Abstract
The epidemiologically most important mechanism of antibiotic resistance in Staphylococcus aureus is associated with mecA–an acquired gene encoding an extra penicillin-binding protein (PBP2a) with low affinity to virtually all β-lactams. The introduction of mecA into the S. aureus chromosome has led to the emergence of methicillin-resistant S. aureus (MRSA) pandemics, responsible for high rates of mortality worldwide. Nonetheless, little is known regarding the origin and evolution of mecA. Different mecA homologues have been identified in species belonging to the Staphylococcus sciuri group representing the most primitive staphylococci. In this study we aimed to identify evolutionary steps linking these mecA precursors to the β-lactam resistance gene mecA and the resistance phenotype. We sequenced genomes of 106 S. sciuri, S. vitulinus and S. fleurettii strains and determined their oxacillin susceptibility profiles. Single-nucleotide polymorphism (SNP) analysis of the core genome was performed to assess the genetic relatedness of the isolates. Phylogenetic analysis of the mecA gene homologues and promoters was achieved through nucleotide/amino acid sequence alignments and mutation rates were estimated using a Bayesian analysis. Furthermore, the predicted structure of mecA homologue-encoded PBPs of oxacillin-susceptible and -resistant strains were compared. We showed for the first time that oxacillin resistance in the S. sciuri group has emerged multiple times and by a variety of different mechanisms. Development of resistance occurred through several steps including structural diversification of the non-binding domain of native PBPs; changes in the promoters of mecA homologues; acquisition of SCCmec and adaptation of the bacterial genetic background. Moreover, our results suggest that it was exposure to β-lactams in human-created environments that has driven evolution of native PBPs towards a resistance determinant. The evolution of β-lactam resistance in staphylococci highlights the numerous resources available to bacteria to adapt to the selective pressure of antibiotics.
Author summary
The emergence and rise of mecA-mediated β-lactam resistance in staphylococci has been one of the greatest concerns of the scientific and medical communities worldwide. However, little is known regarding the origin of the mecA gene determinant. In this study we demonstrate that antibiotic pressure in the human environment and in food additives used in livestock was the major driving force of the evolution and spread of resistance to β-lactams. Furthermore, we confirm the previous findings suggesting that the development of resistance occurs in primitive species of staphylococci through diversification of a native penicillin binding protein involved in cell wall synthesis. We also demonstrate that resistance was achieved through four distinct mechanisms: accumulation of substitutions in a specific domain of the protein; diversification of the promoter of the gene; acquisition of SCCmec, and adaptation of the genetic background. Our results highlight the resources that primitive bacteria used to thrive in a changing environment that has led to the methicillin-resistant Staphylococcus aureus (MRSA) pandemics.
Introduction
The most important antibiotic resistance mechanism in staphylococci is associated with the mecA gene, which confers resistance to the large class of β-lactam antibiotics. mecA is carried on a mobile genetic element called staphylococcal cassette chromosome mec (SCCmec) [1], which always inserts at the same locus in the chromosome, in the 3’ end of orfX (which encodes a RNA methyltransferase) [1, 2]. Several studies have demonstrated that acquisition of mecA confers to staphylococci a competitive advantage in the hospital, community and veterinary environments [3, 4]. Introduction of the mecA determinant into the S. aureus genome on multiple occasions, has led to the emergence and worldwide dissemination of several methicillin-resistant S. aureus (MRSA) clones [5].
The mecA determinant encodes an extra penicillin-binding protein (PBP2a). The expression of resistance is achieved by a slow rate of acylation of PBP2a as well as a low affinity of the enzyme for β-lactams [6]. Structural studies have revealed that the poor acylation rate, that PBP2a presents when in contact with β-lactams, is due to a distorted active site, provided by the flexibility of the non-binding (NB) domain and regions surrounding the active site groove in the transpeptidase (TP) domain [7]. Furthermore, the position of Ser403 is crucial for the nucleophilic attack of the β-lactam ring, which leads to acylation of the protein [7].
The first clinical MRSA isolates were identified in the UK in 1961, shortly after the introduction of methicillin into clinical practice [8, 9]. Early MRSA were found to present a heterogeneous profile of resistance to β-lactams [10]. Further studies have revealed that mutations in genes associated with cell division as well as central metabolism (the so-called auxiliary genes) influence the expression of β-lactam resistance and the resulting phenotype [11]. Moreover, the expression of homogeneous high level resistance has been associated with the activation of the bacterial stringent response, provoked by mutations in the relA system [12, 13] and related regulons and genes [14]. These findings underline the importance of the S. aureus genetic background in the expression of β-lactam resistance.
The rapid emergence of MRSA raised the hypothesis that mecA was already present in the staphylococcal gene pool prior to the introduction of methicillin. In fact, a ubiquitous homologue named mecA1, with 80% nucleotide identity to mecA has been identified in the primitive coagulase-negative Staphylococcus sciuri [15]. Several lines of evidence suggest that mecA1 is the precursor of mecA. While mecA1 does not confer resistance to β-lactams in S. sciuri, there are reports of β-lactam-resistant strains that have alterations in the promoter region of this gene [16]. When introduced experimentally into a S. aureus strain, mecA1 was able to confer β-lactam resistance and produce a protein with properties resembling that of MRSA PBP2a [17, 18]. Additional mecA homologues have been identified in related species, including a mecA homologue (mecA2) with 90% nucleotide identity with mecA in Staphylococcus vitulinus [19]. Furthermore, mecA along with its regulators, mecI and mecRI, has been identified in a small number of Staphylococcus fleurettii isolates [20].
Despite the importance of mecA in the epidemiology of antibiotic resistant staphylococci, the evolutionary history of this gene has remained unclear. The purpose of this study was to shed light on the evolutionary steps linking the native mecA homologues identified in primitive coagulase negative staphylococci to the β-lactam resistance gene mecA and the resistance phenotype.
Results
Homologues of mecA are abundant in S. sciuri, S. vitulinus and S. fleurettii
The putative precursor of mecA is mecA1, previously shown to be ubiquitous in S. sciuri (15), but the frequency of the other mecA homologues (mecA2 and mecA) in the remaining species of the S. sciuri group remained unclear. Additionally, the location of mecA homologues in the chromosome was unknown.
A search for mecA homologues by BLAST analysis in the genomes of 106 S. sciuri, S. vitulinus and S. fleurettii isolates collected from humans and animals showed that all strains carried at least one copy of mecA homologue. These were found either in the orfX (SCCmec insertion site) or 200 kb from orfX, a site that from now on, we will call native location. We confirmed that, in our collection, mecA1 was present in all S. sciuri isolates [15] and mecA was present in all S. fleurettii strains [20] at the native location. S. vitulinus was different from the other species, since half of the strains (n = 9) carried mecA2 [19], and the remaining strains either carried mecA (n = 6) or did not carry any mecA homologue in this region (n = 3).
mecA1 is a hot spot for diversification
Alignment of all mecA1, mecA2 and mecA sequences (S1A Fig) showed that mecA1 was extremely diverse, including a total of 44 different alleles (SID = 97.2%, CI = 95.7%-98.7%) that varied between 93–100% in nucleotide identity (S1B Fig). In contrast, mecA2 and mecA were highly conserved (mecA2: SID = 70.4%, CI = 60.5%-80.2%; mecA: SID = 21.6%, CI = 9.7%-33.6%) varying from 99.75 to 100% in nucleotide identity.
Furthermore, amino acid sequence predictions showed that the SID of mecA1-encoded PBP4 was still very high, 96.2% (CI = 94.5%-97.9%). Interestingly, although both the nonbinding (NB) and transpeptidase (TP) domains were under purifying selection (dN/dS<1), the NB domain accumulated many more amino acid substitutions (36%) and showed a higher dN/dS per site (0.19) than the TP domain (8%; dN/dS = 0.05).
The genetic diversity observed for mecA1 appears to have resulted both from recombination and mutation events, wherein the average recombination/mutation rate/site was estimated to be 0.15:1. According to RDP4 analysis, the recombination observed in mecA1 has been driven by recombination between different S. sciuri mecA1 alleles (Supplementary S1B Fig). Although according to our data recombination in mecA1 was not such a frequent event, the recombining mecA1 alleles represented 60.5% of the S. sciuri population. In addition, all but two S. sciuri isolates showing oxacillin resistance carried recombining alleles, suggesting that recombination in mecA1 was important for the development of resistance in this species.
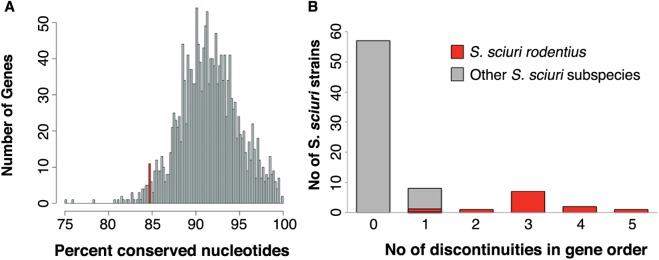
Overall, neither genetic diversity nor recombination were features affecting the entire S. sciuri genomes. This was obvious by the lower fraction of conserved positions of mecA1 (84.7%) when compared to the remaining core genes (91.57%; stdev 3.43) (Fig 1A), and by the fact that mecA1 was among the 2.5% most variable genes in the core genome (see supplementary S2 Table and Fig 1A). Additionally, for the great majority of strains (n = 57, 75%) the order of the 1759 core genes was conserved (0 discontinuities in gene order), when compared with the S. sciuri sciuri reference genome NCTC12103 (see Table 1 and Fig 1B).
Fig 1. Distribution of the percentage of conserved nucleotides among the 1759 core genes of the 76 S. sciuri strains analyzed in this study.
The conservation percentage of mecA1 is shown in red (A). Number of discontinuities in the order of the core genes in the 76 S. sciuri strains analyzed in this study, when compared to S. sciuri sciuri reference strain NCTC12103 (B).
Table 1. Number of discontinuities in the order of 1759 core genes of the 76 S. sciuri genomes when compared with the S. sciuri sciuri reference genome NCTC12103.
| Discontinuities In Gene Order | 0 | 1 | 2 | 3 | 4 | 5 |
| Number of Genomes | 57 | 8 | 1 | 7 | 2 | 1 |
The only subspecies that, according to our data, has probably a higher recombination rate is S. sciuri rodentius, since the genomes of all the strains belonging to this subspecies showed at least one discontinuity in their genome. Furthermore, this subspecies comprised the highest number of discontinuities in gene order (1–5 discontinuites). The other subspecies showing discontinuities were the subspecies S. sciuri sciuri and a putative new subspecies (see item The genetic background was associated with the emergence of β-lactam resistance in S. sciuri)), but this corresponded to a single discontinuity and was a rare occurrence among these subspecies.
Altogether, these results suggest that mecA1 is a hotspot for diversification in S. sciuri.
Different levels of oxacillin resistance were observed in all species of S. sciuri group
To assess the level of resistance to oxacillin, we determined the epidemiological cut-off (ECOFF) value for oxacillin in the S. sciuri group of species (S2 Fig), since the currently available MIC breakpoints are defined only for clinically significant Staphylococcus species. According to this analysis, the oxacillin breakpoint for resistance was set at 3 μg/ml oxacillin.
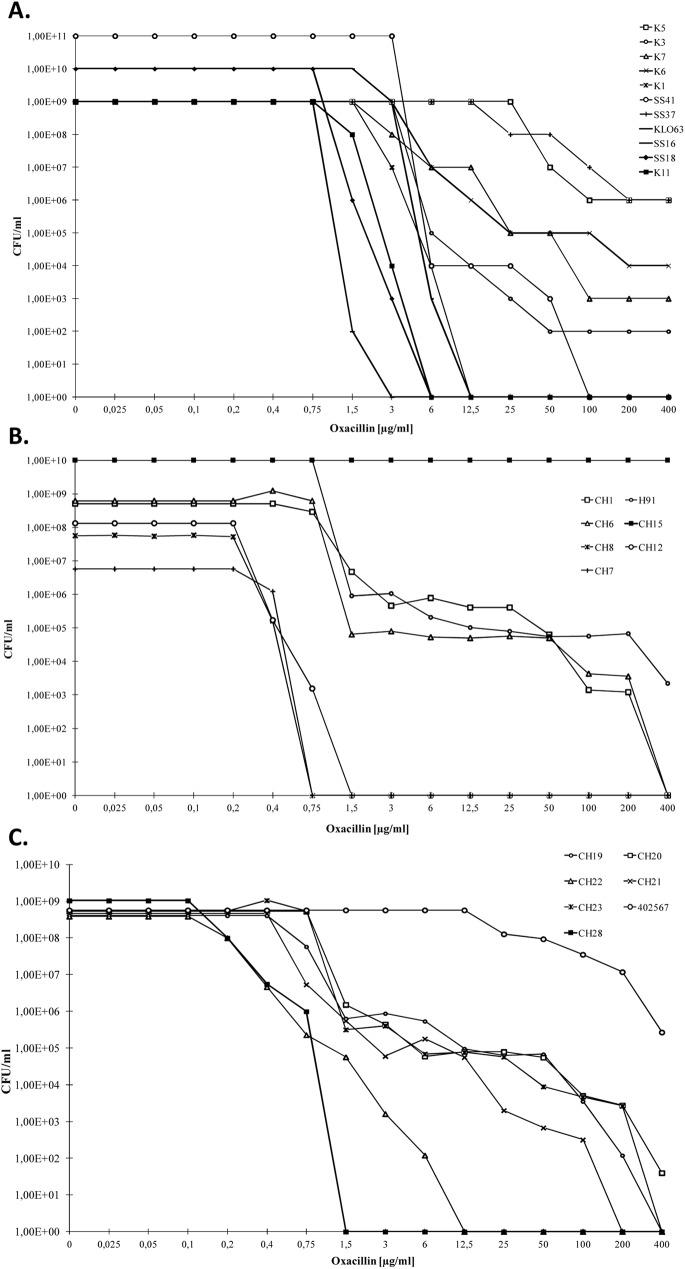
Considering this breakpoint, the great majority of S. sciuri strains carrying only mecA1 (54/60) was susceptible to oxacillin, but six strains were resistant (K4, K5, K7, Jug17, SS37 and SS41) as determined by Etests. From the 54 susceptible strains, 24 produced heterogeneous profiles when analysed by oxacillin population analysis profiles (PAPs), and almost half of these isolates (11 out of 24) were able to grow at concentrations up to 6–100 μg/ml (Fig 2A). Moreover, the 16 S. sciuri strains that carried mecA in addition to mecA1 were all resistant (MIC 16 to >256 μg/ml), and representative strains showed an heterogeneous profile and were able to survive at concentrations up to 800 μg/ml of oxacillin (Fig 2A and Table 2).
Fig 2.
Oxacillin susceptibility population analysis profiles (PAPs) for representative S. sciuri (A)[15, 21], S. vitulinus (B) and S. fleurettii (C).
Table 2. Main characteristics of β-lactam resistant strains as defined by the ECCOF of 3 μg/mL.
| Strain | Date of isolation | Host | MIC μg/ml (eTest/PAP) | Mechanism of resistance | Phylogenetic group | mec allele | Recombinant mecA1 allele |
|---|---|---|---|---|---|---|---|
| M1234 | 2009 | Human | >256 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| M692 | 2007 | Human | 96 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| M2590 | 2012 | Human | >256 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| M2276 | 2011 | Human | >256 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| D573 | 2007 | Human | >256 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| M1653 | 2010 | Human | >256 | SCCmec | S. sciuri new 2 | mecA 9 /mecA1 6 | + |
| CH17 | 2010 | Horse | >256 | SCCmec | S. sciuri new 2 | mecA 8 /mecA1 7 | + |
| CH18 | 2010 | Horse | >256 | SCCmec | S. sciuri new 2 | mecA 8 /mecA1 7 | + |
| M2710 | 2012 | Human | >256 | SCCmec, altered PBP4 | S. sciuri new 2 | mecA 7 /mecA1 4 | + |
| HSM851 | 2010 | Human | 16 | SCCmec, altered PBP4 | S. sciuri new 2 | mecA 7 /mecA1 4 | + |
| Jug17 | 2002 | Human | >256 | Altered PBP4 | S. sciuri new 2 | mecA1 4 | + |
| K3 | 1992 | Human | >256 | SCCmec/ alterations mecA1 promoter | S. sciuri rodentius | mecA10/mecA1 17 | + |
| K4 | 1992 | Human | >256 | Alterations mecA1 promoter | S. sciuri rodentius | mecA1 17 | + |
| K5 | 1992 | Human | 25 | Alterations mecA1 promoter | S. sciuri rodentius | mecA1 17 | + |
| K7 | 1992 | Human | >256 | Alterations mecA1 promoter | S. sciuri rodentius | mecA1 17 | + |
| SS37 | 1996 | Human | 25 | Alterations mecA1 promoter | S. sciuri rodentius | mecA1 17 | + |
| SS41 | 1996 | Human | 3 | Alterations mecA1 promoter | S. sciuri rodentius | mecA1 17 | + |
| CH16 | 2010 | Human | 24 | SCCmec | S. sciuri rodentius | mecA 7 /mecA1 19 | + |
| K6 | 1992 | Human | >256 | SCCmec | S. sciuri rodentius | mecA 7 /mecA1 42 | - |
| M1640 | 2010 | Human | 96 | SCCmec | S. sciuri sciuri | mecA 7 /mecA1 37 | - |
| Jug1 | 2002 | Dog | >256 | SCCmec | S. sciuri new 1 | mecA 7 /mecA1 16 | + |
| M1886 | 2011 | Human | 64 | SCCmec | S. sciuri new 1 | mecA 7 /mecA1 43 | - |
| CH2 | 2004 | Horse | 4 | Genetic background? | S. vitulinus | mecA 4 | - |
| CH5 | 2005 | Horse | >256 | Genetic background? | S. vitulinus | mecA 4 | - |
| CH15 | 2004 | Horse | >256 | alterations mecA2 promoter | S. vitulinus | mecA2 2 | - |
| CH19 | 2010 | Horse | 8 | mecA native location | S. fleurettii | mecA 1 | - |
| CH20 | 2010 | Horse | 6 | mecA native location | S. fleurettii | mecA 3 | - |
| CH21 | 2010 | Horse | 4 | mecA native location | S. fleurettii | mecA 2 | - |
| CH23 | 2010 | Horse | 4 | mecA native location | S. fleurettii | mecA 2 | - |
| CH24 | 2010 | Horse | >256 | mecA native location | S. fleurettii | mecA 2 | - |
| CH25 | 2010 | Horse | 4 | mecA native location | S. fleurettii | mecA 6 | - |
| CH26 | 2010 | Horse | >256 | mecA native location | S. fleurettii | mecA 2 | - |
| CH27 | 2010 | Horse | 4 | mecA native location | S. fleurettii | mecA 2 | - |
| CH29 | 2010 | Horse | 4 | mecA native location | S. fleurettii | mecA 2 | - |
| 402567 | 2004 | Horse | >256 | mecA native location | S. fleurettii | mecA 5 | - |
Like in S. sciuri, in S. vitulinus, the great majority of strains carrying either mecA2 or mecA were oxacillin-susceptible, but some of these strains showed a heterogeneous profile in which sub-populations could grow above the MIC (100–400 μg/ml) (Fig 2B). Moreover, a few strains displayed a resistant phenotype (CH15, CH2 and CH5) (see Table 2 and Fig 2B).
In contrast, the great majority of S. fleurettii isolates were resistant to oxacillin (MIC 4->256 μg/ml) with subpopulations that were able to grow at concentrations up to 25–400 μg/ml (Fig 2C), but two strains showed a susceptible phenotype (CH22 and CH28) (see Table 2 and Fig 2C).
Oxacillin resistance emerged by multiple molecular strategies
In order to understand the mechanisms associated with the oxacillin resistance phenotypes exhibited by S. sciuri, S. vitulinus and S. fleurettii we looked for: differences in the structure of proteins encoded by mecA homologues; changes in the expression of mecA homologues; presence of SCCmec; and differences in the genetic background.
Alteration in the structure of the active site in mecA homologue-encoded PBPs was associated with β-lactam resistance
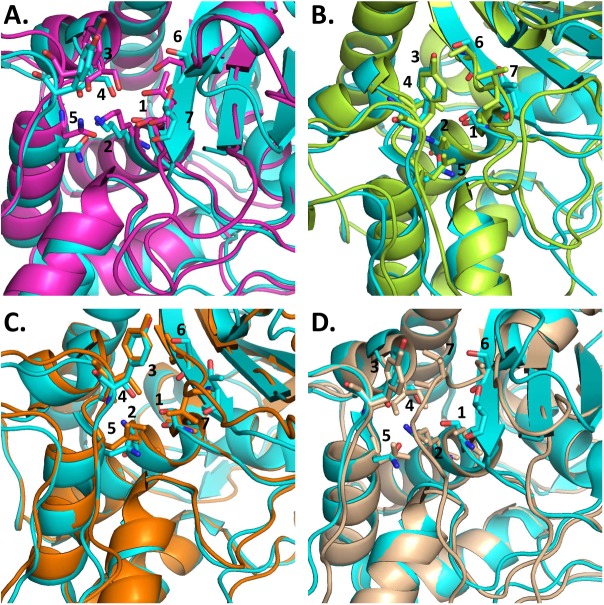
To test if the nucleotide diversity of different mecA homologues could explain the different levels of oxacillin susceptibility observed, we compared the structure of the proteins encoded by different mecA homologues (mecA allele 5, mecA2 allele 2, mecA1 allele 4, mecA1 allele 17, mecA1 allele 21, mecA1 allele 22, mecA1 allele 25 and mecA1 allele 42) with the structure of PBP2a using a modeling approach. We observed that in multiple occasions, in S. sciuri, S. vitulinus and S. fleurettii, the level of oxacillin susceptibility could be related to alterations occurring in the active site grove that could lead to a higher or lower exposure of the catalytic amino acid Ser403 (PBP2a)/Ser401 (PBP4).
This was the case of the protein encoded by mecA1 allele 42, present in the oxacillin-susceptible S. sciuri carnaticus type strain K11 [22], in which the residues Ser596 and Thr598, were not located in a β-sheet motif, in contrast to what was found in PBP2a (Fig 3C). The position of these residues, which surround the active site groove, was otherwise more relaxed, suggesting that access to Ser401 is probably facilitated, explaining the susceptible phenotype observed. The structures predicted for the remaining mecA1 alleles analyzed were similar. This association between the phenotype and the protein structure was likewise found in the S. sciuri strains Jug17, HSM851 and M2710, carrying allele mecA1 4 (Fig 3D), all showing high-level resistance to oxacillin, in which Thr598 was much closer to Tyr444, thus “closing” the active site groove and protecting Ser401 from interacting with the β-lactam ring.
Fig 3. Alignment of the active centre of PBP2a (highlighted in cyan blue) and representative PBPs putatively encoded by mecA homologues.
The structure of the PBP was predicted by Modeller and the alignment was produced in Pymol. Oxacillin-resistant S. fleurettii 402567 mecA allele 5/PBP2a (A). Oxacillin-susceptible S. vitulinus CH10 mecA allele 2/PBP2a (B). Oxacillin-susceptible S. sciuri K11 mecA1 allele 42/PBP2a.1 (C). Oxacillin-resistant S. sciuri JUG17 mecA1 allele 4/PBP2a (D). 1. Ser401/Ser403. 2. Lys404/Lys406. 3. Tyr444/Tyr446. 4. Ser460/Ser462. 5. Asn464/Asn466. 6. Ser596/Ser598. 7. Thr598/Thr600.
In addition, the protein encoded by the most frequent mecA2 allele (mecA2 2) in S. vitulinus, (which is associated with oxacillin susceptibility in almost all strains), had residues Ser403 and Thr600 (Fig 3B) in positions different from those found in PBP2a. This could lead to higher exposure of Ser403 to the β-lactam ring. The only strain carrying mecA2 allele 2 that was resistant to oxacillin (CH15) had an alteration in the promoter of the protein (see section below—Mutations in the promoter of mecA homologues gave rise to β-lactams resistance).
Another example, in S. fleurettii, is the protein encoded by mecA allele 5, associated with high level of oxacillin resistance that had the exact same residues as S. aureus PBP2a. Although these residues were not in the exact same position, their orientation was the same (Fig 3A), suggesting that they should have a similar rate of acylation.
Mutations in the promoter of mecA homologues gave rise to β-lactam resistance
Genetic changes in the mecA1 promoter of S. sciuri strains SS37 and SS41 –namely the insertion of IS256 and a single-nucleotide polymorphism (SNP)–respectively, were previously reported by Couto et al. to be associated with a resistance phenotype [16]. In our collection, we additionally identified several cases of alterations in the promoter region (200 bp upstream of mecA homologues) that were associated both with the expression level of the PBPs and to the oxacillin susceptibility profile observed.
For instance, the oxacillin-resistant S. sciuri rodentius strains K4, K5 and K7 showed alterations in -10 and -35 sequences when compared to the susceptible strain K11 (see S3 Fig). In particular, we were able to identify in these strains the same nucleotide alterations previously reported for the oxacillin resistant SS41 strain [16]. For S. vitulinus, the promoter regions of two strains carrying the mecA2 allele 2 –one susceptible (CH10) and the other resistant to oxacillin (CH15)–were compared. Whereas the ribosome binding site (RBS) sequence, GGGAGGG, was located immediately upstream of mecA2 in strain CH15 (at position -3), this same sequence was located further upstream (at position -6) in strain CH10. Finally, for S. fleurettii, the promoter of the susceptible strain (CH28) showed a deletion of 16 bp at position -29 upstream of mecA, possibly at the -10 region (TATACT), when compared to strain CH22, which expresses a higher level of heteroresistance (see Fig 2C).
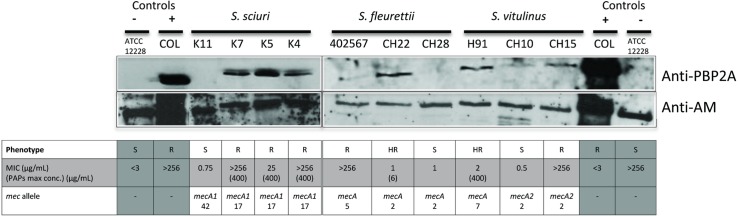
As shown in Fig 4, all the described alterations in the promoter sequence could be associated with differences in the expression of the mecA homologues encoded proteins. In particular, expression of mecA1 in resistant S. sciuri strains K4, K5, K7 and of mecA2 in S. vitulinus strain CH15 was increased when compared to the susceptible strains K11 and CH10. The expression of mecA in the S. fleurettii susceptible strain CH28 was decreased when compared to the heterogenous strain CH22.
Fig 4. Western blotting of the membrane fraction of S. sciuri, S. fleurettii and S. vitulinus using a polyclonal antibody raised against S. aureus PBP2a and a polyclonal antibody raised against the amidase (AM) domain of S. aureus Atl protein.
Lanes 1 and 14: S. epidermidis strain ATCC12228; Lanes 2 and 13: S. aureus strain COL; Lane 3: S. sciuri carnaticus strain K11; 4: S. sciuri rodentius strain K7; 5: S. sciuri rodentius strain K5; 6: S. sciuri rodentius strain K4; 7: S. fleurettii strain 402567; 8: S. fleurettii strain CH22; 9: S. fleurettii strain CH28; 10: S. vitulinus strain H91; 11: S. vitulinus strain CH10; 12: S. vitulinus strain CH15.
The association between nucleotide alterations in the sequence of the mecA homologues and their respective promoter regions and the resistant phenotype to oxacillin, was found to be statistically significant (p<0.05), suggesting that these associations were not due to chance.
Other factors that are described to influence mecA expression in S. aureus are the regulatory systems mecI/mecR1 and blaI/blaR1 that are induced in the presence of antibiotic [23, 24]. The mecA was the only mec homologue in which mecI/mecR1 were found upstream the gene and although a blaZ homologue was found in the three species (67% aminoacid sequence identity), it seems not to have the capacity to hydrolyze the β-lactam ring as observed using the nitrocefin test. Moreover, no difference in the expression of mec homologues was observed in the presence of oxacillin by western blotting, which suggests that these regulators in species of the S. sciuri group do not respond to the same stimulus as in S. aureus.
The presence of SCCmec is associated with β-lactam resistance only in S. sciuri
The main mechanism of β-lactam resistance is associated with the presence of SCCmec [1]. This element occurred in 20% of all S. sciuri analyzed and in all subspecies except S. sciuri carnaticus (see Table 2) and was always associated with high-level resistance (16<MIC<256) (see Table 2). Although in SCCmec carrying strains, mecA1 was also present, the majority of mecA1 alleles (mecA1 6, mecA1 7, mecA1 8, mecA1 37, mecA1 42) and promoters found in these strains were carried by oxacillin-susceptible strains too, suggesting that SCCmec and not mecA1 is responsible for the resistance phenotype (see supplemental S1 Table). Three strains carried both SCCmec and alterations in mecA1 structure (HSM851 and M2710) or promoter (K3), which were identified above as being possibly associated with resistance. In these cases both mechanisms may be contributing to the resistance phenotype.
In the other two species SCCmec was either absent (S. fleurettii) or did not confer resistance to oxacillin (S. vitulinus) (see Table 2 and S3B Fig). The absence of the resistance phenotype, in S. vitulinus, in spite of the presence of SCCmec is puzzling. However, this is not related to the lack of mecA expression since, as shown by Western blotting, strain H91, carrying SCCmec, showed an expression level of the encoded PBP that was higher than the negative control ATCC12228.
The genetic background was associated with the emergence of β-lactam resistant phenotype in S. sciuri
The contribution of several housekeeping genes to the optimal expression of methicillin resistance was previously described in S. aureus [11, 14], and evidence has been presented that not all S. aureus lineages are adapted to express methicillin-resistance [25, 26].
The phylogenetic reconstruction based on the number of SNP differences in the core genome of species of the S. sciuri group revealed the existence of three well-defined phylogenetic groups, corresponding to each of the three species. While the core genomes of S. fleurettii and S. vitulinus had an average 3000–9000 SNPs and 4000–7000 SNPs difference, respectively, S. sciuri core genomes differed in average by 15000 SNPs, (S3A–S3C Fig). Moreover, within S. sciuri species five different clusters were identified, that probably correspond to five different subspecies: the three previously described subspecies (S. sciuri sciuri, S. sciuri rodentius and S. sciuri carnaticus) and two putative new subspecies. The phylogenetic clustering shown might have been influenced by recombination events occurring in S. sciuri rodentius (see above). However, with the exception of one strain (K4), all the S. sciuri rodentius strains identified by other methods, like tuf and 16S rDNA sequencing, clustered together in the same large subspecies branch, suggesting that genetic recombination must have mainly altered the phylogenetic relationships at the strain level only, not altering significantly the definition of the subspecies.
The resistance phenotypes were clearly associated with phylogeny, mainly in S. sciuri. The isolates showing β-lactam resistance were almost exclusively (19/22) confined to S. sciuri rodentius and S. sciuri subspecies new 2 and to specific clusters within each of these subspecies, which were distinct from the clusters containing susceptible isolates (p<0.05) (See S3C Fig and Fig 5). Moreover, resistant strains were distributed along phylogeny according to the mechanism of resistance involved. While strains showing alterations in promoter were exclusively associated with the subspecies S. sciuri rodentius, those showing alterations in the structure of the proteins encoded by the mec homologue or having SCCmec structures belonged mainly (14/17) to the putative subspecies new 2 (Table 2) (p<0.05). These results suggest that the genetic background was a key factor for the expression of resistance in S. sciuri. However, the identification of the genetic background factors contributing to resistance were not further explored.
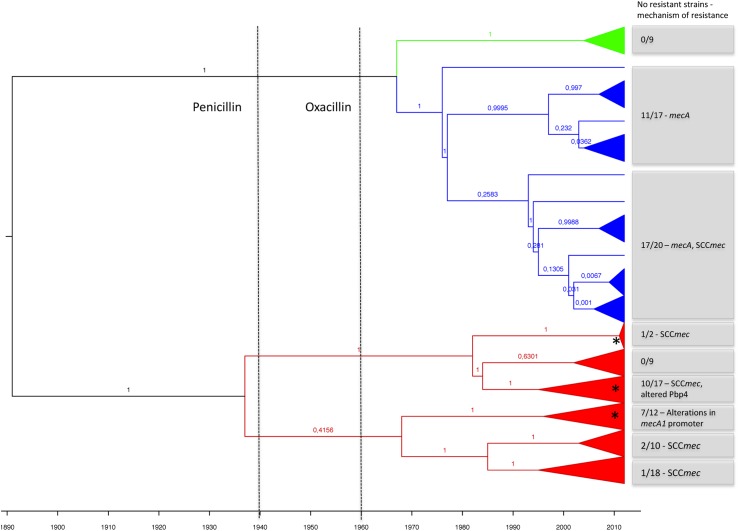
Fig 5. Evolutionary history of mecA homologue alleles.
BEAST analysis of the nucleotide sequence of mecA homologues using the random clock and constant population models. mecA1 alleles are shown in red, mecA alleles are shown in marine blue and mecA2 alleles are shown in green. Numbers next to tree branches are the posteriors for the tree. Dashed lines indicate the time of introduction of penicillin and oxacillin into clinical practice in humans. Grey boxes include the number of resistant isolates within each branch and the associated mechanisms of resistance. Asterisks indicate the clusters in which recombinant mecA1 alleles were identified.
In contrast to S. sciuri, in which emergence of β-lactam resistance appears to be strongly associated with phylogeny, strains of S. vitulinus and S. fleurettii, with very few exceptions, were uniformly susceptible and resistant to β-lactams, respectively (see supplementary S1 Table). However, in these species we could also find examples that illustrate the impact of the genetic background in β-lactam resistance. In particular, we found that S. fleurettii strains carrying the exact same gene allele as susceptible S. vitulinus (like mecA allele 4 and mecA allele 2) showed in contrast, high-level of resistance to β-lactams.
Human and human created environments were drivers of β-lactam resistance
S. sciuri is widely disseminated in nature, being found in different animal species and, occasionally, isolated from human infections, whereas S. vitulinus and S. fleurettii host range is mainly restricted to animals (36–39). Nonetheless, the three species live in environments created by humans in which antibiotic usage is frequent, namely in hospitals and farms.
Data resulting from this study provided evidence that antibiotic deployment in these environments were probably the drivers of β-lactam resistance development. This is illustrated by the finding that all β-lactam resistant S. sciuri, were collected from human sources or from animals in close contact with humans (horses and dogs), and not from wild animals (p<0.05). Moreover, all S. vitulinus and S. fleurettii included in this study originated from animal species in close contact with humans and were either intrinsically resistant to β-lactams or had the capacity to develop resistance.
Antibiotic usage is linked to the emergence of β-lactam resistance
Antibiotic resistance is believed to be the result of antibiotic pressure imposed on bacteria. Bayesian phylogenetic reconstruction was used to explore the association between the time of emergence of resistant phenotypes and antibiotic use.
The MCC tree resulting from BEAST analysis of mecA homologs using a random molecular clock and a constant size population model showed that the time to the most recent common ancestor (tMRCA) of all mecA homologues alleles was estimated to be in 1891 (1845–1976 95%HPD) (see Fig 5), before the introduction of antibiotics in the clinical practice, and that two clusters split in 1937 (1892–1968 95%HPD), one originating mecA1 and the other mecA2 and mecA (Fig 5 and S1B Fig). The mecA1 began diversifying in 1968 (1951–1986 95%HPD), which coincided with the emergence of recombining alleles and the emergence of β-lactam resistance. This was contemporaneous with the use of penicillin and methicillin as a treatment in humans (1940 and 1960, respectively) and of penicillin as a feed additive in production animals (1950–1960).
According to our results, the first mecA2 allele emerged in a S. vitulinus strain, approximately in 1967 (1930–1976 95%HPD). The development of mecA occurred later, in S. fleurettii, in 1977 (1961–1997 95%HPD), suggesting mecA could have been already present in the population when methicillin was first introduced into clinical practice, in 1961. The SCCmec was estimated to have emerged afterwards (1982–1994 95%HPD) in S. sciuri rodentius [22] (Fig 5). Once created, SCCmec appears to have been rapidly disseminated to other staphylococcal species like S. aureus; coincidently, it was during the 1980s and 1990s that MRSA pandemic clones began to expand worldwide.
The 95% HPD values obtained for the dates presented are wide, particularly at deeper nodes, thus comprising considerable uncertainty. This may result from the type of strain collection analyzed, which was non-random and enriched for more recent isolates. Alternatively, the findings may reflect occurrence of purifying selection and recombination in mecA1. In particular, leaps of diversity due to recombination in mecA1 or to a weak/mild purifying selection may have led to the estimation of a date that is posterior to the true date of emergence. However, the MCC tree based on mecA genes in the absence of recombination sites (and using the same molecular clock and population models), showed no relevant differences when compared to the tree constructed in the presence of recombination, neither in the population structure nor in the dating of evolutionary events.
Discussion
The mechanism of β-lactam resistance mediated by mecA in Staphylococcus is one of the most efficient mechanisms of resistance to antibiotics, providing resistance to virtually all members of the large class of β-lactams. Several studies have shown that the mecA precursor was a native gene (mecA1) not providing resistance in Staphylococcus sciuri, the most primitive staphylococcal species [15, 18]. However, the evolutionary steps leading to phenotypic resistance remained unclear. In this study, we showed that species of the S. sciuri group developed multiple strategies during their evolutionary history to develop β-lactam resistance including (i) structural diversification of a native PBP, (ii) changes in the promoter of the mecA homologues, (iii) SCCmec acquisition and (iv) adaptation of the genetic background.
Although the TP domain has been described as the crucial domain for PBP activity [7], our results are the first to identify a fundamental role of the NB domain for its full performance. In particular, we found that alterations in the NB domain of proteins encoded by the mecA homologues can have impact on the level of distortion of the active site groove and on the consequent access of the substrate (or the antibiotic) to the Ser401/Ser403, the key aminoacid residues at the catalytic site. The existence of subtle changes in the NB domain of PPBs can give rise to proteins with different levels of activity. Since the different mecA homologues have a very conserved TP domain, the evolution from a susceptible to a resistance determinant probably involved alterations mainly in the NB domain of the protein.
An additional mechanism driving β-lactam resistance involved alterations in the promoter of mecA homologues: either deletions around the RBS site or alterations in -10 and -35 regions. The association of changes in the promoter with an increased mecA1 expression and a resultant resistance phenotype was a phenomenon previously observed in a few strains of S. sciuri [16]. In this study we confirmed that these type of events probably occurred with a relatively high frequency in the overall S. sciuri population and also in S. vitulinus, during their evolutionary history. This event occurred in the promoters of mecA1 and mecA2 only, and may represent a molecular strategy used by the bacteria to circumvent antibiotic pressure, in the absence of a low affinity PBP. We found a good correlation between the alterations in the promoter of these genes and both the expression of their encoded proteins as well as the corresponding resistance phenotypes. A previous study analyzing the mechanism of β-lactam resistance in S. sciuri strains showed a total correlation of the resistance phenotype with an increase in both mecA1 transcription and mecA1-encoded PBP translation (16), suggesting that post-transcriptional and post-translational regulation, if occurring, appear not to have disturbed the link between the alterations in the promoter and the observed expression of resistance.
Another event associated with the emergence of resistance was the acquisition of SCCmec by S. sciuri and S. vitulinus. However, in this case the correlation between the phenotype and the genotype was only observed for S. sciuri. The absence of a resistant phenotype in S. vitulinus strains carrying mecA either in the native location or within SCCmec is puzzling. We show that the susceptibility is not associated with the absence of gene expression, but post-translational modifications may be involved. Another alternative is that access of the antibiotic to its target may be blocked, by an unknown mechanism.
In addition, our results demonstrate that–similarly to the case of MRSA [11, 14, 27]–the genetic background also plays an important role in the expression of β-lactam resistant phenotype of this primitive group of staphylococci. The most obvious examples are the absence of resistant phenotype in the presence of mecA in S. vitulinus and the development of resistance in particular phylogenetic clusters of S. sciuri. Genes involved in general metabolism were already shown to play important roles in the expression of β-lactam resistance in S. aureus suggesting an interplay between the overall metabolism and β-lactam resistance [27] [28].
The observation that unknown factors in genetic background are important for the expression of resistance does not allow to establishing definitely a direct correlation between nucleotide substitutions observed in the promoter sequence and mec homologue genes and the resistance phenotype. To substantiate this, an ideal approach would be to test the different promoters and express the different mec homologue variants in an appropriate S. sciuri genetic background. However, these studies are very difficult to perform due to the lack of genetic tools available in this species.
The fact that such diversified mechanisms leading to β-lactam resistance were found in different species of the S. sciuri group together with accumulation of more than one of these mechanisms at different time points, generating redundancy, are evidence for the persistent antibiotic pressure that these species experienced during their evolutionary history. Moreover, the diversification, recombination and purifying selection, observed in mecA1 gene, in opposition to the remaining chromosome, in the majority of S. sciuri strains further highlights the specific response of a bacterial species to the environmental pressure by antibiotics.
Antibiotic pressure giving rise to β-lactam resistance appears to be directly linked to exposure to human created environments, since resistance was exclusively observed in clinical isolates of human origin or from production animals, where high doses of antibiotics are generally used, and absent from wild animals where antibiotic pressure is limited to the level of antibiotics present in nature. This is in accordance with the Bayesian analysis performed, in which the estimated dates of occurrence of key events in mecA homologues evolution coincided with the time of introduction of antibiotics in veterinary and human clinical settings [29].
A limitation of this study is the fact that the reconstructed phylogeny of the mecA homologues was based on the Bayesian analysis of genes, which we showed to be under recombination and purifying selection. Additionally, it was based on a sampling framework that was non-random and that constituted an underrepresentation of S. sciuri, S. vitulinus and S. fleurettIi population diversity, namely in host range, dates of isolation and geographic region [30]. Consequently, inexact estimations of the evolutionary path of mecA homologues, mainly of mecA1, may have been generated, adding uncertainty to the dating of the evolutionary events of mecA homologs, namely to the existence of overlap between the emergence of resistance phenotypes and the use of antibiotics.
Overall our data suggest that the first evolutionary steps leading to mecA-mediated β-lactam resistance in Staphylococcus occurred in the most primitive staphylococcal species by several molecular mechanisms, in response to β-lactam pressure, both in humans and livestock. These results highlight the complexity of the evolution of mecA-mediated β-lactam resistance.
Methods
Ethical Statement
Human isolates were obtained as part of routine surveillance and laboratory testing and were analyzed anonymously. All data was collected in accordance with the European Parliament and Council decision for the epidemiological surveillance and control of communicable disease in the European community [31, 32]. Ethical approval and informed consent were for that reason not required. The animal isolates originated from nasal and skin swabs and bovine milk and some were collected as part of previous studies in Denmark [33, 34] and Switzerland [19, 35]. According to the national legislations, formal ethical approval was not required since samples were collected by non-invasive sampling procedures and no animal tissues were collected.
Bacterial strain collection
A collection of 106 staphylococcal isolates, comprising 76 S. sciuri, 18 S. vitulinus and 12 S. fleurettii was assembled. This is a convenience sample, however, we believe it reasonably reproduces the species distribution and diversity of hosts that exist in nature, as previously described [36–39].
Regarding S. sciuri, 28 isolates were obtained from humans, while the remaining 45 isolates were recovered from both wild and domesticated mammals (Supplementary S1 Table). Isolates were collected in different countries (Czech Republic, Denmark, Portugal, Switzerland, Sweden, former Yugoslavia, Mozambique, Panama and USA) between 1972 and 2012. S. vitulinus and S. fleurettii isolates were collected from horses and bovine mastitis milk samples, in Denmark, Switzerland and the Netherlands, in 2004, 2005 and 2010. The S. sciuri isolates were identified at the species level by 16S rRNA ribotyping and API-Staph (Biomerieux, France). S. fleurettii and S. vitulinus were identified at the species level by sequencing of 16S rRNA or sodA and Maldi-tof analysis (Microflex LT, Bruker Daltonics GmbH, Bremen) [19, 35, 40]. Species identification was confirmed by phylogenetic analysis of tuf gene nucleotide sequence [41].
β-lactam susceptibility
Was assessed by oxacillin Etest (bioMérieux, France). The breakpoint for defining susceptibility was evaluated as suggested by EUCAST (www.eucast.org). An epidemiological cut-off value (ECOFF) was determined by considering the MIC to oxacillin of S. sciuri and S. vitulinus isolates not carrying mecA (wild type) and isolates carrying mecA (non-wild type; resistant). All S. fleurettii strains carried mecA and were therefore considered resistant. The distribution of MIC values was plotted (S2 Fig) and isolates were considered susceptible when MIC < 3 μg/ml. Moreover, population analysis profiles (PAPs) for oxacillin were determined for representative isolates (28/60 S. sciuri exclusively carrying mecA1, 23/37 isolates carrying mecA, 9/9 isolates carrying mecA2) as previously described [42]. The PAP results of S. sciuri isolates have already been published [15, 21].
Whole-genome sequencing and de novo assembly
DNA was extracted using the phenol/chloroform extraction method (S. sciuri) and the DNEasy Blood & Tissue Kit (S. vitulinus and S. fleurettii) (Qiagen, Limburg, The Netherlands). Sequencing was performed using a HiSeq (Illumina, San Diego, USA) with an estimated coverage of 40x and a read length of 100 bp. The reads were assembled de novo using VELVET [43] and VelvetOptimiser (https://github.com/Victorian-Bioinformatics-Consortium/VelvetOptimiser.git).
Reference genome S. fleurettii 402567
DNA of S. fleurettii 402567 was prepared by phenol/chloroform extraction and was sequenced using PacBio RS apparatus (Pacific Biosciences, Menlo Park, USA). De novo assembly was performed using HGAP 3 (https://github.com/PacificBiosciences/Bioinformatics-Training/wiki/HGAP-in-SMRT-Analysis).
A reference genome was produced by combining Illumina and PacBio sequencing data for a single strain, S. fleurettii isolate 402567. PacBio reads were combined with Illumina reads obtained for each isolate in CLC Genomics Workbench (Qiagen, Hilden, Germany), using the Genome Finishing module. The resulting contigs were ordered using the closed genome of Staphylococcus xylosus, the species most closely related to S. fleurettii with a closed genome (NCBI accession number CP007208.1; average nucleotide identity with S. sciuri, 78%; S. vitulinus, 77.1%; and S. fleurettii, 78.5%). Gaps (eight) were closed by mapping Illumina data of remaining S. fleurettii strains to the contigs. The resulting closed genome was annotated with RAST (http://rast.nmpdr.org/).
Estimation of strain-to-strain phylogenies
The reference genome S. fleurettii 402567 was used to perform a SNP analysis of the predicted core genome of S. sciuri, S. vitulinus and S. fleurettii isolates. SNP analysis was performed using Stampy (version 1.0.11) where reads were mapped to the reference genome. SNP calling was performed using SAMtools (version 0.1.12), and Neighbor Joining (NJ) analysis was used to assess the phylogeny. Trees were drawn using FigTree (http://tree.bio.ed.ac.uk/software/figtree/).
Phylogenetic analysis of mecA homologues
Nucleotide sequences of mecA homologues were identified by BLAST analysis and were extracted from the sequence of the contigs. Alignments with the entire gene or regions corresponding to specific domains were performed with ClustalW [44]. Phylogenetic trees were constructed with a neighbor-joining algorithm. We used BEAST software (v1.8.3) [45] to investigate the temporal evolution of mecA homologues. Estimation of substitution rates and divergence times of the tree internal nodes was performed using the HKY nucleotide substitution model. The Markov chain Monte Carlo (MCMC) analysis was run up to 107 generations and checked for convergence by examining that the effective sample size (ESS) values were greater than 200 for all parameters. Strict, random, uncorrelated and fixed clock models under a constant population size model were compared for their fit to the data using marginal likelihood (stepping stone and path sampling) (see S3 Table) and Bayes factor (see S4 Table). The best-fit clock model (random clock) was then tested with the constant size population and the exponential growth population models. No significant differences in timescales or tree topology were obtained when the two different population size models were used. A burn-in of 10% was removed of each BEAST run and the maximum clade credibility (MCC) tree was selected from the posterior tree distribution using the program TreeAnnotator (available as part of the BEAST package). Final trees were annotated with FigTree (http://tree.bio.ed.ac.uk/software/figtree/). The BEAST analysis was performed for the entire set of mec homologue sequences and for the sequences belonging to each mec gene separately. To assess the impact of recombination on the phylogeny, the same analysis was repeated with the mec gene homologue sequences from which nucleotides under recombination were deleted (RDP4 software).
Estimation of dN/dS ratios
To verify if the non-binding and the transpeptidase domain of mecA1 were under positive selection, estimates of overall dN/dS ratios (number of non-synonymous substitutios per site/number of synonymous substitutions per site) were produced for the nucleotide sequence of each domain, using the program MEGA6 [46].
Estimation of recombination/mutation rates
RDP4 [47] was used to predict which parts of the mecA homologue sequences were under recombination and to estimate the mecA1 recombination/mutation rate.
Modeling of protein structure
The structure of representative proteins encoded by the mecA homologues was predicted using ModWeb (https://modbase.compbio.ucsf.edu/modweb/) [48]. Structures of one mecA allele, one mecA2 allele and six mecA1 alleles (representing each major clade of the phylogenetic tree, 0.015 distance cut off) were obtained. Alignments of the structures modeled with PBP2a (protein database, PDB code 1MWU) were produced in PyMol (The PyMOL Molecular Graphics System, Version 1.5.0.3 Schrödinger, LLC) and visually inspected for relevant alterations of the protein structure.
Assessment of genetic diversity and synteny of S. sciuri core genes
The genetic diversity of the different mecA homologues was assessed by the Simpson’s index of diversity (SID) [49], using a confidence interval of 95%. The online tool available at http://darwin.phyloviz.net/ComparingPartitions/ was used. To find the core genes of the 76 S. sciuri genomes, we used Prokka [50] and Roary [51]. The sequences of the aligned core genes were compared using Weblogo version 2.8.2 [52] and the number of conserved positions were determined for each core gene.
To determine the order of the 1759 core genes in each contig of the 76 S. sciuri assembled genomes a consensus sequence of each core gene was blasted against the 76 S. sciuri genomes and the reference genome NCTC12103 and their position assigned. The order of the core genes in each contig of the 76 genome sequences was compared to the order of the core genes in the NCTC12103 genome, and the total number of discontinuities was determined using an in-house script.
Statistical analysis
Association between variables within the data was done using the Qui2 test with 95% confidence level.
Purification of staphylococcal membrane fraction
S. aureus strain COL, S. epidermidis strain ATCC12228, S. sciuri strains K11, K7, K5 and K4, S. fleurettii strains 402567, CH22, CH28 and S. vitulinus strains H91, CH10 and CH15, were grown in 250 ml of TSB at 37°C with aeration to an OD600nm of 0.7. Cells were harvested, washed and ressuspended in buffer A (50 mM Tris pH 7.5, 150 mM NaCl, 5 mM MgCl2) with phenylmethylsulfonyl fluoride (0.5 mM) and submitted to freeze-thaw cycles. All subsequent steps were performed at 4°C. Lysostaphin (100 μg/ml), Lysozyme (50 μg/ml), DNase (10 μg/ml), RNase (10 μg/ml), PMSF (0.5 mM) β-mercaptoethanol (10 mM) were added and the cell suspensions were incubated on ice for 30 min, followed by 5 cycles of sonication of 30 sec and 2 min intervals. Unbroken cells and cellular debris were removed by centrifugation of 5 min at 5000 g and the resulting supernatants were centrifuged at 50,000 g for 1h and washed in 50 mM phosphate buffer, pH 7.0. The obtained membrane fraction was resuspended in 25mM phosphate buffer pH 7.0, 1% Triton X-100, 10 mM MgCl2, 20% glycerol. Total protein concentration was determined using the BCA assay (Pierce, Thermo Scientific, USA).
Detection of PBP2a by western blotting
Membrane preparations (50 μg) were separated by SDS polyacrylamide gel electrophoresis (8% acrylamide-0.06% bisacrylamide) at constant current of 20 mA. The proteins were transferred onto nitrocellulose Hybond-ECL membranes (GE Healthcare Life Sciences, USA) using the wet blotting system (Bio-Rad, USA) for 90 min. Membranes were kept on PBS-Tween with 5% low-fat milk O/N and incubated with 5 mM diethyl pyrocarbonate (DEPC), to inhibit binding of S. aureus protein A to IgG [53] and rabbit polyclonal anti PBP2a antibody (raised against the synthetic peptide NH2-CGSKKFEKGMKKLGVGEDIPSDYPF; RayBiotech) at 1:1000 dilution for 1 hour. After two washes the membranes were incubated with the anti-rabbit secondary antibody conjugated to horseradish peroxidase (PerkinElmer, USA) at 1:5000 dilution for 1 hour. The chemiluminiscent signal was detected using Western Lightning Plus-ECL (PerkinElmer) and CL-XPosure film (Thermo Scientific). The membrane was incubated in stripping buffer (62.5 mM Tris-HCL pH 6.7, 100 mM β -mercaptoethanol, 2% SDS) at 50°C for 30 min and re-hybridized with 5mM DEPC and polyclonal antibody raised against the amidase domain of S. aureus Atl protein, at 1:1000 dilution for 5h.
Accession numbers
The raw reads of the 106 isolates analyzed in this study and the closed genome of S. fleuretti were deposited in ENA with the following accession number PRJEB18761.
Supporting information
The distribution of the different mecA homologue alleles in the population of isolates studied is also shown. Phylogenetic group (S. sciuri sciuri, S. sciuri rodentius, S, sciuri carnaticus, S. sciuri new subspecies group 1, S. sciuri new subspecies group 2, S. vitulinus, S. fleurettii), origin of the strains and oxacillin MIC are also shown. β-lactam resistant strains are highlighted in bold. NB: non-binding domain: TP: transpeptidase domain.
(DOCX)
(XLSX)
(XLSX)
(XLSX)
mecA homologues. The sequences of each mec homologue gene was extracted from the de novo assembly contigs and aligned with ClustalW. The tree was performed with UPGMA method, under the Jukes-Cantor substitution model, with a bootstrap of 100 replicates. The unrooted tree is shown (A). Identification of recombination events among mecA1 alleles. The recombinant parts of mecA1 alleles are clustered apart from the remaining portion of the allele. Moreover, a color code is applied to identity the putative major parents that were involved in the recombination events (B).
(TIF)
Distribution of oxacillin MICs of S. sciuri (A) and S. vitulinus (B) as determined by Etest. “Wild-type” S. sciuri strains: S. sciuri strains carrying mecA1 only; “Resistant” S. sciuri strains: S. sciuri strains carrying mecA1 and mecA. “Wild-type” S. vitulinus strains: S. vitulinus strains carrying mecA2; “Resistant” S. vitulinus strains: S. vitulinus strains carrying mecA.
(TIF)
Unrooted phylogenetic tree based on the number of SNP differences found among the predicted core genome of the strains. The reference genome used was S. fleurettii 402567. S. fleurettii (A). S. vitulinus (B). S. sciuri (C).
(TIF)
Acknowledgments
The authors acknowledge Dr. Kloos for the unrestricted gift of the great majority of the S. sciuri isolates that were used in this study. In addition, we thank Dr. Ivo Sedlácek, Dr. Oto Melter and Dr. José Melo-Cristino for providing some of the S. sciuri strains that are part of this study and Dr. Engeline van Duijkeren from the National Institute for Public Health and the Environment (RIVM, Denmark) for providing the strains S. fleurettii 402567 and S. vitulinus 401946. We additionally thank Dr. Isabel Couto for the initial characterization of S. sciuri strains.
Data Availability
Data used in this study are deposited in ENA with the accession number PRJEB18761.
Funding Statement
This work was financially supported by: Project LISBOA-01-0145-FEDER-007660 (Microbiologia Molecular, Estrutural e Celular) funded by Fundo Europeu de Desenvolvimento Regional through COMPETE2020 - Programa Operacional Competitividade e Internacionalização and by national funds through Fundação para a Ciência e a Tecnologia; Project UID/Multi/04378/2013 (Unidade de Ciências Biomoleculares Aplicadas-UCIBIO), funded by national funds from Fundação para a Ciência e a Tecnologia and co-financed by the European Regional Development Fund under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007728); project PTDC/BIA-EVF/117507/2010 and PTDC/FIS-NAN/0117/2014 from Fundação para a Ciência e a Tecnologia; European Society of Clinical Microbiology and Infectious Diseases Research Grants 2010, awarded to MM; and US Public Health Service Award R01-AI457838-15, awarded to AT. JR was supported by fellowship SFRH / BD / 72675 / 2010 from Fundação para a Ciência e a Tecnologia and grant FEMS-RG-2014-0078 from the Federation of European Microbiology Societies.
References
- 1.Katayama Y, Ito T, Hiramatsu K. A new class of genetic element, staphylococcus cassette chromosome mec, encodes methicillin resistance in Staphylococcus aureus. Antimicrob Agents Chemother. 2000;44(6):1549–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boundy S, Safo MK, Wang L, Musayev FN, O'Farrell HC, Rife JP, et al. Characterization of the Staphylococcus aureus rRNA methyltransferase encoded by orfX, the gene containing the staphylococcal chromosome cassette mec (SCCmec) insertion site. J Biol Chem. 2013;288(1):132–40. PubMed Central PMCID: PMCPMC3537007. doi: 10.1074/jbc.M112.385138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Lencastre H, Oliveira D, Tomasz A. Antibiotic resistant Staphylococcus aureus: a paradigm of adaptive power. Curr Opin Microbiol. 2007;10(5):428–35. doi: 10.1016/j.mib.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hiramatsu K, Ito T, Tsubakishita S, Sasaki T, Takeuchi F, Morimoto Y, et al. Genomic Basis for Methicillin Resistance in Staphylococcus aureus. Infect Chemother. 2013;45(2):117–36. PubMed Central PMCID: PMCPMC3780952. doi: 10.3947/ic.2013.45.2.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monecke S, Coombs G, Shore AC, Coleman DC, Akpaka P, Borg M, et al. A field guide to pandemic, epidemic and sporadic clones of methicillin-resistant Staphylococcus aureus. PLoS One. 2011;6(4):e17936 PubMed Central PMCID: PMCPMC3071808. doi: 10.1371/journal.pone.0017936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuda C, Suvorov M, Vakulenko SB, Mobashery S. The basis for resistance to beta-lactam antibiotics by penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus. J Biol Chem. 2004;279(39):40802–6. doi: 10.1074/jbc.M403589200 [DOI] [PubMed] [Google Scholar]
- 7.Lim D, Strynadka NC. Structural basis for the beta lactam resistance of PBP2a from methicillin-resistant Staphylococcus aureus. Nat Struct Biol. 2002;9(11):870–6. doi: 10.1038/nsb858 [DOI] [PubMed] [Google Scholar]
- 8.Jevons MP, Coe AW, Parker MT. Methicillin resistance in staphylococci. Lancet. 1963;1(7287):904–7. [DOI] [PubMed] [Google Scholar]
- 9.Dyke KG, Jevons MP, Parker MT. Penicillinase production and intrinsic resistance to penicillins in Staphylococcus aureus. Lancet. 1966;1(7442):835–8. [DOI] [PubMed] [Google Scholar]
- 10.de Lencastre H, Chung M, Westh H. Archaic strains of methicillin-resistant Staphylococcus aureus: molecular and microbiological properties of isolates from the 1960s in Denmark. Microb Drug Resist. 2000;6(1):1–10. doi: 10.1089/mdr.2000.6.1 [DOI] [PubMed] [Google Scholar]
- 11.de Lencastre H, Tomasz A. Reassessment of the number of auxiliary genes essential for expression of high-level methicillin resistance in Staphylococcus aureus. Antimicrob Agents Chemother. 1994;38(11):2590–8. PubMed Central PMCID: PMCPMC188247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mwangi MM, Kim C, Chung M, Tsai J, Vijayadamodar G, Benitez M, et al. Whole-genome sequencing reveals a link between β-lactam resistance and synthetases of the alarmone (p)ppGpp in Staphylococcus aureus. Microb Drug Resist. 2013;19(3):153–9. PubMed Central PMCID: PMCPMC3662374. doi: 10.1089/mdr.2013.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim C, Mwangi M, Chung M, Milheiriço C, Milheirço C, de Lencastre H, et al. The mechanism of heterogeneous beta-lactam resistance in MRSA: key role of the stringent stress response. PLoS One. 2013;8(12):e82814 PubMed Central PMCID: PMCPMC3857269. doi: 10.1371/journal.pone.0082814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dordel J, Kim C, Chung M, Pardos de la Gándara M, Holden MT, Parkhill J, et al. Novel determinants of antibiotic resistance: identification of mutated loci in highly methicillin-resistant subpopulations of methicillin-resistant Staphylococcus aureus. MBio. 2014;5(2):e01000 PubMed Central PMCID: PMCPMC3993859. doi: 10.1128/mBio.01000-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Couto I, de Lencastre H, Severina E, Kloos W, Webster JA, Hubner RJ, et al. Ubiquitous presence of a mecA homologue in natural isolates of Staphylococcus sciuri. Microb Drug Resist. 1996;2(4):377–91. doi: 10.1089/mdr.1996.2.377 [DOI] [PubMed] [Google Scholar]
- 16.Couto I, Wu SW, Tomasz A, de Lencastre H. Development of methicillin resistance in clinical isolates of Staphylococcus sciuri by transcriptional activation of the mecA homologue native to the species. J Bacteriol. 2003;185(2):645–53. doi: 10.1128/JB.185.2.645-653.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu SW, de Lencastre H, Tomasz A. Recruitment of the mecA gene homologue of Staphylococcus sciuri into a resistance determinant and expression of the resistant phenotype in Staphylococcus aureus. J Bacteriol. 2001;183(8):2417–24. doi: 10.1128/JB.183.8.2417-2424.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antignac A, Tomasz A. Reconstruction of the phenotypes of methicillin-resistant Staphylococcus aureus by replacement of the staphylococcal cassette chromosome mec with a plasmid-borne copy of Staphylococcus sciuri pbpD gene. Antimicrob Agents Chemother. 2009;53(2):435–41. PubMed Central PMCID: PMCPMC2630592. doi: 10.1128/AAC.01099-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schnellmann C, Gerber V, Rossano A, Jaquier V, Panchaud Y, Doherr MG, et al. Presence of new mecA and mph(C) variants conferring antibiotic resistance in Staphylococcus spp. isolated from the skin of horses before and after clinic admission. J Clin Microbiol. 2006;44(12):4444–54. PubMed Central PMCID: PMCPMC1698435. doi: 10.1128/JCM.00868-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsubakishita S, Kuwahara-Arai K, Sasaki T, Hiramatsu K. Origin and molecular evolution of the determinant of methicillin resistance in staphylococci. Antimicrob Agents Chemother. 2010;54(10):4352–9. doi: 10.1128/AAC.00356-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Couto I, Sanches IS, Sá-Leão R, de Lencastre H. Molecular characterization of Staphylococcus sciuri strains isolated from humans. J Clin Microbiol. 2000;38(3):1136–43. PubMed Central PMCID: PMCPMC86357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kloos WE, Ballard DN, Webster JA, Hubner RJ, Tomasz A, Couto I, et al. Ribotype delineation and description of Staphylococcus sciuri subspecies and their potential as reservoirs of methicillin resistance and staphylolytic enzyme genes. Int J Syst Bacteriol. 1997;47(2):313–23. doi: 10.1099/00207713-47-2-313 [DOI] [PubMed] [Google Scholar]
- 23.Ryffel C, Kayser FH, Berger-Bächi B. Correlation between regulation of mecA transcription and expression of methicillin resistance in staphylococci. Antimicrob Agents Chemother. 1992;36(1):25–31. PubMed Central PMCID: PMCPMC189220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hackbarth CJ, Chambers HF. blaI and blaR1 regulate beta-lactamase and PBP 2a production in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 1993;37(5):1144–9. PubMed Central PMCID: PMCPMC187918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Enright MC, Robinson DA, Randle G, Feil EJ, Grundmann H, Spratt BG. The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc Natl Acad Sci U S A. 2002;99(11):7687–92. doi: 10.1073/pnas.122108599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliveira DC, Tomasz A, de Lencastre H. Secrets of success of a human pathogen: molecular evolution of pandemic clones of meticillin-resistant Staphylococcus aureus. Lancet Infect Dis. 2002;2(3):180–9. [DOI] [PubMed] [Google Scholar]
- 27.de Lencastre H, de Jonge BL, Matthews PR, Tomasz A. Molecular aspects of methicillin resistance in Staphylococcus aureus. J Antimicrob Chemother. 1994;33(1):7–24. [DOI] [PubMed] [Google Scholar]
- 28.Ba X, Harrison EM, Edwards GF, Holden MT, Larsen AR, Petersen A, et al. Novel mutations in penicillin-binding protein genes in clinical Staphylococcus aureus isolates that are methicillin resistant on susceptibility testing, but lack the mec gene. J Antimicrob Chemother. 2014;69(3):594–7. PubMed Central PMCID: PMCPMC3922151. doi: 10.1093/jac/dkt418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chambers HF, Deleo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–41. PubMed Central PMCID: PMCPMC2871281. doi: 10.1038/nrmicro2200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lapierre M, Blin C, Lambert A, Achaz G, Rocha EP. The Impact of Selection, Gene Conversion, and Biased Sampling on the Assessment of Microbial Demography. Mol Biol Evol. 2016;33(7):1711–25. PubMed Central PMCID: PMCPMC4915353. doi: 10.1093/molbev/msw048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Europea Parliament and the Council of the EU (1998) Decision number 2119/98/EC of the European Parliament and of the Council of 24 September 1998: setting up a network for the epidemiological surveillance and control of communicable diseases in the community. Official J Eur Communities L268/1.
- 32.The European Commission of the European Communities (2000) Commission decision of 22 December 1999 on the communicable diseases to be progressively covered by the community network under decision number 2119/98/EC of the Parliament and of the Council. Official J Eur Communities L 28/50.
- 33.Bagcigil FA, Moodley A, Baptiste KE, Jensen VF, Guardabassi L. Occurrence, species distribution, antimicrobial resistance and clonality of methicillin- and erythromycin-resistant staphylococci in the nasal cavity of domestic animals. Vet Microbiol. 2007;121(3–4):307–15. doi: 10.1016/j.vetmic.2006.12.007 [DOI] [PubMed] [Google Scholar]
- 34.Moodley A, Guardabassi L. Clonal spread of methicillin-resistant coagulase-negative staphylococci among horses, personnel and environmental sites at equine facilities. Vet Microbiol. 2009;137(3–4):397–401. doi: 10.1016/j.vetmic.2009.01.034 [DOI] [PubMed] [Google Scholar]
- 35.Frey Y, Rodriguez JP, Thomann A, Schwendener S, Perreten V. Genetic characterization of antimicrobial resistance in coagulase-negative staphylococci from bovine mastitis milk. J Dairy Sci. 2013;96(4):2247–57. doi: 10.3168/jds.2012-6091 [DOI] [PubMed] [Google Scholar]
- 36.Nemeghaire S, Argudín MA, Feßler AT, Hauschild T, Schwarz S, Butaye P. The ecological importance of the Staphylococcus sciuri species group as a reservoir for resistance and virulence genes. Vet Microbiol. 2014;171(3–4):342–56. doi: 10.1016/j.vetmic.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 37.Nagase N, Sasaki A, Yamashita K, Shimizu A, Wakita Y, Kitai S, et al. Isolation and species distribution of staphylococci from animal and human skin. J Vet Med Sci. 2002;64(3):245–50. [DOI] [PubMed] [Google Scholar]
- 38.Stepanovic S, Dakic I, Morrison D, Hauschild T, Jezek P, Petrás P, et al. Identification and characterization of clinical isolates of members of the Staphylococcus sciuri group. J Clin Microbiol. 2005;43(2):956–8. PubMed Central PMCID: PMCPMC548121. doi: 10.1128/JCM.43.2.956-958.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calazans-Silva AC, Medeiros PT, Araujo DM, Carvalho BO, Coelho IS, Coelho SM, et al. Genetic analysis of mecA gene and detection of homologue pbpD in Stahylococcus sciuri group. Braz J Microbiol. 2014;45(2):651–5. PubMed Central PMCID: PMCPMC4166295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poyart C, Quesne G, Boumaila C, Trieu-Cuot P. Rapid and accurate species-level identification of coagulase-negative staphylococci by using the sodA gene as a target. J Clin Microbiol. 2001;39(12):4296–301. PubMed Central PMCID: PMCPMC88539. doi: 10.1128/JCM.39.12.4296-4301.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martineau F, Picard FJ, Ke D, Paradis S, Roy PH, Ouellette M, et al. Development of a PCR assay for identification of staphylococci at genus and species levels. J Clin Microbiol. 2001;39(7):2541–7. PubMed Central PMCID: PMCPMC88182. doi: 10.1128/JCM.39.7.2541-2547.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Lencastre H, Sa Figueiredo AM, Urban C, Rahal J, Tomasz A. Multiple mechanisms of methicillin resistance and improved methods for detection in clinical isolates of Staphylococcus aureus. Antimicrob Agents Chemother. 1991;35(4):632–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zerbino DR, Birney E. Velvet: algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008;18(5):821–9. PubMed Central PMCID: PMCPMC2336801. doi: 10.1101/gr.074492.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thompson JD, Higgins DG, Gibson TJ. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994;22(22):4673–80. PubMed Central PMCID: PMCPMC308517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Drummond AJ, Suchard MA, Xie D, Rambaut A. Bayesian phylogenetics with BEAUti and the BEAST 1.7. Mol Biol Evol. 2012;29(8):1969–73. PubMed Central PMCID: PMCPMC3408070. doi: 10.1093/molbev/mss075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28(10):2731–9. PubMed Central PMCID: PMCPMC3203626. doi: 10.1093/molbev/msr121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin D, Rybicki E. RDP: detection of recombination amongst aligned sequences. Bioinformatics. 2000;16(6):562–3. [DOI] [PubMed] [Google Scholar]
- 48.Martí-Renom MA, Stuart AC, Fiser A, Sánchez R, Melo F, Sali A. Comparative protein structure modeling of genes and genomes. Annu Rev Biophys Biomol Struct. 2000;29:291–325. doi: 10.1146/annurev.biophys.29.1.291 [DOI] [PubMed] [Google Scholar]
- 49.Simpson EH. Measurement of species diversity. Nature. 1949;163:688. [Google Scholar]
- 50.Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30(14):2068–9. doi: 10.1093/bioinformatics/btu153 [DOI] [PubMed] [Google Scholar]
- 51.Page AJ, Cummins CA, Hunt M, Wong VK, Reuter S, Holden MT, et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics. 2015;31(22):3691–3. PubMed Central PMCID: PMCPMC4817141. doi: 10.1093/bioinformatics/btv421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crooks GE, Hon G, Chandonia JM, Brenner SE. WebLogo: a sequence logo generator. Genome Res. 2004;14(6):1188–90. PubMed Central PMCID: PMCPMC419797. doi: 10.1101/gr.849004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nguyen HM, Rocha MA, Chintalacharuvu KR, Beenhouwer DO. Detection and quantification of Panton-Valentine leukocidin in Staphylococcus aureus cultures by ELISA and Western blotting: diethylpyrocarbonate inhibits binding of protein A to IgG. J Immunol Methods. 2010;356(1–2):1–5. PubMed Central PMCID: PMCPMC2878937. doi: 10.1016/j.jim.2010.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The distribution of the different mecA homologue alleles in the population of isolates studied is also shown. Phylogenetic group (S. sciuri sciuri, S. sciuri rodentius, S, sciuri carnaticus, S. sciuri new subspecies group 1, S. sciuri new subspecies group 2, S. vitulinus, S. fleurettii), origin of the strains and oxacillin MIC are also shown. β-lactam resistant strains are highlighted in bold. NB: non-binding domain: TP: transpeptidase domain.
(DOCX)
(XLSX)
(XLSX)
(XLSX)
mecA homologues. The sequences of each mec homologue gene was extracted from the de novo assembly contigs and aligned with ClustalW. The tree was performed with UPGMA method, under the Jukes-Cantor substitution model, with a bootstrap of 100 replicates. The unrooted tree is shown (A). Identification of recombination events among mecA1 alleles. The recombinant parts of mecA1 alleles are clustered apart from the remaining portion of the allele. Moreover, a color code is applied to identity the putative major parents that were involved in the recombination events (B).
(TIF)
Distribution of oxacillin MICs of S. sciuri (A) and S. vitulinus (B) as determined by Etest. “Wild-type” S. sciuri strains: S. sciuri strains carrying mecA1 only; “Resistant” S. sciuri strains: S. sciuri strains carrying mecA1 and mecA. “Wild-type” S. vitulinus strains: S. vitulinus strains carrying mecA2; “Resistant” S. vitulinus strains: S. vitulinus strains carrying mecA.
(TIF)
Unrooted phylogenetic tree based on the number of SNP differences found among the predicted core genome of the strains. The reference genome used was S. fleurettii 402567. S. fleurettii (A). S. vitulinus (B). S. sciuri (C).
(TIF)
Data Availability Statement
Data used in this study are deposited in ENA with the accession number PRJEB18761.