We studied postoperative pain trajectories and associated factors. Expectation of severe postoperative pain was associated with higher intensity of experimental and postoperative pain.
Keywords: Acute pain trajectories, Breast cancer, Pain expectation, Psychological distress
Abstract
The aim of this study was to identify clinical risk factors for unfavorable pain trajectories after breast cancer surgery, to better understand the association between pain expectation, psychological distress, and acute postoperative pain. This prospective study included 563 women treated for breast cancer. Psychological data included questionnaires for depressive symptoms and anxiety. Experimental pain tests for heat and cold were performed before surgery. The amount of oxycodone needed for satisfactory pain relief after surgery was recorded. Pain intensity in the area of operation before surgery and during the first postoperative week and expected intensity of postoperative pain were recorded using the Numerical Rating Scale (NRS 0-10). Pain trajectories were formed to describe both initial intensity (the intercept) and the direction of the pain path (the slope). Factors associated with higher initial pain intensity (the intercept) were the amount of oxycodone needed for adequate analgesia, psychological distress, type of axillary surgery, preoperative pain in the area of the operation, and expectation of postoperative pain. The higher the pain initially was, the faster it resolved over the week. Expectation of severe postoperative pain was associated with higher scores of both experimental and clinical pain intensity and psychological factors. The results confirm that acute pain after breast cancer surgery is a multidimensional phenomenon. Psychological distress, pain expectation, and the patients' report of preoperative pain in the area to be operated should be recognized before surgery. Patients having axillary clearance need more efficient analgesic approaches.
1. Introduction
Breast cancer is the most common type of cancer among women in developed countries,24 and surgery is an essential part of treatment. Severe acute postoperative pain is associated with longer hospitalization and increased health care costs.8,40 It also affects the patients' quality of life and increases the risk of persistent pain.10,20,31
Factors associated with acute postsurgical pain are known to some extent. A review23 suggests that 4 significant factors associate with postoperative pain intensity across surgery types: preoperative pain, anxiety, age, and type of surgery. High levels of preoperative anxiety,14,23,25,41 psychological distress, and maladaptive coping style after surgery are known risk factors for higher intensity of acute postoperative pain in general.12,35,38 Earlier studies exploring factors associating with acute postoperative pain after breast cancer surgery11,25,34,35 have used one measurement or the mean of several measures as indicators of acute pain. Chapman et al.15 have suggested that pain trajectories consisting of both the intensity and the direction of the pain path would give a more precise picture of the course of acute pain.
Pain expectation has been suggested to affect the intensity of acute pain.19,30,35,38,39,45 Expectations can lead to both psychological and physiological responses.28,47 Pain expectation is related to other psychological factors such as anxiety, but it may also directly affect the experience of pain intensity.28,35 Koyama et al.29 have suggested that a person's mental representation of the upcoming sensation of pain modulates the neural processes and influences the actual sensation of pain. The expectation of pain partially activates the same areas of the brain that actual pain does.4,5,29 It is also known that the expectation of a high intensity of pain may lead to heightened attention and awareness toward pain because of its natural threat value.17,48
The aim of this study was to describe pain trajectories: the intercept and the slope of a linear trend for pain intensities recorded during the first postoperative week after breast cancer surgery and to identify factors that are associated with acute pain trajectories. Because trajectories are potentially good indicators for pain chronification,1 we explored more thoroughly the factors that contribute to pain trajectories characterized by high pain intercepts (high pain intensity) and unfavorable slopes (poor resolution of pain). We examined factors that are easy to screen during the preoperative and perioperative phase: demographic and surgery-related factors, oxycodone consumption in the immediate postoperative period, pain expectation, and psychological distress expressed as depressive symptoms and anxiety. We also studied the association of pain expectation with both clinical and experimental pain variables. The aim was to evaluate whether patients with high pain expectations are more sensitive to pain stimulation in general. By identifying the patients who are at the highest risk for acute postoperative pain, ultimately, we could offer more personalized care and target limited resources more accurately.
The main hypothesis was that expecting more severe postoperative pain and having high preoperative distress would have a significant impact on acute postoperative pain trajectories.
2. Materials and methods
2.1. Patients
Patients were recruited at the Breast Surgery Unit of the Helsinki University Central Hospital. Women aged 18 to 75 years with histologically proven newly diagnosed invasive breast cancer (T1-4 N0-3 M0) and who were to undergo either mastectomy or breast-conserving surgery, with sentinel node biopsy, axillary clearance, or both were recruited to the study. None of the patients had oncoplastic breast-conserving procedures or immediate reconstruction. Patients had to be fluent in Finnish. Of the 1536 eligible consecutive patients, 1149 patients were asked to participate in the study. One hundred twenty-six patients declined and 23 patients were withdrawn: 12 patients due to a contraindication to the anesthetic protocol, 6 patients because of change in the type of surgery or violation of the protocol, and 5 patients for logistic reasons. After the initiation of the study, a total of 567 patients were asked to assess the amount of pain they expected to have after surgery (NRS 0-10). Four of these patients were excluded because the final histology of the surgical specimen showed no cancer. Thus, 563 patients form the cohort of the current report. The whole cohort of 1000 patients has been described in more detail earlier.26 Oral and written consent was obtained from all patients. The Coordinating Ethics Committee of the Helsinki University Central Hospital approved the study protocol. The patients were operated on between August 2006 and December 2010.
2.2. Questionnaires and treatment-related data
The patients met a research nurse 1 to 3 days before surgery. After giving informed consent, patients filled in the questionnaires. Background data included age, height, and weight calculated as body mass index (BMI), number of previous operations (other than breast surgery), number of previous breast operations, previous chronic pain condition of any kind (eg, fibromyalgia, low back pain, headaches), and smoking (never, yes, stopped, or periodic).
The patient was also asked to report on a Numerical Rating Scale (NRS 0-10) if she currently had any pain in the area to be operated on. Intensity of pain was recorded in 3 separate regions: the breast, the axilla, and the upper arm. The highest rating in any one of these locations was used as an indication of pain intensity (“worst pain”). Psychological questionnaires were also included. Sum scores of the Beck Depression Inventory (BDI)6 and the State-Trait Anxiety Inventory (STAI state and STAI trait)46 were calculated. A preoperative question regarding the patient's expectation of pain was asked using an NRS scale of 0 to 10: “how much pain you expect to have after the operation?”
After surgery, the patients' records were reviewed for the type of surgery (breast resection with sentinel node biopsy, breast resection with axillary clearance, mastectomy with sentinel node biopsy, mastectomy with axillary clearance).
2.3. Experimental pain
The research nurse performed the experimental cold and heat pain tests before surgery. After explaining the tests carefully to the patients, cold pain was measured by immersing the hand and wrist contralateral to surgery in a circulating cold water bath (2°C-4°C) (JULACO USA Inc, Allentown, PA) for the maximum time the patient could tolerate but no longer than 90 seconds. Total time to withdrawal was measured. Patients assessed the intensity of pain (NRS 0-10) every 15 seconds during the test and at withdrawal.
Contact heat pain intensity was measured using the 16 × 16 mm2 thermode of the TSA-II NeuroSensory Analyzer (Medoc Ltd, Ramat Yishai, Israel). We exposed the volar side of the forearm contralateral to surgery for 5 seconds to temperatures of 43°C and 48°C, once each. Patients assessed the intensity of pain (NRS 0-10) at the end of the test.
2.4. Anesthesia
The standardized anesthetic protocol was developed in collaboration with the treating anesthesiologists who were either members of the research team of who were supervised by members of the research team. Also the breast surgeons were part of the research team (or supervised by members of the team). The patients were premedicated with diazepam 2.5 to 15 mg and acetaminophen 1 g orally. Anesthesia consisted of intravenous infusions of remifentanil, propofol, and the muscle relaxant rocuronium. During skin closure, fentanyl (1 μg/kg, intravenously [i.v.]), ondansetron (4 mg, i.v.), and dehydrobenzperidol (0.01 mg/kg, i.v.) were given. No regional or local anesthesia was used. Acetaminophen (1 g) was given orally every 8 hours as a basic analgesic, according to the clinical guidelines. We have described the anesthesia protocol in more detail in a previous publication.26
2.5. Postoperative pain
In the postanesthesia care unit, the research nurse titrated pain relief with intravenous oxycodone and on the ward the patients self-administered oxycodone through a patient-controlled analgesia device. The total consumption of oxycodone was recorded. The amount of oxycodone (mg/kg) that the patient needed to have satisfactory pain relief for the first time after surgery was used as a proxy for immediate postoperative pain for the statistical analyses. A more detailed report of the pain during the first 20 hours has been published before.26
At home, the patients were asked to record the intensity of pain in the operated area (NRS 0-10) 3 times daily (morning, day, evening) on days 1 to 7 after surgery. Pain was assessed in the same areas (the breast, the axilla, and the upper arm), and “worst pain” was calculated as before surgery. When leaving the hospital, the patients were given instructions to take 1 g of acetaminophen up to 3 times daily for postoperative pain and, if pain relief was not adequate, to take ibuprofen 600 mg up to 3 times daily. If ibuprofen was contraindicated, the patients were advised to replace acetaminophen by the combination tablet Panacod that contains 500 mg acetaminophen and 30 mg codeine. Daily use of acetaminophen 1 g, ibuprofen 600 mg, and Panacod was recorded on all 7 postoperative days and the total amount of daily medication was combined as one variable. The sum of the amount of consumed analgesics was used as an independent variable for the regression analyses to control its influence on postoperative pain.
2.6. Statistical analysis
SPSS software version 19.0.0.1 for Windows (SPSS Inc, Chicago, IL) was used to conduct descriptive statistics and patient subgroup comparisons. Descriptive statistics were calculated for all variables. Mean and standard deviation were used for normally distributed variables, medians (range) for nonnormally distributed variables, and number (percentage) for categorical data. Test of normality was conducted using the Kolmogorov–Smirnov test and by estimating skewness and kurtosis of all variables.
2.7. Psychological data
Singular missing items in psychological questionnaires were imputed, replacing the missing item with the mean value of the other items the person had answered. This was done because one missing answer would omit the patient totally from the statistical analyses, whereas imputing does not have a strong influence on the results. There were 60 psychological questionnaire items in total (BDI 20, STAI state 20, and STAI trait 20) that the patients answered. In most cases, there was only 1 missing item per person. If there were ≥20% of missing items per questionnaire, the patient's data were removed from the analyses. The number of missing data exceeded that criteria in 2 patients in BDI, 7 and 6 patients in STAI state and trait, respectively. Cronbach alpha coefficients were calculated to estimate the reliability (internal consistency) for the BDI, STAI state anxiety, and STAI trait anxiety scales. They were α = 90, α = 95, and α = 92, respectively. Three categories of anxiety scale scores were defined according to the STAI manual guidelines46: low (20-39), moderate (40-59), and high (60-80) anxiety for both STAI scales. Two categories were defined for the BDI in accordance with the BDI manual guidelines6: no or low depressive symptoms (0-18) and moderate or severe depressive symptoms (19-63). The categories of BDI and both STAI scales were combined to form a general measure of distress as follows: State and Trait Anxiety scales: low 0, moderate to high 1; and Depressive symptoms: low 0, moderate to severe 1. The range of the category sum scores was 0 to 3, a higher score indicating a higher level of distress.
2.8. Pain trajectories
The R statistical package (version 3.2.2) was used to calculate pain trajectories. Linear models were calculated using Python 2.7.11 module Statsmodels (version 0.6.1). The pain trajectory of each patient was summarized by a linear latent growth curve. Trajectories were formed to describe 2 features of pain during the first postoperative week: pain intercept that represents the intensity of pain on the hypothetical day zero assessment point and the slope that represents the change of the pain intensity with time. A negative slope indicates that pain is decreasing and a positive slope the opposite. These features were calculated by fitting a regression line across the pain measures of the 7 postoperative days using an ordinary least squares fit. This gives an approximation of the real pain trajectories and also simultaneously minimizes measurement error, which is always a source of bias when a person evaluates her pain level. The purpose of growth curve modelling is to individually estimate the dynamic course of acute pain. Similar to Chapman et al.,15 we also formed 3 slope groups regarding the direction of the curves: individual slope values with 50% confidence intervals (CIs) were calculated and slopes with CIs crossing value zero were defined as flat slopes, whereas entirely positive CIs were considered increasing slopes and entirely negative CIs were defined as decreasing slopes. This was done to describe the distribution of the studied patients into these 3 groups of different pain resolutions (slopes).
2.9. Regression analyses
We built 2 linear regression models, one to explain the intercept of the linear trend for each individual (hypothetical initial pain intensity) and the other to explain the change of the pain intensity with time (the slope). For both models, we chose the explanatory variables to include to the model, by fitting a simple linear regression model. Each variable associated individually with a liberal threshold (P < 0.2) was included in the multivariate models. Stepwise elimination was used to determine the variables in the final model.
2.10. Subgroup analyses
In addition to the linear regression analyses that defined factors associated with acute postoperative pain trajectories, we analyzed more closely the role of expectation and its relation to experimental pain variables and psychological variables. We used the Mann–Whitney U test to compare patients expecting severe postoperative pain (NRS ≥7/10) with those expecting no or mild pain (NRS ≤3/10). For experimental pain measures, we used NRS 0 to 10 at the end of the heat pain test and the total time the patients tolerated cold pain.
3. Results
The data of the 563 patients who were asked to rate their expectation of postsurgical pain were compared with those of the 433 patients who were not. The 2 groups differed only in one studied variable: the mean age of the patients who were not asked about their pain expectation was higher (in average by 17 months) than those who were asked (P = 0.027).
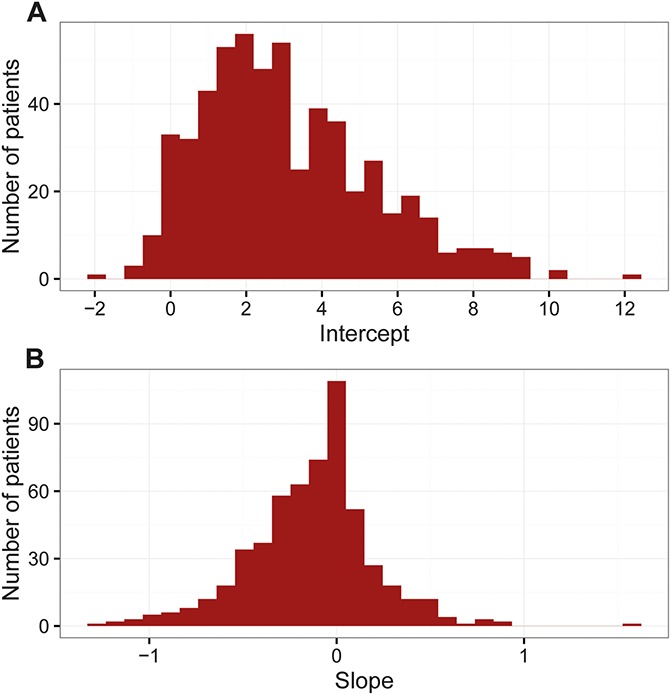
The descriptive background data are presented in Table 1. An analysis of the frequency distributions revealed that 7.6% of the patients reported moderate or severe pain (≥4/10) before surgery in the area to be operated. Figure 1A shows the distribution of the hypothetical initial pain intensities (the intercept), and Figure 1B shows the distribution of the pain resolutions (the slope). In 31.1% of the patients the pain remained quite stable over the first week (flat slope), in 19% of the patients pain increased over the week (positive slope), and in 49.7% the pain decreased over the week (negative slope). Figure 2 displays a scatter plot of how the intercept and the slope relate to each other. Of the majority of the patients who initially had more severe pain (high intercept), pain also resolved faster (negative slope). However, there was a small group of patients who had high initial pain intensity (high intercept) and the pain was still increasing over the week (positive slope). The average pain intercept and the slope were 3.1 (SD 2.30) and −0.13 (SD 0.33), respectively.
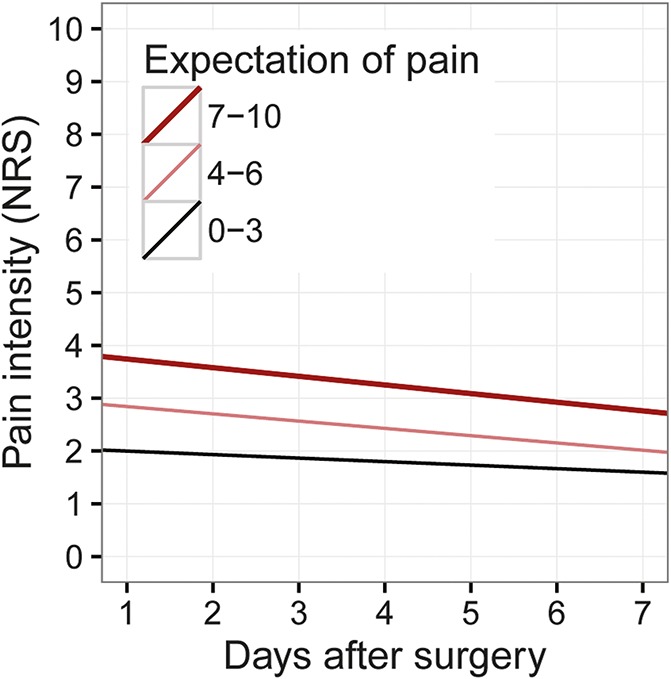
Table 1.
Descriptive data.
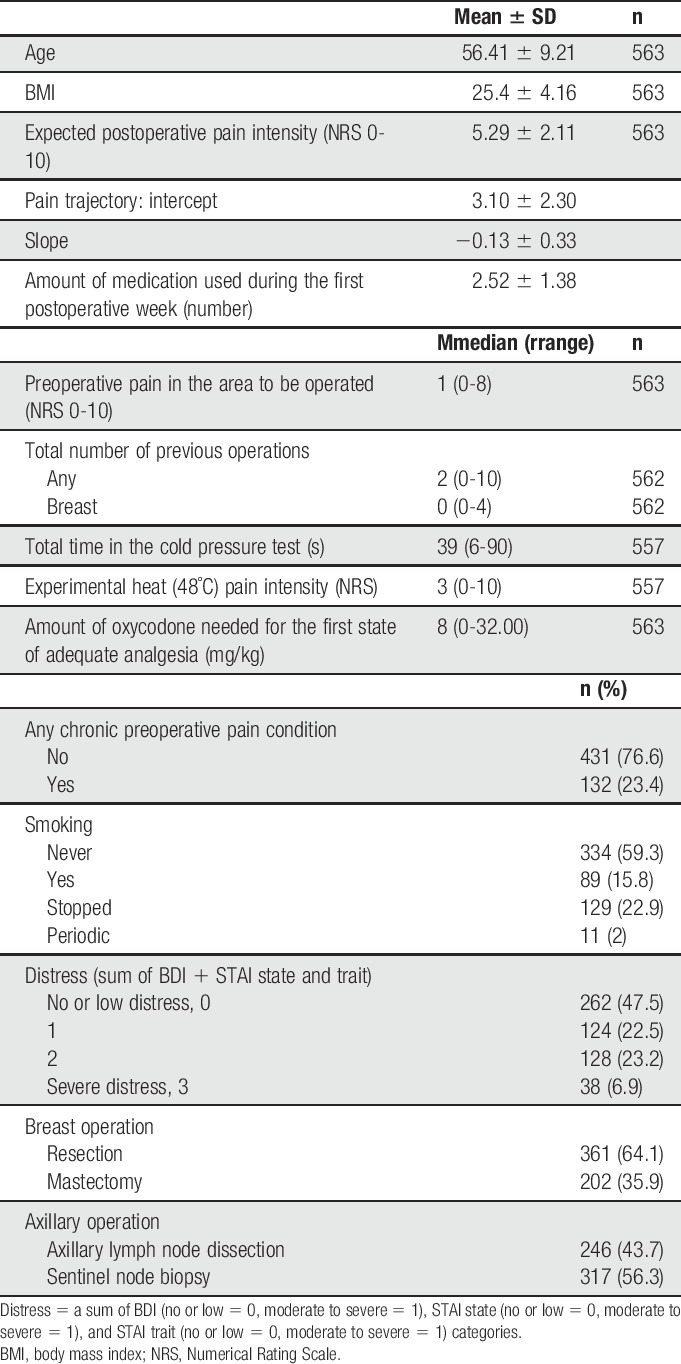
Figure 1.
(A) Distribution of the hypothetical initial pain intensities (intercept), n = 563. (B) Distribution of the changes of pain intensity over the first week (slope), n = 563.
Figure 2.
Jittered scatterplot showing the correlation between the hypothetical initial pain intensity (intercept) and change in pain intensity per day (slope), n = 563.
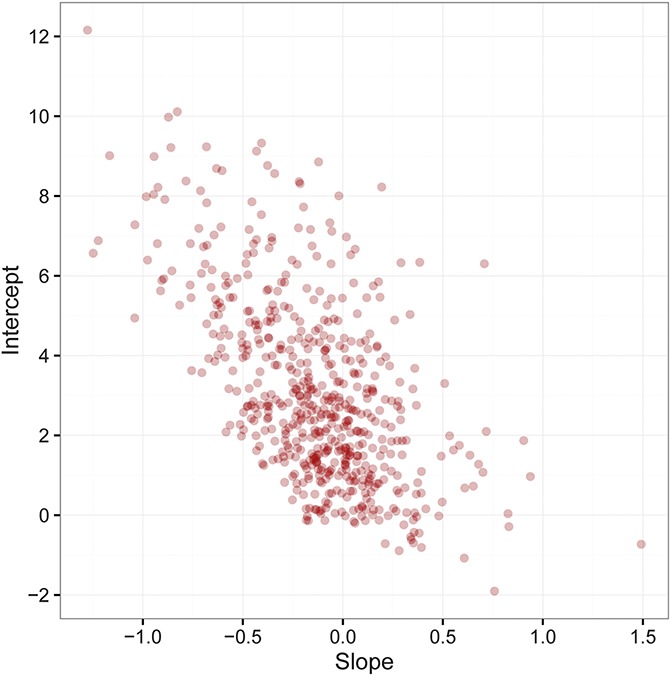
A majority of the patients, 84.4%, expected postoperative pain to be moderate to severe. Figure 3 shows the average pain trajectories of patients who expected postoperative pain intensity (0-3/10, 4-6/10, and 7-10/10). Patients who expected more severe pain had a higher average intercept (3.9, SD 2.6) compared with those who expected low pain (2.1, SD 2.6). However, pain also resolved slightly faster if the patient expected higher pain (β= −0.02, P = 0.02).
Figure 3.
The first week pain trajectories for patient groups expecting no or low, moderate, or severe postoperative pain. NRS, Numerical Rating Scale.
Frequency distributions of the categories for the psychological variables were as follows STAI state anxiety: low 52.9%, moderate 40.6%, and high 6.5%, and STAI trait anxiety: low 66.6%, moderate 31.4%, and high 2.6%. Most of the patients, 90.9%, had a BDI score indicating no or low depressive symptoms, and 9.1% had a score indicating moderate or severe depressive symptoms. When combining the distress categories, approximately half of the patients, 47.5%, reported no or mild symptoms in all of the questionnaires (distress category score 0; Table 1) and 6.9% of the patients scored moderate or high depressive symptoms and anxiety in all of the 3 questionnaires (category score 3; Table 1). The pain trajectories also varied according to the level of presurgery distress (Fig. 4). Patients with higher amount of psychological distress had higher pain intercepts. Also, patients with axillary clearance surgery had higher pain intercepts compared with sentinel node biopsy (Fig. 5).
Figure 4.
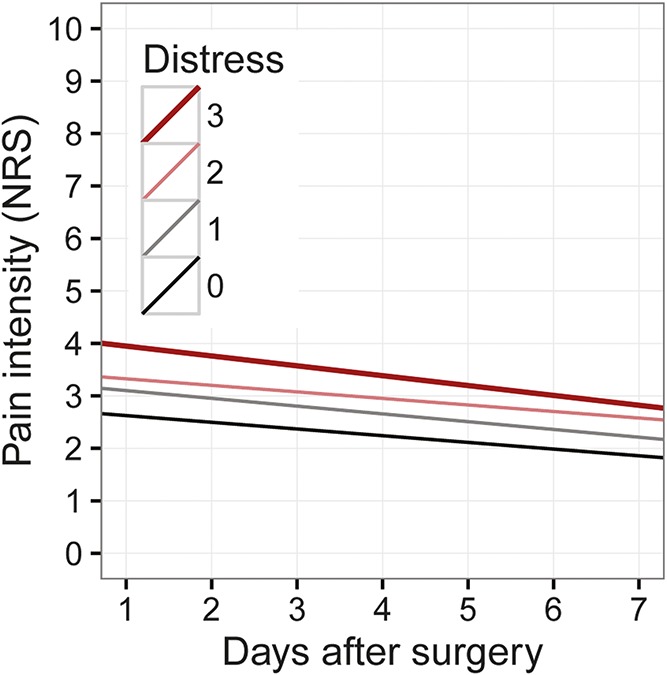
The first week pain trajectories for patient groups having different amount of preoperative distress (0 = no distress and 3 = severe distress). NRS, Numerical Rating Scale.
Figure 5.
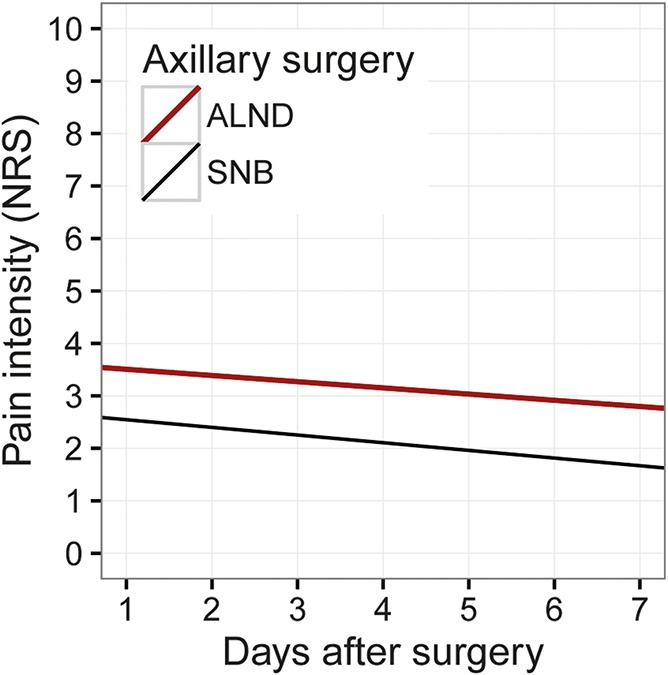
The first week pain trajectories representing women having either axillary clearance or sentinel node biopsy. ALND, axillary lymph node dissection; NRS, Numerical Rating Scale; SNB, sentinel node biopsy.
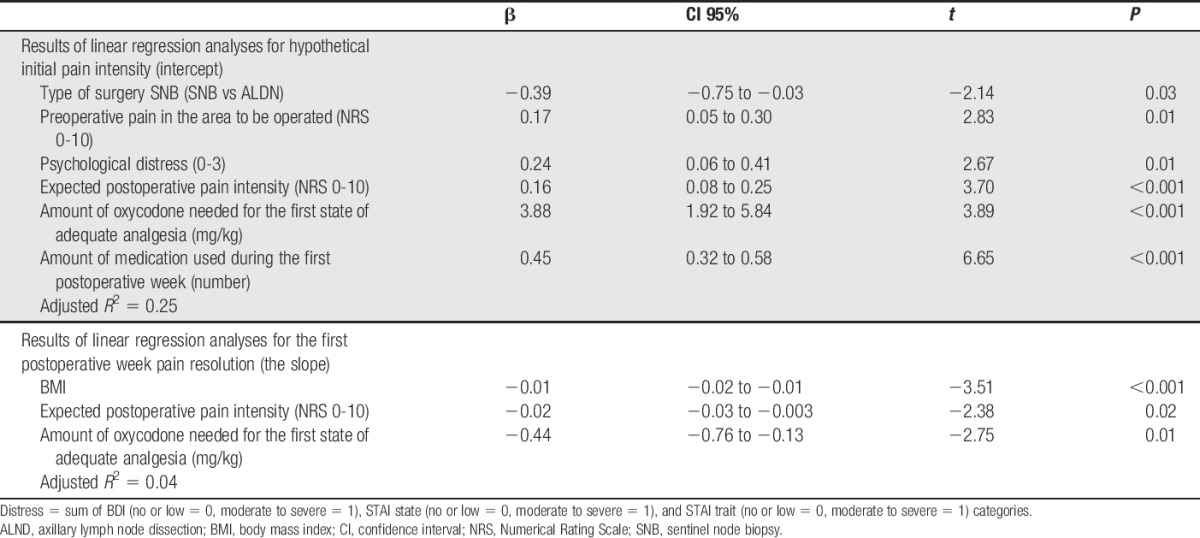
The variables that were chosen for inclusion in the initial regression model for hypothetical initial pain intensity (the intercept) were age, chronic preoperative pain condition (other pains), preoperative pain in the area to be operated, distress, the amount of expected postoperative pain intensity, smoking, the type of axillary surgery, and the amount of oxycodone needed for the first state of adequate analgesia. The explanatory variables chosen for inclusion in the regression model to explain the pain resolution (the slope) were BMI, the amount of expected postoperative pain intensity, type of breast surgery, smoking, and the amount of oxycodone needed for the first state of adequate analgesia. In both models, we controlled for the amount of medication used during the postoperative week
The results of the multivariate analyses are presented in Table 2. Of the preoperative factors, the type of axillary surgery, higher psychological distress, higher expectation of pain, higher preoperative pain intensity, and the amount of oxycodone needed for satisfactory pain relief for the first time after surgery were associated with higher initial pain intensity (the intercept). This model explained 25% of the variance of the intercept (adjusted R2 = 0.25). The variables that were associated with a more efficient pain resolution (the slope) were higher BMI, the expectation of higher levels of postoperative pain, and the amount of oxycodone needed for satisfactory pain relief for the first time after surgery. The adjusted R2 for these variables was 0.04.
Table 2.
Results of linear regression analyses for hypothetical initial pain intensity (intercept), and for the first postoperative week pain resolution (the slope).
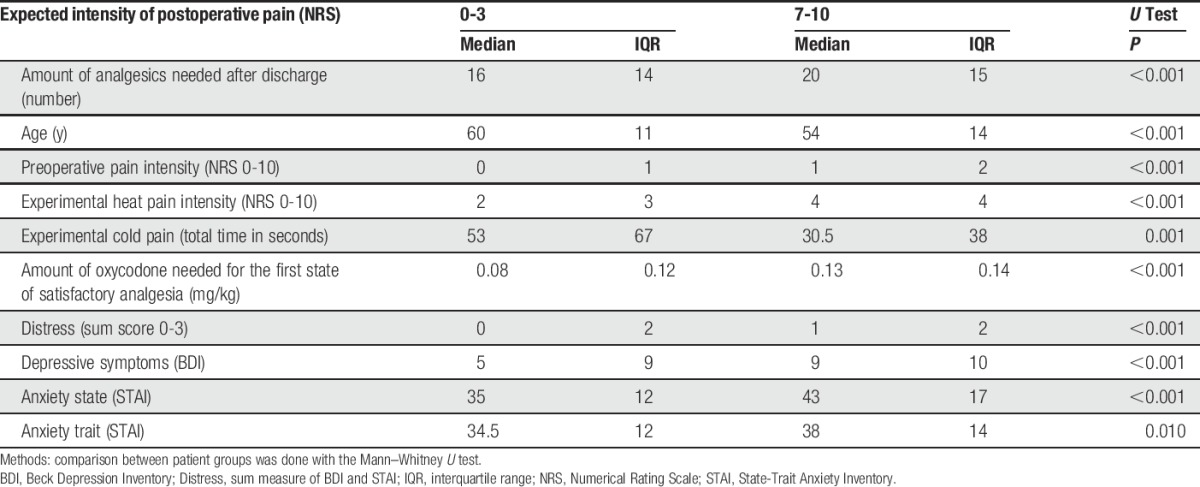
The results of the comparison of the 2 extremes of the pain expectation groups, patients expecting no or low pain intensity (≤3/10; N = 88) or expecting severe pain intensity (≥7/10; N = 160), are presented in Table 3. Patients expecting severe postoperative pain were, before surgery, statistically significantly more sensitive to heat pain, and more intolerant of cold pain. They were also younger, reported more preoperative pain, and had higher scores for depression (BDI), anxiety (STAI state and STAI trait), and distress combined. They also needed more oxycodone to be satisfied for the first time after the surgery and consumed more analgesics during the first postoperative week.
Table 3.
Descriptive data and comparison between groups expecting low (NRS 0-3) or high (NRS 7-10) postoperative pain.
4. Discussion
The aim of this prospective study was to describe acute pain trajectories after breast cancer surgery and to identify factors that were associated with trajectory variables. The hypothetical initial pain intensity (the intercept) and pain resolution (the slope) described in trajectories characterize the course of pain measures over days better than traditional single measure or mean of several measures.15 We wanted to identify factors that are easy to screen preoperatively and perioperatively to target interventions to those patients who are at risk of more intense or longer-lasting acute postoperative pain. In addition to preoperative factors, we wanted to determine whether the type of surgery and the amount of oxycodone needed to achieve the first state of adequate pain relief in the postanesthesia care unit could be used as predictors of initial pain intensity or as predictors of how the pain is resolving over the first postoperative week. Furthermore, we also wanted to better understand the association between pain, including experimental pain, and psychological factors: pain expectation and distress. We did not include experimental pain sensitivity in the multivariate model because the method is not feasible in a clinical setting, and our aim was to identify clinically useful methods for assessing the factors associated with postsurgical pain. However, the information from the experimental pain tests was used to better understand the relationship between pain expectations and pain sensitivity in general.
The results support our main hypotheses: expectations of higher postoperative pain and high preoperative distress predict more intense postoperative pain (intercept) after breast cancer surgery. Other variables predicting more intense postoperative pain included type of surgery (axillary clearance), preoperative pain in the area of the operation, and the amount of oxycodone needed to obtain the first state of adequate pain relief. Furthermore, factors associated with a more rapid pain resolution were higher BMI, higher pain expectations, and a higher amount of oxycodone needed. The overall result of the trajectory model was that the relationship between the 2 trajectory variables was negative: the higher the pain intensity initially was, the faster it resolved over the week. This finding is consistent with a previous study done with different surgical procedures.1
Factors that were significantly associated with the slope explained only 4% of the variance. This underlines the diversity of factors affecting the course of postsurgical pain. In approximately one fifth of the patients, the pain increased over the week. This is more than in earlier studies1,15 done with different surgical procedures, which may explain the disparate results. In this study, we combined state anxiety, trait anxiety, and depressive symptoms to form one variable, thus aiming to create a measure of general psychological distress. Psychological distress is an understandable and very common reaction to severe health problems such as breast cancer.33,36,42 The results of our study are quite consistent with previous studies emphasizing the role of psychological variables such as anxiety, depression, distress, and also pain expectations for acute pain after surgery, regardless of methods and research settings.11,25,34,35,39
Our results also suggest that pain expectations are influenced by both pain sensitivity and psychological factors. Those patients who expected very severe postoperative pain (NRS ≥7/10) were more distressed, reported more pain on all pain variables including preoperative pain and experimental pain tests, needed more oxycodone to achieve adequate pain relief for the first time in the postanesthesia care unit, and reported more intense postoperative pain. They also consumed more analgesics during the postoperative week.
Our results are in line with a study that showed that more distressed individuals (healthy volunteers) were more vigilant toward experimental pain.22 The expectation of pain plausibly reflects the tendency toward hypervigilant behavior.17 The tendency to focus attention on pain may be even stronger in patients with breast cancer, compared with patients with nonmalignant pain, because for most women, breast cancer represents a serious threat. It has been previously shown that the fear of pain naturally directs more attention toward pain sensation.7,27 Unfortunately, we did not specifically ask about the patients' fearful thoughts. Our study suggests that the patients who expected to have severe postoperative pain intensity were more sensitive to experimental pain, as well as to clinical pain. These results merit further studies regarding, eg, whether genetic factors or previous adverse experiences can explain some of these associations.
The relationship between pain, psychological distress, and pain expectations is important to consider when interventions are planned. Brown et al.9 showed that by interfering with negative expectation of pain, they were able to diminish pain ratings in experimental pain tests. It is possible that the expectation of pain also reflects fears and worries about whether pain medication will relieve postsurgical pain. In clinical settings, positive information about the effectiveness of analgesics16 and attentional training,37,43 teaching the patient to have a better control over pain-related thoughts and feelings, may decrease both fear and expectation of pain.
Clinicians should be aware that the majority of the patients in this study expected to have clinically significant pain after the surgery, but less than half of the patients actually experienced such pain. The subgroup of patients with high pain expectations needs to be studied further to understand the underlying mechanisms. In the clinic, expectations of severe postoperative pain need to be noted before breast cancer surgery, especially in patients with high distress. The clinician should be alerted to the importance of adequate and supportive information about the upcoming surgery. If the information given by medical professionals about the surgery and its possible adverse effects leads to heightened anxiety, fear, and expectations of postoperative pain, this may function as a nocebo to the patient.
Our study is consistent with previous studies showing that preoperative pain in the area to be operated on is a risk factor for both acute and persistent pain.18,19,21,32,44,45 Preoperative pain can be related to regional inflammation caused by the tumor.13 The reported severity of preoperative pain and higher expectations of postsurgical pain may also be linked to each other. In this study, most of the patients who expected to have postoperative pain (≥4/10) also reported more pain preoperatively. The effects of preoperative pain may be partially explained by heightened awareness toward sensations in the breast diagnosed for cancer and a hypervigilant reaction toward pain.17 However, the mechanisms are probably multifactorial and are not as yet fully understood. Preoperative pain in the breast area is an easy signal for the clinician to assess and important to recognize, especially when it appears along with distress and negative expectations.
Axillary clearance is a well-established risk factor for both acute and persistent postoperative pain.2,3,25 This may be explained by the more extensive surgery in the axilla, with potential injuries to the sensory intercostobrachial nerves and by the dissection of lymphatics also from the arm, potentially causing lymphedema. However, according to our results, axillary clearance is not associated with a more negative pain resolution over the first week.
Pain trajectories have been suggested to have a mediating role for pain persistence.1 This is an interesting hypothesis and future studies on breast cancer surgery-related pain should address this. Further studies also are needed to look more closely at subgroups of patients with different slopes and at the causal relationships of different slopes to acute and persistent pain.
This study has several shortcomings. Expectations of pain were not assessed in all patients in the original cohort. There was a statistically significant difference in age between those who provided ratings of expected pain and those who did not. Nonraters were on average 17 months older than raters. This is possibly a random phenomenon without clinical relevance. Our method of assessing distress was quite long and likely not feasible in daily clinical routine. A thorough assessment of depression and anxiety may be tedious for both the clinician and the patient. Simpler methods for screening overall psychological distress are needed for easier use in the clinical setting. Asking the patients about their concerns and fears about the upcoming surgery and pain might have yielded more information. We did not ask about the intensity of pain at home in relation to specific situations such as at rest or during movement; instead, our patients simply were asked to rate their overall intensity of pain. Also, participation in a study may provide the patient with a sense of security and ease psychological distress, which may be a possible source of bias.
5. Conclusions
The results of this prospective study with a large sample of women highlight that acute pain after breast cancer surgery is a multidimensional problem. Psychological distress, pain expectations, and patients' reports of preoperative pain in the area to be operated on should be recognized and assessed before surgery. Moreover, patients who have axillary clearance need more efficient analgesic approaches. Clinicians need to be alerted to these risk factors and take measures to minimize their influence.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Acknowledgements
The authors are grateful to research nurses Eija R. Ruoppa and Minna Kaiponen, Department of Anesthesia, Helsinki University Hospital, for the invaluable assistance and devotion to this project. The authors are grateful to Leslie Hearn, MSc, for his valuable help in proofreading the manuscript.
This study was supported by grants from the Academy of Finland (110489, 217028, 139795), Signe and Ane Gyllenberg Foundation, Helsinki University Central Hospital Research Funds (TYH2008225, TYH2010210, TYH2012212) and European Union Seventh Framework Program (FP7) under grant agreement no. 602891.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- [1].Althaus A, Arranz Becker O, Neugebauer E. Distinguishing between pain intensity and pain resolution: using acute post-surgical pain trajectories to predict chronic post-surgical pain. Eur J Pain 2014;18:513–21. [DOI] [PubMed] [Google Scholar]
- [2].Andersen KG, Duriaud HM, Jensen HE, Kroman N, Kehlet H. Predictive factors for the development of persistent pain after breast cancer surgery. PAIN 2015;156:2413–22. [DOI] [PubMed] [Google Scholar]
- [3].Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: a critical review of risk factors and strategies for prevention. J Pain 2011;12:725–46. [DOI] [PubMed] [Google Scholar]
- [4].Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain 2005;9:463–84. [DOI] [PubMed] [Google Scholar]
- [5].Atlas LY, Wager TD. How expectations shape pain. Neurosci Lett 2012;520:140–8. [DOI] [PubMed] [Google Scholar]
- [6].Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- [7].Boersma K, Linton SJ. Expectancy, fear and pain in the prediction of chronic pain and disability: a prospective analysis. Eur J Pain 2006;10:551–7. [DOI] [PubMed] [Google Scholar]
- [8].Brodner G, Van Aken H, Hertle L, Fobker M, Von Eckardstein A, Goeters C, Buerkle H, Harks A, Kehlet H. Multimodal perioperative management–combining thoracic epidural analgesia, forced mobilization, and oral nutrition–reduces hormonal and metabolic stress and improves convalescence after major urologic surgery. Anesth Analg 2001;92:1594–600. [DOI] [PubMed] [Google Scholar]
- [9].Brown CA, Seymour B, Boyle Y, El-Deredy W, Jones AKP. Modulation of pain ratings by expectation and uncertainty: behavioral characteristics and anticipatory neural correlates. PAIN 2008;135:240–50. [DOI] [PubMed] [Google Scholar]
- [10].Bruce J, Thornton AJ, Powell R, Johnston M, Wells M, Heys SD, Thompson AM, Cairns Smith W, Chambers WA, Scott NW; Recovery Study Group. Psychological, surgical, and sociodemographic predictors of pain outcomes after breast cancer surgery: a population-based cohort study. PAIN 2014;155:232–43. [DOI] [PubMed] [Google Scholar]
- [11].Bruce J, Thornton AJ, Scott NW, Marfizo S, Powell R, Johnston M, Wells M, Heys SD, Thompson AM. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer 2012;107:937–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Burns J, Moric M. Psychosocial factors appear to predict postoperative pain: interesting, but how can such information be used to reduce risk? 2011;15:90–9. [Google Scholar]
- [13].Cabodi S, Taverna D. Interfering with inflammation: a new strategy to block breast cancer self-renewal and progression? Breast Cancer Res 2010;12:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Caumo W, Schmidt AP, Schneider CN, Bergmann J, Iwamoto CW, Adamatti LC, Bandeira D, Ferreira MB. Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand 2002;46:1265–71. [DOI] [PubMed] [Google Scholar]
- [15].Chapman CR, Donaldson GW, Davis JJ, Bradshaw DH. Improving individual measurement of postoperative pain: the pain trajectory. J Pain 2011;12:257–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Colloca L, Benedetti F. How prior experience shapes placebo analgesia. PAIN 2006;124:126–33. [DOI] [PubMed] [Google Scholar]
- [17].Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull 1999;125:356–66. [DOI] [PubMed] [Google Scholar]
- [18].Gerbershagen HJ, Rothaug J, Kalkman CJ, Meissner W. Determination of moderate-to-severe postoperative pain on the numeric rating scale: a cut-off point analysis applying four different methods. Br J Anaesth 2011;107:619–26. [DOI] [PubMed] [Google Scholar]
- [19].Gramke HF, de Rijke JM, van Kleef M, Kessels AG, Peters ML, Sommer M, Marcus MA. Predictive factors of postoperative pain after day-case surgery. Clin J Pain 2009;25:455–60. [DOI] [PubMed] [Google Scholar]
- [20].Hickey OT, Burke SM, Hafeez P, Mudrakouski AL, Hayes ID, Shorten GD. Severity of acute pain after breast surgery is associated with the likelihood of subsequently developing persistent pain. Clin J Pain 2010;26:556–60. [DOI] [PubMed] [Google Scholar]
- [21].Hoofwijk DM, Fiddelers AA, Peters ML, Stessel B, Kessels AG, Joosten EA, Gramke HF, Marcus MA. Prevalence and predictive factors of chronic postsurgical pain and poor global recovery one year after outpatient surgery. Clin J Pain 2015;31:1017–25. [DOI] [PubMed] [Google Scholar]
- [22].Huber C, Kunz M, Artelt C, Lautenbacher S. Attentional and emotional mechanisms of pain processing and their related factors: a structural equations approach. Pain Res Manag 2010;15:229–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2009;111:657–77. [DOI] [PubMed] [Google Scholar]
- [24].Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. [DOI] [PubMed] [Google Scholar]
- [25].Katz J, Poleshuck EL, Andrus CH, Hogan LA, Jung BF, Kulick DI, Dworkin RH. Risk factors for acute pain and its persistence following breast cancer surgery. PAIN 2005;119:16–25. [DOI] [PubMed] [Google Scholar]
- [26].Kaunisto MA, Jokela R, Tallgren M, Kambur O, Tikkanen E, Tasmuth T, Sipila R, Palotie A, Estlander AM, Leidenius M, Ripatti S, Kalso EA. Pain in 1,000 women treated for breast cancer: a prospective study of pain sensitivity and postoperative pain. Anesthesiology 2013;119:1410–21. [DOI] [PubMed] [Google Scholar]
- [27].Keogh E, Thompson T, Hannent I. Selective attentional bias, conscious awareness and the fear of pain. PAIN 2003;104:85–91. [DOI] [PubMed] [Google Scholar]
- [28].Kirsch I. Response expectancy as a determinant of experience and behavior. Am Psychol 1985;40:1189–202. [Google Scholar]
- [29].Koyama T, McHaffie JG, Laurienti PJ, Coghill RC. The subjective experience of pain: where expectations become reality. Proc Natl Acad Sci U S A 2005;102:12950–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Logan DE, Rose JB. Is postoperative pain a self-fulfilling prophecy? Expectancy effects on postoperative pain and patient-controlled analgesia use among adolescent surgical patients. J Pediatr Psychol 2005;30:187–96. [DOI] [PubMed] [Google Scholar]
- [31].Masselin-Dubois A, Attal N, Fletcher D, Jayr C, Albi A, Fermanian J, Bouhassira D, Baudic S. Are psychological predictors of chronic postsurgical pain dependent on the surgical model? A comparison of total knee arthroplasty and breast surgery for cancer. J Pain 2013;14:854–64. [DOI] [PubMed] [Google Scholar]
- [32].Meretoja TJ, Leidenius MH, Tasmuth T, Sipila R, Kalso E. Pain at 12 months after surgery for breast cancer. JAMA 2014;311:90–2. [DOI] [PubMed] [Google Scholar]
- [33].Montgomery GH, Bovbjerg DH. Expectations of chemotherapy-related nausea: emotional and experiential predictors. Ann Behav Med 2003;25:48–54. [DOI] [PubMed] [Google Scholar]
- [34].Montgomery GH, Bovbjerg DH. Presurgery distress and specific response expectancies predict postsurgery outcomes in surgery patients confronting breast cancer. Health Psychol 2004;23:381–7. [DOI] [PubMed] [Google Scholar]
- [35].Montgomery GH, Schnur JB, Erblich J, Diefenbach MA, Bovbjerg DH. Presurgery psychological factors predict pain, nausea, and fatigue one week after breast cancer surgery. J Pain Symptom Manage 2010;39:1043–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Montgomery GH, Weltz CR, Seltz M, Bovbjerg DH. Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. Int J Clin Exp Hypn 2002;50:17–32. [DOI] [PubMed] [Google Scholar]
- [37].Morley S, Shapiro DA, Biggs J. Developing a treatment manual for attention management in chronic pain. Cogn Behav Ther 2004;33:1–11. [DOI] [PubMed] [Google Scholar]
- [38].Pan PH, Coghill R, Houle TT, Seid MH, Lindel WM, Parker RL, Washburn SA, Harris L, Eisenach JC. Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Anesthesiology 2006;104:417–25. [DOI] [PubMed] [Google Scholar]
- [39].Pan PH, Tonidandel AM, Aschenbrenner CA, Houle TT, Harris LC, Eisenach JC. Predicting acute pain after cesarean delivery using three simple questions. Anesthesiology 2013;118:1170–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002;95:627–34, table of contents. [DOI] [PubMed] [Google Scholar]
- [41].Pinto PR, McIntyre T, Ferrero R, Almeida A, Araujo-Soares V. Risk factors for moderate and severe persistent pain in patients undergoing total knee and hip arthroplasty: a prospective predictive study. PLoS One 2013;8:e73917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Schubart JR, Emerich M, Farnan M, Stanley Smith J, Kauffman GL, Kass RB. Screening for psychological distress in surgical breast cancer patients. Ann Surg Oncol 2014;21:3348–53. [DOI] [PubMed] [Google Scholar]
- [43].Sharpe L, Ianiello M, Dear BF, Nicholson Perry K, Refshauge K, Nicholas MK. Is there a potential role for attention bias modification in pain patients? Results of 2 randomised, controlled trials. PAIN 2012;153:722–31. [DOI] [PubMed] [Google Scholar]
- [44].Sipila R, Estlander AM, Tasmuth T, Kataja M, Kalso E. Development of a screening instrument for risk factors of persistent pain after breast cancer surgery. Br J Cancer 2012;107:1459–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Sommer M, de Rijke JM, van Kleef M, Kessels AG, Peters ML, Geurts JW, Patijn J, Gramke HF, Marcus MA. Predictors of acute postoperative pain after elective surgery. Clin J Pain 2010;26:87–94. [DOI] [PubMed] [Google Scholar]
- [46].Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, Jacobs AG, editors. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto: Consulting Psychologists Press, Inc., 1983. [Google Scholar]
- [47].Tracey I. Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nat Med 2010;16:1277–83. [DOI] [PubMed] [Google Scholar]
- [48].Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. PAIN 2000;85:317–32. [DOI] [PubMed] [Google Scholar]


