in the C5 ISB group than in the control group or conventional ISB group (86 [17] vs 23 [18] or 64 [14], respectively; P < 0.01, Table 3).
Table 2.
Degree of numbness and weakness.
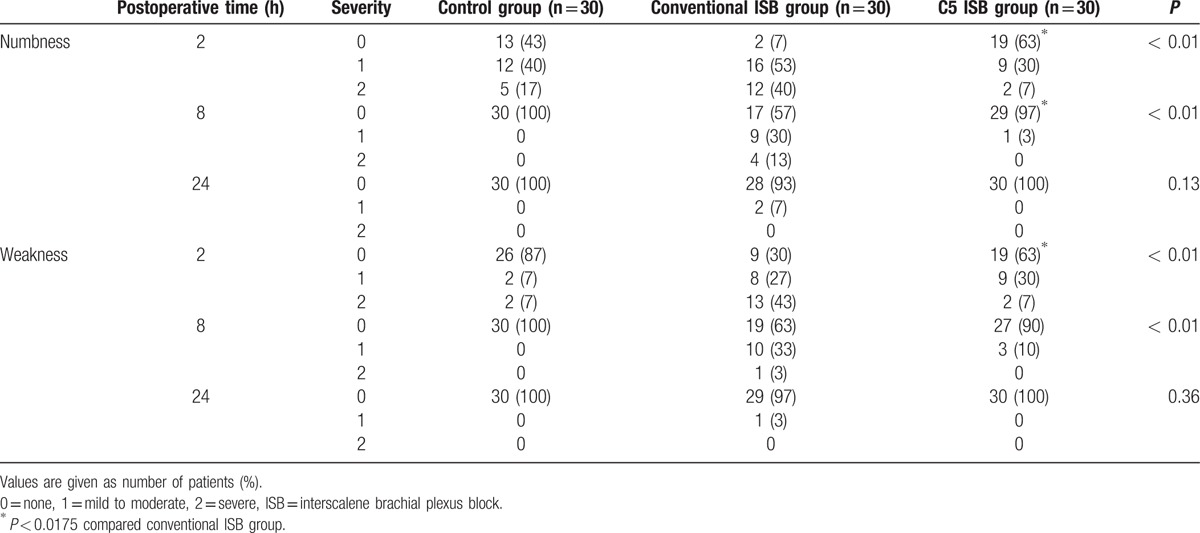
Table 3.
Oxygen saturation and patients’ satisfaction scores.
4. Discussion
We performed this prospective, randomized, controlled trial to determine whether the C5 approach during ISB is possible in decreasing postoperative pain without adverse events after arthroscopic shoulder surgery. The present study indicates that ISB with the C5 approach provided effective analgesia during the early postoperative period compared with a subacromial catheter alone. The incidence of adverse effects related to ISB, including numbness and weakness in the blocked arm, was reduced in patients who received ISB using the C5 approach compared with those who received ISB using the conventional approach.
Our results indicate that ISB with the C5 approach showed comparable postoperative analgesia with the conventional approach during the early postoperative period (2 and 8 hours after surgery). In the present study, ISB was performed by targeting the C5 root in the C5 ISB group whereas the needle was targeted to the C5–6 roots/superior-middle trunk between the anterior and the middle scalene muscle in the conventional ISB group.[9] The C5 nerve root is the most superficial nerve root in the interscalene space, although the C5–7 roots are surrounded by the same anatomical barriers, including the scalene muscles and the prevertebral fascia. The C5 nerve root is typically situated at the apex of the anterior scalene muscle.[12] Sometimes, it transverses through or along the edge of the anterior scalene muscle,[13] in which case, it may be spared after ISB using the conventional approach. In contrast to the conventional approach, C5 was explored more proximally in the C5-targeting control group and local anesthetics were injected around the C5 root, minimizing the effect of local anesthetics on the lower brachial plexus.
There was no difference in the postoperative pain scores at 24 hours among the groups; this might be explained by the fact that ISB was performed using a bolus injection instead of using a postoperative catheter and the effects of local anesthesia decreased gradually in both ISB groups. All patients in the current study underwent ISB with a subacromial catheter to provide adjunct analgesia at the end of surgery, and the catheter was connected to a PCA device postoperatively.
ISB with the C5 approach reduced the incidence and degree of numbness and weakness in the blocked arm. Numbness and weakness are common phenomena after ISB with the conventional approach.[14] ISB with the C5 approach seemed to have less influence on the lower brachial plexus (C7, C8, and T1) than ISB with the conventional approach. This result suggests that ISB with the C5 approach can improve the quality of recovery and increase patient satisfaction scores.
Most patients in both ISB groups—conventional and C5 approaches—showed a lower oxygen saturation than the control group. This may be explained by possible phrenic nerve palsy, which is one of the most common adverse effects of ISB with a reported incidence of up to 100%.[15,16] ISB with the C5 approach in this study did not reduce the incidence of phrenic nerve palsy due to possible unintended cephalad spread of local anesthetic to the phrenic nerve.
The present study also has a few limitations to be considered when interpreting the results. First, 20 mL of 0.375% ropivacaine was used to prolong postoperative analgesia in patients under ISB with both C5 and conventional approaches. Spread and absorption of the local anesthetic into the adjacent structures cannot be excluded, and this may interfere with the interpretation of the results. In a previous investigation, a low-volume ISB (5 mL) was associated with fewer respiratory complications, including diaphragmatic paralysis and postoperative oxygen desaturation, while providing equivalent analgesia when compared with a 20-mL ultrasound-guided technique.[15] Another study that investigated the effectiveness of various volumes at the C5 level also showed that a large-volume (20 mL) ISB was associated with increased complaints of dyspnea, whereas a small-volume (5 mL) ISB was associated with statistically higher pain scores in the early postoperative period.[17] Second, the phrenic nerve palsy that occurred was not confirmed by a chest radiography or pulmonary function test. Instead, the decrease in oxygen saturation in the PACU was used as a surrogate for phrenic nerve palsy. Nevertheless, these results are consistent with the findings reported in a previous study that showed even the smallest volumes of anesthetic at the C5 level induced ipsilateral diaphragmatic paresis and increased diaphragmatic motion on the contralateral side.[17] Third, the subacromial catheter connected PCA consumption was not recorded in this study, since the PCA device did not show an exact amount of consumption.
In conclusion, the C5 approach during ISB provided comparable analgesia to the conventional approach during ISB. This suggests that the former may be an effective alternative method of pain control after arthroscopic shoulder surgery for rotator cuff repair, since it—in addition to providing comparable analgesia—reduced the incidence and degree of numbness and weakness in the blocked arm, while at the same time increased the overall patient satisfaction scores.
Footnotes
Abbreviation: ISB = interscalene brachial plexus block.
The authors have no funding and conflicts of interest to disclose.
References
- 1.Borgeat A, Ekatodramis G. Anaesthesia for shoulder surgery. Best Pract Res Clin Anaesthesiol 2002; 16:211–225. [DOI] [PubMed] [Google Scholar]
- 2.Fredrickson MJ, Stewart AW. Continuous interscalene analgesia for rotator cuff repair: a retrospective comparison of effectiveness and cost in 205 patients from a multi-provider private practice setting. Anaesth Intensive Care 2008; 36:786–791. [DOI] [PubMed] [Google Scholar]
- 3.Krone SC, Chan VW, Regan J, et al. Analgesic effects of low-dose ropivacaine for interscalene brachial plexus block for outpatient shoulder surgery-a dose-finding study. Reg Anesth Pain Med 2001; 26:439–443. [DOI] [PubMed] [Google Scholar]
- 4.Busfield BT, Lee GH, Carrillo M, et al. Subacromial pain pump use with arthroscopic shoulder surgery: a short-term prospective study of complications in 583 patients. J Shoulder Elbow Surg 2008; 17:860–862. [DOI] [PubMed] [Google Scholar]
- 5.Coghlan JA, Forbes A, McKenzie D, et al. Efficacy of subacromial ropivacaine infusion for rotator cuff surgery. A randomized trial. J Bone Joint Surg Am 2009; 91:1558–1567. [DOI] [PubMed] [Google Scholar]
- 6.Fredrickson MJ, Abeysekera A, Price DJ, et al. Patient-initiated mandatory boluses for ambulatory continuous interscalene analgesia: an effective strategy for optimizing analgesia and minimizing side-effects. Br J Anaesth 2011; 106:239–245. [DOI] [PubMed] [Google Scholar]
- 7.Renes SH, Rettig HC, Gielen MJ, et al. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med 2009; 34:498–502. [DOI] [PubMed] [Google Scholar]
- 8.Dobie KH, Shi Y, Shotwell MS, et al. New technique targeting the C5 nerve root proximal to the traditional interscalene sonoanatomical approach is analgesic for outpatient arthroscopic shoulder surgery. J Clin Anesth 2016; 34:79–84. [DOI] [PubMed] [Google Scholar]
- 9.Fredrickson MJ, Price DJ. Analgesic effectiveness of ropivacaine 0.2% vs 0.4% via an ultrasound-guided C5-6 root/superior trunk perineural ambulatory catheter. Br J Anaesth 2009; 103:434–439. [DOI] [PubMed] [Google Scholar]
- 10.Narouze SN, Vydyanathan A, Kapural L, et al. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med 2009; 34:343–348. [DOI] [PubMed] [Google Scholar]
- 11.Moon JY, Lee SC. US-guided interventions cervical spine injections. Austin J Anesthesia and Analgesia 2014; 2:1014. [Google Scholar]
- 12.Soeding P, Eizenberg N. Review article: anatomical considerations for ultrasound guidance for regional anesthesia of the neck and upper limb. Can J Anaesth 2009; 56:518–533. [DOI] [PubMed] [Google Scholar]
- 13.Kessler J, Gray AT. Sonography of scalene muscle anomalies for brachial plexus block. Reg Anesth Pain Med 2007; 32:172–173. [DOI] [PubMed] [Google Scholar]
- 14.Lenters TR, Davies J, Matsen FA. (3rd). The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg 2007; 16:379–387. [DOI] [PubMed] [Google Scholar]
- 15.Riazi S, Carmichael N, Awad I, et al. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth 2008; 101:549–556. [DOI] [PubMed] [Google Scholar]
- 16.Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991; 72:498–503. [DOI] [PubMed] [Google Scholar]
- 17.Hartrick CT, Tang YS, Siwek D, et al. The effect of initial local anesthetic dose with continuous interscalene analgesia on postoperative pain and diaphragmatic function in patients undergoing arthroscopic shoulder surgery: a double-blind, randomized controlled trial. BMC Anesthesiol 2012; 12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]


