Abstract
Objectives:
To study the ocular manifestations in patients diagnosed with leukemia or myeloproliferative disorders and to derive an association between the ocular manifestations and hematological parameters of the patients.
Materials and Methods:
This observational and descriptive study was conducted in a Tertiary Care Center of Dehradun, North India over a period of 1 year. All the diagnosed cases of leukemia and myeloproliferative diseases attending the Oncology Department were included. Patients underwent a detailed ocular examination. The hematological parameters were also recorded including hemoglobin (Hb), total leukocyte count (TLC), and platelet count.
Results:
The study included 102 patients out of which, there were 66 males (64.7%), and 36 were females (35.3%) with an age range of 5–80 years. A total of forty patients showed ocular manifestations (39.3%). Extraocular manifestations were seen in 10.8% patients while intraocular manifestations were noted in 45.1% patients of acute leukemia and 7.7% patients of chronic leukemia. These ocular manifestations showed a significant association with low Hb (P = 0.000), raised TLC (P = 0.004), and low platelet count (P = 0.000). The most common ocular manifestation was intraretinal hemorrhages followed by roth spots. Among acute myeloid leukemia patients (23.5%), the presence of intraretinal hemorrhages was significantly associated with low Hb (Mann–Whitney U-test = 25.000, P = 0.007). The patients of acute lymphoblastic leukemia (25.4%) showed significant association between intraretinal hemorrhages and low platelet count (Mann–Whitney U-test = 44.000, P = 0.046) and roth spots with low Hb (Mann–Whitney U-test = 11.000, P = 0.000). Ocular manifestations were more commonly seen in acute leukemias as compared to chronic leukemias.
Conclusion:
Ocular examination is recommended in all leukemic patients as ocular manifestations may go unnoticed, most patients being asymptomatic and could be an early sign of worsening of disease.
Keywords: Leukemia, myeloproliferative disorders, ocular manifestations, Leucémie, troubles myéloprolifératifs, manifestations oculaires
Résumé
Objectifs:
étudier les manifestations oculaires chez les patients diagnostiqués avec la leucémie ou de troubles myéloprolifératifs et d’en tirer une association entre les manifestations oculaires et les paramètres hématologiques des patients.
Matériel et Méthodes:
Cette étude observationnelle et descriptive a été menée dans un centre de soins tertiaires de Dehradun, Inde du Nord sur une période de 1 an. Tous les cas diagnostiqués de leucémie et de maladies myéloprolifératifs assistant au département d’oncologie ont été inclus. Les patients ont subiune analyse détaillée des paramètres hématologiques examination. The oculaires ont également été enregistrées, y compris l’hémoglobine (Hb), nombre total de leucocytes (TLC), et la numération plaquettaire.
Résultats:
L’étude a inclus 102 patients sur lesquels, il y avait 66 hommes (64,7%), et 36 étaient des femmes (35,3%) avec une tranche d’âge des 5-80 ans. Un total de quarante patients ont montré des manifestations oculaires (39,3%). manifestations extraoculaires ont été observées chez 10,8% des patients alors que les manifestations intraoculaires ont été notées dans 45,1% des patients de courte durée leucémie et 7,7% des patients de leucémie chronique. Ces manifestations oculaires ont montré une association significative avec une faible Hb (P = 0,000), soulevé TLC (P = 0,004), et une faible numération plaquettaire (P = 0,000). La manifestation oculaire la plus fréquente était hémorragies intrarétiniennes suivie par des taches roth. Parmi les patients atteints de leucémie myéloïde aiguë (23,5%), la présence d’hémorragies intrarétiniennes était significativement associée à une faible Hb (Mann-Whitney U-test = 25,000, P = 0,007). Les patients de leucémie lymphoblastique aiguë (25,4%) ont montré une association significative entre les hémorragies intrarétiniennes et une faible numération plaquettaire (Mann-Whitney U-test = 44.000, P = 0,046) et des taches roth à faible Hb (Mann-Whitney U-test = 11.000, P = 0,000). Les manifestations oculaires ont été plus fréquemment observées dans les leucémies aiguës par rapport aux leucémies chroniques.
Conclusion:
Ocular examen est recommandé chez tous les patients leucémiques comme des manifestations oculaires peuvent passer inaperçues, la plupart des patients étant asymptomatiques et pourraient être un signe précoce d’une aggravation de la maladie.
Introduction
Leukemia is a malignant proliferative disorder of leukopoietic bone marrow stem cells. It is characterized by over-crowding of the bone marrow by immature neoplastic leukocytes and widespread infiltration of organs, tissues, and peripheral blood with immature leukocytes.[1] According to the Indian Council of Medical Research, there have been 229,811 males and 157,933 females suffering from the disease.[2] They can be classified on the basis of the type of white blood cells affected as lymphoid or myeloid leukemias and based on the clinical course of disease as acute or chronic leukemias.[3]
Knowledge of ocular involvement in leukemia is important because the eye is the only site where the leukemic involvement of nerves and blood vessels can be observed directly.[4] Liebreich was the first to described leukemic retinopathy in the 1860s. Ever since reports show that virtually all intraocular structures may be involved.[5,6] Patients have been reported with leukemic infiltrates of the optic nerve, choroid, retina, iris, ciliary body, and anterior chamber. Retinal changes can be related to direct invasion of tissue by neoplastic cells, to manifestations of associated hematological abnormalities such as anemia, thrombocytopenia, hyperviscosity states, to opportunistic infections, or to unrelated chance findings.[5] The ocular manifestations of leukemia can be divided into direct manifestations (leukemic infiltrates), possible direct manifestations (e.g., white-centered retinal hemorrhages/roth spots), manifestations of complications of leukemia (chiefly anemia, thrombocytopenia, and hyperviscosity states), opportunistic infections, and those related to medical therapy.[5] There is no literature available to describe the difference between manifestations of acute and chronic leukemia. Manifestations were found to be more common in acute leukemia in a study by Reddy et al.[7] while a study by Eze et al.[1] showed more ocular manifestations in chronic leukemia. The present study was carried out to assess ocular involvement in patients of leukemia and various myeloproliferative disorders and to derive an association between these ocular manifestations and hematological parameters of the patients.
Materials and Methods
The present study was conducted in the Department of Ophthalmology, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Dehradun, India over a period of 12 months, from January 2014 to December 2014. It was an observational descriptive study. All diagnosed cases of leukemia and myeloproliferative disorders presenting to Department of Oncology were included in the study after informed consent. These included acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), chronic lymphoblastic leukemia (CLL), non-Hodgkin's lymphoma (NHL), and multiple myeloma (MM).
Patients with a history of diabetes, hypertension, any intraocular surgeries in the past 3 months, autoimmune disorders, vascular occlusions, or hematological disorders were excluded from the study. The study was approved by the ethical committee of the Swami Ram Himalayan University.
Data collection
Data collection was done according to preset format. This included a demographic profile of the patient, medical history, record of hematological parameters including hemoglobin (Hb), total leukocyte count (TLC), and platelet count. The complete ophthalmic examination was done including best-corrected visual acuity (BCVA) on retro illuminated Snellen's chart, slit lamp biomicroscopy for the anterior segment and posterior segment evaluation by + 90D (Volk Optical Inc.), and indirect ophthalmoscope (Keeler Ltd., Winsor, UK). Posterior segment examination was performed after pupillary dilation with 1% tropicamide eye drops (Tropicacyl eye drops, Sunways India). Anterior and posterior segment photographs were taken for records except in patients unable to cooperate for clinical pictures. Intraocular pressure (IOP) was recorded with Goldmann applanation tonometer except in patients unable to rest chin on the slit lamp, in whom IOP was measured by tonopen (AVIA Reichert). In debilitated patients, initial examination was done bedside, and retinal examination was done using a direct ophthalmoscope (Welch Allyn, USA) and indirect ophthalmoscope. Patients were then examined in eye outpatient department if necessary.
Data management and statistical analysis
Interpretation and analysis of obtained results were carried out using IBM SPSS version 20, SPSS Inc., Chicago, Illinios, the USA for descriptive statistics. Association between ocular manifestation and hematological parameters was checked by Mann–Whitney U-test. Statistical significance of the data was checked at 5% level of significance, P < 0.05 taken as statistically significant.
Results
In this study, 102 patients diagnosed with leukemia and myeloproliferative disorders were included, out of which 64.7% patients were males, and 35.3% were females with male: female ratio of 1.8:1. Sixty-eight (66.7%) patient was newly diagnosed while 34 (33.3%) patients were existing patients on treatment. The patients were between the age ranges of 5–80 years (mean 39.27 ± 19.76 years). Table 1 shows the distribution of patients according to diagnosis, age, and sex.
Table 1.
Distribution of patients according to diagnosis, age, and sex
| Study groups | 0-20 years (%) | 21-40 years (%) | 41-60 years (%) | 61-80 years (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | |
| AML (n=24) | 5 (5) | 3 (3) | 7 (6.9) | 6 (6) | 2 (2) | 0 | 1 (1) | 0 |
| ALL (n=26 | 6 (6) | 5 (5) | 4 (4) | 5 (5) | 4 (4) | 2 (2) | 0 | 0 |
| CML (n=15) | 1 (1) | 0 | 3 (3) | 3 (3) | 4 (4) | 1 (1) | 2 (2) | 1 (1) |
| CLL (n=3) | 0 | 0 | 0 | 0 | 2 (2) | 0 | 1 (1) | 0 |
| NHL (n=15 | 2 (2) | 0 | 3 (3) | 2 (2) | 5 (5) | 1 (1) | 2 (2) | 0 |
| MM (n=19) | 0 | 0 | 0 | 1 (1) | 6 (6) | 1 (1) | 6 (6) | 5 (5) |
| Total | 14 (13.7) | 08 (7.8) | 17 (16.7) | 17 (16.7) | 23 (22.5) | 05 (5) | 12 (11.8) | 06 (5.8) |
AML=Acute myeloid leukemia, ALL=Acute lymphoblastic leukemia, CML=Chronic myeloid leukemia, CLL=Chronic lymphoblastic leukemia, NHL=Non-Hodgkin’s lymphoma, MM=Multiple myeloma
In the study group, 88 (86.3%) patients had BCVA 6/18 or more in better eye, 4 (4%) patients had visual acuity more than 3/60, and <6/18 in better eye while 10 (9.8%) patients had visual acuity <3/60 in their better eye. The mean IOP of the patients was 14.19 ± 3.960 mm of Hg.
Ocular manifestations were noted in 40 (39.3%) out of the 102 patients. Manifestations were broadly grouped as extraocular manifestations and intraocular manifestation. Extraocular manifestations were seen in 11 patients (10.8%) out of which subconjunctival hemorrhage being the most common. Ten patients with extraocular manifestation also had intraocular manifestation. Furthermore, the extraocular manifestations were most frequently seen in patients with acute leukemias (9.8%) as compared to chronic leukemias (1%) [Figure 1]. Patients of NHL and MM had no ocular findings.
Figure 1.
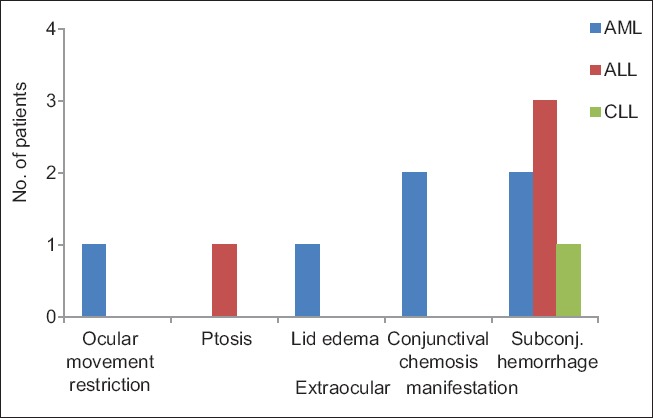
Extraocular manifestations in the study group (AML = Acute myeloid leukemia, ALL = Acute lymphoblastic leukemia, CLL = Chronic lymphoblastic leukemia)
Intraocular manifestations were more commonly seen than extraocular manifestations in this study. Thirty-nine patients had posterior segment involvement. Posterior segment was more commonly involved in acute leukemia (45.1%) than chronic leukemia (7.7%). The most common posterior segment finding was intraretinal hemorrhages seen in 32 (31.3%) patients, followed by Roth's spots seen in 26 (25.4%) patients [Table 2]. Eleven patients had preretinal bleed associated with intraretinal hemorrhage and roth spots while four patients had disc edema associated with intraretinal hemorrhage and roth spots.
Table 2.
Intraocular manifestations in the study group
| Intraocular findings (n=102) | AML (%) | ALL (%) | CML (%) | CLL (%) | Total (%) |
|---|---|---|---|---|---|
| Retinal hemorrhage | |||||
| Intraretinal hemorrhage | 5 (4.9) | 6 (5.9) | 2 (1.9) | 0 | 13 (12.7) |
| Roth spots | 4 (3.9) | 2 (1.9) | 0 | 1 (1) | 7 (6.8) |
| Both | 6 (5.9) | 9 (8.9) | 2 (1.9) | 2 (1.9) | 19 (18.6) |
| Disc edema | 2 (1.9) | 1 (1) | 1 (1) | 0 | 4 (3.9) |
| Preretinal bleed | 7 (6.9) | 4 (3.9) | 0 | 0 | 11 (10.8) |
AML=Acute myeloid leukemia, ALL=Acute lymphoblastic leukemia, CML=Chronic myeloid leukemia, CLL=Chronic lymphoblastic leukemia
Table 3 shows the association of ocular manifestations with mean hematological parameters. Ocular manifestations were significantly associated with low Hb (P = 0.000), raised TLC (P = 0.004), and low platelet count (P = 0.000).
Table 3.
Association of mean hematological parameters with ocular manifestations
| n=102 | Mean Hb (±SD) (mg/dl) | Mean TLC (±SD) (thousands/cumm) | Mean platelet (±SD) (thousands/cumm) |
|---|---|---|---|
| With ocular manifestations (n=40) | 7.35 (±2.81) | 84.16 (±132.9) | 75.16 (±78.39) |
| Without ocular manifestations (n=62) | 9.92 (±2.59) | 21.89 (±45.17) | 171.33 (±100.11) |
| Mann-Whitney U-test | 618.500 | 817.000 | 571.000 |
| P | 0.000 | 0.004 | 0.000 |
SD=Standard deviation, Hb=Hemoglobin, TLC=Total leukocyte count
Among 24 patients of AML, 16 patients (16%) had ocular manifestations and the occurrence of ocular manifestations showed a significant association with increased TLC (P = 0.05). Of 26 patients (25%) of ALL, 17 (16%) presented with ocular manifestations showing significant association with low Hb (P = 0.01) and low platelet count (P = 0.04). The number of CML patients with ocular manifestations was 4 (4%) out of 15 patients, and no association between blood parameters and manifestations could be derived in these patients. There were only three patients diagnosed with CLL with all three having ocular involvement. Association with hematological parameters could not be derived due to low number of patients [Table 4].
Table 4.
Association of mean hematological parameters with ocular manifestations in acute myeloid leukemia, acute lymphoblastic leukemia, and chronic myeloid leukemia
| Diagnosis (n=65) | Mean Hb (±SD) (mg/dl) | Mean TLC (±SD) (thousands/cumm) | Mean platelet (±SD) (thousands/cumm) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| With findings | Without findings | P | With findings | Without findings | P | With findings | Without findings | P | |
| AML (n=24) | 7.2 (±2.5) | 9.1 (±2.1) | 0.11 | 77.2 (±129.5) | 15.5 (±18.9) | 0.05 | 56.3 (±57.1) | 110.9 (±103.4) | 0.46 |
| ALL (n=26) | 7.6 (±3.1) | 10.3 (±2.6) | 0.01 | 78.6 (±113.7) | 9.2 (±10.6) | 0.20 | 69.5 (±84.2) | 195.5 (±154.8) | 0.04 |
| CML (n=15) | 8.8 (±2.3) | 9.3 (±2.1) | 0.79 | 192.4 (±234.4) | 81.13 (±85.5) | 0.43 | 96.8 (±110.6) | 158.2 (±130.0) | 0.29 |
AML=Acute myeloid leukemia, ALL=Acute lymphoblastic leukemia, CML=Chronic myeloid leukemia, Hb=Hemoglobin, TLC=Total leukocyte count, SD=Standard deviation
The most commonly noted posterior segment finding was intraretinal hemorrhages found in 32 patients (31.3%), followed by roth spots found in 26 patients (25.4%). Intraretinal hemorrhages were more commonly seen in acute leukemia (26 patients, 25.4%) than chronic leukemia (six patients, 5.8%). Among these, AML patients showed a significant association between intraretinal hemorrhages and low Hb while patients with ALL showed its significance with low platelet count. Among patients of chronic leukemia, no significant association between intraretinal hemorrhages and hematological parameters could be derived [Table 5].
Table 5.
Association of intraretinal hemorrhages with hematological parameters
| Diagnosis (n=65) | Mean Hb (±SD) (mg/dl) | Mean TLC (±SD) (thousands/cumm) | Mean platelet (±SD) (thousands/cumm) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intraretinal hemorrhages | Intraretinal hemorrhages | Intraretinal hemorrhages | |||||||
| Present | Absent | P | Present | Absent | P | Present | Absent | P | |
| AML (n=24) | 6.41 (±2.53) | 9.07 (±1.77) | 0.007 | 78.07 (±148.90) | 38.47 (±60.17) | 0.147 | 62.80 (±62.29) | 84.55 (±90.48) | 0.706 |
| ALL (n=26) | 7.82 (±3.25) | 9.62 (±3.02) | 0.102 | 87.13 (±118.82) | 10.25 (±10.68) | 0.287 | 72.34 (±89.61) | 168.81 (±150.72) | 0.046 |
| CML (n=15) | 8.87 (±2.34) | 9.29 (±2.06) | 0.794 | 192.45 (±234.47) | 81.13 (±85.55) | 0.433 | 96.83 (±110.65) | 158.25 (±130.04) | 0.117 |
AML=Acute myeloid leukemia, ALL=Acute lymphoblastic leukemia, CML=Chronic myeloid leukemia, Hb=Hemoglobin, TLC=Total leukocyte count, SD=Standard deviation
Roth spots were the second most frequently seen finding among patients. It was noted in 21 patients of acute leukemia (20.5%) and five patients of chronic leukemia (4.9%). Patients diagnosed with ALL showed a significant association between roth spots and low Hb while there was no significant association with the blood parameters of patients with AML. Association among patients of chronic leukemia could not be derived due to a small number of patients [Table 6].
Table 6.
Association of Roth spots with hematological parameters
| Diagnosis (n=50) | Roth spots | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Hb (±SD) (mg/dl) | Mean TLC (±SD) (thousands/cumm) | Mean platelet (±SD) (thousands/cumm) | |||||||
| Present | Absent | P | Present | Absent | P | Present | Absent | P | |
| AML (n=24) | 7.44 (±1.93) | 8.14 (±2.87) | 0.292 | 100.34 (±161.37) | 25.39 (±23.79) | 0.364 | 62.70 (±69.73) | 83.07 (±84.89) | 0.520 |
| ALL (n=26) | 6.08 (±2.01) | 10.42 (±2.67) | 0.000 | 80.11 (±109.78) | 35.90 (±85.93) | 0.169 | 65.86 (±77.42) | 147.83 (±145.42) | 0.186 |
AML=Acute myeloid leukemia, ALL=Acute lymphoblastic leukemia, Hb=Hemoglobin, TLC=Total leukocyte count, SD=Standard deviation
Discussion
Leukemia and lymphomas are disorders that may affect the eye. The ophthalmic symptoms and findings can be the initial manifestation of the systemic illness. There can be various direct and indirect manifestations of the disease which may go unnoticed, without any symptoms but may be vision threatening at the same time.[5]
Acute leukemia is a condition seen more commonly in younger age group in comparison to chronic leukemia. A similar finding was seen in this study, where the age of 102 patients ranged from 5 to 80 years, the mean age being 27.46 ± 15.24 years in acute leukemia, and 46.27 ± 17.53 years in chronic leukemia. Comparable ranges were stated by Guyer et al. (mean age 33.3 years)[8] and Reddy and Jackson (mean age 34.6 years)[4] in their studies done on acute leukemia.
There were 66 males (64.7%) and 36 females (35.3%) included in the study, thus showing male preponderance in all types of disorders except the acute leukemia (13% females in AML and 10% in ALL). This result was similar to results of a study by Querques et al.[9] where a female preponderance in AML patients was noted (54.4%). Results of male preponderance in other disorders were comparable in studies by Eze et al.[1] having 62.5% males and Omoti et al.[10] which had 66.1% males and 33.9% females, and Suresh et al. having 62.5% males.[11]
The cases of acute leukemia (48%) were more in the current study compared to chronic leukemia (18%). This result was supported by Suresh et al. having 87.5% patients with acute leukemia[11] and Koshy et al.[12] On the other hand, studies done by Eze et al.[1] and Omoti et al.[13] showed contrasting results (70.2% and 66.6% patients with chronic leukemia, respectively). This can be attributed to the fact that the incidence of chronic leukemia in Asia is lower than the western countries.[7,14]
The ocular involvement was seen in 32% in acute leukemia and 7% in chronic leukemia in this study. Reddy et al. in Malaysia documented ocular findings in 35.5% patients of acute leukemia. They, however, reported a higher percentage of involvement in chronic leukemia (34.9%)[7] than this study. A higher incidence of ocular manifestations was noted by Eze et al. in Nigeria where the ocular involvement was higher in chronic leukemia (70.9%) than acute leukemia (33.3%) owing to a higher hospital prevalence of chronic leukemia in Nigeria.[1]
Fourteen (13.7%) patients in this study had visual acuity <6/18 due to direct ocular involvement. In comparison, Eze et al.[1] reported a visual loss of 32.1% in their study while Schachat et al. reported a visual loss of 5%.[15] This difference in the percentage of visual loss in these studies probably reflects the unequal quality and assessbilitity to health care in different parts of the world, and studies from African subcontinent have reported higher leukemic retinopathy.[1,16]
The study included 15% patients of NHL and 19% patients of MM, which was comparable to reports of Holt and Gordon-Smith[17] having 14.4% of MM and Suresh et al. with 12.5% patients of MM in their study in Chennai.[11] Omoti et al.[10] reported that 31.4% patients of NHL in their study had ocular involvement. In this study, these patients showed no ocular involvement. This could be explained by the fact that these patients were already on treatment and had their hematological parameters within normal ranges.
Eleven out of 102 patients (10.8%) patients in the study group showed extraocular manifestations out of which 90.9% (ten patients) were of acute leukemia, and 9.1% (one patient) were from chronic leukemia. Similar results were reported by Reddy et al.[7] while results of Eze et al.[1] were found to be contrasting, with extraocular manifestations more commonly noted in patients of chronic leukemia. Owing to the higher number of patients of chronic leukemia in their study group.
Intraocular involvement was more common in this study and was more in acute leukemia. Comparable results were reported by Reddy et al., (33.7%)[7] Koshy et al., (51.9%)[12] and Suresh et al. (56.25%)[11] in their studies. Studies conducted on retinal involvement in leukemia and myeloproliferative disorders by Guyer et al.,[8] Reddy and Jackson[4] abu el-Asrar et al.,[18] and Querques et al.[9] noted retinal abnormalities in patients of acute leukemia and showed comparable results.
In this study, the most commonly noted posterior segment findings were intraretinal hemorrhages followed by roth spots. They were seen more in acute leukemia than chronic leukemia, and this was supported by results noted in a study done by Reddy and Jackson[4] and Suresh et al.[11] Preretinal bleed was seen in 10.8% patients in this study. Similar results were seen in a study done in Chennai[11] and studies done in Nigeria[1] and Malaysia.[4] In contrast to our study, where no ocular involvement was seen in patients of NHL, the study done by Omoti et al.[10] showed disc edema in 2% patients and optic atrophy in 2% patients.
Ocular manifestations in this study were significantly associated with low Hb, raised TLC, and low platelet counts. Holt and Gordon-Smith[17] in their study noted similar associations with low Hb and low platelet count but no association with raised TLC. Association of hematological parameters was further studied based on types of leukemia and types of hemorrhages.
Among the patients of acute leukemia where intraretinal hemorrhages were note in 26 patients, its significant association could be derived with low Hb (P = 0.007) in AML, the result being supported by Holt and Gordon-Smith (P < 0.01),[17] Guyer et al.(P = 0.05),[8] and Suresh et al.[11] Among patients of ALL, low Hb was not significantly associated with intraretinal hemorrhages. In these patients, low platelet count (P = 0.046) was found to be associated with intraretinal hemorrhages. Similar results were also reported by Reddy and Jackson[4] Guyer et al.,[8] and Holt and Gordon-Smith[17] On the other hand, abu el-Asrar et al.[18] and Suresh et al.[11] noted a significant association of intraretinal hemorrhage with low Hb, in the patients of ALL.
Roth spots were the second most common manifestation seen in 21 patients of acute leukemia. No association of roth spots with any hematological parameters could be derived in patients having AML. This result was supported by Guyer et al.[8] However, contrasting results were noted in studies conducted by Reddy and Jackson[4] and abu el-Asrar et al.,[18] where a strong relationship between roth spots and high TLC were noted. Patients of ALL in this study showed roth spots associated with low Hb. However, this result was dissimilar to that of Guyer et al. showing no association of roth spots with any of the three hematological parameters.[8]
There are few limitations of this study. This study was hospital-based, and the sample size was small. The study group consisted of both newly diagnosed cases and patients already on treatment.
Conclusion
The eye is the only site for direct visualization of visceral involvement and metastasis and also third most common extramedullary site for involvement.[12] In this study, 39.3% patients had ocular involvement. Ocular involvement is also considered to be the early sign of worsening of the disease process among the patients of leukemia and myeloproliferative disorders with lower survival rate.[19,20] Hence, there is a need for an ocular examination in all such patients to predict worsening and need for early intervention to provide a better quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Eze BI, Ibegbulam GO, Ocheni S. Ophthalmic manifestations of leukemia in a tertiary hospital population of adult Nigerian Africans. Middle East Afr J Ophthalmol. 2010;17:325–9. doi: 10.4103/0974-9233.71599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sinha S. Cancer in India: Prevalence, Management and Outcome. Prospects for Research. [Last accessed on 2016 Jan 16]. Available from: http://www.icmr.nic.in .
- 3.Pokharel M. Leukemia: A review article. IJARPB. 2012;2:397–407. [Google Scholar]
- 4.Reddy SC, Jackson N. Retinopathy in acute leukaemia at initial diagnosis: Correlation of fundus lesions and haematological parameters. Acta Ophthalmol Scand. 2004;82:81–5. doi: 10.1046/j.1600-0420.2003.00197.x. [DOI] [PubMed] [Google Scholar]
- 5.Do DV, Dhaliwal RS, Schachat AP. Leukemias and lymphomas. In: Ryan SJ, editor. Retina. Part 2. 5th ed. Vol. 3. China: Elsevier; 2013. pp. 2359–72. [Google Scholar]
- 6.Mateo J, Ascaso FJ, Núñez E, Peiro C, González G, Cristóbal JA. Faderl S, editor. Ophthalmological manifestations in acute lymphoblastic leukemia. Novel Aspects in Acute Lymphoblastic Leukemia. Croatia, European Union: InTech. 2011. [Last accessed on 2016 Feb 02]. Available from: http://www. intechopen.com/ books/novel-aspects-in-acute-lymphoblastic-leukemia/ophthalmologicalmanifestations- in-acutelymphoblastic-leukemia .
- 7.Reddy SC, Jackson N, Menon BS. Ocular involvement in leukemia - A study of 288 cases. Ophthalmologica. 2003;217:441–5. doi: 10.1159/000073077. [DOI] [PubMed] [Google Scholar]
- 8.Guyer DR, Schachat AP, Vitale S, Markowitz JA, Braine H, Burke PJ, et al. Leukemic retinopathy. Relationship between fundus lesions and hematologic parameters at diagnosis. Ophthalmology. 1989;96:860–4. doi: 10.1016/s0161-6420(89)32809-0. [DOI] [PubMed] [Google Scholar]
- 9.Querques G, Russo V, Martinez A, Sarra GM, Iaculli C, Delle Noci N. Retinal abnormalities in adult acute myeloid leukemia: Semeiological features and prognostic correlations. Analysis of 178 cases. J Fr Ophtalmol. 2007;30:819–23. doi: 10.1016/s0181-5512(07)92616-9. [DOI] [PubMed] [Google Scholar]
- 10.Omoti AE, Omoti CE, Momoh RO. Ophthalmic disorders in adult lymphoma patients in Africa. Middle East Afr J Ophthalmol. 2009;16:252–5. doi: 10.4103/0974-9233.58420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suresh K, Sampath R, Tanvi Ocular manifestations in hematological disorders. SRJM. 2011;4:1–4. [Google Scholar]
- 12.Koshy J, John MJ, Thomas S, Kaur G, Batra N, Xavier WJ. Ophthalmic manifestations of acute and chronic leukemias presenting to a tertiary care center in India. Indian J Ophthalmol. 2015;63:659–64. doi: 10.4103/0301-4738.169789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omoti AE, Omoti CE, Momoh RO. Ocular disorders in adult leukemia patients in Nigeria. Middle East Afr J Ophthalmol. 2010;17:165–8. doi: 10.4103/0974-9233.63081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wetzler M, Byrd JC, Bloomfield CD. Acute and chronic myeloid leukemia. In: Fauci AS, editor. Harrison's Principles of Internal Medicine. 17th ed. Vol. 1. New York: McGraw Hill; 2008. pp. 677–86. [Google Scholar]
- 15.Schachat AP, Markowitz JA, Guyer DR, Burke PJ, Karp JE, Graham ML. Ophthalmic manifestations of leukemia. Arch Ophthalmol. 1989;107:697–700. doi: 10.1001/archopht.1989.01070010715033. [DOI] [PubMed] [Google Scholar]
- 16.Alemayehu W, Shamebo M, Bedri A, Mengistu Z. Ocular manifestations of leukaemia in Ethiopians. Ethiop Med J. 1996;34:217–24. [PubMed] [Google Scholar]
- 17.Holt JM, Gordon-Smith EC. Retinal abnormalities in diseases of the blood. Br J Ophthalmol. 1969;53:145–60. doi: 10.1136/bjo.53.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.abu el-Asrar AM, al-Momen AK, Kangave D, Harakati MS, Ajarim DS. Correlation of fundus lesions and hematologic findings in leukemic retinopathy. Eur J Ophthalmol. 1996;6:167–72. doi: 10.1177/112067219600600213. [DOI] [PubMed] [Google Scholar]
- 19.Ohkoshi K, Tsiaras WG. Prognostic importance of ophthalmic manifestations in childhood leukaemia. Br J Ophthalmol. 1992;76:651–5. doi: 10.1136/bjo.76.11.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russo V, Scott IU, Querques G, Stella A, Barone A, Delle Noci N. Orbital and ocular manifestations of acute childhood leukemia: Clinical and statistical analysis of 180 patients. Eur J Ophthalmol. 2008;18:619–23. doi: 10.1177/112067210801800420. [DOI] [PubMed] [Google Scholar]


