Abstract
Given the lack of active nurses in industrialized countries throughout the world, in combination with demographic changes, it is of utmost importance to protect nurses’ well-being and to prevent psychological distress, because of their strong association with premature occupational leave. The aim of this study was to investigate the effects of quality of leadership and social support at work on well-being and psychological distress of nurses and to determine whether nurses’ overcommitment mediates the relationship between the abovementioned determinants and the outcomes. A cross-sectional survey design was used to gather our data. This study utilized part of the database of the Nurses’ Early Exit Study. A total of 34,771 nurses (covering all nurse qualifications) working in hospitals, nursing homes, and home-care institutions in 8 European countries filled out a questionnaire (response rate = 51.4%). For all model variables (job satisfaction, satisfaction with salary, positive affectivity, personal burnout, negative affectivity, quality of leadership, social support from immediate supervisor, social support from near colleagues, and overcommitment), psychometrically sound, that is, valid and reliable measures were used. Outcomes from testing a structural equation mediation model indicated that, respectively, positive and negative influences of leadership quality and social support from supervisor and colleagues on nurses’ well-being and psychological distress are partially mediated, that is, reduced, by nurses’ overcommitment. Social work environment is highly important in relation to nurses’ well-being and psychological distress.
Keywords: overcommitment, psychological distress, quality of leadership, social support at work, well-being
1. Introduction
Like in all industrialized countries across the world, European countries face a serious shortage of nurses.[1,2] The aging and dejuvenization of the working population,[3] together with the decreasing rates of nurses entering the labor market, are worsening this situation. All in all, the demands of nurses at work are high: work conditions change rapidly, and nurses are supposed to ensure high standards of quality and professionalism,[4] and to handle complex situations effectively.[5–7] Obviously, inherent tensions in nursing, such as time pressure, staff shortages, and increasing demands for high performance,[8,9] exist and are examples of physically demanding work structures combined with emotionally demanding work settings.[10] On top of this, most Western countries struggle with an increased need for nursing care, as the “baby boomer” generation reaches retirement age.[11] In a situation of massive premature leave (before one's retirement age) of nurses from a healthcare institution, which is highly likely in case nurses lack well-being and suffer from psychological distress,[12] both highly needed organizational and individual expertise is lost, and the employer needs to invest huge costs in recruiting, hiring, and training new staff.[13] In the next section, we conceptualize the key outcome variables that are dealt with in our study.
Psychological well-being is considered to be a combination of positive affective states and functioning effectively.[14,15] In line with Dodge et al[16] who argued that psychological, social, and physical resources should be part of the concept of well-being, we included satisfaction with payment as a component of well-being, next to job satisfaction and positive affectivity.[17] Negative affectivity, reflected in emotions such as anxiety, sadness, irritability, is considered to be part of psychological distress, which is strongly related with reduced quality and duration of life, and increased use of health services.[18] Next to negative affectivity, we include burnout as an indicator of psychological distress. The following paragraphs go into the predictor variables and the mediator that have been incorporated in our empirical work.
Given the serious lack of sufficiently qualified applicants for nursing education in many European countries,[19] the objective of our study was to better understand how organizational determinants, such as quality of leadership and social support at the workplace, may increase nurses’ well-being and prevent psychological distress and to investigate the possible mediating role of overcommitment. Quality of leadership can be defined as the extent to which the leader actively invests in a positive work climate, provides clarity, and puts efforts to achieve a common goal.[20] It has been identified as an important factor that may be related to important employee outcomes, such as job performance, job satisfaction, retention,[21,22] and to the workers’ employability.[10,23] High-quality leaders are able to generate a favorable work climate[10,24] by encouraging sound communication processes and by enabling their staff members to participate in decision-making. In addition, quality of leadership includes competences, such as dealing with interpersonal conflict and hostility, establishing more cooperative relationships.[25] Based on the above, we hypothesized that quality of leadership is an important predictor of well-being and psychological distress.[26]
Nurses’ social support of their supervisor and near colleagues is one of the most important factors when facing challenging work demands.[12] Social support can be defined by the availability of helping relations to others and by its quality[27] and may consist of direct help, feedback, information, and emotional support.[28] Social support at work is positively related to nurses’ staying in their job,[29] to further professional development,[30] to satisfaction with their work,[10,24,31] and to well-being,[32] and it negatively relates to stress reactions, burnout, and absenteeism.[33–35]
In addition, as previously indicated, we also investigated whether overcommitment might play a mediating role in the hypothesized relationships. Although the possible impact of similar determinants in the light of well-being and psychological distress has been dealt with in previous scholarly work,[36,37] to the best of our knowledge, no research up to now has addressed a model wherein the possible mediating role of nurses’ overcommitment was examined. The Effort–Reward Imbalance (ERI) model[38] shows the interactions between the work environment and its direct or indirect effect on employees’ health, and its general assumption comprises that employees spent effort at work in order to get reward in terms of money, opportunities for better jobs, or reputation. However, as there is often an imbalance between effort and reward, that is, the experience of high effort and low reward, many employees may suffer from work-related stress and illness. This imbalance could be caused by structural conditions, such as too many stressful reorganizations within a short time span, but may also concern individual-level factors, such as working overtime while facing a lack of career opportunities.[39] Overcommitment as a cognitive and motivational pattern is characterized by an excessive job involvement[40] that hinders the employee to balance his/her efforts and rewards. It appears that in case employees experience mastering challenging situations as a reward and overestimate their coping competencies, this might lead to an inability to recover fully, and through this to negative effects for health.[40]
In order to theoretically frame our research model and to justify the hypothesized associations between the key variables, we build upon COR (conservation of resources) theory[41,42] and aim to contribute to the scholarly and societal debates on the relationship between work conditions and healthcare professionals’ individual outcomes. COR theory is based on the assumption that people are focused on protecting the resources they have, in order to be able to respond to all kinds of demands that are posed to them, as the loss of valuable resources is endangering their abilities to cope.[41](p.513). In other words, when, in our case, nurses perceive a threat or an actual loss of resources (in our study social work context factors), or when they fail to receive sufficient return on their investment of resources (in our model overcommitment), they are assumed to experience negative individual outcomes (in our model a decrease in well-being and an increase in distress) (“loss spiral”)[41] Analogously, in case nurses’ social work context is perceived to be a resource, rather than as a stressor or demand, (cf.),[43] it is plausible that they may gain from it, leading to a higher amount of positive individual outcomes (in our model an increase in well-being and a decrease in psychological distress) (“gain spiral”).[41] Therefore, in this contribution, and to prevent chance capitalization, both a “loss” and “gain” spiral will be tested simultaneously.
2. Methodology
2.1. Sample and procedure
This study utilized part of the database of a large European study on nurses’ reasons, circumstances, and consequences surrounding premature departure from the nursing profession (Nurses’ Early Exit [NEXT]),[1] financed by the European Commission within the 5th framework program. The NEXT study has been approved by the ethical committee of the University of Wuppertal in Germany. Participating countries were Belgium, Germany, Finland, France, Italy, the Netherlands, Poland, and Slovakia. Stratified sampling has been used in order to, as far as possible, reflect the national distribution of nurses working in 3 different types of institutions (hospitals, nursing homes, and home-care institutions) and to cover the different regions in each country in a representative way. In particular, we have tried our best to ensure proportionate ratio regarding employment figures, gender distribution, age structure, and working hours across the distinguished types of institutions, while at the same time incorporating the geographical spread across the specific regions in each participating country.[1]
The questionnaires were sent to a total of 77,681 nurses resided in these countries (covering all nurse qualification levels), who were working in hospitals, nursing homes, and home-care institutions. A total of 39,894 participants returned the questionnaire, implying a response rate of 51.4% for the total investigation, ranging from 30.0% to 76.9% for the participating countries. After first data processing and cleaning, the final sample of this study consisted of 34,771 nurses.
3. Measures
3.1. Dependent variables
Job satisfaction was measured with a thoroughly validated 4-item scale from the Copenhagen Psychosocial Questionnaire (COPSOQ)[44] (e.g., how pleased are you with the physical working conditions?). For all items, a 4-point rating scale was used (response categories: very unsatisfied, unsatisfied, satisfied, and very satisfied). Internal consistencies (Cronbach α) ranged from 0.69 to 0.82 across participating countries.
Satisfaction with salary: This 3-item scale was developed by the NEXT study group[1] (e.g., how satisfied are you with your pay in relation to your need for income?). All items were scored using a 5-point rating scale ranging from not at all to very much. Internal consistencies (Cronbach α) ranged from 0.70 to 0.84 across participating countries.
Positive affectivity: This scale was developed by Watson et al[45] (Positive and Negative Affect Schedule [PANAS]). Participants rated the extent to which they “in general” feel in a certain way. Items were alert, excited, active, interested, attentive, determined, proud, inspired, strong, and enthusiastic and were all scored using a 5-point rating scale (response categories: very slightly or not at all, a little, moderately, quite a bit, and extremely). Internal consistencies (Cronbach α) ranged from 0.68 to 0.77 across participating countries.
Personal burnout was measured with a 6-item scale from the COPSOQ.[44] All items were scored using a 5-point rating scale (response categories: never/almost never, once or a few times during a month, once or twice a week, 3–5 times during a week, and [almost] every day) and indicated how often they feel tired, are physically exhausted, are emotionally exhausted, think: I can’t take it anymore, feel worn out, and feel weak and susceptible to illness. Internal consistencies (Cronbach α) ranged from 0.84 to 0.91 across participating countries.
Negative affectivity: This scale was developed by Watson et al[45] (PANAS). Participants rated the extent to which they “in general” feel in a certain way. Items were jittery, nervous, irritable, upset, distressed, scared, guilty afraid, ashamed, and hostile and were all scored using a 5-point rating scale (response categories: very slightly or not at all, a little, moderately, quite a bit, and extremely). Internal consistencies (Cronbach α) ranged from 0.79 to 0.87 across participating countries.
3.2. Independent variables
Quality of leadership: The quality of leadership scale was taken from the COPSOQ.[44] All 4 items (e.g., to what extent would you say that your superior makes sure that the individual member of the staff has good development opportunities?) were scored using a 5-point rating scale (response categories: to a very small extent, not very much, somewhat, to some extent, and to a large extent). Internal consistencies (Cronbach α) ranged from 0.87 to 0.92 across participating countries.
Social support from immediate supervisor: A total of 4 items from Van der Heijden[24] were used to measure this variable: “Is your immediate supervisor able to evaluate the value of your work and its results?,” “Does your immediate supervisor regularly express an opinion on your work?,” “Is your immediate supervisor in general ready to help you with the performance of your tasks?,” and “Does your immediate supervisor regularly give you supportive advice?.” For the first item, a 6-point rating scale was used, ranging from (1) not at all to (6) very much. For the second and fourth item, a 6-point rating scale was used, ranging from (1) never to (6) very often. For the third item, a 6-point rating scale was used, ranging from (1) in my opinion, (s)he shows little willingness to help me to (6) in my opinion, (s)he is very willing to help me. Internal consistencies (Cronbach α) ranged from 0.81 to 0.87 across participating countries.
Social support from near colleagues: This variable was measured by nominally identical items,[24] with obviously “near colleagues” instead of “immediate supervisor” in the item formulation. Internal consistencies (Cronbach α) ranged from 0.72 to 0.79 across participating countries.
3.3. Mediator
Overcommitment: This scale was taken from the ERI model[38] and comprised 6 items (e.g., I get easily overwhelmed by time pressures at work). All items were scored using a 4-point rating scale (response categories: strongly disagree, disagree, agree, and strongly agree). Internal consistencies (Cronbach α) ranged from 0.70 to 0.82 across participating countries.
3.4. Control variables
In line with previous research,[36] and to control for possible confounding effects, age and gender were used as control variables. Age was measured in years; gender was measured with a binary item (male/female).
3.5. Analysis
The influence of leadership quality and social support from key parties (i.e., one's supervisor and near colleagues) on nurses’ well-being and psychological distress, and the mediating role of nurses’ overcommitment, was investigated by means of a Structural Equation Model, which involved 2 sequential steps in the analysis. In the first step, the measurement model of the 2 endogenous latent constructs well-being and psychological distress was estimated. Similar to previous research about the psychometric structure of well-being and psychological distress,[46] job satisfaction, satisfaction with salary, and positive affectivity were used as manifest indicators of well-being. Personal burnout and negative affectivity were used as manifest indicators of psychological distress. This hypothesized structure showed a very good fit to the data, and it was found that all indicators loaded significantly on the intended factor, and that no cross-loadings were present. In the second step, the manifest independent variables, the mediator, and the control variables were included in the model, and the full structural equation model was estimated. Model fit was assessed by commonly used criteria[47]: the result of the χ2 test (nonsignificant test indicates a good fit), Root Mean Square Error of Approximation (RMSEA) (root [good fit <0.05], Comparative Fit Index [CFI]/Tucker–Lewis Index [TLI] [good fit >0.95], and Standardized Root Mean Square Residual [SRMR] [good fit <0.05]).Correlation residuals were checked to identify possible model misspecifications. Bootstrapped confidence intervals (CIs) for parameter estimates were calculated. All estimation procedures and calculations were done with Mplus 7 (Muthén & Muthén, Los Angeles, CA).[48]
4. Results
Descriptive statistics of all model variables are summarized in Table 1. The final model is illustrated in Fig. 1. After the specification of 2 residual correlations (between positive and negative affectivity, on the one hand, and job satisfaction and satisfaction with salary, on the other hand), the measurement model showed a very good fit to the data (χ2 = 66.536, P = 0.000; RMSEA = 0.028; CFI/TLI = 0.997/0.985; SRMR = 0.008) (RMSEA, CFI, TLI, and SRMR). Thus, estimation of the full structural equation model was warranted.
Table 1.
Descriptive statistics: correlations.
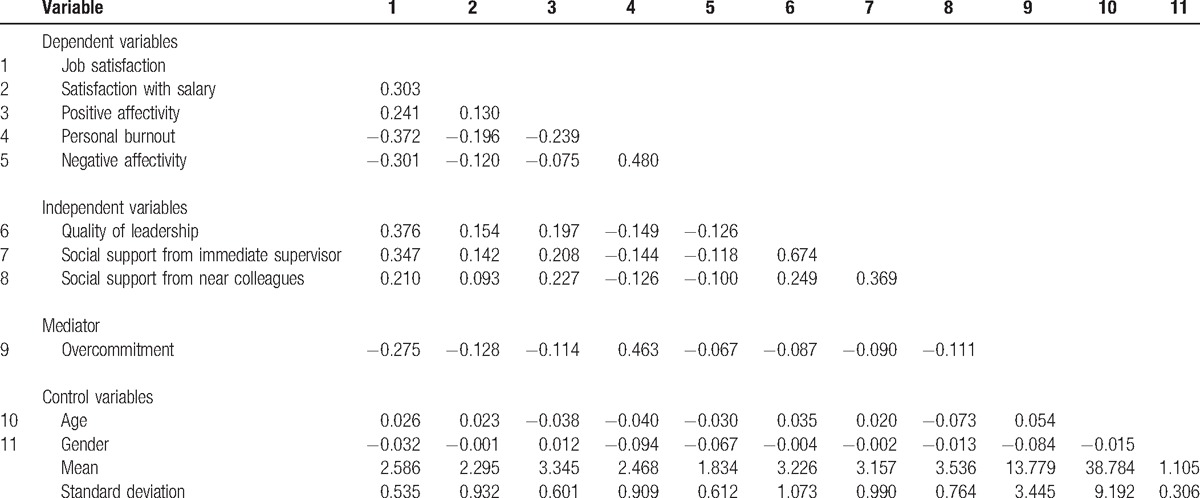
Figure 1.
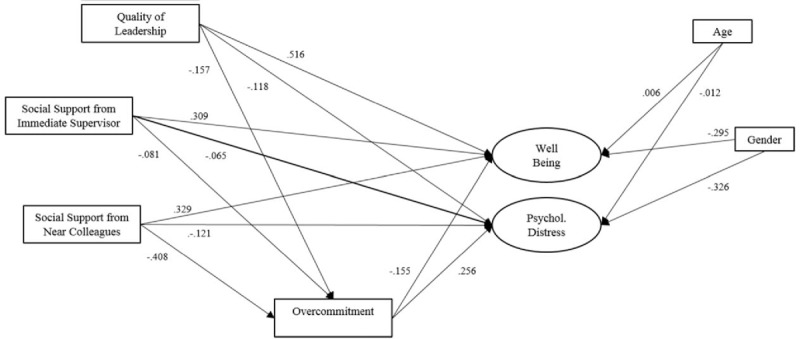
The final SEM model. Only significant (unstandardized) coefficients are shown. Model fit: χ2 = 1091.378, P = 0.000; RMSEA = 0.037; CFI/TLI = 0.971/0.941; SRMR = 0.021. Measurement model not shown. CFI = Comparative Fit Index, RMSEA = Root Mean Square Error of Approximation, SEM = Structural Equation Modelling, SRMR = Standardized Root Mean Square Residual, TLI = Tucker–Lewis Index.
In addition, female nurses, compared to their male counterparts, experienced higher well-being, yet, higher psychological distress, at the same time. Moreover, well-being appeared to increase with age, while psychological distress was found to be more pronounced among younger nurses, and appeared to decline across the life span. Regarding the mediating role of overcommitment in the relationship between social support from supervisors/colleagues and leadership quality, on the one hand, and well-being and psychological distress, on the other hand, the overarching pattern of results was as follows. Quality of leadership (β = 0.516, standard deviation [SD] = 0.021, 95% CI = [0.483, 0.550]), social support from one's supervisor (β = 0.309, SD = 0.019, 95% CI = [0.278, 0.340]), and social support from near colleagues (β = 0.329, SD = 0.020, 95% CI = [0.297, 0.362]) had a positive influence on nurses’ well-being. These direct effects, however, appeared to be partially mediated by nurses’ overcommitment. More specifically, the total effect of social support from one's supervisor was reduced by βind = 0.013 (SD = 0.004, 95% CI = [0.005, 0.020]), while the total effect of social support from near colleagues was reduced by βind = 0.063 (SD = 0.005, 95% CI = [0.055, 0.071]), and, finally, the total effect of quality of leadership was reduced by βind = 0.024 (SD = 0.004, 95% CI = [0.018, 0.031]).
Moreover, quality of leadership (β = −0.118, SD = 0.011, 95% CI = [−0.136, −0.100]), social support from one's supervisor (β = −0.065, SD = 0.012, 95% CI = [−0.086, −0.045]), and social support from near colleagues (β = −0.121, SD = 0.012, 95% CI = [−0.141, −0.101]) had a negative influence on nurses’ psychological distress. In other words, all 3 determinant factors were able to diminish nurses’ psychological distress. These direct effects again appeared to be reduced, that is, partially mediated, through nurses’ overcommitment. More specifically, the total effect of quality of leadership was reduced by βind = −0.040 (SD = 0.006, 95% CI = [−0.051, −0.030], while the total effect of social support from one's supervisors was reduced by βind = −0.021 (SD = 0.007, 95% CI = [−0.032, −0.009], and, finally, the total effect of social support from near colleagues was reduced by βind = −0.104 (SD = 0.007, 95% CI = [−0.117, −0.092]). Taken together, the significant, respectively positive and negative, influences of leadership quality and social support from one's supervisor and near colleagues on nurses’ well-being and psychological distress were indeed reduced by nurses’ overcommitment. Furthermore, all 3 factors, and, in particular, social support from colleagues, also showed the potential to reduce nurses’ overcommitment: quality of leadership (β = −0.157, SD = 0.025, 95% CI = [−0.198, −0.116]), social support from one's supervisor (β = −0.081, SD = 0.028, 95% CI = [−0.126, −0.035]), and social support from near colleagues (β = −0.408, SD = 0.028, 95% CI = [−0.455, −0.362]) were all negatively related to nurses’ overcommitment.
5. Discussion
COR theory[41,42] was used to theoretically frame a research model that was aimed to investigate the effect of nurses’ social work environment (i.e., quality of leadership and social support from supervisor/near colleagues) on well-being and psychological distress, and to determine whether nurses’ overcommitment mediates this model's relationships. In line with COR theorizing, we found empirical support for both the so-called loss and gain spiral that were hypothesized. More specifically, in case nurses perceive their social work environment as threatening or when they experience a lack of social support from key parties in the organization (i.e., their supervisor and near colleagues), it is likely that their well-being will decrease and their psychological distress will increase, in particular so in case they are overcommitted to their work (“loss” spiral). In a similar vein, in case nurses perceive an ample amount of support from key parties, it is likely that these individual outcomes will improve, reflected in an increase in well-being and a decrease in psychological distress, yet, especially so when they are not overcommitted to their job (“gain” spiral). Moreover, it appears that a high-quality social work environment can also prevent nurses from being overcommitted to their job.
Because we used self-report measures for all model variables, a common-method bias may exist.[49] Future work might incorporate both nurses’ self-assessments and assessments by supervisors and/or near colleagues to increase the validity of the outcomes. Moreover, future research is needed to investigate the possible impact of other factors on well-being and psychological distress, such as work–life balance, and to further investigate possible moderator effects, such as nursing team size and climate, and other organizational, team, and work characteristics such as task interdependence. We may also conduct more research testing possible country and cultural differences in our model relationships. In addition, since the investigated variables are not static, there is a need for getting more insight in processes of change and development, which requires longitudinal studies. Nevertheless, we think that our results are noteworthy and add to the insights obtained from previous work in the relationship between social work context and individual outcomes.
This study indicates that nurses’ social work environment is highly important and that their well-being might be at stake in case they experience an unsupportive work environment, reflected in inadequate leadership, and a lack of social support from one's supervisor and near colleagues. Healthcare organizations should focus on increasing awareness among supervisors and nursing staff by paying thorough attention to possible hindering and stimulating effects of nurses’ social work environment, and the role they themselves play in this regard. Nurses should provide interpersonal support to one another but should also take the responsibility to request for it if needed. Obviously, a climate that is characterized by safety and integrity is key here, and by monitoring the quality of the working climate, by protecting them against overcommitment, and by enhancing the sustainability of their careers throughout the life span, that is, until official retirement age,[10,50] their well-being can be protected. The latter is highly important to safeguard both the quality and quantity of health care that will be provided in the future, and to secure its supply.
Footnotes
Abbreviations: CFI = Comparative Fit Index, COPSOQ = Copenhagen Psychosocial Questionnaire, COR = conservation of resources, ERI = Effort–Reward Imbalance, NEXT = Nurses’ Early Exit, PANAS = Positive and Negative Affect Schedule, RMSEA = root mean square error of approximation, SRMR = standardized root mean square residual, TLI = Tucker–Lewis Index.
Funding/support: The present study was financed by the European Commission within the 5th framework program.
The authors have no conflicts of interest to disclose.
References
- [1].Hasselhorn H, Tackenberg P, Mueller B. Working conditions and intent to leave the profession among nursing staff in Europe. A Research Project Initiated by SALTSA (Joint Program for Working Life Research in Europe) and Funded by the European Committee (QLK6-CT-2001-00475). Uppsala, Sweden:SALTSA: European work life research at Uppsala University; 2003;http://www.turi-network.eu/Members/Full-members/SALTSA-European-work-life-research-at-Uppsala-University [Google Scholar]
- [2].Boamah SA, Laschinger H. The influence of areas of worklife fit and work-life interference on burnout and turnover intentions among new graduate nurses. J Nurs Manag 2016;24:E164–74. [DOI] [PubMed] [Google Scholar]
- [3].Shultz KS, Adams GA. Aging and Work in the 21st Century. London:Lawrence Erlbaum Associates; 2007. [Google Scholar]
- [4].Collin K, Paloniemi S, Mecklin JP. Promoting inter-professional teamwork and learning. J Educ Work 2010;23:43–63. [Google Scholar]
- [5].Berings MGMC, Poell RF, Van Veldhoven MJ. van Woerkom MJ, Poell RF. Antecedents of nurses’ on-the-job learning. Workplace Learning: Concepts, Measurement and Application. London:Routledge; 2010. 71–87. [Google Scholar]
- [6].Mukamel DB, Temkin-Greener H, Delavan R, et al. Team performance and risk-adjusted health outcomes in the Program of All-Inclusive Care for the Elderly (PACE). Gerontologist 2006;46:227–37. [DOI] [PubMed] [Google Scholar]
- [7].Shin IS, Kim JH. The effect of problem-based learning in nursing education: a meta-analysis. Adv Health Sci Educ 2013;18:1103–20. [DOI] [PubMed] [Google Scholar]
- [8].Heinemann GD, Zeiss AM. Team Performance in Health Care: Assessment, and Development. Berlin:Springer Science & Business Media; 2002. [Google Scholar]
- [9].Gartmeier M, Gruber H, Heid H. Tracing error-related knowledge in interview data: negative knowledge in elder care nursing. Educ Gerontol 2010;36:733–52. [Google Scholar]
- [10].Van der Heijden BIJM, Demerouti E, Bakker AB, et al. Work-home interference among nurses: reciprocal relationships with job demands and health. J Adv Nurs 2008;62:572–84. [DOI] [PubMed] [Google Scholar]
- [11].Buchan J, Duffield C, Jordan A. Solving’ nursing shortages: do we need a New Agenda? J Nurs Manag 2015;23:543–5. [DOI] [PubMed] [Google Scholar]
- [12].Estryn-Behar M, Van der Heijden BIJM, Oginska H, et al. The impact of social work environment, teamwork characteristics, burnout and personal factors upon intent to leave among European nurses. Med Care 2007;45:939–50. [DOI] [PubMed] [Google Scholar]
- [13].Kammeyer-Mueller JD, Wanberg CR. Unwrapping the organizational entry process: disentangling multiple antecedents and their pathways to adjustment. J Appl Psychol 2003;88:779–94. [DOI] [PubMed] [Google Scholar]
- [14].Huppert FA. Psychological well-being: evidence regarding its causes and consequences. Appl Psychol Health Well-Being 2009;1:137–64. [Google Scholar]
- [15].Winefield HR, Gill TK, Taylor AW, et al. Psychological well-being and psychological distress: is it necessary to measure both? Psychol Well-Being: Theory Res Pract 2012;2:3. [Google Scholar]
- [16].Dodge R, Daly A, Huyton J, et al. The challenge of defining wellbeing. Int J Wellbeing 2012;2:222–35. [Google Scholar]
- [17].Jeffrey K, Mahony S, Michaelson J, et al. Well-being at Work. A Review of the Literature. 2014;London, UK:NEF Consulting, 1–56. [Google Scholar]
- [18].Lahey BB. Public health significance of neuroticism. Am Psychol 2009;64:241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mazhindu DM, Griffiths L, Pook C, et al. The nurse match instrument: exploring professional nursing identity and professional nursing values for future nurse recruitment. Nurse Educ Pract 2016;18:36–45. [DOI] [PubMed] [Google Scholar]
- [20].Northouse PG. Leadership: Theory and Practice. London:Sage; 1997. [Google Scholar]
- [21].Gerstner CR, Day DV. Meta-analytic review of leader-member exchange theory: correlates and construct issues. J Appl Psychol 1997;82:827–44. [Google Scholar]
- [22].Stordeur S, D’hoore W, Vandenberghe C. Leadership, organizational stress, and emotional exhaustion among nursing hospital staff. J Adv Nurs 2001;35:533–42. [DOI] [PubMed] [Google Scholar]
- [23].Van der Heijden BIJM, Bakker AB. Towards a mediation model of employability enhancement: a study of employee-supervisor pairs in the building sector. Career Dev Q 2011;59:232–48. [Google Scholar]
- [24].Van der Heijden BIJM, Van Dam K, Hasselhorn HM. Intention to leave nursing: the importance of interpersonal work context, work-home interference, and job satisfaction beyond the effect of occupational commitment. Career Dev Int 2009;14:616–35. [Google Scholar]
- [25].Kristensen TS, Hannerz H, Høgh A, et al. The Copenhagen Psychosocial Questionnaire – a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 2005;31:438–49. [DOI] [PubMed] [Google Scholar]
- [26].Nelson K, Boudrias JS, Brunet L, et al. Authentic leadership and psychological well-being at work of nurses: the mediating role of work climate at the individual level of analysis. Burnout Res 2014;1:90–101. [Google Scholar]
- [27].Viswesvaran C, Sanchez JI, Fisher J. The role of social support in the process of work stress: a meta-analysis. J Vocational Behav 1999;54:314–34. [Google Scholar]
- [28].House J. Work Stress and Social Support. Boston, Reading, MA:Addison-Wesley; 1981. [Google Scholar]
- [29].Karsh B, Booske BC, Sainfort F. Job and organizational determinants of nursing home employee commitment, job satisfaction and intent to turnover. Ergonomics 2005;48:1260–81. [DOI] [PubMed] [Google Scholar]
- [30].Leicher V, Mulder RH. Team learning, team performance and safe team climate in elder care nursing. Team Perform Manage 2016;22:399–414. [Google Scholar]
- [31].Irvine DM, Evans MG. Job satisfaction and turnover among nurses: integrating research findings across studies. Nurs Res 1995;44:246–53. [PubMed] [Google Scholar]
- [32].Brunetto Y, Shriberg A, Farr-Wharton R, et al. The importance of supervisor–nurse relationships, teamwork, wellbeing, affective commitment and retention of North American nurses. J Nurs Manag 2013;2:827–37. [DOI] [PubMed] [Google Scholar]
- [33].Beehr TA, King LA, King DW. Social support and occupational stress: talking to supervisors. J Vocational Behav 1990;36:61–81. [Google Scholar]
- [34].Happell B, Dwyer T, Reid-Searl K, et al. Nurses and stress: recognizing causes and seeking solutions. J Nurs Manag 2013;21:638–47. [DOI] [PubMed] [Google Scholar]
- [35].Lee RT, Ashforth BE. A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol 1996;81:123–33. [DOI] [PubMed] [Google Scholar]
- [36].Akerboom S, Maes S. Beyond demand and control: the contribution of organizational risk factors in assessing the psychological well-being of health care employees. Work Stress 2006;20:21–36. [Google Scholar]
- [37].Avanzi L, Zaniboni S, Balducci C, et al. The relation between overcommitment and burnout: does it depend on employee job satisfaction? Anxiety Stress Coping 2014;27:455–65. [DOI] [PubMed] [Google Scholar]
- [38].Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol 1996;1:27. [DOI] [PubMed] [Google Scholar]
- [39].Siegrist J, Starke D, Chandola T. The measurement of effort–reward imbalance at work: European comparisons. Soc Sci Med 2004;58:1483–99. [DOI] [PubMed] [Google Scholar]
- [40].Joksimovic L, Starke D, vd Knesebeck O, et al. Perceived work stress, overcommitment, and self-reported musculoskeletal pain: across-sectional investigation. Int J Behav Med 2002;9:122–38. [DOI] [PubMed] [Google Scholar]
- [41].Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol 1989;44:513–24. [DOI] [PubMed] [Google Scholar]
- [42].Hobfoll SE. Folkman S. Conservation of resources theory: its implication for stress, health, and resilience. The Oxford Handbook of Stress, Health, and Coping. Oxford:Oxford University Press; 2011. 127–47. [Google Scholar]
- [43].Buelens M, Poelmans SA. Enriching the Spence and Robbins’ typology of workaholism: demographic, motivational and organizational correlates. J Organ Change Manage 2004;17:440–58. [Google Scholar]
- [44].Kristensen TS. A New Tool for Assessing Psychosocial Factors at Work: The Copenhagen Psychosocial Questionnaire. Copenhagen:National Institute of Health; 2000. [Google Scholar]
- [45].Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS Scales. J Pers Soc Psychol 1988;47:1063–70. [DOI] [PubMed] [Google Scholar]
- [46].Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. J Consult Clin Psychol 1983;5:730. [DOI] [PubMed] [Google Scholar]
- [47].Kline R. Principles and Practice of Structural Equation Modeling. 4th ed.London:The Guilford Press; 2015. [Google Scholar]
- [48].Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables: User's Guide. Los Angeles:Muthén & Muthén; 1998–2012. [Google Scholar]
- [49].Doty DH, Glick WH. Common methods bias: does common methods variance really bias results? Organ Res Methods 1998;1:374–406. [Google Scholar]
- [50].Van der Heijden B, De Vos A. Pachana NA. Sustainable employability and aging. Springer Science + Business Media, Encyclopedia of Geropsychology. Singapore:2015. [Google Scholar]


