Abstract
Oxidized phospholipids (OxPL) are abundant in atherosclerotic plaques. They are also bound to circulating plasminogen after myocardial infarction (MI), and their binding to plasminogen may accentuate fibrinolysis. We sought to assess whether circulating levels of plasminogen and OxPL bound to plasminogen (OxPL-PLG) increase following acute MI and whether this increase differs between atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI. We measured circulating levels of plasminogen and OxPL-PLG at 0, 6, 24, 48 h, and >3 months (stable state) following acute MI and following an angiogram for stable coronary artery disease (CAD). Forty-nine subjects met the criteria for acute MI, of whom 34 had clearly defined atherothrombotic (n = 22) or non-atherothrombotic (n = 12) MI; 15 patients met the criteria for stable CAD. Mean baseline levels of plasminogen and OxPL-PLG were lower in the acute MI group than in the stable CAD group (9.75 vs 20.2, p < 0.0001 for plasminogen and 165.5 vs 275.1, p = 0.0002 for OxPL-PLG) and did not change over time or between time points, including the 3-month follow-up. Mean baseline levels of plasminogen and OxPL-PLG were also lower in atherothrombotic (Type 1) than in non-atherothrombotic (Type 2) MI subjects (8.65 vs 12.1, p < 0.03 for plasminogen and 164.5 vs 245.7, p = 0.02 for OxPL-PLG), and this relationship did not change over time or between time points. Plasminogen and OxPL-PLG were lower in patients presenting with an acute MI than in those with stable CAD and also in those with atherothrombotic MI (Type 1) vs. those with non-atherothrombotic MI (Type 2). These findings persisted at a median follow-up of 3 months post-MI. The association of plasminogen and OxPL-PLG with acute MI, particularly atherothrombotic MI (Type 1), could reflect a reduced fibrinolytic capacity, associated with an increased risk of atherothrombotic events differentiating stable CAD from unstable CAD and atherothrombotic MI (Type 1) from non-atherothrombotic MI (Type 2). Additional study with a larger sample size is warranted.
Keywords: Atherothrombosis, Oxidized phospholipids, Plasminogen, Acute myocardial infarction, Biomarkers
Introduction
Acute myocardial infarction (MI) remains a leading cause of death worldwide [1]. It is diagnosed most often by the combination of an increase in the circulating levels of proteins (typically cardiac troponin) that leak from the necrotic myocardium, with at least one of the following: symptoms of ischemia, electrocardiographic changes consistent with ischemia, imaging evidence of new loss of viable myocardium, or the identification of an intracoronary thrombus by angiography or autopsy [2]. While circulating levels of cardiac proteins such as cardiac troponin are specific indicators of myocardial necrosis, the levels of these proteins often do not increase to diagnostic values for several hours after the start of an acute MI [3]. Therefore, current diagnostic criteria for acute MI often fail to identify patients before the induction of irreversible myocardial necrosis. Moreover, circulating levels of cardiac proteins report myocardial necrosis, which is the outcome of the triggering event, rather than the cause and therapeutic target itself (i.e., plaque disruption and ensuing atherothrombosis). Hence, these measurements cannot distinguish tissue necrosis caused by coronary atherothrombosis from other causes of necrosis such as demand ischemia or stress cardiomyopathy [4]. Although patients with atherothrombotic (Type 1) MI derive substantial benefit from current anticoagulant and antiplatelet therapies, many patients with non-atherothrombotic (Type 2) MI would be expected to experience only the bleeding risks, without the clinical benefits. Therefore, in patients presenting with symptoms suggestive of acute MI, the ability to identify an atherothrombotic MI prior to substantial myocardial necrosis (troponin release) and to quickly distinguish atherothrombotic from non-atherothrombotic MI would materially increase treatment safety and effectiveness for these patients.
Atherothrombotic MI is triggered by the disruption of plaques, followed by the formation of an occlusive thrombus. Therefore, the event ideally could be detected prior to irreversible myocardial necrosis, either by an increase in blood levels of plaque constituents or by systemic changes indicating atherothrombosis. Vulnerable plaques are lipid-rich lesions that contain large amounts of oxidized phospholipids (OxPL) [5–9]. Although most oxidized lipids remain sequestered within the vessel wall, small amounts of OxPL covalently bound to apolipoprotein B (apoB), lipoprotein(a) [10, 11], and plasminogen are also present in the circulation [12, 13]. Circulating levels of OxPL bound to apoB have been found to be positively associated with the presence and extent of angiographically documented coronary and peripheral arterial disease [14]. Furthermore, OxPL bound to apoB has been reported to increase in both plasma and distal protection devices after percutaneous coronary, carotid, and peripheral intervention and in the days to months following an acute MI [7, 10, 11, 14, 15].
Recently, Leibundgut et al. reported that, relative to healthy controls and subjects with stable coronary artery disease (CAD), OxPL bound to plasminogen (OxPL-PLG) increases in the days after an acute MI [13]. They also found that the presence of OxPL on plasminogen facilitates fibrinolysis in vitro, implicating OxPL-PLG in the pathophysiology of atherothrombotic, as opposed to non-atherothrombotic, acute MI [13]. Prior studies have shown that circulating levels of OxPL bound to apolipoprotein B-100, which reflect primarily the OxPL present on lipoprotein(a), rise acutely during acute MI and immediately following percutaneous coronary intervention in patients with stable CAD and during recanalization of chronic total occlusions [10, 11, 16, 17]. Nevertheless, it remains unclear whether acute atherothrombotic MI results in immediate release of OxPL and whether this release could be an early index of plaque rupture or thrombus formation that might be useful in distinguishing atherothrombotic from non-atherothrombotic acute MI. To assess this possibility, we prospectively measured the basal levels as well as the change in plasminogen and OxPL-PLG in subjects with acute MI and in those with stable CAD undergoing coronary angiography. In addition, we compared the levels and change in plasminogen and OxPL-PLG in subjects with an atherothrombotic (Type 1) MI and those with a non-atherothrombotic (Type 2) MI, categorized according to the novel and stringent criteria developed for this study.
Methods
Enrollment population
Following institutional review board approval, participants were recruited from two hospitals in Louisville, Kentucky, between March 2012 and August 2013 and followed prospectively. Subject of two types were sought for enrollment: those with suspected acute MI and those with suspected stable CAD. All participants provided written informed consent.
Enrollment criteria for both groups required that each patient be >18 years of age and scheduled for coronary angiography within 48 h. Subjects who received fibrinolysis were not eligible. Those enrolled in the suspected acute MI group must have reported ischemic symptoms lasting >10 min, within 24 h of enrollment, and had to meet at least one of the following four criteria: (1) new or presumably new ST-segment depression >0.1 mV; (2) elevated troponins or CK-MB levels within 24 h of enrollment; (3) ≥1 mm ST-segment elevation in ≥2 contiguous electrocardiogram (ECG) leads; or (4) ≥1 mm ST-segment depression in V1 and V2 (posterior wall infarct). Subjects considered for enrollment in the suspected stable CAD group were required to have presented for angiography as an elective procedure. Patients in the suspected stable CAD group were excluded on the basis of any one of the following criteria: (1) hospitalization for acute coronary syndrome (ACS) or clinical instability within 4 weeks prior to planned enrollment; (2) coronary artery bypass graft (CABG) surgery within 1 year prior to planned enrollment; (3) percutaneous coronary intervention (PCI) within 12 weeks prior to planned enrollment; (4) stroke within 12 weeks prior to planned enrollment; (5) presence of unstable angina or symptoms refractory to maximal medical therapy; (6) presence of significant co-morbidities likely to cause death within 2 years; or (7) significant active history of substance abuse within 5 years of enrollment. Subjects were asked to decline enrollment if they would not be able to return to the medical campus for a 3-month stable follow-up.
Enrolled subjects were given a written appointment with instructions on how to complete the study follow-up prior to leaving the hospital. They also received a reminder phone call from the study nurse or principal investigator approximately 1 week prior to the scheduled follow-up. Appointments were changed when necessary to accommodate the subjects’ schedules, and transportation was arranged if needed. Study follow-up appointments were scheduled to coincide with the subjects’ medical care appointments when possible and preferred by the subjects. Parking vouchers were given to all subjects who used paid parking.
History, physical exam, clinical laboratory, and ECG data
All subjects were evaluated by study personnel, and each subject’s history, physical examination results, clinical laboratory data, and ECG data were collected prior to measurement of plasminogen or OxPL-PLG. The subject’s medical records were used to aid in the collection of pertinent medical history. A single study physician (APD) read all ECGs in accordance with a priori study guidelines. Standard laboratory data (troponin, creatinine, blood cell, and platelet counts) were obtained from the treating hospital clinical laboratory at standardized study time points: at the time of the angiogram (T0) and 6 (T6), 24 (T24), and 48 (T48) hours post-angiogram (unless the subject was discharged from the hospital prior to this time point). Follow-up history, physical exam results, and laboratory data were collected at a single follow-up (TF/U) visit 3 to 12 (median, 3.27) months after the procedure or hospitalization for acute MI, when the subject was in a stable condition.
Biochemical analyses
The cohort was constructed to maximize the chance for discovering new biology related to acute MI; therefore, samples were collected at multiple time points, including a follow-up when the subject was in a stable state. Enrollment sample collection via an arterial sheath took place at the time of coronary angiography after a 5–10 mL waste draw. All available follow-up samples (T6, 24, 48 h, and >3 months) were collected from a peripheral vein, preferably a virgin vein, without a tourniquet (maximum pressure of <40 mmHg via blood pressure cuff), using a 21G needle, after >10 ml of clinical blood collection (waste draw), and into a tube containing ethylenediamine tetraacetic acid (EDTA). Sample processing time was rigorously standardized. Plasminogen and OxPL-PLG were measured by a blinded, independent laboratory (University of California, San Diego) as described previously [10]. In brief, to measure plasminogen levels, microtiter well plates (Dynex Technologies, Chantilly, Virginia) were incubated with a mouse monoclonal anti-human plasminogen antibody (Meridian Life Science, Saco, Maine) at 5 μg/ml overnight at 4 °C; the plates were than washed, and human plasma was added (1:32,000 dilution). Plasminogen was detected with biotinylated guinea pig anti-human plasminogen antibody in a chemiluminescence enzyme-linked immunosorbent assay (ELISA). OxPL-PLG was determined in a similar manner using biotinylated EO6 antibody, but at a plasma dilution of 1:400. The assay’s limit of quantification was 0.01-500 nanoMPC, with a coefficient of variance of 3.1–4.8 nanoMPC. This assay normalized all wells to the same amount of plasminogen and therefore measured OxPL independent of plasma plasminogen levels. All measurements were performed in triplicate.
Serum cardiac troponin I concentrations were measured by either of two independent CLIA-approved laboratories, the University of Louisville or KentuckyOne Jewish Hospital. The Ortho Vitros 5600 assay was used to measure cardiac troponin I in subjects receiving treatment at the University of Louisville Hospital. For this assay, the 99 % cut-off level for a healthy population was 0.035 ng/ml with a coefficient of variation (CV) <10 %. This assay further defined 0.12 ng/ml as the most efficient (more specific) cut-off point for the diagnosis of acute MI. The Beckman Access assay was used to measure cardiac troponin I in subjects receiving treatment at KentuckyOne Jewish Hospital. For this assay, the 99 % cut-off level for a healthy population was 0.04 ng/ml, but a CV < 10 % was not achieved until 0.06 ng/ml. This assay defined 0.5 ng/ml as the most efficient (more specific) cut-off point for the diagnosis of acute MI.
Coronary angiographic assessment
Angiograms were examined in a blinded fashion for all subjects by the Johns Hopkins Quantitative Angiographic Core Laboratory. The criteria for identifying and quantifying coronary thrombosis and atherosclerotic burden were jointly developed by the Core lab and the study team from existing published data [18–25].
Histological data
Coronary aspiration, with intent to retrieve the culprit coronary thrombosis, is standard of care in ST-segment elevation myocardial infarction (STEMI) patients. Aspiration attempt was left to the discretion of the subject’s treating interventional cardiologist. All samples from aspiration attempts were strained, immediately preserved in formalin, and sent to CVPath Institute, Inc., Gaithersburg, Maryland, for blinded histological evaluation by a pathologist specialized in the analysis of coronary thrombosis [26, 27].
Study cohort
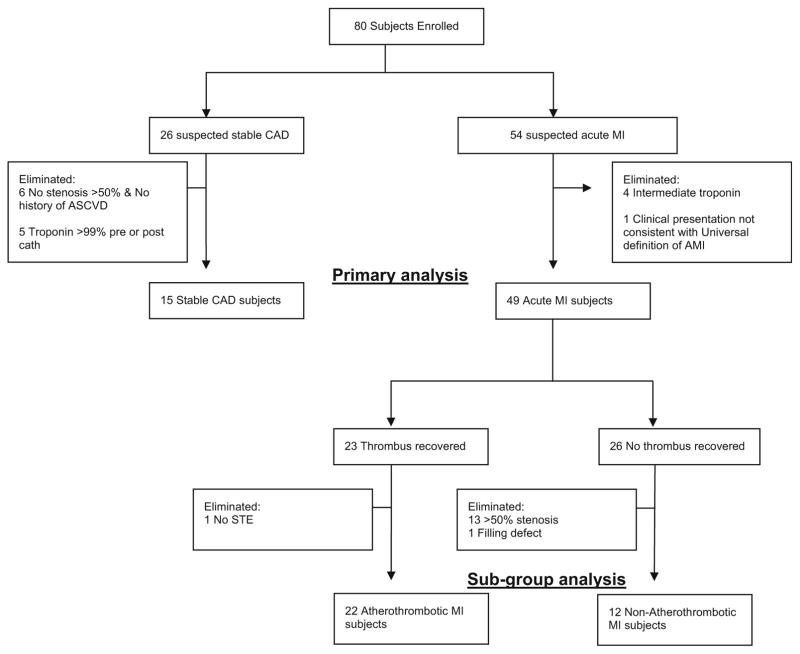
The following strict a priori criteria were used to define the study analysis groups: Acute MI was defined as a clinical event in a subject presenting to the cardiac catheterization laboratory for a non-elective procedure, with a cardiac troponin I greater than the most efficient diagnostic cut-off point as specified by the assay manufacturer (several-fold higher than the 99 percentile for a healthy population for both assays used in this study) and meeting Joint ESC/ACCF/AHA/WHF criteria [2] for an acute MI (Table 1). Patients with stable CAD were identified as those presenting for an elective cardiac catheterization with a past medical history of atherosclerosis, as evidenced by CABG, PCI, stroke/transient ischemic attack (TIA), carotid endarterectomy (CEA), peripheral artery bypass procedure, abdominal aortic aneurysm (AAA) repair, or >50 % stenosis in 1 or more coronary vessels on enrollment angiogram. Additional criteria included normal thrombolysis in myocardial infarction (TIMI) flow and myocardial perfusion grade (MPG) in all vessels as well as pre- and post-procedure cardiac troponin I <99 % for a healthy population specific to the assay used (Table 1). Subjects who did not meet either stable CAD or acute MI criteria were eliminated from the study in order to limit confounding from mis-classification and produce an ideal cohort for discovering new biochemical/clinical characteristics related to acute MI (Fig. 1).
Table 1.
Study phenotype criteria
| Study Phenotype | Criteria
|
|||
|---|---|---|---|---|
| Troponin (ng/ml) | Histology | Presentation | Blinded Angiographic Assessment |
|
| Stable CAD (n = 15) |
Ortho Vitros 5600 Assay: “Peak” Troponin Level < 0.035 Beckman Access “Peak” Troponin Level < 0.04 |
Elective coronary angiogram History of CVD: CABG, PCI, CVA/TIA, CEA, PAD or AAA procedure –or angiographic criteria |
Satisfies ALL criteria below:
|
|
| Acute MI (n = 49) |
Ortho Vitros 5600 Assay: “Peak” Troponin Level > 0.12 Beckman Access “Peak” Troponin Level > 0.5 |
Non-elective coronary angiogram Clinical presentation consistent with WHF/ECC/ACC/AHA Universal definition of AMI |
||
| Atherothrombotic MI (n = 22) |
Ortho Vitros 5600 Assay: “Peak” Troponin Level > 0.12 Beckman Access “Peak” Troponin Level > 0.5 -and- >30 % increase in troponin from T0 to T6 |
Histologically confirmed coronary thrombus 0–4 days old by blinded pathological assessment. | Non-elective coronary angiogram Clinical presentation consistent with WHF/ECC/ACC/AHA Universal definition of AMI |
Stenosis in the vessel which thrombus was recovered of 50–100 % -and- ST elevation in territory supplied by the vessel in which thrombus was recovered. |
| non- Atherothrombotic MI (n = 12) |
Ortho Vitros 5600 Assay: “Peak” Troponin Level > 0.12 Beckman Access “Peak” Troponin Level > 0.5 |
No histologically confirmed thrombus recovered. | Clinical presentation consistent with WHF/ECC/ACC/AHA Universal definition of AMI | Satisfies ALL 5 criteria below, in all vessels:
|
CAD coronary artery disease, MI myocardial infarction, TIMI thrombolysis in myocardial infarction, MPG myocardial perfusion grade, CABG coronary artery bypass grafting, PCI percutaneous coronary intervention, CVA cerebral vascular accident, TIA transient ischemic attack, CEA carotid endarterectomy, PAD peripheral artery disease, AAA abdominal aortic aneurysm
Fig. 1.
Enrollment and analysis cohorts
Acute MI was further stratified into atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI. Because no national guidelines exist for differentiating atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI, we developed novel conservative (stringent) criteria (Table 1) to eliminate borderline cases from our analysis and limit confounding from misclassification, with the goal of identifying biological characteristics related to acute atherothrombotic MI (Fig. 1). Our criteria expand upon those previously proposed by our group [28] and now include a combination of prospectively collected historical, physical, electrocardiographic, histological, biochemical, and angiographic (blinded core lab assessment) data that we believe are more robust than any other published criteria for distinguishing Type 1 and Type 2 MI [29–35]. The definition of atherothrombotic MI included the criteria for acute MI criteria as well as (1) the presence of a histologically confirmed (by blinded pathological assessment) coronary thrombus 0 to 4 days old, (2) a 50 to 100 % stenosis in the vessel in which thrombus was recovered, (3) ST elevation in the territory supplied by the vessel in which the thrombus was recovered, and (4) an elevated troponin and >30 % increase in troponin between T0 and T6 h (Table 1). Non-atherothrombotic MI was defined as meeting the criteria for acute MI, but with (a) no recovery of a histologically confirmed thrombus, and (b) satisfaction of all of the following five criteria in all vessels: <50 % stenosis, no filling defect, simple Ambrose lesion morphology, TIMI flow = 3, and TIMI myocardial perfusion grade (TIMI MPG) = 3 (Table 1).
Statistical analysis
Baseline subject characteristics were summarized by study group. For categorical characteristics, frequencies and percentages are reported, along with Fisher’s exact test p-values, to compare distributions by study group. For continuous characteristics, mean and standard deviation are reported, along with the appropriate statistical test for comparing the study groups. In addition to visual inspection of histograms, Shapiro–Wilk tests were conducted for continuous characteristics to determine whether any of the characteristics were not approximately normally distributed. P values derived from Student’s t test are reported for study group comparisons, unless the homogeneity of variances assumption was not met or the variable was not approximately normally distributed. In the first case, a Welch’s t test was conducted; in the second, a Wilcoxon rank-sum test was used.
Study outcomes were evaluated using repeated measures analysis of variance (ANOVA)—conducted separately for plasminogen and OxPL-PLG. The repeated measures ANOVA models included fixed effects for group, time point, and group × time point as well as a random effect for study subject. The inclusion of these fixed effects allowed for testing: (1) whether mean analyte levels differed by study group; (2) whether analyte levels differed across time points; and (3) whether time-course differed by study group. The P-values corresponding to Type III SS F-tests are reported for determining statistical significance. For the primary analysis comparing the acute MI and stable CAD study groups, T0, T6, and TF/U measurements were used. For the subgroup analysis comparing the atherothrombotic (Type 1) MI and non-atherothrombotic (Type 2) MI subgroups, T0, T6, T24, and TF/U measurements were used. The random effect for study subject assumed a compound symmetry covariance structure. Statistical power for both the primary and acute MI subgroup analyses was retrospectively calculated using the observed analyte means, variances, and group sizes [36].
To identify potential confounders in the repeated measures analysis, the relationships between the analytes and baseline cohort characteristics were examined. Values for signed r2, where r is the Pearson correlation coefficient, are presented to show the magnitude, direction, and significance of associations between a characteristic and an analyte at baseline. To determine whether plasminogen and OxPL-PLG were significantly collinear, despite OxPL measurements being made on a standardized amount of plasminogen, signed r2 for the two analytes was computed by time point.
Statistical analyses were conducted in SAS 9.4 (SAS Institute Inc., 2013); graphics were generated in base R version 3.0.2 (R Core Team, 2013). The manuscript is in compliance with the STROBE (& MOOSE) guidelines for observational studies.
Results
Eighty subjects were enrolled in this study. To limit misclassification, subjects with indeterminate diagnosis were eliminated from further analysis. A total of 49 patients met the criteria for an acute MI, of which a subset had clearly defined atherothrombotic (n = 22) MI or non-atherothrombotic MI (n = 12), and 15 patients met the criteria for stable CAD (Table 1; Fig. 1). Excluding any constrained differences resulting from the enrollment criteria, several risk factors differed significantly between individuals in the acute MI group and those with stable CAD. The prevalence of smoking and heart rate on presentation was higher among acute MI subjects, whereas body mass index (BMI) and prevalence of hyperlipidemia and diabetes were higher among the subjects with stable CAD (Table 2). Excluding constrained differences resulting from the enrollment criteria, the time from presentation to angiogram, the peak troponin, and the baseline glucose values differed between individuals in the atherothrombotic MI group and those in the non-atherothrombotic MI group (Table 3).
Table 2.
Baseline subject characteristics for primary analysis
| Variable | Acute MI Group (N = 49) | Stable CAD Group (N = 15) | p value |
|---|---|---|---|
| Age (mean ± SD) years | 58.6 ± 14.4 | 61.3 ± 8.9 | 0.49 |
| Males (%) | 65.3 | 53.3 | 0.54 |
| Caucasian race (%) | 77.6 | 93.3 | 0.09 |
| Current smoker (%) | 53.1 | 20.0 | 0.04 |
| Currently consumes alcohol (%) | 32.7 | 46.7 | 0.37 |
| History of dyslipidemia (%) | 46.9 | 86.7 | 0.01 |
| History of diabetes mellitus (%) | 10.2 | 40.0 | 0.03 |
| History of hypertension (%) | 61.2 | 93.3 | 0.06 |
| History of atherosclerosis (%) (MI, CAD, PCI, CABG) | 38.8 | 100.0 | < 0.0001 |
| History of congestive heart failure (%) | 8.2 | 6.7 | 1.00 |
| History of chronic renal failure (%) | 8.2 | 0.0 | 0.28 |
| History of stroke (%) | 10.2 | 0.0 | 0.33 |
| HR at time of presentation (mean ± SD) | 85 | 66 | < 0.0001 |
| MAP at time of presentation (mean ± SD) | 102.8 ± 24.7 | 91.4 ± 14.3 | 0.09 |
| BMI at time of presentation (mean ± SD) | 27.5 ± 7.24 | 33 ± 7.08 | 0.02 |
| Time (h) elapsed presentation to angiogram (median ± IQR, range) | 3.5 ± 16.0, 36 | 2.0 ± 1.0, 3 | 0.21b |
| Baseline troponin (mean ± SD, range) mg/dL | 5.59 ± 10.83, 55.3 | 0.009 ± 0.003, 0.01 | < 0.0001b |
| Peak troponin (mean ± SD, range) | 33.5 ± 37.9, 150.3 | 0.008 ± 0.004, 0.01 | < 0.0001b |
| Glucose at baseline (mean ± SD, range) | 142.1 ± 56.5, 285 | 131.6 ± 30.6, 107 | 0.35a |
| Creatinine at baseline (mean ± SD, range) | 1.13 ± 0.79, 4.34 | 0.92 ± 0.17, 0.66 | 0.10a |
| ST elevation on EKG at baseline | 63.3 | 0.0 | < 0.0001 |
| At least one vessel with ≥50 % coronary stenosis on enrollment angiogram | 73.5 | 40.0 | 0.03 |
| Aspirin use at time of enrollment (%) | 89.8 | 86.7 | 0.66 |
| P2Y12 Inhibitors use at enrollment (%) | 53.1 | 50.0 | 0.77 |
MI myocardial infarction, CAD coronary artery disease, PCI percutaneous coronary intervention, CABG coronary artery bypass grafting, HR heart rate, SBP systolic blood pressure, DBP diastolic blood pressure, MAP mean arterial pressure, BMI body mass index, ACE-I angiotensin converting enzyme inhibitor
Welch’s t-test
Wilcoxon rank-sum test
Table 3.
Baseline subject characteristics for acute MI subgroup analysis
| Variable | Type 1 MI (N = 22) | Type 2 MI (N = 12) | p value |
|---|---|---|---|
| Age (mean ± SD) years | 58.7 ± 15.1 | 56.3 ± 16.6 | 0.67 |
| Males (%) | 72.7 | 41.7 | 0.14 |
| Caucasian race (%) | 86.4 | 66.7 | 0.21 |
| Current smoker (%) | 45.5 | 50.0 | 1.00 |
| Currently consumes alcohol (%) | 36.4 | 33.3 | 0.78 |
| History of dyslipidemia (%) | 54.5 | 33.3 | 0.30 |
| History of diabetes mellitus (%) | 9.1 | 0.0 | 0.53 |
| History of hypertension (%) | 45.5 | 75.0 | 0.19 |
| History of atherosclerosis (%) (MI, CAD, PCI, CABG) | 40.9 | 33.3 | 0.73 |
| History of congestive heart failure (%) | 0.0 | 8.3 | 0.35 |
| History of chronic renal failure (%) | 4.5 | 8.3 | 0.43 |
| History of stroke (%) | 4.5 | 25.0 | 0.12 |
| HR at time of presentation (mean ± SD) | 87.4 ± 27.2 | 88.3 ± 27.5 | 0.93 |
| MAP at time of presentation (mean ± SD) | 104.1 ± 19.8 | 95.4 ± 26.9 | 0.29 |
| BMI at time of presentation (mean ± SD) | 27.5 ± 7.4 | 27.8 ± 6.7 | 0.90 |
| Time (hours) elapsed presentation to angiogram (median ± IQR, range) | 1.0 ± 1.0, 13.0 | 18.0 ± 9.5, 30.0 | < 0.0001b |
| Baseline Troponin (mean ± SD, range) mg/dL | 7.8 ± 14.9, 55.3 | 2.4 ± 2.9, 9.8 | 0.76b |
| Peak troponin (mean ± SD, range) | 51.6 ± 41.2, 145.7 | 11.6 ± 22.0, 68.2 | 0.0002b |
| Glucose at baseline (mean ± SD, range) | 166.5 ± 58.9, 246 | 118.0 ± 47.7, 182 | 0.01a |
| Creatinine at baseline (mean ± SD, range) | 0.98 ± 0.43, 2.38 | 1.21 ± 1.07, 3.80 | 0.50a |
| ST Elevation on EKG at baseline | 100.0 | 25.0 | < 0.0001 |
| At least one vessel with ≥50 % coronary stenosis on enrollment angiogram | 100.0 | 0.0 | < 0.0001 |
| Aspirin use at time of enrollment (%) | 86.4 | 91.7 | 1.00 |
| P2Y12 Inhibitors use at enrollment (%) | 45.5 | 50.0 | 1.00 |
MI myocardial infarction, CAD coronary artery disease, PCI percutaneous coronary intervention, CABG coronary artery bypass grafting, HR heart rate, SBP systolic blood pressure, DBP diastolic blood pressure, MAP mean arterial pressure, BMI body mass index, ACE-I angiotensin converting enzyme inhibitor
Welch’s t-test
Wilcoxon rank-sum test
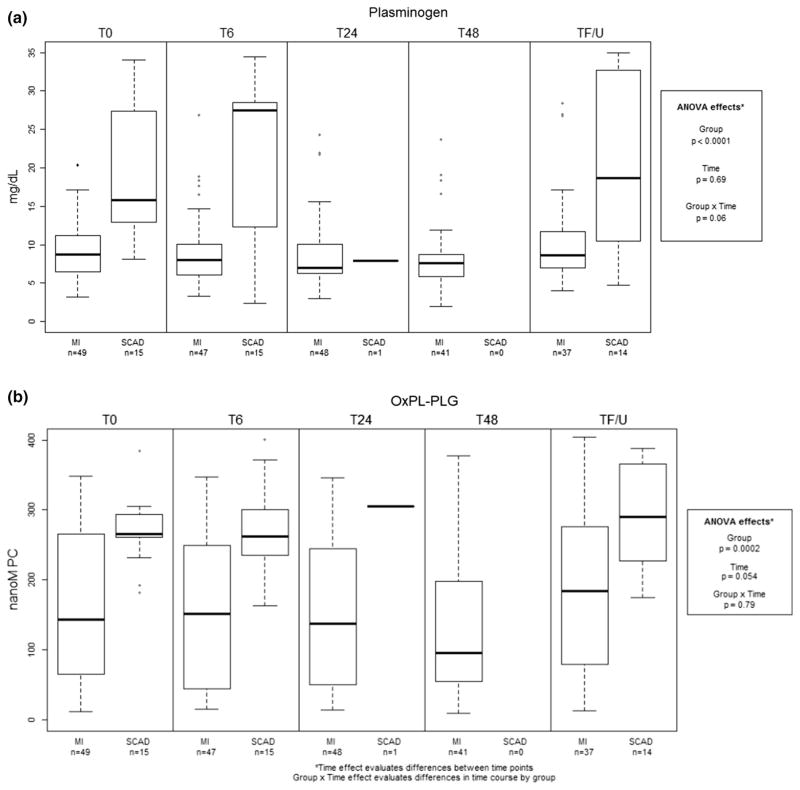
For our primary analysis, estimated mean plasminogen was significantly lower in MI subjects (9.75 mg/dL; 95 % CI 8.1–11.4) than in stable CAD subjects (20.2 mg/dL; 95 % CI 17.3–23.2) (p < 0.0001; Fig. 2). The plasminogen level did not change significantly between time T0, T6, and T/FU for either the acute MI or stable CAD subjects (p = 0.69); furthermore, the delta in plasminogen levels between the acute MI and stable CAD patients was not significantly different at T0, T6, and T/FU (p = 0.06). The estimated mean OxPL-PLG was significantly lower in MI subjects (165.5 nanoMPC; 95 % CI 138.3–192.75) than in stable CAD subjects (275.1 nanoMPC; 95 %CI 226.1–324.1) (p <0.0002; Fig. 2). OxPL-PLG levels did not change significantly between time T0, T6, and T/FU for either the acute MI or stable CAD subjects (p = 0.054); furthermore, the delta in OxPL-PLG between the two groups was unchanged at T0, T6, and T/FU (p = 0.79). Using a repeated measures ANOVA, we had>90 % power to detect a difference in plasminogen and OxPL-PLG over time in acute MI and stable CAD subjects.
Fig. 2.
Plasminogen (a) and OxPL-PLG (b) levels in acute MI and stable CAD groups at all study time points
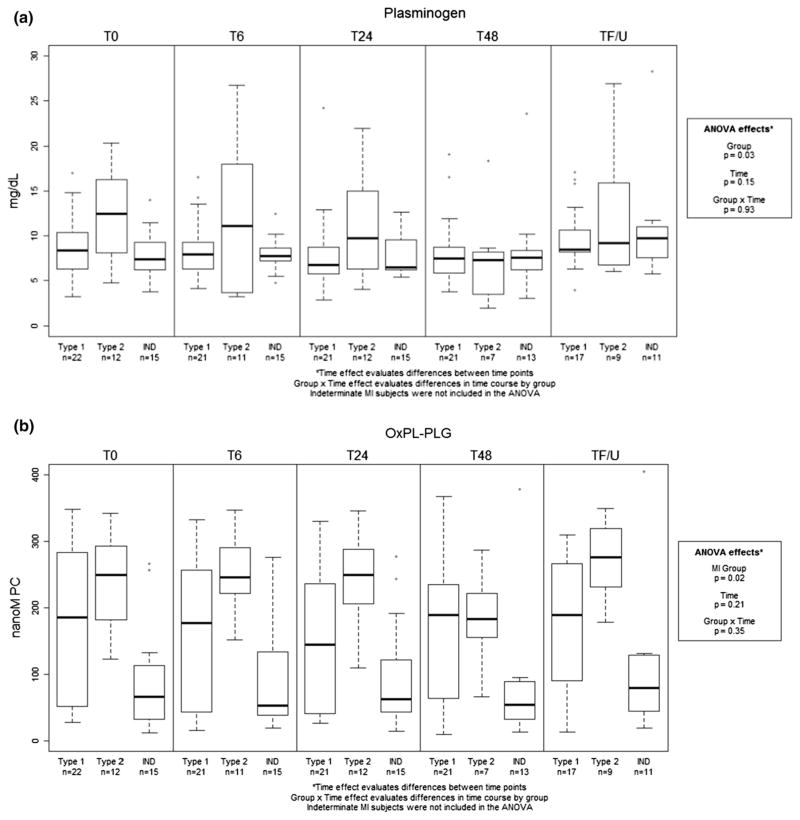
In our subgroup analysis, the estimated mean plasminogen was significantly lower in atherothrombotic (Type 1) subjects (8.65 mg/dL; 95 % CI 6.8–10.5) than in non-atherothrombotic (Type 2) subjects (12.1 mg/dL; 95 % CI 9.5–14.6) (p = 0.03; Fig. 3). Plasminogen levels did not change significantly between times T0, T6, T24, and T/FU for either the atherothrombotic or non-atherothrombotic subjects (p = 0.15); furthermore, the delta in plasminogen between atherothrombotic and non-atherothrombotic subjects was consistent at all time points measured (p = 0.93). The estimated mean OxPL-PLG was significantly lower in atherothrombotic subjects (164.5 nanoMPC; 95 % CI 124.65–204.4) than in the non-atherothrombotic subjects (245.7 nanoMPC; 95 %CI 191.7–299.8) (p = 0.02). The OxPL-PLG level did not change significantly between times T0, T6, T24, and T/FU for either group of subjects (p = 0.21); furthermore, the delta in OxPL-PLG between atherothrombotic and non-atherothrombotic subjects was unchanged at the time points measured (p = 0.35). Using a repeated measures ANOVA, we had >90 % power to detect a difference in plasminogen and OxPL-PLG over time in atherothrombotic (Type 1) and non-atherothrombotic (Type 2) subjects.
Fig. 3.
Plasminogen (a) and OxPL-PLG (b) levels in atherothrombotic MI (Type 1) and non-atherothrombotic MI (Type 2) sub-groups at all study time points
The levels of both plasminogen and OxPL-PLG at baseline were positively associated with heart rate and with whether percutaneous coronary intervention (PCI) was performed (Table 4). Moreover, a significant gender effect was observed in baseline OxPL-PLG levels (p = 0.04). Interestingly, while the measurement of OxPL-PLG represented the levels of OxPL on microtiter well plates normalized for similar concentrations of plasminogen and was therefore independent of plasma plasminogen levels, plasma plasminogen levels explained 21 % to 26 % of the variance of OxPL-PLG at each time point (Table 5).
Table 4.
Association between plasminogen and OxPL-PLG and cohort characteristics
| Baseline oxPL bound to plasminogen signed r2 | p value | Baseline plasminogen signed r2 | p value | |
|---|---|---|---|---|
| SBP | −0.001 | 0.83 | −0.002 | 0.70 |
| DBP | −0.017 | 0.31 | −0.018 | 0.29 |
| MAP | −0.008 | 0.48 | −0.011 | 0.42 |
| Heart rate | −0.061 | 0.05 | −0.068 | 0.04 |
| Respiratory rate | 0.000 | 0.96 | −0.006 | 0.54 |
| Height | −0.039 | 0.12 | −0.038 | 0.12 |
| Weight | 0.020 | 0.26 | 0.018 | 0.29 |
| BMI | 0.051 | 0.07 | 0.056 | 0.06 |
| Gender | 0.067 | 0.04 | 0.033 | 0.15 |
| Race* | 0.000 | 0.93 | 0.002 | 0.71 |
| Diabetes† | 0.020 | 0.26 | 0.020 | 0.06 |
| Dyslipidemia† | 0.006 | 0.64 | 0.033 | 0.15 |
| Smoking‡ | 0.241 | 0.24 | 0.000 | 0.98 |
| Age | 0.000 | 0.94 | 0.000 | 0.93 |
| Presentation time§ to T0 | −0.009 | 0.47 | −0.012 | 0.39 |
| Symptom onset time to T0 | 0.028 | 0.26 | 0.001 | 0.80 |
| Baseline glucose | −0.020 | 0.27 | −0.034 | 0.14 |
| Baseline platelets | 0.005 | 0.59 | 0.038 | 0.12 |
| Baseline creatinine | −0.030 | 0.17 | −0.008 | 0.47 |
| PCI | 0.060 | 0.05 | 0.145 | 0.002 |
Bolded text indicates significant at p < 0.05
Pearson correlation coefficients: ANOVA F test statistic, SBP systolic blood pressure, DBP diastolic blood pressure, MAP mean arterial pressure, BMI body mass index
White vs. non-white
Yes/Borderline vs. No/Unknown
Current vs. Never/Former
Time between first hospital contact for symptoms leading to angiogram and T0 blood collection
Table 5.
Association between plasminogen and OxPL-PLG measured by Pearson correlation coefficient
| OxPL-PLG T0 | OxPL-PLG T6 | OxPL-PLG T24 | OxPL-PLG T48 | OxPL-PLG T F/U | |
|---|---|---|---|---|---|
| Plasminogen T0 | 0.48 | 0.45 | 0.37 | 0.21 | 0.36 |
| Plasminogen T6 | 0.48 | 0.49 | 0.44 | 0.28 | 0.42 |
| Plasminogen T24 | 0.42 | 0.41 | 0.51 | 0.27 | 0.45 |
| Plasminogen T48 | 0.37 | 0.19 | 0.39 | 0.50 | 0.39 |
| Plasminogen T F/U | 0.48 | 0.48 | 0.33 | 0.28 | 0.51 |
Bolded text indicates significant at p < 0.05
OxPL-PLG oxidized phospholipid bound to plasminogen, T time, F/U follow up (>3 months)
Discussion
The results of this study show that subjects presenting with acute MI have lower levels of plasminogen and OxPL-PLG than do subjects with stable CAD. The levels of both analytes were consistently lower for 48 h following acute MI and at a median follow-up of 3.2 months post-MI (stable state). This persistent difference may be related to differences in the thrombotic state that differentiate stable CAD from unstable CAD and could be reflective of an increased risk for developing acute MI in CAD patients. Consistent with this notion, our subgroup analysis showed that the levels of OxPL-PLG were consistently lower in atherothrombotic MI (Type 1) than in subjects with non-atherothrombotic MI (Type 2), both at 48 h following acute MI and also at a median follow-up of 3.2 months post-MI. No significant change in OxPL-PLG from baseline levels was observed in any study group within the first 48 h or at more than 3 months following an acute MI.
Measurement of OxPL-PLG in our study confirmed previous observations [13] that OxPL are bound to plasminogen and that, in addition to apoB and Lp(a), plasminogen represents a significant carrier of circulating phospholipids. Moreover, at each time point examined, we found that there were statistically significant correlations between the abundance of OxPL-PLG and plasminogen levels. This observation suggests that in patients with acute MI or stable CAD, the availability of OxPL is not limiting and, furthermore, that there may be a stoichiometric relationship between the extent of OxPL bound to PLG and the abundance of plasminogen. Therefore, additional research is warranted to evaluate the relationship of total OxPL-PLG burden to acute MI, specifically atherothrombotic MI (Type 1). Leibundgut et al. have reported that covalent modification of plasminogen by OxPL facilitates clot lysis [13]. Our novel finding that OxPL-PLG is lower in atherothrombotic MI (Type 1) than in non-atherothrombotic MI (Type 2) further supports the hypothesis that OxPL-PLG plays a clinically relevant role in clot lysis; however, further study is required to understand the mechanism of this increase in clot lysis time and how it contributes to the in vivo resolution of thrombi.
The consistently lower levels of plasminogen that we observed in patients with acute MI, as compared to those with stable CAD, were reflected in an earlier study by Lei-bundgut et al [13]. and suggest that acute MI is accompanied by a decrease in fibrinolytic activity. Our study is, to our knowledge, the first to demonstrate lower plasma levels of plasminogen in atherothrombotic MI (Type 1) versus non-atherothrombotic MI (Type 2). This finding may reflect a reduced fibrinolytic activity in atherothrombotic MI (Type 1) when compared to non-atherothrombotic MI (Type 2). We also found that several risk factors such as diabetes and smoking were higher in MI than in stable CAD patients; however, it is unlikely that lower levels of plasminogen in MI patients could be attributed to these differences, because diabetes has little effect on plasma plasminogen levels [37], and smoking is associated with an increase, rather than a decrease, in plasminogen [38]. Thus, the lower levels of plasminogen and OxPL-PLG in Type 1 MI patients may be related to reduced fibrinolytic capacity and an increased risk of an atherothrombotic event, which differentiates stable CAD from unstable CAD. As such, measurement of plasma levels of plasminogen and OxPL-PLG may allow for the identification of stable CAD patients who are highly susceptible to major adverse cardiovascular events [39], and these analytes may serve as a therapeutic target for reducing atherothrombotic risk.
Our observation that baseline plasma levels of plasminogen and OxPL-PLG are lower in individuals with acute MI than in those with stable CAD, although also consistent with some published work [13], is at odds with other studies. Hoffmeister et al. found no difference in plasminogen levels in 42 subjects initially admitted to the ICU with acute coronary syndrome and 25 subjects with stable CAD [40]. This study was limited by the fact that 31 of the 42 acute coronary syndrome subjects were creatinine kinase normal unstable angina patients [40]. A case–control study found that subjects presenting with an acute MI had higher plasminogen than their age-matched controls presenting for an orthopedic surgery [41]. This effect, however, was deemed non-significant after controlling for measures (C-reactive protein) or causes of inflammation (smoking) [41].
The fact that the decrease in both plasminogen and OxPL-PLG in patients with MI was sustained for >3 months in our study is in contrast with the work of Leibundgut et al., who found no difference in either analyte at 4 or 7 months post-acute MI when compared to subjects with stable CAD [13]. Prospective cohort and case–control studies have demonstrated both positive correlation and no correlation of plasminogen, tPA, or PAI-1 with incident CAD and MI [41–46]. Also, in the studies that found a positive correlation, the associations were not consistently independent of other cardiovascular risk factors [41, 43, 45, 46]. The relationship between OxPL-PLG and risk of future acute MI is less well studied. Our findings, if confirmed in larger clinical trials, may indicate that lowered levels of plasminogen and OxPL-PLG are risk factors for acute MI in subjects with clinically stable CAD. Such a finding would be consistent with the role of plasminogen and OxPL in facilitating the resolution of arterial thrombus [13]. Future studies powered for cardiovascular events can help clarify whether OxPL-PLG levels can actually predict future outcomes in acute MI.
Leibundgut et al. [13], reported that both plasminogen and OxPL on plasminogen rise rapidly in the first month after MI and then decline toward baseline. However, we found no evidence of an increase in the levels of plasminogen or OxPL-PLG after acute MI or acute atherothrombotic MI (Type 1). Potential explanations for the disparate results between the two studies include differences in the timing of sample collection and in cohort characteristics. In their study, Leibundgut et al. collected samples on enrollment, at the time of hospital discharge (approximately 4 days), and 30, 120, and 210 days after enrollment [13]. In contrast, our study was designed to evaluate changes that occur very early after acute MI; therefore, it is possible that we failed to measure an increase in OxPL-PLG that occurs >48 h post-MI but diminishes thereafter in the following months (prior to our average follow-up measure at 3.3 months). A delayed elevation of plasminogen has been demonstrated in subjects with unstable angina [47]. If that is the case, the delay in elevation occurs after thrombus formation has been incited and after treatment decisions have been made for an acute MI. Therefore, the utility of such a delayed elevation as a single diagnostic test will be limited, given the lack of change peri-MI and the level of overlap in plasminogen and OxPL-PLG ranges in acute MI, stable CAD, atherothrombotic MI, and non-atherothrombotic MI, despite the differences in mean value. However, our findings indicate that further research is warranted to evaluate the utility of these analytes, in combination with other factors, for the early diagnosis of acute MI and for distinguishing atherothrombotic and non-atherothrombotic MI.
Misclassification of subjects into study groups (acute MI versus stable CAD) could have been a source of bias or variability in the results between our studies and those of other investigators. Our methodology for the classification of subjects into study groups was designed to create “ideal” circumstances for identifying new biological characteristics related to acute MI. Toward this end, we required subjects to meet very conservative criteria for membership in either the acute MI or the stable CAD study group and eliminated borderline cases from our analysis (Table 1; Fig. 1). We also further evaluated atherothrombotic MI (Type 1) versus non-atherothrombotic MI (Type 2), given the biology of plasminogen and its potential relationship to atherothrombotic but not non-atherothrombotic MI. Again, we defined very conservative criteria for membership into the atherothrombotic or non-atherothrombotic subgroups and eliminated borderline cases in order to limit bias from misclassification (Table 1; Fig. 1). Other published criteria for the classification of atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI rely almost exclusively on physicians’ retrospective review of clinical data alone, with only one study evaluating coronary angiography in all subjects classified as non-atherothrombotic MI [29, 30, 32–35]. Our criteria for the classification of atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI expand upon criteria we previously introduced [28], to now include prospective collection of historical, electrocardiographic, biochemical, angiographic (blinded core lab evaluation) and histological data. We believe these criteria are superior to all other criteria proposed to date and will serve to facilitate further research on atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI.
Previous studies have shown that serum plasminogen levels are significantly influenced by age, gender, body mass index, physical activity, cholesterol, smoking, alcohol use, inflammation, and serum triglycerides [41, 48–50]. In our study, we found an association between OxPL-PLG levels, gender, heart rate, and PCI. The influence of multiple factors other than acute MI on plasminogen and OxPL-PLG levels may explain the disparate results between studies. A notable difference between our study and that of Leibundgut et al. [13] is the composition of the acute MI subjects in the cohort of each study. The cohort in our study included 49 subjects (65 % males) meeting a priori criteria for acute MI, whereas MI subjects in the cohort of Leibundgut et al. comprised only 8 subjects (all males).
Limitations
In the acute phase of this study, our measures of plasminogen and OxPL-PLG did not extend beyond 48 h, limiting our ability to directly compare our data to prior research demonstrating an increase in these analytes at a mean of 4 days post-MI. However, the present study was designed to identify very early biological events associated with acute MI; therefore, a delayed elevation of these analytes would make attribution to the precipitating pathophysiology of acute MI unlikely. While ours is the largest study of OxPL-PLG in subjects with acute MI to date, the sample size is still limited, particularly in the exploratory subgroup analyses. Examination of our findings in a larger cohort is warranted. Finally, this study does not have long-term follow-up data on cardiovascular events and is therefore unable to evaluate these analytes as predictors of events in stable CAD and post-MI patients.
Conclusion
In summary, we report here a sustained suppression of both plasminogen and OxPL-PLG in patients with acute MI versus stable CAD and atherothrombotic MI (Type 1) versus non-atherothrombotic MI (Type 2). This finding may be related to the underlying pathobiology that differentiates stable CAD from unstable CAD and atherothrombotic MI (Type 1) from non-atherothrombotic MI (Type 2), indicating that lowered plasminogen and OxPL-PLG may be a risk factor for acute atherothrombotic MI (type 1) in patients with clinically stable CAD. This finding warrants further exploration in larger outcome studies. Because we found that the levels of both plasminogen and OxPL-PLG were modestly, but significantly, correlated, the usefulness of OxPL-PLG as an independent diagnostic or prognostic test also needs to be evaluated in larger studies. Finally, we have introduced novel criteria for defining atherothrombotic (Type 1) and non-atherothrombotic (Type 2) MI.
Acknowledgments
We would like to thank all of the subjects who generously consented to participate in this study. We also appreciate the University of Louisville Diabetes and Obesity Center, the University of Louisville and the KentuckyOne Jewish Hospitals, CVPath Institute, Inc., Gaithersburg, Maryland, and the Johns Hopkins Quantitative Angiographic Core Laboratory. This work was supported in part by a grant from the American Heart Association (11CRP7300003) and the National Institute of General Medical Sciences (GM103492). Dr. Rai was supported by Wendell Cherry Chair in Clinical Trial Research and generous support from Dr. DM Miller, Director James Graham Brown Cancer Center. We thank Dr. Deborah MClellan for editorial assistance.
Grant support American Heart Association (11CRP7300003) and National Institute of General Medical Sciences (GM103492).
Abbreviations
- AAA
Abdominal aortic aneurysm
- ACS
Acute coronary syndrome
- ApoB
Apolipoprotein B
- BP
Blood pressure
- CABG
Coronary artery bypass graft
- CAD
Coronary artery disease
- CEA
Carotid endarterectomy
- CVD
Cardiovascular disease
- EDTA
Ethylenediamine tetraacetic acid
- ELISA
Enzyme-linked immunosorbent assay
- ECG
Electrocardiogram
- LBBB
Left bundle branch block
- MI
Myocardial infarction
- MPG
Myocardial perfusion grade
- OxPL
Oxidized phospholipids
- OxPL-PLG
Oxidized phospholipids bound to plasminogen
- PAI-1
Plasminogen activator inhibitor-1
- PCI
Percutaneous coronary intervention
- PLG
Plasminogen
- STEMI
ST-segment elevation myocardial infarction
- TIA
Transient ischemic attack
- TIMl
Thrombolysis in myocardial infarction
- tPA
Tissue plasminogen activator
Footnotes
Disclosures Sample measurements were made in the laboratory of Dr. Sotirios Tsimikas, University of California, San Diego, La Jolla, California. Coronary aspiration material was evaluated at CVPath Institute, Inc., Gaithersburg, Maryland. Coronary angiography was evaluated at the Johns Hopkins Quantitative Angiographic Core Laboratory, Baltimore, Maryland. Dr. Tsimikas is named as co-inventor and receives royalties from patents owned by the University of California, San Diego, on oxidation-specific antibodies. No author has any relationships with industry pertinent to this work.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics C, Stroke Statistics S. Executive summary: heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 2.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Biomarker S, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Subcommittee ECG, Chaitman BR, Clemmensen PM, Johanson P, Hod H, Imaging S, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJ, Classification S, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Intervention S, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Document R, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR Joint ESCAAHAWHFTFfUDoMI, Authors/Task Force Members C, Guidelines ESCCfP, Trials Registries S, Trials Registries S, Trials Registries S, Trials Registries S. Third universal definition of myocardial infarction. J Am College Cardiol. 2012;60(16):1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [Google Scholar]
- 3.Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, Bickel C, Baldus S, Warnholtz A, Frohlich M, Sinning CR, Eleftheriadis MS, Wild PS, Schnabel RB, Lubos E, Jachmann N, Genth-Zotz S, Post F, Nicaud V, Tiret L, Lackner KJ, Munzel TF, Blankenberg S. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. New Engl J Med. 2009;361(9):868–877. doi: 10.1056/NEJMoa0903515. [DOI] [PubMed] [Google Scholar]
- 4.Newby LK, Jesse RL, Babb JD, Christenson RH, De Fer TM, Diamond GA, Fesmire FM, Geraci SA, Gersh BJ, Larsen GC, Kaul S, McKay CR, Philippides GJ, Weintraub WS. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2012;60(23):2427–2463. doi: 10.1016/j.jacc.2012.08.969. [DOI] [PubMed] [Google Scholar]
- 5.Choi SH, Yin H, Ravandi A, Armando A, Dumlao D, Kim J, Almazan F, Taylor AM, McNamara CA, Tsimikas S, Dennis EA, Witztum JL, Miller YI. Polyoxygenated cholesterol ester hydroperoxide activates TLR4 and SYK dependent signaling in macrophages. PLoS One. 2013;8(12):e83145. doi: 10.1371/journal.pone.0083145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Itabe H, Takeshima E, Iwasaki H, Kimura J, Yoshida Y, Imanaka T, Takano T. A monoclonal antibody against oxidized lipoprotein recognizes foam cells in atherosclerotic lesions. Complex formation of oxidized phosphatidylcholines and polypeptides. J Biol Chem. 1994;269(21):15274–15279. [PubMed] [Google Scholar]
- 7.Ravandi A, Leibundgut G, Hung MY, Patel M, Hutchins PM, Murphy RC, Prasad A, Mahmud E, Miller YI, Dennis EA, Witztum JL, Tsimikas S. Release and capture of bioactive oxidized phospholipids and oxidized cholesteryl esters during percutaneous coronary and peripheral arterial interventions in humans. J Am Coll Cardiol. 2014;63(19):1961–1971. doi: 10.1016/j.jacc.2014.01.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsimikas S, Duff GW, Berger PB, Rogus J, Huttner K, Clopton P, Brilakis E, Kornman KS, Witztum JL. Pro-inflammatory interleukin-1 genotypes potentiate the risk of coronary artery disease and cardiovascular events mediated by oxidized phospholipids and lipoprotein(a) J Am Coll Cardiol. 2014;63(17):1724–1734. doi: 10.1016/j.jacc.2013.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Dijk RA, Kolodgie F, Ravandi A, Leibundgut G, Hu PP, Prasad A, Mahmud E, Dennis E, Curtiss LK, Witztum JL, Wasserman BA, Otsuka F, Virmani R, Tsimikas S. Differential expression of oxidation-specific epitopes and apolipoprotein(a) in progressing and ruptured human coronary and carotid atherosclerotic lesions. J Lipid Res. 2012;53(12):2773–2790. doi: 10.1194/jlr.P030890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsimikas S, Bergmark C, Beyer RW, Patel R, Pattison J, Miller E, Juliano J, Witztum JL. Temporal increases in plasma markers of oxidized low-density lipoprotein strongly reflect the presence of acute coronary syndromes. J Am Coll Cardiol. 2003;41(3):360–370. doi: 10.1016/s0735-1097(02)02769-9. [DOI] [PubMed] [Google Scholar]
- 11.Tsimikas S, Lau HK, Han KR, Shortal B, Miller ER, Segev A, Curtiss LK, Witztum JL, Strauss BH. Percutaneous coronary intervention results in acute increases in oxidized phospholipids and lipoprotein(a): short-term and long-term immunologic responses to oxidized low-density lipoprotein. Circulation. 2004;109(25):3164–3170. doi: 10.1161/01.CIR.0000130844.01174.55. [DOI] [PubMed] [Google Scholar]
- 12.Edelstein C, Pfaffinger D, Yang M, Hill JS. Scanu AM (2010) Naturally occurring human plasminogen, like genetically related apolipoprotein(a), contains oxidized phosphatidylcholine adducts. Biochim Biophys Acta. 1801;7:738–745. doi: 10.1016/j.bbalip.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leibundgut G, Arai K, Orsoni A, Yin H, Scipione C, Miller ER, Koschinsky ML, Chapman MJ, Witztum JL, Tsimikas S. Oxidized phospholipids are present on plasminogen, affect fibrinolysis, and increase following acute myocardial infarction. J Am Coll Cardiol. 2012;59(16):1426–1437. doi: 10.1016/j.jacc.2011.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsimikas S, Kiechl S, Willeit J, Mayr M, Miller ER, Kronenberg F, Xu Q, Bergmark C, Weger S, Oberhollenzer F, Witztum JL. Oxidized phospholipids predict the presence and progression of carotid and femoral atherosclerosis and symptomatic cardiovascular disease: five-year prospective results from the Bruneck study. J Am Coll Cardiol. 2006;47(11):2219–2228. doi: 10.1016/j.jacc.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Bertoia ML, Pai JK, Lee JH, Taleb A, Joosten MM, Mittleman MA, Yang X, Witztum JL, Rimm EB, Tsimikas S, Mukamal KJ. Oxidation-specific biomarkers and risk of peripheral artery disease. J Am Coll Cardiol. 2013;61(21):2169–2179. doi: 10.1016/j.jacc.2013.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fefer P, Tsimikas S, Segev A, Sparkes J, Otsuka F, Kolodgie F, Virmani R, Juliano J, Charron T, Strauss BH. The role of oxidized phospholipids, lipoprotein (a) and biomarkers of oxidized lipoproteins in chronically occluded coronary arteries in sudden cardiac death and following successful percutaneous revascularization. Cardiovasc Revasc Med. 2012;13(1):11–19. doi: 10.1016/j.carrev.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Tsimikas S, Witztum JL, Miller ER, Sasiela WJ, Szarek M, Olsson AG, Schwartz GG Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering Study I. High-dose atorvastatin reduces total plasma levels of oxidized phospholipids and immune complexes present on apolipoprotein B-100 in patients with acute coronary syndromes in the MIRACL trial. Circulation. 2004;110(11):1406–1412. doi: 10.1161/01.CIR.0000141728.23033.B5. [DOI] [PubMed] [Google Scholar]
- 18.Ambrose JA, Almeida OD, Sharma SK, Dangas G, Ratner DE. Angiographic evolution of intracoronary thrombus and dissection following percutaneous transluminal coronary angioplasty (the Thrombolysis and Angioplasty in Unstable Angina [TAUSA] trial) Am J Cardiol. 1997;79(5):559–563. doi: 10.1016/s0002-9149(96)00815-6. [DOI] [PubMed] [Google Scholar]
- 19.Ambrose JA, Almeida OD, Sharma SK, Torre SR, Marmur JD, Israel DH, Ratner DE, Weiss MB, Hjemdahl-Monsen CE, Myler RK, et al. Adjunctive thrombolytic therapy during angioplasty for ischemic rest angina. Results of the TAUSA Trial. TAUSA Investigators. Thrombolysis and Angioplasty in Unstable Angina trial. Circulation. 1994;90(1):69–77. doi: 10.1161/01.cir.90.1.69. [DOI] [PubMed] [Google Scholar]
- 20.Ambrose JA, Israel DH. Angiography in unstable angina. Am J Cardiol. 1991;68(7):78B–84B. doi: 10.1016/0002-9149(91)90388-2. [DOI] [PubMed] [Google Scholar]
- 21.Capone G, Wolf NM, Meyer B, Meister SG. Frequency of intracoronary filling defects by angiography in angina pectoris at rest. Am J Cardiol. 1985;56(7):403–406. doi: 10.1016/0002-9149(85)90875-6. [DOI] [PubMed] [Google Scholar]
- 22.Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E, Group TS. Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation. 2002;105(16):1909–1913. doi: 10.1161/01.cir.0000014683.52177.b5. [DOI] [PubMed] [Google Scholar]
- 23.Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van De Werf F, Braunwald E. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000;101(2):125–130. doi: 10.1161/01.cir.101.2.125. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW. Multiple complex coronary plaques in patients with acute myocardial infarction. New Engl J Med. 2000;343(13):915–922. doi: 10.1056/NEJM200009283431303. [DOI] [PubMed] [Google Scholar]
- 25.Zack PM, Ischinger T, Aker UT, Dincer B, Kennedy HL. The occurrence of angiographically detected intracoronary thrombus in patients with unstable angina pectoris. Am Heart J. 1984;108(6):1408–1412. doi: 10.1016/0002-8703(84)90684-7. [DOI] [PubMed] [Google Scholar]
- 26.Kramer MC, Rittersma SZ, de Winter RJ, Ladich ER, Fowler DR, Liang YH, Kutys R, Carter-Monroe N, Kolodgie FD, van der Wal AC, Virmani R. Relationship of thrombus healing to underlying plaque morphology in sudden coronary death. J Am Coll Cardiol. 2010;55(2):122–132. doi: 10.1016/j.jacc.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 27.Kramer MC, van der Wal AC, Koch KT, Ploegmakers JP, van der Schaaf RJ, Henriques JP, Baan J, Jr, Rittersma SZ, Vis MM, Piek JJ, Tijssen JG, de Winter RJ. Presence of older thrombus is an independent predictor of long-term mortality in patients with ST-elevation myocardial infarction treated with thrombus aspiration during primary percutaneous coronary intervention. Circulation. 2008;118(18):1810–1816. doi: 10.1161/CIRCULATIONAHA.108.780734. [DOI] [PubMed] [Google Scholar]
- 28.DeFilippis AP, Oloyede OS, Andrikopoulou E, Saenger AK, Palachuvattil JM, Fasoro YA, Guallar E, Blumenthal RS, Kickler TS, Jaffe AS, Gerstenblith G, Schulman SP, Rade JJ. Thromboxane A(2) generation, in the absence of platelet COX-1 activity, in patients with and without atherothrombotic myocardial infarction. Circul J. 2013;77(11):2786–2792. doi: 10.1253/circj.cj-12-1421. [DOI] [PubMed] [Google Scholar]
- 29.Ambrose JA, Loures-Vale A, Javed U, Buhari CF, Aftab W. Angiographic correlates in type 1 and 2 MI by the universal definition. JACC Cardiovasc Imaging. 2012;5(4):463–464. doi: 10.1016/j.jcmg.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 30.Javed U, Aftab W, Ambrose JA, Wessel RJ, Mouanoutoua M, Huang G, Barua RS, Weilert M, Sy F, Thatai D. Frequency of elevated troponin I and diagnosis of acute myocardial infarction. Am J Cardiol. 2009;104(1):9–13. doi: 10.1016/j.amjcard.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Melberg T, Burman R, Dickstein K. The impact of the 2007 ESC-ACC-AHA-WHF Universal definition on the incidence and classification of acute myocardial infarction: a retrospective cohort study. Int J Cardiol. 2010;139(3):228–233. doi: 10.1016/j.ijcard.2008.10.021. [DOI] [PubMed] [Google Scholar]
- 32.Morrow DA, Wiviott SD, White HD, Nicolau JC, Bramucci E, Murphy SA, Bonaca MP, Ruff CT, Scirica BM, McCabe CH, Antman EM, Braunwald E. Effect of the novel thienopyridine prasugrel compared with clopidogrel on spontaneous and procedural myocardial infarction in the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction 38: an application of the classification system from the universal definition of myocardial infarction. Circulation. 2009;119(21):2758–2764. doi: 10.1161/CIRCULATIONAHA.108.833665. [DOI] [PubMed] [Google Scholar]
- 33.Saaby L, Poulsen TS, Diederichsen AC, Hosbond S, Larsen TB, Schmidt H, Gerke O, Hallas J, Thygesen K, Mickley H. Mortality rate in type 2 myocardial infarction: observations from an unselected hospital cohort. Am J Med. 2014;127(4):295–302. doi: 10.1016/j.amjmed.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 34.Saaby L, Poulsen TS, Hosbond S, Larsen TB, Pyndt Diederichsen AC, Hallas J, Thygesen K, Mickley H. Classification of myocardial infarction: frequency and features of type 2 myocardial infarction. Am J Med. 2013;126(9):789–797. doi: 10.1016/j.amjmed.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 35.Stein GY, Herscovici G, Korenfeld R, Matetzky S, Gottlieb S, Alon D, Gevrielov-Yusim N, Iakobishvili Z, Fuchs S. Type-II myocardial infarction–patient characteristics, management and outcomes. PLoS One. 2014;9(1):e84285. doi: 10.1371/journal.pone.0084285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muller KE, Lavange LM, Ramey SL, Ramey CT. Power calculations for general linear multivariate models including repeated measures applications. J Am Stat Assoc. 1992;87(420):1209–1226. doi: 10.1080/01621459.1992.10476281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Konieczynska M, Fil K, Bazanek M, Undas A. Prolonged duration of type 2 diabetes is associated with increased thrombin generation, prothrombotic fibrin clot phenotype and impaired fibrinolysis. Thromb Haemost. 2014;111(4):685–693. doi: 10.1160/TH13-07-0566. [DOI] [PubMed] [Google Scholar]
- 38.Allen RA, Kluft C, Brommer EJ. Effect of chronic smoking on fibrinolysis. Arteriosclerosis. 1985;5(5):443–450. doi: 10.1161/01.atv.5.5.443. [DOI] [PubMed] [Google Scholar]
- 39.Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, Badimon JJ, Stefanadis C, Moreno P, Pasterkamp G, Fayad Z, Stone PH, Waxman S, Raggi P, Madjid M, Zarrabi A, Burke A, Yuan C, Fitzgerald PJ, Siscovick DS, de Korte CL, Aikawa M, Juhani Airaksinen KE, Assmann G, Becker CR, Chesebro JH, Farb A, Galis ZS, Jackson C, Jang IK, Koenig W, Lodder RA, March K, Demirovic J, Navab M, Priori SG, Rekhter MD, Bahr R, Grundy SM, Mehran R, Colombo A, Boerwinkle E, Ballantyne C, Insull W, Jr, Schwartz RS, Vogel R, Serruys PW, Hansson GK, Faxon DP, Kaul S, Drexler H, Greenland P, Muller JE, Virmani R, Ridker PM, Zipes DP, Shah PK, Willerson JT. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part I. Circulation. 2003;108(14):1664–1672. doi: 10.1161/01.CIR.0000087480.94275.97. [DOI] [PubMed] [Google Scholar]
- 40.Hoffmeister HM, Jur M, Ruf-Lehmann M, Helber U, Heller W, Seipel L. Endothelial tissue-type plasminogen activator release in coronary heart disease: Transient reduction in endothelial fibrinolytic reserve in patients with unstable angina pectoris or acute myocardial infarction. J Am Coll Cardiol. 1998;31(3):547–551. doi: 10.1016/s0735-1097(97)00531-7. [DOI] [PubMed] [Google Scholar]
- 41.Meltzer ME, Doggen CJ, de Groot PG, Rosendaal FR, Lisman T. Plasma levels of fibrinolytic proteins and the risk of myocardial infarction in men. Blood. 2010;116(4):529–536. doi: 10.1182/blood-2010-01-263103. [DOI] [PubMed] [Google Scholar]
- 42.Folsom AR, Aleksic N, Park E, Salomaa V, Juneja H, Wu KK. Prospective study of fibrinolytic factors and incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Arterioscler Thromb Vasc Biol. 2001;21(4):611–617. doi: 10.1161/01.atv.21.4.611. [DOI] [PubMed] [Google Scholar]
- 43.Hoffmeister A, Rothenbacher D, Khuseyinova N, Brenner H, Koenig W. Plasminogen levels and risk of coronary artery disease. Am J Cardiol. 2002;90(10):1168–1170. doi: 10.1016/s0002-9149(02)02792-3. [DOI] [PubMed] [Google Scholar]
- 44.Ridker PM, Vaughan DE, Stampfer MJ, Manson JE, Hennekens CH. Endogenous tissue-type plasminogen activator and risk of myocardial infarction. Lancet. 1993;341(8854):1165–1168. doi: 10.1016/0140-6736(93)90998-v. [DOI] [PubMed] [Google Scholar]
- 45.Salomaa V, Rasi V, Kulathinal S, Vahtera E, Jauhiainen M, Ehnholm C, Pekkanen J. Hemostatic factors as predictors of coronary events and total mortality: The FINRISK ‘92 Hemostasis Study. Arterioscler Thromb Vasc Biol. 2002;22(2):353–358. doi: 10.1161/hq0202.104078. [DOI] [PubMed] [Google Scholar]
- 46.Yamagishi K, Aleksic N, Hannan PJ, Folsom AR, Inverstigators AS. Coagulation factors II, V, IX, X, XI, and XII, plasminogen, and alpha-2 antiplasmin and risk of coronary heart disease. J Atheroscler Thromb. 2010;17(4):402–409. doi: 10.5551/jat.3673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffmeister HM, Jur M, Wendel HP, Heller W, Seipel L. Alterations of coagulation and fibrinolytic and kallikrein-kinin systems in the acute and postacute phases in patients with unstable angina pectoris. Circulation. 1995;91(10):2520–2527. doi: 10.1161/01.cir.91.10.2520. [DOI] [PubMed] [Google Scholar]
- 48.Jenkins GR, Seiffert D, Parmer RJ, Miles LA. Regulation of plasminogen gene expression by interleukin-6. Blood. 1997;89(7):2394–2403. [PubMed] [Google Scholar]
- 49.Kida M, Wakabayashi S, Ichinose A. Expression and induction by IL-6 of the normal and variant genes for human plasminogen. Biochem Biophys Res Commun. 1997;230(1):129–132. doi: 10.1006/bbrc.1996.5909. [DOI] [PubMed] [Google Scholar]
- 50.Kostka T, Para J, Kostka B. Cardiovascular diseases (CVD) risk factors, physical activity (PA) and plasma plasminogen (Plg) in a random sample of community-dwelling elderly. Arch Gerontol Geriatr. 2009;48(3):300–305. doi: 10.1016/j.archger.2008.02.011. [DOI] [PubMed] [Google Scholar]