Supplemental Digital Content is Available in the Text.
Key Words: pelvic fracture, internal fixator, Majeed, symphyseal disruption, anterior fixatior, ramus fracture, pelvic fixation, functional outcomes, heterotopic ossification, pelvic deformity index, lateral femoral cutaneous nerve
Abstract
Objective:
To describe our experience using the anterior internal pelvic fixator (INFIX) for treating pelvic ring injuries.
Design:
Case Series.
Setting:
Level 1 Trauma Center.
Patients:
Eighty-three patients with pelvic ring injuries were treated with INFIX. Follow-up average was 35 months (range 12–80.33).
Intervention:
Surgical treatment of pelvic ring injuries included reduction, appropriate posterior fixation, and INFIX placement.
Outcome Measurements:
Reduction using the pelvic deformity index and pubic symphysis widening, Majeed functional scores, complications; infection, implant failure, heterotopic ossification (HO), nerve injury, and pain.
Results:
All patients healed in an appropriate time frame (full weight bearing 12 weeks postoperation). The average pelvic deformity index reduction (injury = 0.0420 ± 0.0412, latest FU = 0.0254 ± 0.0243) was 39.58%. The average reduction of pubic symphysis injuries was 56.92%. The average Majeed score of patients at latest follow-up was 78.77 (range 47–100). Complications were 3 infections, 1 case of implant failure, 2 cases implantation too deep, 7 cases of lateral femoral cutaneous nerve irritation, and 3 cases of pain associated with the device. HO was seen in >50% of the patients, correlated with increased age (P < 0.007), injury severity score (P < 0.05) but only 1 case was symptomatic.
Conclusions:
The pelvic injuries had good functional and radiological outcomes with INFIX and the appropriate posterior fixation. The downside is removal requiring a second anesthetic, there is a learning curve, HO often occurs, the lateral femoral cutaneous nerve may get irritated which often resolves once the implants are removed. Surgery-specific implants need to be developed.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
INTRODUCTION
The use of an anterior external fixator (Exfix) in the treatment of pelvic injuries is effective and may be lifesaving.1–19 Exfix is associated with pin-tract infections (25%–50% of pts),1,2,4,10–15,17,19,20 osteomyelitis (7%),1,2,10,11,14,17 loosening (10%),10,11,14,15,17 loss of reduction (up to 33%),2,4,10 is difficult to use in obese patients,7 and can be restrictive to movement.
The anterior subcutaneous internal pelvic fixator (INFIX)21 attempts to address these issues and has been used by several groups with good early results for reduction, fracture healing, patient mobility, comfort, and has acceptable complication rates.21–26 The reported complications include heterotopic ossification (HO), lateral femoral cutaneous nerve (LFCN) irritation, loss of fixation,21,22,27 and recent reports of femoral nerve palsy.28 The construct is biomechanically superior to the anterior 2 pin external fixator in stiffness when tested in single leg stance in an anterior–posterior compression type 3 (APC3) pelvic model,29 as strong as a femoral distractor for compressing the sacroiliac joint in an APC injury,30 equivalent to an external fixator in repetitive motion testing of translational stiffness and superior to an external fixator in repetitive motion testing of rotational stiffness.31 The purpose of this report is to evaluate our experience with INFIX, quantifying the results using radiographic measures,32–34 functional outcomes,35 complications, and technical issues we have encountered and learned from.
PATIENTS AND METHODS
An institutional review board–approved retrospective study was performed on 83 consecutive patients who underwent implantation of an INFIX between November 2007 and September 2014 at our institution and had a minimum of 12 months follow-up. Twenty-six patients in our database were not included because of loss of follow up (21) or early death (4). The surgical technique, reduction of the injury and, equipment for implantation, was previously described21,36 and demonstrated on the Orthopaedic Trauma Association video gallery37,38 (Fig. 1). The INFIX apparatus in this article was made with long pedicle or Schanz screws and rods from Johnson and Johnson Depuy Synthes (Paoli, PA).
FIGURE 1.
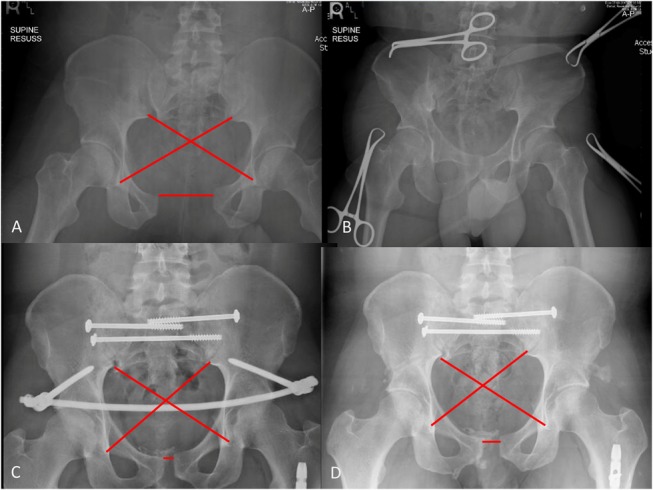
AP-pelvis x-ray of implanted INFIX showing measurements taken to calculate PDI values and symphyseal widening. A, AP pelvis injury film, (B) after application of a binder, (C) after surgery with the INFIX and posterior fixation, and (D) after removal of INFIX. Editor's Note: A color image accompanies the online version of this article.
We recorded demographic information including body mass index (BMI), fracture classifications, associated injuries with the injury severity score (ISS), timing of treatment, mechanism of injury, comorbidities and complications. Functional outcomes were assessed using the Majeed score, and radiographic outcomes were measured using the pelvic deformity index (PDI)32,34 and distraction of the pubic symphysis (PS).
Patients
The indications for surgery included an unstable pelvic fracture (OTA/AO classification 61-B or C 76 pts) as a result of a motor vehicle collision or pedestrian hit by a vehicle, falls, or crush injury; a painful pathologic fracture unresponsive to pain medications and failing to heal (6 patients); and an insufficiency fracture which was chronic and painful to the point of preventing ambulation (1 patient) (Table 1). The average age of the patients was 41.67 ± 15.9 years (median 42 years, range 14–86 years). There were 57 (68.7%) men and 26 (31.3%) women. The average ISS was 22.75 ± 11.2 (median 21, range 5–57) and BMI was 27.6 ± 7.4 (median 26.3, range 17.03–48.0). The average time from fixation to survey was 33.29 months (range 12.15–80.33). Eighty of the 83 patients also required posterior fixation and 11 had temporary external fixators/femoral distractors placed before definitive treatment with INFIX. In all cases, the conversion was performed within a week.
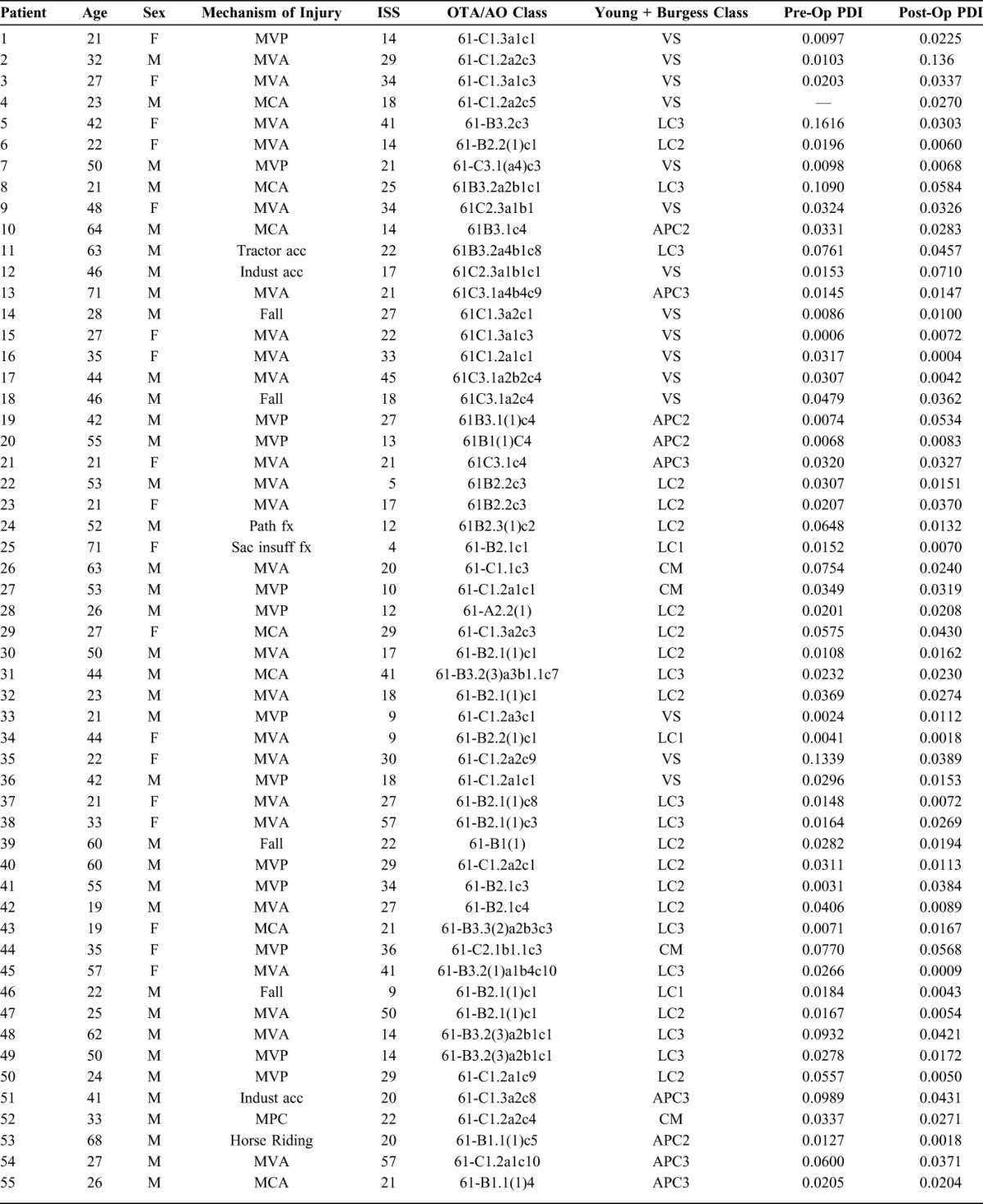
TABLE 1.
Demographics, Fracture Classifications, Reductions Based on PDI Values and Majeed Scores
Pelvic fractures were graded separately by an orthopaedic surgery resident and 2 fellowship-trained orthopaedic trauma surgeons using the OTA/AO39 and Young and Burgess40 classification systems. AP-pelvis radiographs were used in conjunction with computed tomography and fluoroscopic manual examination under anesthesia to classify the fractures. In the case of disagreements, a consensus was reached after a discussion. The fracture asymmetry was measured on anterior posterior pelvis x-rays using the cross measurement method first described by Keshishyan32 and later modified by Lefaivre33,34 (PDI Fig. 1). Measurement of PS displacement was performed using the largest width of the PS for disruptions. These measurements were performed preoperatively, postoperatively, after INFIX removal and at latest follow-up. Functional outcomes were assessed using the scoring system described by Majeed.35 This was obtained at the latest clinic visit (47 patients) or by phone survey (36 patients).
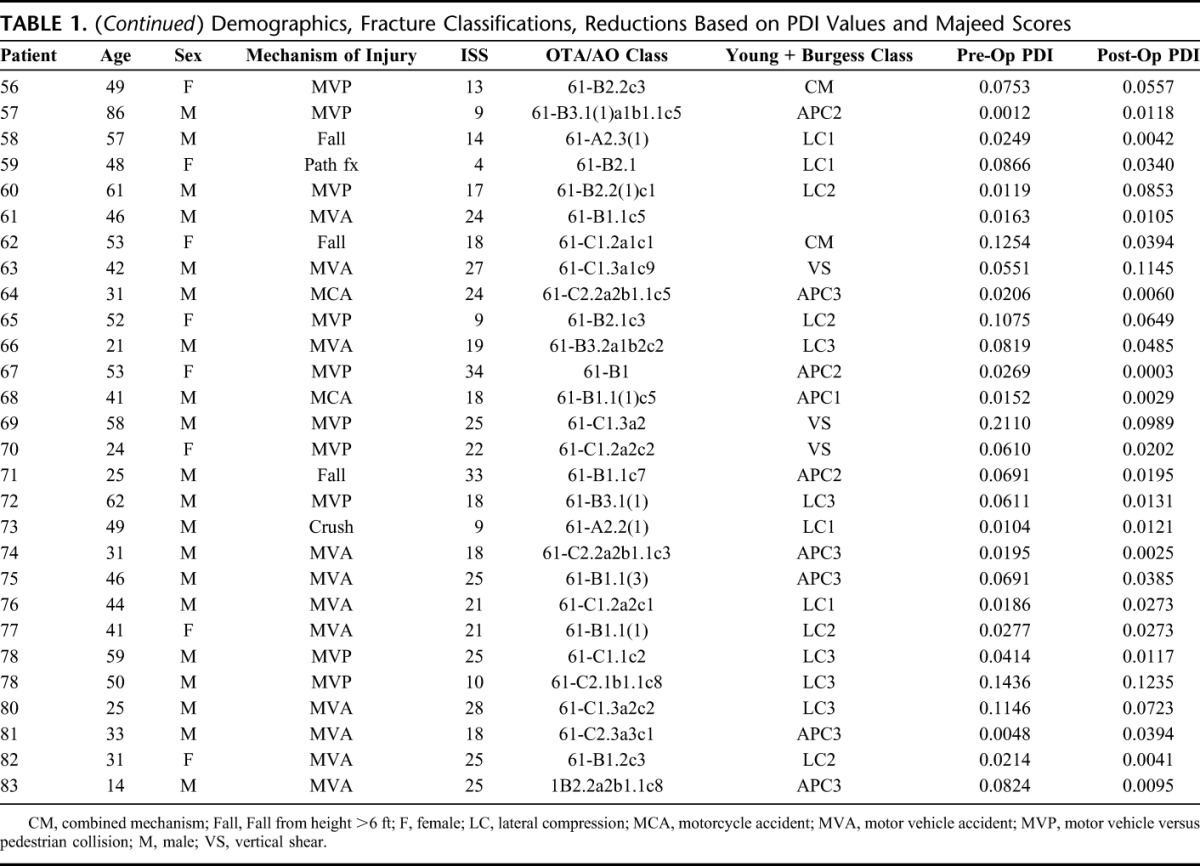
HO in the soft tissues surrounding the implants was determined on x-rays at 3 months postoperation before INFIX removal and at latest follow-up. The severest grade of the 2 x-rays was used. HO was graded based on size and appearance as none, some HO (wispy or diffuse <30 mm), and severe HO (>30 mm) (Fig. 2). The patients' left and right sides were evaluated separately, with the side having the most severe grade determining the overall HO classification.
FIGURE 2.
HO. A, None. B, Some HO < 3 cm in any direction. C, Severe HO > 3 cm in any direction.
Other complications were tabulated. Lessons learned from technical failures and improvements to the original technique are described and demonstrated.37
All statistical analyses were performed using Pearson correlation coefficients, the t test, or analysis of variance (ANOVA) in Microsoft Excel, where applicable. Statistical significance was determined as P < 0.05.
RESULTS
Fracture Healing
The pelvic injury was deemed to be healed when the patient was allowed to fully weight bear. In our study, all patients were allowed to be full weight bearing by 12 weeks postoperation without difficulty. Four patients did not weight bear at 12 weeks because of spinal cord injury (2) and 2 who had pathological fractures with multiple other conditions preventing weight bearing. There has been no case of nonunion from a traumatic fracture in this case series.
Fracture Reduction
The average reduction was 39.6% of the original injury (PDI). Patients who suffered injuries to the PS (30) experienced a 56.9% reduction of the injury after reduction and implantation of INFIX. Of these injuries, 17 had an original displacement greater than 25 mm, 9 between 15 and 25 mm, and 4 less than 15 mm. With the INFIX in place, there were 26 (PS < 14 mm) very good, 4 (15–25 mm) good symphyseal reductions (see Table, Supplemental Digital Content 1, http://links.lww.com/BOT/A845). Loss of reduction occurred in one case where the implants were improperly secured by one of our surgeons during the early stages of the study. This case was reinstrumented with the same implants the next day with C-rings to reinforce the construct and led to a good outcome.
Implant Retention
INFIX is typically removed after 3 months or when the fracture has demonstrated healing on x-ray. The average time of removal was 5.3 ± 5.4 months (median 3.7, range 0.3–49.5 months). The average time to removal was greater than 3 months as often patients are scheduled for the removal but patient or scheduling issues delayed the procedure and this number also includes several patients who did not want to have it removed when we suggested (including one who decided on removal at 49.5 months postoperation). Three patients had the device removed early because of the development of an infection. Seventy-three of the 83 implants were removed. Six patients died before removal (all had cancer, implant retained >12 months), 1 was unable to be removed because of complications with anesthesia, and 3 declined. Neither of these 3 patients complained about any discomfort from the INFIX. One patient had the implant in for 49.5 months and delivered 2 children vaginally with the bar in place.41
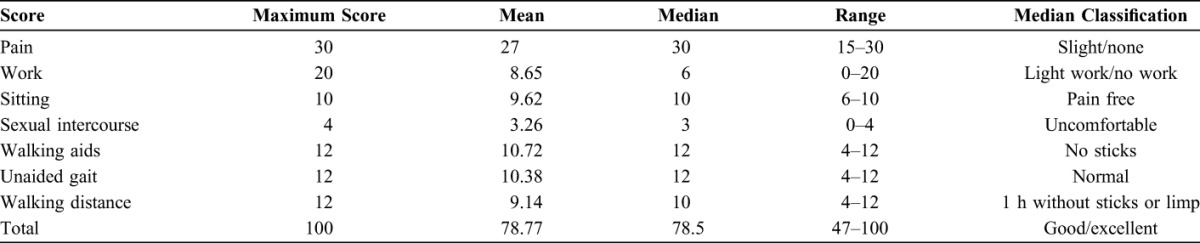
Outcome Scores
The average follow-up was 35 ± 12.4 months (range 12–80.33 months) and the average Majeed score was 78.8 ± 13.8 (median 78.5, range 47–100). Majeed scores were collected and analyzed by individual category (Table 2). Pearson correlations were used to test for correlations between Majeed score and several other factors. In this series, a higher ISS was correlated with a poorer Majeed score (P < 0.0001 ANOVA). There was little correlation between the Majeed Score and age (ρ = −0.19) or reduction (PDI ρ = −0.15). Majeed scores verses length of follow-up <24 months (75.72) and >24 months (78.61) showed no significant difference (P = 0.50 t test).
TABLE 2.
Breakdown of Majeed Scores by Subsection
COMPLICATIONS
HO
No sign of HO was seen in 32.5% of patients, some HO was found in 32.5%, and 35% had developed severe HO. Only 2 patients had symptoms related to HO. One patient had severe HO and complained for 4 months after removal of implants, did not let us remove it and the patient stopped complaining about it. A second patient had severe HO unrelated to the INFIX but to a massive soft tissue injury. This patient had multiple upper and lower extremity injuries including a proximal femur fracture.
ANOVA tests were performed to ascertain a relationship between HO: Majeed scores, duration of fixation, ISS, GCS, sex, race, and age. Older age and HO classes were statistically significant with a P value of 0.007. The relationship between higher ISS and HO development was found to be statistically significant with a P value of 0.05 using a t test. The length of time the INFIX was in place, GCS, sex, race, Majeed scores showed no significant relationship with the development of HO.
Infection
Infection at the surgical site was noted in 3 cases. One patient had a bladder injury with the suprapubic catheter placed above the bikini line at the time of INFIX placement. However, the urological team decided to reposition the catheter later that week and placed the catheter through the area of the INFIX bar (see Figure, Supplemental Digital Content 2, http://links.lww.com/BOT/A844). They were unfamiliar with the INFIX device and we failed to communicate its location. This led to an infection which required removal of the implant at 3 weeks. No loss of reduction was encountered as there was good posterior fixation. A second patient was noncompliant; he walked right away on the fracture and developed a posterior infection which presented 4 months after insertion. The third patient was obese, had a Morel-Lavallee lesion, and developed a superficial infection at the surgical site which eventually infected the hardware. We removed the implants, preformed serial irrigation and debridements's with eventual resolution after 6 weeks of intravenous antibiotics. At latest follow-up, there has been no recurrence of infection.
Persistent irritation of the LFCN was observed in 7 cases, none of which were problematic and resolved once the implants were removed. Our feeling is that as many as 25% of the patients have some irritation of the LFCN, most are minor and can be from numbness to paresthesia that resolve quickly. Persistent irritation was felt to be complaints that are still present at the time of implant removal. One patient developed numbness and dysesthesia at removal. These did not lead to any long-term difficulty.
Implant revision occurred in 3 of the early cases. In one case, the rods and caps were improperly secured, resulting in loss of reduction requiring revision as with the addition of C-Clamps.38 In 2 morbidly obese patients, the INFIX bar was placed too deep, causing discomfort, a crease in the lower abdomen, and swelling in the legs and occurred in our first series that we reported.21 The screws were too short and sunk too far into the iliac wing at the anterior inferior iliac spine. The implants were removed and replaced with 110 mm screws which protruded from the anterior inferior iliac spine almost 50 mm so that the heads sat at the level of the subcutaneous rod. No further problems occurred in these individuals and they healed uneventfully.
Three cases of discomfort clearly caused by the device were observed all in very thin women. Each tolerated the situation and had the device removed at 3 months.
DISCUSSION
Physicians are always seeking better ways to provide treatment to their patients. It was this spirit that led to the development of the INFIX device as an alternative to the widely used external fixator for definitive fixation of anterior pelvic ring injuries. The INFIX technique was developed with obese individuals in mind, but as we became more confident, we expanded our indications. As such, our patients had a mean BMI of 27.6 (median 26.3, range 17.03–48.0), and we do not restrict its use to obese patients. Patients find INFIX comfortable and are able to sit and move without limitation.21,22
The Keshishyan cross method was chosen to analyze reduction because of its reliability compared with other methods described in the literature.42 Our average reduction was 39.6% and an average reduction in PDI of 0.0166 ± 0.0343. A limitation of this method is that it frequently underestimates the severity of the fracture and the quality of the reduction in AP compression (APC) injuries as the disruption may be symmetric and thus give a very low PDI. Thus diastasis of the PS is important in assessing the severity and reduction of these APC injuries. A 56.9% reduction was seen in these 30 patients with 26 (PS < 14 mm) very good, 4 (PS 15–25 mm) good. There was loss of reduction in one case which required revision as reported above because of unfamiliarity with the implants. Loss of reduction has been reported with the use of polyaxial pedicle screws in APC3 injuries.22,27 We performed a biomechanical study to test this issue and found that polyaxial screws failed in distraction at about 150N, whereas monoaxial screws did not.31 Another study confirmed this.43 If polyaxial systems are chosen, we recommend the use of C-Clamps outside these screws to reinforce the construct (Fig. 1C) or using the Universal Spine System fracture module (Synthes Spine, Paoli, PA) which is very strong.31,37
We chose to use the Majeed functional outcomes score as it is easy to perform, but shows similar validity when compared with other accepted methods of evaluating functional outcomes of pelvic fractures.33 Median Majeed scores for pain, sitting, standing, and unaided gait all had scores within the highest range (Table 2). Sexual intercourse and walking distance score medians were within the second highest score. The only set of scores not within the highest 2 ranges in terms of median and mean were work scores. This discrepancy in work scores could reflect economic or personal factors such as the high rate of unemployment within our city (24% according to the Bureau of Labor Statistics). Overall, the Majeed scores indicate positive long-term results for the patients. We performed statistical analysis to ascertain significant relationships and correlations between different factors and Majeed scores. Most results were statistically inconclusive. However, greater ISS, which denote greater and more traumatic injuries, were found to have worse functional outcomes or lower Majeed scores score (P < 0.0001 ANOVA).
The complications associated with the INFIX procedure have previously been described,21,22 and most of these complications are not unique to INFIX. They can occur with other fixation methods. Pin-tract infections are common in anterior external fixators (25%–50% of pts),1,2,4,10–15,17,19,20 and the INFIX procedure also had infections in our hands although much reduced 3/83 (3.6%) because of the internal position. In patients who had an external fixator using supra-acetabular pin placement, we used a new screw path to place the INFIX after removing the external fixator pins.
Parasthesias in the distribution of the LFCN is a common occurrence with the INFIX and in our series was persistent in 7 patients. It may occur with an external fixator when using supra-acetabular pin placement as well due to the proximity of the device to the LFCN.44 Removal of the device at the end of treatment solved the issue in each one of the patients except one but it was not found to be a problem as reported by this patient. Femoral nerve palsies have been reported in the literature as a complication of INFIX.28 We have not experienced this in our patients. We feel that placing the screws too deep can lead to compression of the underlying structures. In our early series, this happened on 2 occasions and led to discomfort and leg swelling. However, it was recognized fairly quickly and revised with longer screws.21 The cases of femoral nerve palsy in an article by Hesse et al28 all occurred in patients operated by surgeons early in their experience with the procedure.
HO around the device seems to be unique to INFIX, as it has not been reported in the literature for external fixation. In our series, it was related to increased ISS (P < 0.05) and age of the patient with older patients suffering more HO (P = 0.007). It was asymptomatic in all patients even at latest follow-up, except in one patient as mentioned in the results. No specific treatment was performed. During hardware removal, one always has the opportunity to remove HO as well. We have conducted this several times when it was present but have not made it a routine practice.
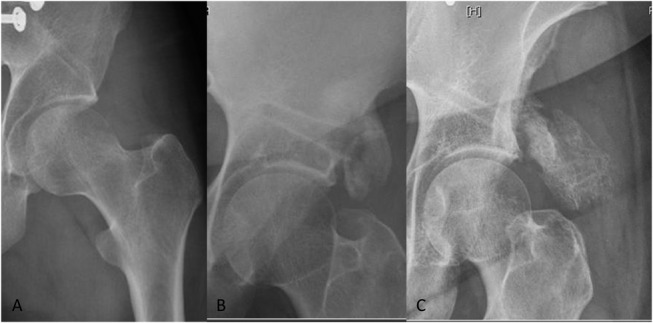
Technical lessons: placing the screw heads too deep in obese patients can lead to compression of the underlying structures, and we recommend to keep the bar very superficial. We have switched from the use of pedicle screws to Schanz pins and the Universal Spine System fracture module (Synthes Spine) which has pins that are 150-mm long and in obese individuals they are useful (Fig. 3). In cases of APC3 injuries, there is sometimes force which exceeds the capability of the polyaxial pedicle screw caps and may lead to failure.22,27 In these cases, we have used monoaxial screws that have a very strong connection, the Schanz pins from the Universal Spine System fracture module, or have placed C-Clamps on the outside of both pedicle screws to reinforce the construct. These are all very strong constructs.31 The ultimate solution for this problem is to have implants specifically for this method which are designed to withstand the loads of a pelvis and have extremely long lengths.
FIGURE 3.
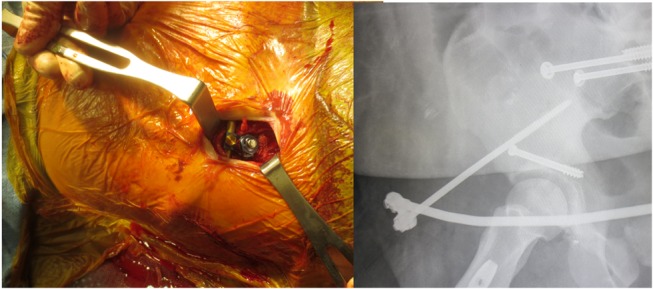
The rod should be placed very superficial. The USS fracture module (Synthes Spine) has pins that are 150-mm long and in really obese individuals, they are very useful. Editor's Note: A color image accompanies the online version of this article.
The limitations of this study include the lack of a control group with fractures treated by the same surgeons using more traditional methods and leaves us with no way to compare INFIX directly with other methods. This is a retrospective study and several prospective comparative studies with INFIX and plates are now starting. Majeed scores were compared in patients who were at different stages of recovery, and although there was no correlation with the length of follow-up (<24 vs. > 24 months), we do believe a more homogenous group of patients would show improvement in scores over time or if we had followed outcome scores during the entire recovery period, this trend may have become apparent in the recovery of each patient. It is still unclear to us from this data set when improvement in outcome begins to plateau. Our study is a larger single-center sample of patients than previously seen in the literature regarding INFIX.
CONCLUSIONS
The pelvic injuries had good functional and radiological outcomes with INFIX and the appropriate posterior fixation. The downside is removal requiring a second anesthetic, there is a learning curve, HO often occurs, the LFCN may get irritated which often resolves once the implants are removed. Surgery-specific implants need to be developed.
Footnotes
R. Vaidya: European Spine Journal, Journal of Orthopaedic Trauma, Editorial or governing board; Smith & Nephew, IP royalties, paid speaker, institutional research grant funding; Depuy Synthes, IP royalties; AO Foundation paid speaker. R. Vaidya is a consultant for Johnson and Johnson Depuy Synthes and Smith and Nephew to develop and FDA-approved INFIX implant which is not used in this article. Over-the-counter spine implants with long screws were used. B. Oliphant: Stock or stock Options Synthes; Paid presenter, or speaker AO Foundation. The remaining authors report no conflict of interest.
Presented as a poster at the Annual Meeting of the Orthopaedic Trauma Association, October 9, 2015, San Diego, CA.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
REFERENCES
- 1.Arazi M, Kutlu A, Mutlu M, et al. The pelvic external fixation: the mid-term results of 41 patients treated with a newly designed fixator. Arch Orthop Trauma Surg. 2000;120:584–586. [DOI] [PubMed] [Google Scholar]
- 2.Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2000;14:475–482. [DOI] [PubMed] [Google Scholar]
- 3.Rockwood CA, Green DP, Bucholz RW, et al. Rockwood and Green's Fractures in Adults. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 4.Gansslen A, Pohlemann T, Krettek C. A simple supraacetabular external fixation for pelvic ring fractures [in German]. Oper Orthop Traumatol. 2005;17:296–312. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Nork SE. Stabilization of unstable pelvic fractures with supraacetabular compression external fixation. J Orthop Trauma. 2007;21:269–273. [DOI] [PubMed] [Google Scholar]
- 6.Haidukewych GJ, Kumar S, Prpa B. Placement of half-pins for supra-acetabular external fixation: an anatomic study. Clin Orthop Relat Res. 2003;269–273. [DOI] [PubMed] [Google Scholar]
- 7.Hupel TM, McKee MD, Waddell JP, et al. Primary external fixation of rotationally unstable pelvic fractures in obese patients. J Trauma. 1998;45:111–115. [DOI] [PubMed] [Google Scholar]
- 8.Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop Relat Res. 1989;66–82. [PubMed] [Google Scholar]
- 9.Lefaivre KA, Starr AJ, Barker BP, et al. Early experience with reduction of displaced disruption of the pelvic ring using a pelvic reduction frame. J Bone Joint Surg Br. 2009;91:1201–1207. [DOI] [PubMed] [Google Scholar]
- 10.Lindahl J, Hirvensalo E, Bostman O, et al. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955–962. [DOI] [PubMed] [Google Scholar]
- 11.Mason WT, Khan SN, James CL, et al. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. [DOI] [PubMed] [Google Scholar]
- 12.Mears DC, Fu FH. Modern concepts of external skeletal fixation of the pelvis. Clin Orthop Relat Res. 1980;65–72. [PubMed] [Google Scholar]
- 13.Riemer BL, Butterfield SL, Diamond DL, et al. Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilization and external fixation. J Trauma. 1993;35:671–675. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 14.Scaglione M, Parchi P, Digrandi G, et al. External fixation in pelvic fractures. Musculoskelet Surg. 2010;94:63–70. [DOI] [PubMed] [Google Scholar]
- 15.Solomon LB, Pohl AP, Sukthankar A, et al. The subcristal pelvic external fixator: technique, results, and rationale. J Orthop Trauma. 2009;23:365–369. [DOI] [PubMed] [Google Scholar]
- 16.Tile M. The management of unstable injuries of the pelvic ring. J Bone Joint Surg Br. 1999;81:941–943. [DOI] [PubMed] [Google Scholar]
- 17.Tucker MC, Nork SE, Simonian PT, et al. Simple anterior pelvic external fixation. J Trauma. 2000;49:989–994. [DOI] [PubMed] [Google Scholar]
- 18.Kim WY, Hearn TC, Seleem O, et al. Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res. 1999;237–244. [DOI] [PubMed] [Google Scholar]
- 19.Majeed SA. External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br. 1990;72:612–614. [DOI] [PubMed] [Google Scholar]
- 20.Wild JJ, Jr, Hanson GW, Tullos HS. Unstable fractures of the pelvis treated by external fixation. J Bone Joint Surg Am. 1982;64:1010–1020. [PubMed] [Google Scholar]
- 21.Vaidya R, Colen R, Vigdorchik J, et al. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26:1–8. [DOI] [PubMed] [Google Scholar]
- 22.Vaidya R, Kubiak EN, Bergin PF, et al. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study. Clin Orthop Relat Res. 2012;470:2124–2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merriman DJ, Ricci WM, McAndrew CM, et al. Is application of an internal anterior pelvic fixator anatomically feasible? Clin Orthop Relat Res. 2012;470:2111–2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuttner M, Klaiber A, Lorenz T, et al. The pelvic subcutaneous cross-over internal fixator [in German]. Der Unfallchirurg. 2009;112:661–669. [DOI] [PubMed] [Google Scholar]
- 25.Muller FJ, Stosiek W, Zellner M, et al. The anterior subcutaneous internal fixator (ASIF) for unstable pelvic ring fractures. Clinical and radiological mid-term results. Int Orthop. 2013;37:2239–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scheyerer MJ, Zimmermann SM, Osterhoff G, et al. Anterior subcutaneous internal fixation for treatment of unstable pelvic fractures. BMC Res Notes. 2014;7:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Owen MT, Tinkler B, Stewart R. Failure and salvage of “INFIX” instrumentation for pelvic ring disruption in a morbidly obese patient. J Orthop Trauma. 2013;27:e243–e246. [DOI] [PubMed] [Google Scholar]
- 28.Hesse D, Kandmir U, Solberg B, et al. Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma. 2014;29:138–143. [DOI] [PubMed] [Google Scholar]
- 29.Vigdorchik JM, Esquivel AO, Jin X, et al. Biomechanical stability of a supra-acetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertically unstable pelvic fractures. J Orthop Surg Res. 2012;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vigdorchik JM, Esquivel AO, Jin X, et al. Anterior internal fixator versus a femoral distractor and external fixation for sacroiliac joint compression and single stance gait testing: a mechanical study in synthetic bone. Int Orthop. 2013;37:1341–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vaidya R, Onwudiwe N, Roth M, et al. Monoaxial pedicle screws are superior to polyaxial pedicle screws and the two pin external fixator for subcutaneous anterior pelvic fixation in a biomechanical analysis. Adv Orthop. 2013;2013:683120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keshishyan RA, Rozinov VM, Malakhov OA, et al. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin Orthop Relat Res. 1995;28–33. [PubMed] [Google Scholar]
- 33.Lefaivre KA, Slobogean GP, Ngai JT, et al. What outcomes are important for patients after pelvic trauma? Subjective responses and psychometric analysis of three published pelvic-specific outcome instruments. J Orthop Trauma. 2014;28:23–27. [DOI] [PubMed] [Google Scholar]
- 34.Lefaivre KA, Blachut PA, Starr AJ, et al. Radiographic displacement in pelvic ring disruption: reliability of 3 previously described measurement techniques. J Orthop Trauma. 2014;28:160–166. [DOI] [PubMed] [Google Scholar]
- 35.Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71:304–306. [DOI] [PubMed] [Google Scholar]
- 36.Vaidya R, Oliphant B, Hudson I, et al. Sequential reduction and fixation for windswept pelvic ring injuries corrects the deformity until healed. Int Orthop. 2013;37:1555–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaidya R, Nasr K, Kanneganti P, et al. The anterior pelvic internal fixator “INFIX” technique. OTA Video Library 2016. Available at https://vimeo.com/147862715. Accessed June 5, 2016.
- 38.Vaidya R, Tonnos F, Nasr K, et al. The anterior subcutaneous pelvic fixator (INFIX) in an anterior posterior compression type 3 pelvic fracture. J Orthop Trauma. 2016;30(suppl 2):S21–S22. [DOI] [PubMed] [Google Scholar]
- 39.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133. [DOI] [PubMed] [Google Scholar]
- 40.Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:981–1000. discussion -2. [PubMed] [Google Scholar]
- 41.Sethi A, Vaidya R, Schneider S, et al. Vaginal delivery after pelvic fracture fixation with a subcutaneous anterior fixator with review of literature of delivery mode in pelvic injuries. Open J Obstet Gynecol. 2014;4:836. [Google Scholar]
- 42.Lefaivre KA, Slobogean G, Starr AJ, et al. Methodology and interpretation of radiographic outcomes in surgically treated pelvic fractures: a systematic review. J Orthop Trauma. 2012;26:474–481. [DOI] [PubMed] [Google Scholar]
- 43.Eagan M, Kim H, Manson TT, et al. Internal anterior fixators for pelvic ring injuries: do monaxial pedicle screws provide more stiffness than polyaxial pedicle screws? Injury. 2015;46:996–1000. [DOI] [PubMed] [Google Scholar]
- 44.Vaidya R, Oliphant B, Jain R, et al. The bikini area and bikini line as a location for anterior subcutaneous pelvic fixation: an anatomic and clinical investigation. Clin Anat. 2013;26:392–399. [DOI] [PubMed] [Google Scholar]


