Abstract
The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) Section III Alternative Model for Personality Disorders (AMPD; APA, 2013) represents an innovative system for simultaneous psychiatric classification and psychological assessment of personality disorders (PD). The AMPD combines major paradigms of personality assessment and provides an original, heuristic, flexible, and practical framework that enriches clinical thinking and practice. Origins, emerging research, and clinical application of the AMPD for diagnosis and psychological assessment are reviewed. The AMPD integrates assessment and research traditions, facilitates case conceptualization, is easy to learn and use, and assists in providing patient feedback. New as well as existing tests and psychometric methods may be used to operationalize the AMPD for clinical assessments.
Keywords: DSM-5, personality disorders, Alternative Model, personality assessment, Level of Personality Functioning Scale, personality traits, PID-5
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Section III Alternative Model for Personality Disorders (AMPD) provides an empirically based, pantheoretical approach to psychological assessment for the purposes of diagnosing personality disorders (PDs) and assessing personality-related problems in living. Severity and style of personality dysfunction are evaluated conjointly through ratings for overall level of personality impairment and specific pathological personality traits. These ratings generate hybrid categorical-dimensional PD diagnoses in addition to dimensional indices of personality psychopathology. Psychological evaluation conducted through the lens of the AMPD generates both psychiatric diagnosis and a psychometric profile of clinical data that can serve as a relatively comprehensive personality assessment.
The AMPD joins two conceptual planes of personality pathology. The first plane covers disturbances in self and interpersonal functioning. The second involves dimensions of maladaptive personality traits assessed through 5 broad trait domains that are partitioned into 25 narrower trait facets. A key feature of the AMPD is that these two conceptual planes are derived from major traditions in psychological assessment as well as decades of empirical research (Bender, Morey, & Skodol, 2011; Krueger & Markon, 2014). This heritage confers scientific and practical advantages. The continuity with clinical assessment traditions facilitates ease of learning and application (Morey, Skodol, & Oldham, 2014).
Importantly, the AMPD accommodates clinicians of varying backgrounds much in the same way that the psychotherapy integration movement bridges theoretical orientations. By virtue of its grounding in established practices of clinical assessment and empirical study, the AMPD rests on and benefits from the pre-existing foundations of clinical assessment, and possesses an intrinsic evidence base. The concepts and variables in the AMPD will be generally familiar to any psychologist with training in personality assessment, making the system relatively easy to use and measurable via validated assessment methods.
The goals of this paper are to introduce the AMPD to practitioners, highlight its roots in established paradigms of personality assessment, briefly review clinical utility and validity evidence, and demonstrate application via a case example. This review of the AMPD emphasizes two themes: its paradigmatic pluralism and kinship to established methods of psychological testing. Table 1 lists key features of the AMPD.
Table 1.
Highlights of the AMPD
|
Development, Description, and Conceptual-Empirical Origins
Zachar, Krueger, and Kendler (2015) provide a fascinating “oral history” of the genesis of the AMPD compiled from interviews with many of the participants involved in revising PD diagnosis for the DSM-5. The reader is referred to this article for details, but, briefly, the process of revision traces to Kupfer, First, and Reiger (2002) in A Research Agenda for DSM-V.1 Eleven conferences took place over several years in which concepts, research, and proposals were reviewed. The Personality and Personality Disorder Work Group examined complex and competing issues and proposals such as prototype versus dimensional diagnosis and the evidential value of clinical experience versus empirical data. The Work Group concluded a hybrid approach to PD diagnosis (Krueger, Skodol, Livesley, Shrout, & Huang, 2007) could enhance acceptance by striking a balance between introducing dimensional elements, which have substantial empirical support, while preserving continuity with extant DSM categories with demonstrated clinical traction. For example, in the DSM-5, Antisocial PD, a categorical concept, can be viewed as dysfunctional behavior related to a combination of dimensions including manipulativeness, callousness, deceitfulness, hostility, risk taking, impulsivity, and irresponsibility.
The AMPD was approved by the DSM-5 Task Force, but the Board of Trustees of the American Psychiatric Association (APA) retained the traditional categorical approach (essentially the DSM-IV PDs) in Section II. Zachar et al. (2015. p. 8) state “as an ‘official’ alternative, the hybrid model is a recognized competitor to the traditional categorical model.” Declared by the APA as an Alternative Model, the AMPD legitimately complements the DSM-5 Section II PD diagnoses and has practical relevance for clinicians. Indeed, the DSM-5 allows for formal coding of the AMPD through use of the DSM-5 code “Other Specified Personality Disorder (301.89).2
Diagnosis with the AMPD requires fulfilling 7 general criteria for PD (DSM-5, p. 761). Most innovative are the first two criteria, Criterion A (level of personality functioning) and Criterion B (maladaptive personality traits). Criterion A involves assessment of disturbance in self functioning (identity and self-direction) and Interpersonal functioning (empathy and intimacy). Criterion B involves assessment of pathological personality traits which are organized into 5 broad trait domains composed of 25 specific trait facets. Criteria C through G cover issues of pervasiveness, stability, early emergence, discrimination from other mental disorders, effects of substances, and developmental stage or sociocultural environment. Table 2 depicts a schematic of Criterion A and B; the reader is referred to Tables S1 and S2 in the online supplemental material for detailed descriptive tables reprinted with permission from the DSM-5.
Table 2.
Schematic of DSM-5 AMPD Criterion A & Criterion B.
| AMPD Criterion A: | |||
|---|---|---|---|
| Level of Personality Functioning Scale (LPFS) | |||
| Self | Interpersonal | ||
| (1) Identity | (2) Self-Direction | (1) Empathy | (2) Intimacy |
| AMPD Criterion B: |
|---|
| PD Trait Domains (broad) and Facets (narrow) |
| Negative Affectivity: Emotional Lability; Anxiousness; Separation Insecurity; Submissiveness; Hostility; Perseveration; Depressivity; Suspiciousness; Restricted Affectivity |
| Detachment: Withdrawal; Intimacy Avoidance; Anhedonia; Depressivity; Restricted Affectivity; Suspiciousness |
| Antagonism: Manipulativenss; Deceitfulness; Grandiosity; Attention Seeking; Callousness; Hostility |
| Disinhibition: Irresponsibility; Impulsivity; Distractibility; Risk Taking Rigid Perfectionism |
| Psychoticism: Unusual Beliefs and Experiences; Eccentricity; Cognitive and Perceptual Dysregulation |
Note: Moderate impairment is required for diagnosis of Criterion A, defined as ≥ 2 or more component ratings of ≥ 2 on a 0–4 point scale. Criterion B consists of 5 Trait Domains (bolded) and 25 Trait Facets. Domains may be rated globally or Facets may be rated individually on a 0–3 scale. Overlap of Facets on more than one Domain occurs because psychopathological personality dimensions do not show simple structure (see Krueger & Markon, 2014). Definitions and further detail on these constructs are available in the online supplemental material and in the DSM-5, Section III.
The AMPD permits diagnosis of six specific PD categories through algorithms for combining ratings of maladaptive traits and specific forms of dysfunction. These are Antisocial, Avoidant, Borderline, Narcissistic, Obsessive-Compulsive, and Schizotypal PD (these six PDs were chosen for inclusion on the bases of empirical support and clinical relevance, and their diagnostic algorithms were calibrated with known prevalence rates of the PDs). Maladaptive personality patterns not covered by these algorithms (which also include PD syndromes such as paranoid, schizoid, histrionic, dependent, and self-defeating) are diagnosed as PD-Trait Specified (PD-TS). In a PD-TS diagnosis, the specific clinically significant traits are stated in lieu of an over-arching category (e.g., PD-TS with suspiciousness, restricted affectivity, and hostility may diagnose “paranoid PD”). This aims to correct the problem of the ambiguous and ubiquitous “PD NOS” diagnosis (Verheul, 2005) by providing a scheme for characterizing the numerous patients who do not fit well into available PD categories. In a related manner, significant traits can be included with categorical diagnoses when indicated, conveniently providing the clinician with information about patient personalities that is not captured by the specific PD category.
Paradigms of Personality Assessment within the AMPD
The AMPD is not necessarily “new” to professional psychologists with a background in psychological assessment because it integrates several historically prominent clinical approaches to personality. To make this point, we refer to Wiggins’ (2003) articulation of five “paradigms” in personality assessment that differ in foci, scope, academic lineage, and preferred tests. The psychodynamic paradigm focuses on internal conflict and mental models (e.g. inner schema, representations) and often makes use of performance-based tests such as the Rorschach or TAT. The personological paradigm represents the classic case history approach and often uses narrative, life story data. The interpersonal paradigm focuses on dynamic social relations, and uses interpersonal circumplex based measures for assessment. The multivariate paradigm is methodologically oriented to factor-analytic models, as instantiated in the Five Factor Model (FFM) instruments. Exemplar instruments of the inductive empirical paradigm in clinical settings include the Minnesota Multiphasic Personality Inventory (MMPI) and its various revisions. Through a collaborative assessment of one individual by prominent representatives of each paradigm, Wiggins (2003) shows how these five assessment paradigms overlap significantly and generate similar conclusions, but also contribute unique and nuanced insights.
The psychodynamic, interpersonal, and personological paradigms of Wiggins (2003) are embedded within Criterion A. These paradigms manifest in the focus on self and other boundaries, dynamics of self-esteem regulation, and emphasis on mode of interpersonal relatedness (Hopwood, Wright, Ansell, & Pincus, 2013). Criterion B prominently reflects the Wiggins (2003) multivariate, empirical, and interpersonal paradigms. For example, the 5 broad, higher-order trait domains and the more narrow 25 trait facets of Criterion B parallel FFMs that derive from quantitative models of normal and abnormal personality data (Krueger & Markon, 2014). Benefitting from the cumulative wisdom of each of these great paradigms of personality assessment, the AMPD is at once both traditional and innovative.3
Criterion A: Level of Personality Functioning and Paradigms of Personality Assessment
Pincus (2005, p. 287) noted, “classification of personality disorders in the post DSM-III/IV era will require greater coordination of definitional theories and systems for describing variation in expression of personality pathology.” From this perspective, the AMPD Criterion A may be regarded as assessing the genus of personality pathology; it defines what PDs have in common that distinguishes them from healthy personality and other forms of psychopathology (Pincus, 2011). Criterion A, operationalized in the DSM-5 Levels of Personality Functioning Scale (LPFS; Bender et al., 2011), defines PD across two broad areas of personality dysfunction. The core components of PD are intrapersonal (self) and interpersonal (other) functioning. These domains span the constructs of identity and self-directedness, and empathy and intimacy, respectively. The LPFS, whose criteria are listed in detail in the DSM-5, orders manifestations of these constructs across level of impairment, thus defining the severity of PD for an individual patient (see Table 2).
Criterion A incorporates important structural elements, developmental processes, and personality dynamics of concern in contemporary psychodynamic, attachment, interpersonal, and social-cognitive theories of personality and psychopathology. Bender et al. (2011) describe in detail the conceptual elements and specific assessment approaches of the LPFS. The LPFS incorporates familiar clinical constructs such as self-esteem stability, perception of self and others, interpersonal boundaries, identity, interpersonal mutuality, mentalization, reflective functioning, and developmental level of personality organization. For example, Otto Kernberg’s (2012) concept of “psycho-structural level” shows parallels with the LPFS of the AMPD. The two overarching dimensions of the LPFS, self and other, parallel the personality constructs of agency and communion within the interpersonal paradigm (Pincus & Hopwood, 2012; Hopwood et al., 2013). The personological paradigm stakes its claim to key aspects of the LPFS in the narrative and subjective data which manifest in psychological identity (Schmeck, Schluter-Muller, Foelsch, & Doering, 2013) and self-esteem regulation (Ronningstam, 2014).
Criterion B: Maladaptive Traits and Paradigms of Personality Assessment
Following Pincus (2011), specific maladaptive personality tendencies of Criterion B may be regarded as the “species” of PD. Particular varieties of PD are profiled through the assessment of maladaptive personality trait dimensions. It should be noted that the term “personality trait” has specific meaning in the realm of human personality. Personality traits differ from many human traits, such as height, that are highly heritable and difficult to modify on an individual basis. In contrast to many physical traits, personality traits reflect similar levels of both genetic and environmental influences, and their expressions are sensitive to environmental contexts (South & DeYoung, 2013). Thus, a maladaptive personality “trait” refers to a tendency that is relatively stable across time and place, but also is amenable to change (Fleeson & Jayawickreme, 2015).
Criterion B assesses maladaptive personality traits derived mainly from the multivariate and empirical paradigms, particularly as exemplified by the Five Factor personality models (e.g., Thomas et al., 2013) and the Personality Psychopathology Five (PSY-5) scales of the MMPI (Harkness, Reynolds, & Lilienfeld, 2014). Table 2 lists the 5 trait domains and 25 trait facets of the AMPD. Facets are specific dimensional elements of personality variation subsumed by 5 broad trait domains: Negative Affectivity, Detachment, Antagonism, Disinhibition, and Psychoticism. These labels emphasize the maladaptive extremes of these traits, but they also map relatively specifically onto domains from the normative FFM tradition (e.g., Gore & Widiger, 2013; Wright & Simms, 2015).4 At the domain level, Negative Affectivity relates to neuroticism, Detachment to introversion, Antagonism to disagreeableness, Disinhibition to low conscientiousness, and Psychoticism to openness.
The DSM-5 personality traits may be assessed with the Personality Inventory for DSM-5 (PID-5; Krueger et al., 2012), which has both self-report and informant report versions, as well as clinician ratings (in which interview, history, and other psychometric data may be used). There is also a brief form of the PID-5, which permits the assessment of domains but not facets. Reviews of empirical research (e.g., Widiger, 2015) conclude the AMPD Criterion B can be reliably measured with the PID-5 which shows strong convergent validity with various well-validated measures.
Utility and Acceptability
Many investigators have noted problems with traditional categorical personality diagnosis such as extensive comorbidity, preponderance of PD-NOS diagnoses, limited convergent validity, heterogeneity within categories, arbitrary diagnostic thresholds, lack of treatment implications, reliance on expert consensus rather than empirical data to develop the nosology, and the questionable assumption that discontinuous categories reflect the nature of PD (Widiger & Trull, 2007). A major goal of the AMPD was to redress such fundamental problems. Bernstein, Iscan, and Maser (2007) found that an appreciable majority (74%) of PD experts surveyed thought that the DSM-IV categorical approach to PDs should be replaced. Furthermore, 87% of respondents believed that personality pathology was dimensional in nature, and 70% indicated that a mixed categorical-dimensional approach to PD diagnosis was the most desirable alternative to DSM-IV.
Nevertheless, some feared that clinical utility would suffer from a dimensional representation of personality problems. For example, Shedler et al. (2010) commented “the proposed system for classifying personality disorders is too complicated, includes a trait-based approach to diagnosis without an adequate clinical rationale, and omits personality syndromes that have significant clinical utility.” (p. 1026). Similarly, Clarkin and Huprich (2011) were concerned that the AMPD “does not often meet criteria for clinical relevance.” (p. 202).5 However, Verheul (2005) pointed out that actually few studies support the relative clinical utility of the categorical model. Those that have been conducted typically compared the DSM approach to the FFM, whose instruments often do not include behaviors at the maladaptive extremes of trait dimensions, resulting in mixed outcomes with some studies supporting the DSM approach and others favoring the FFM. Summarizing, Mullins-Sweatt and Lengel (2012) noted the critical importance of evaluating diagnostic systems with comparable methods of assessment. When comparable methodologies are used, the FFM (dimensional approach) demonstrates equivalent or better clinical utility than the DSM categorical model. This questions the claim that a dimensional approach would reduce perceived acceptability or clinical utility. It also should be noted that the increased dimensionalization within the DSM-5 harmonizes with the NIMH Research Doman Criteria (RDoC) (Cuthbert & Insel, 2013), an explicitly dimensional trans-diagnostic (albeit more neurobiological) model, connecting the AMPD with other contemporary frameworks in psychiatric classification.
Morey, Bender, and Skodol (2013) tested this issue directly by surveying 337 mental health clinicians (26% psychiatrists, 63% psychologists, and 11% other professional disciplines) who evaluated one of their patients for PD features listed in DSM-IV and in the AMPD of DSM-5. After applying each diagnostic model, clinicians evaluated the clinical utility of that model with respect to communication with patients and with other professionals, comprehensiveness, descriptiveness, ease of use, and utility for treatment planning. These perceptions were compared across DSM-IV and the three components of the AMPD as well as between psychiatrists and non-psychiatrists. The DSM-5 dimensional trait model was seen as more useful than the DSM-IV model in 5 of 6 comparisons (all but ease of use)—a perception shared by psychiatrists as well as other professionals (Morey et al., 2014).
The AMPD innovatively organizes terminology, concepts, and techniques inherent in traditional paradigms of assessment already familiar to many professionals, and this likely will facilitate learning and applying the model. Given that clinicians in these recent studies were almost entirely unfamiliar with the AMPD at the time the studies were conducted, these findings strongly suggest, in contrast to concerns around poor acceptance and loss of clinical utility, the use of the AMPD may significantly increase the acceptance and perceived clinical utility of DSM PD diagnosis. Indeed, user acceptance and comfort should increase as training guides and materials are developed (Zachar & First, 2014) and clinical examples are made available (Bach, Markon, Simonsen, & Krueger, 2015).
Validity
The AMPD has produced a relatively large body of initial research. Both the LPFS and PID-5 instruments have exhibited acceptable reliability across a host of studies using different populations. Zimmermann et al. (2015) examined the structure of Criterion A in two samples, one of lay people and another of mental health practitioners, using informant rather than self-reports. They found that (a) the four sub-domains of Criterion A generally conform to the expected structure, (b) patterns of associations among these scales support the use of a general factor [i.e., global LPFS elevation], but (c) details of the model and the measure remain to be resolved. Specifically, not all descriptors loaded most strongly on their designated domain, nor did they all achieve their hypothesized level of severity. There is also some overlap between Criterion A and B due to the use of pathological trait variants (Pincus, 2013), which leads to a “collapsing” of the structure when factored together (Zimmermann et al., 2015). Nonetheless, these results broadly support the hypothesized structure of the Model in general and of the LPFS in particular.
Several studies demonstrate the criterion validity of Criterion A. The Criterion A constructs significantly predict the presence and number of PDs in diverse samples (Few et al., 2013; Morey et al., 2013). Morey et al. (2014) found that an LPFS score of moderate or greater demonstrated 84.6% sensitivity and 72.7% specificity for identifying patients who met criteria for at least one Section II PD diagnosis, and Criterion A significantly incremented the ten combined Section II PD categories when predicting functional impairment, prognosis, and treatment intensity.
There has been an even more rapid accumulation of research supporting the Criterion B trait model over the past several years. The structure of the DSM-5 trait model was initially developed based on factor analyses of responses to PID-5 items in large representative population samples. Therefore, it is not surprising that the structure replicates in samples of undergraduates (Wright, Thomas, et al., 2012), US community samples (Creswell, Bachrach, Wright, Pinto, & Ansell, in press), European samples (Zimmermann, Altenstein, et al., 2014), informant reports (Markon, Quilty, Bagby, & Krueger, 2013), and clinician reports (Morey et al., 2013).
Importantly, the AMPD traits can account for large portions of the variance in the Section II PD constructs, whether assessed via self-report (Hopwood, Thomas, Markon, Wright, & Krueger, 2012) or interview (Few et al., 2013). Morey and Skodol (2013) provide evidence that diagnostic rules for DSM-5 PDs result in greater correspondence between DSM-IV and DSM-5 than was observed between DSM-III and DSM-III-R. In addition, the AMPD traits surpass Section II PD criterion counts and psychiatric symptoms in predicting psychosocial impairment (Simms & Calabrese, in press). Beyond comparisons of the Section III and Section II systems, the content validity of the PID-5 has received substantial support (e.g., Anderson et al., 2013; Hopwood, Schade, Krueger, Wright, & Markon, 2013). In addition, concurrent validity for key clinical personality constructs less well conceptualized in DSM-IV also appears strong; pathological narcissism, including both more vulnerable and more grandiose aspects (Wright, Pincus et al., 2013), and psychopathy (Fossati et al., 2013) are reasonably well captured by the DSM-5 traits. Thus, the DSM-5 trait model appears to be on solid empirical footing.
Wright et al. (2015) examined the stability of the DSM-5 traits in a sample of psychiatric outpatients, finding that the DSM-5 traits were highly stable over the course of 1.4 years in terms of mean level (average Cohen’s d = −.11) and rank order (average r/disattenuated r = .67/.79). Further, the DSM-5 traits significantly predicted future dysfunction across a variety of domains (e.g., life-satisfaction, interpersonal problems, social, occupational functioning, etc.), and individual changes in traits over the course of the study were significantly associated with changes in functioning. Although additional longitudinal work is necessary, these initial results suggest that, in contrast to the traditional DSM categories and symptoms, the DSM-5 Section III traits better match the levels of consistency that are a defining feature of PD and evident in studies of longitudinal impairment (Morey & Hopwood, 2013).
Current and emerging investigation substantially advances validation of the AMPD (Morey, Benson, Busch, & Skodol, 2015), despite caveats (Widiger & Crego, 2015). Kendler (2009) argued that a diagnostic system should be built from a bottom-up, iterative process rooted in empirical findings. This contrasts with the traditional “top-down” approach of consensus of authoritative bodies (e.g., the standard Section II categorical PDs; Markon, 2013). Generated from cumulative trends in personality assessment science, the AMPD comes closer to Kendler’s (2009) desideratum than previous classifications. This is not an academic or esoteric matter. The empirical grounding of the AMPD establishes its place within evidence-based treatment methods. This status furthermore paves the way for increased use in forensic practice.
Clinical Use of the AMPD
The AMPD can be learned and used reliably with minimal specific training (Few et al., 2013; Morey et al., 2015; Zimmermann, Benecke et al., 2014). Its integration of major assessment paradigms confers transferability to well-known tests, common constructs, and widely-used interpretive frameworks. Clinicians can use several available resources to familiarize themselves with the model, starting with review of the DSM-5 Section III chapter. Particularly useful are tables in DSM-5 (pp.775–781) specifying indicators for the LPFS and defining the 5 trait domains and 25 trait facets of Criterion B (versions of which are Table S1 and S2 in the online supplemental material). Current reviews of the literature such as Morey et al. (2015), Krueger & Markon (2014), and Widiger (2015) provide key background.
Morey & Stagner (2012) used the AMPD to inform psychotherapy with a severely disturbed patient with narcissistic pathology. In this case report, they showed how psychotherapeutic postures informed by the AMPD (i.e., adopting “mirroring” and transference-based strategies) produced treatment gains greater than had been achieved in previous therapy conducted from DSM-IV formulations. Ronningstam (2014) showed how AMPD constructs related to dynamics of self-esteem management help in formulating subjective data that otherwise would appear discrepant with overt behavior. Examining the construct of identity in two complex clinical cases, Schmeck et al. (2013) showed how the AMPD increments traditional PD diagnosis and guides treatment planning. Bach, Markon, et al. (2015) provided six detailed patient case reports using the AMPD. They showed how the AMPD differentially guides diagnosis, treatment, and patient feedback strategies.
In practice, a global rating of “2” or more (moderate impairment) on two of the four dimensions (identity, self-direction, empathy, and intimacy) of the LPFS is required for a diagnosis of PD. LPFS ratings may be formulated from observation, history, interview, and psychological test data. Bender et al. (2011) detailed many test and interview approaches from which the LPFS was developed; these measures may be used in practice to inform ratings on the LPFS. Because Criterion A addresses overall level of personality impairment, severity or profile elevation indices from tests such as the MMPI-2 or Personality Assessment Inventory (PAI) are relevant. Performance based assessment methods such as the Rorschach or Thematic Apperception Test (TAT) also provide measures of overall level of personality functioning. For example, well-validated measures from the R-PAS systematization of the Rorschach procedures (Viglione, Perry, Giromini, & Meyer, 2011), and the Social Cognition and Object Relations scale (SCORS; Westen, Lohr, Silk, Gold, & Kerber, 1990) of the TAT provide indices of level of personality functioning.
Regarding Criterion B, the AMPD does not specify how to determine significance with traits or facets. Rational decision and convention (Samuel, Hopwood, Krueger, Thomas, & Ruggero, 2013) suggest ratings of “2” (sometimes true) or “3” (very true) on the 25 single-item Facet scales reflect clinical significance. Clinicians may use the PID-5 norms (Krueger, Derringer, Markon, Watson, & Skodol, 2012) to compute standard scores, and define “high scores” with a conventional cut-off (e.g., 65 or 70T) with either PID-5 self-report or informant forms. One may also apply clinical ratings to the five trait domains, or use values of the (significant) facets that constitute respective trait domains to calculate overall scores (Samuel et al., 2013). These data then can be used to determine the hybrid categorical-dimensional diagnoses (e.g., avoidant, borderline, etc.) following the algorithms provided in the DSM-5.
Research provides strong support for the PID-5 in the assessment of Criterion B traits. Maples et al. (2015) showed that a short form of the PID-5 (100 items) was capable of assessing both the facets and domains reliably and validly. This short form may be useful when time is limited. Samuel (2015) comprehensively reviewed clinician diagnostic agreement in the domain of PDs, comparing interview, self-report, and informant-report formats. He concluded levels of agreement are fairly robust, albeit minor to moderate method differences exist (see also Markon, Quilty, Bagby, & Krueger, 2013). Samuel (2015) opined self-report and informant-report assessment compares favorably with interview-based assessment, and recommended the PID-5 as a promising approach to PD diagnosis.
Popular psychometric instruments can also inform clinical ratings of traits and facets. For example, the MMPI-2 PSY-5 scales correspond to the AMPD maladaptive traits (Anderson et al., 2013). PAI scales can reliably indicate and discriminate Criterion B maladaptive traits (Hopwood et al., 2013). The Millon Multiaxial Clinical Inventory (MCMI-III; Craig, 2005), Dimensional Assessment of Personality Pathology (Livesley, Jackson, & Schroeder, 1989), Schedule for Nonadaptive and Adaptive Personality (SNAP; Clark, 1993), and the Computerized Adaptive Assessment of Personality Disorder (CAT-PD; Simms et al., 2011) are other inventories directly relevant to PD assessment. From the cognitive-behavioral therapy (CBT) perspective, the Beck and Beck (1991) Personality Beliefs Questionnaire and CBT-based measures from Schema Therapy closely map onto the AMPD (Hopwood et al., 2013; Bach, Lee, Mortensen, & Simonsen, 2015). The Shedler-Westen Assessment Procedure (SWAP; Shedler & Westen, 2007), involving Q-sort clinician ratings of clinical observations, provides quantitative indicators of PD syndromes. Performance-based (aka “projective”) testing similarly can assist trait and facet determinations. Weiner’s (2015) review of “explicit” (i.e., structured, self-report) and “implicit” (i.e., unstructured, performance) assessment of PDs, and Bornstein’s (2015) “process assessment” model, integrating structured and unstructured methods, summarize how performance-based methods inform PD evaluation.
Psychological assessment with the AMPD parallels the “Review of Systems” diagnostic approach used in clinical medicine, as noted in the DSM-5 (APA, 2013, p. 774; see also Harkness et al., 2014). In other words, all relevant spheres of diagnostic concern are systematically surveyed. Practically-speaking, this means that following a determination of moderate or greater elevation on the LPFS, all five trait domains and 25 facets are reviewed. Psychodiagnostically, this “review of systems” helps to ensure important data are not overlooked. This is a crucial point because diagnostic impressions can be colored by urgent or dramatic signs and symptoms. Although clinicians, like people in general, tend to make quite accurate impressionistic assessments (e.g., Ambady’s [2010] program of research demonstrating the accuracy of “thin-slicing” in person perception), inferences are subject to error unless deliberate, systematic analysis is also employed. Much like a pilot with a pre-flight checklist prior to take off, “review of systems” with the 5 traits and 25 facets safeguards diagnostic appraisal from common forms of error and omission.
Structured interview formats for the AMPD are currently in development (Zachar & First, 2014). Waugh (2014) offers a clinician-friendly template (PDLT-C) for organizing data within the AMPD framework similar to Gordon and Bornstein’s (2015) Psychodiagnostic Chart-2 [PDC-C]. However, typically, the clinician simply synthesizes observations and inferences into AMPD ratings.
Albeit a new PD system, inclusion in the DSM-5 confers legitimacy in forensic settings as well (Zachar et al., 2015). It’s growing clinical and research record brings scientific credibility sufficient for supplemental use in the forensic arena. In point of fact, one author (MHW) has used the AMPD in administrative law settings in which the diagnosis of PD was disputed.
Case Example
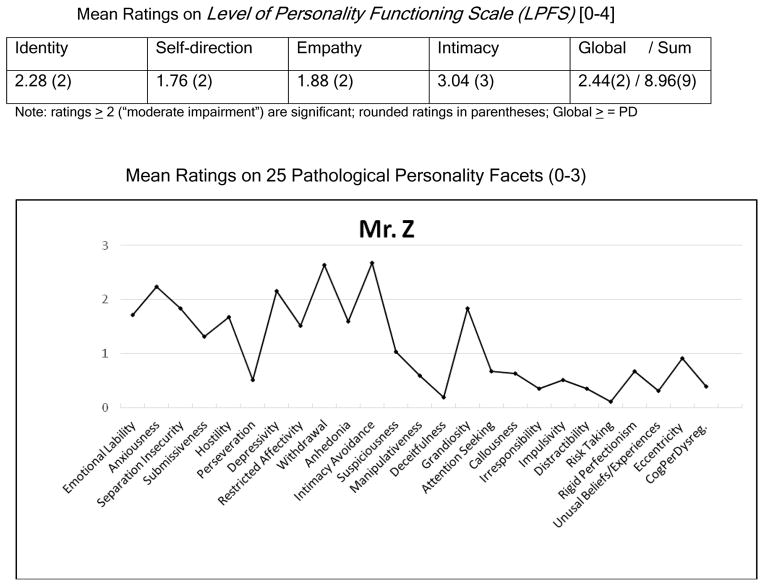
We present a case with a profile of AMPD results that will look familiar to most clinicians. This case example not only illustrates use of AMPD ratings, but demonstrates the ease and consistency with which clinicians can apply the AMPD. A convenience sample of clinicians (n=25) evaluated a case vignette abstracted from Kohut’s (1979) classic article, “The two analyses of Mr. Z” (vignette available from MHW). Kohut (1979) described a patient in an orthodox psychoanalysis, followed by a subsequent analysis informed by self-psychology.6 The 263-word case vignette was composed from Kohut’s (1979) depiction of Mr. Z’s history, presentation, and behavior (i.e., anxious, retiring, intellectualizing, thin-skinned, lonely, and rejection-sensitive) in the early phase of analysis. This case reflects aspects of “vulnerable” narcissism, a presentation which may be more difficult to capture in common diagnostic systems (Pincus & Lukowitsky, 2010). Raters were blind to the identity of the case (except for MHW); they included 12 clinicians and 13 academic clinical psychologists (theoretical orientations included psychodynamic, interpersonal, cognitive-behavioral, and integrative), with a median of 20 years clinical experience, and many with expertise in personality assessment and/or PDs. Raters were not formally trained. They were simply asked to provide an AMPD diagnosis for the case vignette and refer to the text of the DSM-5, Section III, as needed. In this way, the clinicians’ ratings likely resembled routine clinical practice as opposed to judgments made under the controlled conditions of research settings. Thus, agreement among raters may reflect typical rather than maximal diagnostic concordance-- offering a more realistic assessment of clinician agreement with the AMPD. Clinicians varied from very little to extensive familiarity with the AMPD. Inter-rater reliability results yielded an intraclass correlation (ICC [2,1]) for the LPFS and 25 trait facets combined of 0.53 for a single rater; across the group of 25 raters, the ICC was 0.97. Thus, there was strong agreement across raters in applying the AMPD to a short case vignette. Also, 24 of 25 clinicians (96%) rated Mr. Z positive on Criterion A, establishing a PD diagnosis (Figure 1). The profile of the 25 trait facets shows elevations on Anhedonia, Anxiousness, Depressivity, Emotional Lability, Grandiosity, Hostility, Restricted Affectivity, Submissiveness, Separation Insecurity, and peak elevations on Intimacy Avoidance and Withdrawal. Applying AMPD diagnostic algorithms (DSM-5, pp. 764–770) to these data yields hybrid categorical-dimensional diagnoses of Avoidant and Borderline PD.
Figure 1.
LPFS scores for Criterion A; Facet scores in profile format for Criterion B, based on ratings of Kohut’s (1979) fictive-autobiographical “Mr. Z.” by 25 clinicians.
Results depict an individual with “moderate” personality impairment (global rating of 2 on LPFS) and particular liability in intimacy aspects of the interpersonal domain. In terms of dispositional traits, the profile shows an anxious individual who is interpersonally detached and reserved, yet also emotionally reactive, irritable or angry, as well as self-focused and sensitive to slights. The AMPD data are consistent with “narcissistic vulnerability” (Pincus, Cain, & Wright, 2014). Raters gave diagnostic impressions prior to the AMPD. Avoidant and narcissistic PD or traits were frequently listed, followed by diagnoses ranging from dysthymia, social anxiety disorder, other depressive and anxiety disorders, to borderline traits. The AMPD ratings appeared to capture many constructs reflected in the clinicians’ diverse diagnostic impressions while providing a psychometric profile of meaningful data. This example illustrates how the AMPD provides data for both diagnosis and psychological assessment; this dual benefit aids clinical practice (e.g., Schmeck et al., 2013; Bach, Markon et al., 2015).
Whither the AMPD?
The AMPD is listed as an Emerging Model and Measure in DSM-5 Section III. A limitation of the AMPD approach is that is not the official Section II PD diagnostic system. The AMPD also has seen critiques. Proponents of a prototype-based diagnostic model (involving ratings of exemplar descriptions of syndromes, as in DSM-I and –II), argue prototype diagnosis provides more clinical utility (Shedler et al., 2010). Some have noted coauthor/academic commonality within the P&PD Work Group and speculated that other views may have received less attention (e.g., Blashfield & Reynolds, 2012; Widiger & Crego, 2015). Crego, Sleep, & Widiger (2015) suggested the clinical utility of some AMPD PD algorithms are not optimal and that other FFM approaches may offer improved clinical utility in trait ratings.
Research on incremental validity of Criterion A (LPFS) over Criterion B’s pathological personality traits has shown mixed results. A cross-sectional study (Few et al., 2013) found little support for incremental validity of Criterion A over Criterion B; however, a study examining prediction of longitudinal criteria (Roche, Jacobson, & Pincus, 2015) found evidence supporting the incremental validity of Criterion A above and beyond Criterion B. The issue of incremental validity and Criterion A and B convergence are subject to further empirical and conceptual explication. From a construct validity point of view (Loevinger, 1957), Criterion A and B require nuanced analysis beyond incremental or predictive validity. Relatedly, Morey (1991) pointed out that diagnostic classifications carry surplus meanings beyond operationalized criteria.
Operationalization of the AMPD certainly requires further study. This includes refinement of thresholds and cut points for ratings, optimal algorithms for hybrid categorical-dimensional diagnoses (Crego et al., 2015), and improved norms for ratings and instruments. The AMPD will receive additional scrutiny of its clinical utility, reliability, and validity. Importantly, traditional psychometric principles (Nelson-Gray, 1991) can be used to evaluate the AMPD diagnostic system and measures. In this regard, a major advantage of the AMPD is that the comparison of a diagnostic system to a psychological test (Blashfield & Livesley, 1991) no longer is “metaphoric.” The assessment paradigms and psychometric specification of the AMPD establish direct connections to psychological testing. Training in the use of the AMPD as well as development of standardized research interviews are receiving attention (Zachar & First, 2014). As more training programs teach the AMPD, future psychologists will be familiar with the approach and its application.7
Summary
Using concepts and assessment techniques familiar to practitioners (e.g., dysfunctional interpersonal boundaries; MMPI-2 PSY-5 Scales; FFM approaches), the AMPD is pluralistic theoretically and methodologically. This pantheoretical approach integrates the nomological nets of major personality assessment paradigms. This heritage confers clinical fidelity and compatibility with many clinical orientations. Practitioners of different orientations and disciplinary background will find many aspects of the AMPD familiar. Furthermore, the AMPD directly connects to instruments commonly used to assess personality and offers AMPD-specific instruments that are in the public domain.
Hybrid categorical-dimensional diagnosis from assessment of severity and style of personality dysfunction rectifies many limitations of traditional PD diagnosis. Through dimensionalization, the AMPD conforms to contemporary conceptualization of PDs and aligns with broader trends in the DSM-5 and with the NIMH RDoC. Emerging validity studies are strong. The central characteristics of the AMPD (dimensionalization, integration of assessment paradigms, and ties to psychological testing) establish its’ place at the forefront of PD diagnosis (Krueger, Hopwood, Wright, & Markon, 2014; Rodriguez-Seijas, Eaton, & Krueger, 2015). In short, the AMPD is an innovative approach to PD diagnosis that synthesizes assessment traditions while alleviating many shortcomings of past diagnostic systems. Not only is this a scientific advance, but the needs of the practicing clinician are met through the twin functions of psychiatric classification and psychological assessment that the AMPD provides.
Supplementary Material
Acknowledgments
The first and second authors took lead in orchestrating the substantive contributions of all authors. Opinions expressed by Mark H. Waugh are his and do not reflect the position of the Oak Ridge National Laboratory, UT-Battelle, LLC, or the U.S. Department of Energy. Aidan Wright’s effort on this project was supported by a grant from the National Institute of Mental Health (L30 MH101760). The opinions expressed are solely those of the authors and not necessarily those of the funding source.
Biographies
Mark H. Waugh received his Ph.D. in clinical psychology from the University of Florida and post-doctoral fellowship from Yale University School of Medicine. He is currently in practice in Oak Ridge, Tennessee, consults to the Oak Ridge National Laboratory, and is clinical faculty at the University Of Tennessee Department Of Psychology. His areas of professional interest include personality assessment, assessment in law enforcement and security settings, and personality theory.
Christopher J. Hopwood received his Ph.D. in clinical psychology from Texas A&M University. He is currently Associate Professor of Clinical Psychology and Director of the Interpersonal Problems Clinic at Michigan State University. His areas of professional interest include personality assessment, personality disorders, and interpersonal processes.
Robert F. Krueger received his Ph.D. in clinical psychology from the University of Wisconsin, Madison. He is currently Distinguished McKnight University Professor and Hathaway Distinguished Professor, and serves as Director of Clinical Training, in the Department of Psychology at the University of Minnesota and was a member of the APA DSM-5 Personality and Personality Disorder Work Group. His areas of professional interest include classification and etiology of psychopathology and personality, using psychometric, quantitative and molecular genetic, and neuroscience approaches.
Leslie C. Morey received his Ph.D. in clinical psychology from the University of Florida. He is currently George T. and Gladys H. Abell Professor at Texas A & M University and former Chair of the Department of Psychology and was a member of the APA DSM-5 Personality and Personality Disorder Work Group. His areas of professional interest include authorship and study of the Personality Assessment Inventor, assessment, diagnosis, classification of personality and psychopathology, personality disorders, and alcoholism.
Aaron L. Pincus received his Ph.D. in clinical psychology from the University of British Columbia. He is currently professor of psychology in the department of psychology at the Pennsylvania State University and Editor-in-Chief of Assessment. His areas of professional interest include interpersonal approaches to personality, personality disorders, and personality assessment.
Aidan G. C. Wright received his Ph.D. in clinical psychology from Pennsylvania State University. He is currently Assistant Professor and Director of the Personality Processes and Outcomes Laboratory in the Department of Psychology at the University of Pittsburgh. His areas of professional interest include basic personality science and integrative study of personality, its pathology, and other forms of psychopathology.
Footnotes
Dimensional representation of PD also was argued prior to and shortly after publication of the DSM-III and every edition since (see Zachar et al., 2015).
The diagnosis Other Specified Personality Disorder involves specification. Specification may be done with the AMPD. In this way the AMPD may be medically coded (301.89).
The neurobiological paradigm is increasingly applied in personality and psychopathology (e.g., Depue & Collins, 1999). It should be noted that some psychobiological constructs (e.g., temperament dimensions; anhedonia, etc.) are represented in the pantheoretical AMPD.
Clinicians familiar with the Cattell-Horn-Carroll distinctions between broad and narrow cognitive abilities (Sternberg, 2012) will note the (multivariate paradigmatic) parallel to the FFM tradition in Criterion B.
These concerns are important and raise issues of theory, methodology, and for traditional practice. For example, the idea of diagnostic categories ultimately is an ontological matter. Clinicians may think in terms of categories, as reflected in traditional categorical diagnoses and the empirical prototype approach to PD diagnosis (Shedler & Westen, 2007). Yet, the way in which clinical phenomena are perceived is not the same as the intrinsic nature of the phenomena (Meehl, 1992).
Current scholarship reveals that “Mr. Z” is Heinz Kohut himself, a fictive-autobiographical statement of his experience in psychoanalysis (Strozier, 2001). Using Mr. Z as a target for AMPD ratings offers historical, heuristic, and clinical relevance.
All of the current authors, representing six clinical psychology doctoral programs, instruct students in the AMPD; numerous other programs also teach the AMPD.
Contributor Information
Mark H. Waugh, Private Practice, Oak Ridge, Tennessee, Oak Ridge National Laboratory, & University of Tennessee
Christopher J. Hopwood, Michigan State University
Robert F. Krueger, University of Minnesota
Leslie C. Morey, Texas A & M University
Aaron L. Pincus, Pennsylvania State University
Aidan G. C. Wright, University of Pittsburgh
References
- Ambady N. The perils of pondering: Intuition and thin slice judgments. Psychological Inquiry. 2010;21:271–278. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (DSM-5) Arlington, VA: Author; 2013. [Google Scholar]
- Anderson JL, Sellbom M, Bagby RM, Quilty LC, Veltri CO, Markon KE, Krueger RF. On the convergence between PSY-5 domains and PID-5 domains and facets: Implications for assessment of DSM-5 personality traits. Assessment. 2013;20:286–294. doi: 10.1177/1073191112471141. [DOI] [PubMed] [Google Scholar]
- Bach B, Markon K, Simonsen E, Krueger R. Clinical utility of the DSM-5 Alternative Model of Personality Disorders: Six Cases from practice. Journal of Psychiatric Practice. 2015;21:1–23. doi: 10.1097/01.pra.0000460618.02805.ef. [DOI] [PubMed] [Google Scholar]
- Bach B, Lee C, Mortensen E, Simonsen E. How do DSM-5 personality traits align with schema therapy constructs? Journal of Personality Disorders. 2015;29:212–240. doi: 10.1521/pedi_2015_29_212. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck JS. The Personality Belief Questionnaire. Bala Cynwid, PA: The Beck Institute for Cognitive Therapy and Research; 1991. [Google Scholar]
- Bender DS, Morey LC, Skodol AE. Toward a model for assessing level of personality functioning in DSM–5, Part I: A review of theory and methods. Journal of Personality Assessment. 2011;93:332–346. doi: 10.1080/00223891.2011.583808. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Iscan C, Maser J the Boards of Directors of the Association for Research in Personality Disorders, the International Society for the Study of Personality Disorders. Opinions of personality disorder experts regarding the DSM-IV personality disorders classification system. Journal of Personality Disorders. 2007;21:536–551. doi: 10.1521/pedi.2007.21.5.536. [DOI] [PubMed] [Google Scholar]
- Blashfield RK, Livesley WJ. Metaphorical analysis of psychiatric classification as a psychological test. Journal of Abnormal Psychology. 1991;100(3):262–270. doi: 10.1037//0021-843x.100.3.262. [DOI] [PubMed] [Google Scholar]
- Blashfield RK, Reynolds SM. An invisible college view of the DSM-5 personality disorder classification. Journal of Personality Disorders. 2012;26:821–829. doi: 10.1521/pedi.2012.26.6.821. [DOI] [PubMed] [Google Scholar]
- Bornstein RR. Process-focused assessment of personality pathology. In: Huprich SK, editor. Personality Disorders: Toward Theoretical and Empirical Integration in Diagnosis and Assessment. Washington, DC: American Psychological Association; 2015. pp. 271–290. [Google Scholar]
- Clark LA. Schedule for Nonadaptive and Adaptive Personality. Minneapolis: University of Minnesota Press; 1993. [Google Scholar]
- Clarkin JF, Huprich SK. Do DSM-5 personality disorder proposals meet criteria for clinical utility? Journal of Personality Disorders. 2011;25:192–205. doi: 10.1521/pedi.2011.25.2.192. [DOI] [PubMed] [Google Scholar]
- Craig RJ, editor. New directions in interpreting the Millon Clinical Multiaxial Inventory-III (MCMI-III) John Wiley & Sons; 2005. [Google Scholar]
- Crego C, Sleep CE, Widiger TA. Clinicians’ judgments of the clinical utility of personality disorder trait descriptions. Journal of Nervous and Mental Disease. 2015 doi: 10.1097/NMD.0000000000000424. Online Advanced Publication. [DOI] [PubMed] [Google Scholar]
- Creswell KG, Bachrach RB, Wright AGC, Pinto AL, Ansell EB. Predicting problematic alcohol use with the DSM-5 alternative model of personality pathology in treatment seeking and non-seeking samples. Personality Disorders: Theory, Research, and Treatment in press. [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Medicine. 2013;11:126–134. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. Behavioral and Brain Sciences. 1999;22:491–517. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, Collins B, MacKillop J. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. Journal of Abnormal Psychology. 2013;122:1057–1069. doi: 10.1037/a0034878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleeson W, Jayawickreme E. Whole trait theory. Journal of Research in Personality. 2015 doi: 10.1016/j.jrp.2014.10.009. Online advanced publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati A, Krueger RF, Markon KE, Borroni S, Maffei C. Reliability and Validity of the Personality Inventory for DSM-5 (PID-5): Predicting DSM-IV Personality Disorders and Psychopathy in Community-Dwelling Italian Adults. Assessment. 2013;20:689–708. doi: 10.1177/1073191113504984. [DOI] [PubMed] [Google Scholar]
- Gordon RM, Bornstein RF. The Psychodiagnostic Chart-2. 2015 Retrieved from https://sites.google.com/site/psychodiagnosticchart/
- Gore WL, Widiger TA. The DSM-5 dimensional trait model and five-factor models of general personality. Journal of Abnormal Psychology. 2013;122:816–821. doi: 10.1037/a0032822. [DOI] [PubMed] [Google Scholar]
- Harkness AR, Reynolds SM, Lilienfeld SO. A review of systems for psychology and psychiatry: adaptive systems, personality psychopathology five (PSY–5), and the DSM–5. Journal of Personality Assessment. 2014;96:121–139. doi: 10.1080/00223891.2013.823438. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Pincus AL, Wright AGC. The interpersonal situation: Integrating personality assessment, clinical formulation, and intervention. In: Samuel D, Lynam D, editors. Purdue symposium on psychological science. New York: Oxford; in press. [Google Scholar]
- Hopwood CJ, Schade N, Krueger RF, Wright AGC, Markon KE. Connecting DSM-5 personality traits and pathological beliefs: Toward a unifying model. Journal of Psychopathology and Behavioral Assessment. 2013;35:162–172. doi: 10.1007/s10862-012-9332-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM-IV personality disorders. Journal of Abnormal Psychology. 2012;121:424–432. doi: 10.1037/a0026656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Wright AGC, Ansell EB, Pincus AL. The interpersonal core of personality pathology. Journal of Personality Disorders. 2013;27:270–295. doi: 10.1521/pedi.2013.27.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Wright AGC, Krueger RF, Shade N, Markon KE, Morey LC. DSM-5 Pathological personality traits and the Personality Assessment Inventory. Assessment. 2013;20:269–285. doi: 10.1177/1073191113486286. [DOI] [PubMed] [Google Scholar]
- Kendler KS. An historical framework for psychiatric nosology. Psychological Medicine. 2009;39(12):1935–1941. doi: 10.1017/S0033291709005753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernberg OF. Overview and critique of the classification of personality disorders proposed for the DSM-5. Swiss Archive for Neurology and Psychiatry. 2012;163:234–238. [Google Scholar]
- Kohut H. The two analyses of Mr. Z. International Journal of Psychoanalysis. 1979;60(1):3–27. [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon K, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine. 2012;42:1879–1890. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hopwood CJ, Wright AG, Markon KE. DSM-5 and the path toward empirically based and clinically useful conceptualization of personality and psychopathology. Clinical Psychology: Science and Practice. 2014;21:245–261. [Google Scholar]
- Krueger RG, Skodol AE, Livesley WJ, Shrout PE, Huang Y. Synthesizing categorical and dimensional approaches to personality disorders: Refining the research agenda for DSM-V, Axis II. International Journal of Methods in Psychiatric Research. 2007;16:65–73. doi: 10.1002/mpr.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annual Review of Clinical Psychology. 2014;10:477–501. doi: 10.1146/annurev-clinpsy-032813-153732. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, First MB, Reiger DA. A research agenda for DSM-5. Washington, DC: American Psychiatric Association; 2002. [Google Scholar]
- Livesley WJ, Jackson DN, Schroeder MJ. A study of the factorial structure of personality pathology. Journal of Personality Disorders. 1989;3:292–306. [Google Scholar]
- Loevinger J. Objective tests as instruments of psychological theory. Psychological Reports. 1957;3:635–694. [Google Scholar]
- Maples JL, Carter NT, Few LR, Crego C, Samuel DB, Williamson RL, Lynam DR, Widiger TA, Markon KE, Krueger RF, Miller JD. Testing whether the DSM-5 personality disorder trait model can be measured with a reduced set of items: An item response theory investigation of the Personality Inventory for DSM-5. Psychological Assessment. 2015 doi: 10.1037/pas0000120. [DOI] [PubMed] [Google Scholar]
- Markon KE. Epistemological pluralism and scientific development: An argument against authoritative nosologies. Journal of personality disorders. 2013;27:554–579. doi: 10.1521/pedi.2013.27.5.554. [DOI] [PubMed] [Google Scholar]
- Markon KE, Quilty LC, Bagby RM, Krueger RF. The development and psychometric properties of an informant-report form of the Personality Inventory for DSM- 5 (PID-5) Assessment. 2013;20:370–383. doi: 10.1177/1073191113486513. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Factors and taxa, traits and types, differences of degree and differences in kind. Journal of Personality. 1992;60:117–174. [Google Scholar]
- Morey LC. Classification of mental disorder as a collection of hypothetical constructs. Journal of Abnormal Psychology. 1991;100:289–293. doi: 10.1037//0021-843x.100.3.289. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ. Stability and change in personality disorders. Annual Review of Clinical Psychology. 2013;9:499–528. doi: 10.1146/annurev-clinpsy-050212-185637. [DOI] [PubMed] [Google Scholar]
- Morey LC, Skodol AE. Convergence between DSM-IV-TR and DSM-5 diagnostic models for personality disorder: Evaluation of strategies for establishing diagnostic thresholds. Journal of Psychiatric Practice. 2013;19:179–193. doi: 10.1097/01.pra.0000430502.78833.06. [DOI] [PubMed] [Google Scholar]
- Morey LC, Bender DS, Skodol AE. Validating the proposed diagnostic and statistical manual of mental disorders, severity indicator for personality disorder. Journal of Nervous and Mental Disease. 2013;201:729–735. doi: 10.1097/NMD.0b013e3182a20ea8. [DOI] [PubMed] [Google Scholar]
- Morey LC, Benson KT, Busch AJ, Skodol AE. Personality disorders in DSM-5: Emerging research on the alternative model. Current Psychiatry Reports. 2015;17:24–33. doi: 10.1007/s11920-015-0558-0. [DOI] [PubMed] [Google Scholar]
- Morey LC, Krueger RF, Skodol AE. The hierarchical structure of clinician ratings of proposed DSM–5 pathological personality traits. Journal of Abnormal Psychology. 2013;122:836–841. doi: 10.1037/a0034003. [DOI] [PubMed] [Google Scholar]
- Morey LC, Skodol AE, Oldham JM. Clinician judgments of clinical utility: A comparison of DSM-IV-TR personality disorders and the alternative model for DSM-5 personality disorders. Journal of Abnormal Psychology. 2014;123:398–405. doi: 10.1037/a0036481. [DOI] [PubMed] [Google Scholar]
- Morey LC, Stagner BH. Narcissistic pathology as a core personality dysfunction: comparing the DSM-IV and the DSM-5 proposal for narcissistic personality disorder. Journal of Clinical Psychology: In Session. 2012;68:908–921. doi: 10.1002/jclp.21895. [DOI] [PubMed] [Google Scholar]
- Mullins-Sweatt SN, Lengel GJ. Clinical utility of the five-factor model of personality disorder. Journal of Personality. 2012;80:1615–1639. doi: 10.1111/j.1467-6494.2012.00774.x. [DOI] [PubMed] [Google Scholar]
- Nelson-Gray RO. DSM-IV: Empirical guidelines from psychometrics. Journal of Abnormal Psychology. 1991;100:308–315. doi: 10.1037//0021-843x.100.3.308. [DOI] [PubMed] [Google Scholar]
- Pincus AL. A contemporary integrative interpersonal theory of personality disorders. In: Lenzenweger M, Clarkin J, editors. Major theories of personality disorder. 2. New York: Guilford; 2005. pp. 282–331. [Google Scholar]
- Pincus AL. Some comments on nosology, diagnostic process, and narcissistic personality disorder in the DSM-5 proposal for personality and personality disorders. Personality Disorders: Theory, Research, and Treatment. 2011;2:41–53. doi: 10.1037/a0021191. [DOI] [PubMed] [Google Scholar]
- Pincus AL. In through the out door: Commentary on “Personality Disorders are The Vanguard of the post-DSM-5.0 Era. Personality Disorders: Theory, Research, and Treatment. 2013;4:363–364. doi: 10.1037/per0000044. [DOI] [PubMed] [Google Scholar]
- Pincus AL, Cain NM, Wright AGC. Narcissistic grandiosity and narcissistic vulnerability in psychotherapy. Personality Disorders: Theory, Research, and Treatment. 2014;5:439–443. doi: 10.1037/per0000031. [DOI] [PubMed] [Google Scholar]
- Pincus AL, Hopwood CJ. A contemporary interpersonal model of personality pathology and personality disorder. In: Widiger TA, editor. Oxford Handbook of Personality Disorders. New York, NY: Oxford University Press; 2012. pp. 372–398. [Google Scholar]
- Pincus AL, Lukowitsky MR. Pathological narcissism and narcissistic personality disorder. Annual Review of Clinical Psychology. 2010;6:8–26. doi: 10.1146/annurev.clinpsy.121208.131215. [DOI] [PubMed] [Google Scholar]
- Roche MJ, Jacobson NC, Pincus AL. Examining the DSM-5 alternative model of personality disorders Criterion A and Criterion B associations with severity, emotional and cognitive triggers, variability, and oscillating patterns of personality impairment in daily life Submitted. [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, Krueger RF. How transdiagnostic factors of personality and psychopathology can inform clinical assessment and intervention. Journal of Personality Assessment. 2015 doi: 10.1080/00223891.2015.1055752. [DOI] [PubMed] [Google Scholar]
- Ronningstam. Beyond the diagnostic traits: A collaborative exploratory diagnostic process for dimensions and underpinnings of narcissistic personality disorder. Personality Disorders: Theory, Research, and Treatment. 2014;5:434–438. doi: 10.1037/per0000034. [DOI] [PubMed] [Google Scholar]
- Samuel DB. A review of the agreement between clinicians’ personality disorder diagnoses and those from other methods and sources. Clinical Psychology Science and Practice. 2015;22:1–19. [Google Scholar]
- Samuel DB, Hopwood CJ, Krueger RF, Thomas KM, Ruggero CJ. Comparing methods for scoring personality disorder types using maladaptive traits in DSM-5. Assessment. 2013;20:353–361. doi: 10.1177/1073191113486182. [DOI] [PubMed] [Google Scholar]
- Schmeck K, Schluter-Muller S, Foelsch P, Doering S. The role of identity in the DSM-5 classification of personality disorders. Child and Adolescent Psychiatry and Mental Health. 2013;7:1–11. doi: 10.1186/1753-2000-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shedler J, Westen D. The Shedler-Westen Assessment Procedure (SWAP): Making personality diagnosis clinically meaningful. Journal of Personality Assessment. 2007;89:41–55. doi: 10.1080/00223890701357092. [DOI] [PubMed] [Google Scholar]
- Shedler J, Beck A, Fonagy P, Gabbard GO, Gunderson J, Kernberg O, Michels R, Westen D. Personality disorders in DSM-5. American Journal of Psychiatry. 2010;167:1027–1028. doi: 10.1176/appi.ajp.2010.10050746. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Calabrese WR. Incremental validity of the DSM-5 Section III personality disorder traits with respect to psychosocial impairment. Journal of Personality Disorder. doi: 10.1521/pedi_2015_29_185. in press. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Goldberg LR, Roberts JE, Watson D, Welte J, Rotterman JH. Computerized adaptive assessment of personality disorder: Introducing the CAT–PD project. Journal of Personality Assessment. 2011;93:380–389. doi: 10.1080/00223891.2011.577475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South SC, DeYoung NJ. Behavior genetics of personality disorders: Informing classification and conceptualization in DSM-5. Personality Disorders: Theory, Research, and Treatment. 2013;4:270–283. doi: 10.1037/a0026255. [DOI] [PubMed] [Google Scholar]
- Sternberg RJ. Intelligence. Wiley Interdisciplinary Reviews: Cognitive Science. 2012;3:501–511. doi: 10.1002/wcs.1193. [DOI] [PubMed] [Google Scholar]
- Strozier CB. Heinz Kohut: The making of a psychoanalyst. New York: Farrar, Straus, & Giroux; 2001. [Google Scholar]
- Thomas KM, Yalch MM, Krueger RF, Wright AGC, Markon KE, Hopwood CJ. The convergent structure of DSM-5 personality trait facets and the five-factor model (FFM) trait domains. Assessment. 2013;20:308–311. doi: 10.1177/1073191112457589. [DOI] [PubMed] [Google Scholar]
- Verheul R. Clinical utility of dimensional models for personality pathology. Journal of Personality Disorders. 2005;19:283–302. doi: 10.1521/pedi.2005.19.3.283. [DOI] [PubMed] [Google Scholar]
- Verheul R, Andrea H, Berghout C, Dolan CC, Busschbach JJV, van der Kroft PJA, Bateman AW, Fonagy P. Severity Indices of Personality Problems (SIPP–118): Development, factor structure, reliability and validity. Psychological Assessment. 2008;20:23–34. doi: 10.1037/1040-3590.20.1.23. [DOI] [PubMed] [Google Scholar]
- Viglione DJ, Perry W, Giromini L, Meyer GJ. Revising the Rorschach Ego Impairment Index to accommodate recent recommendations about improving Rorschach validity. International Journal of Testing. 2011;11:349–364. [Google Scholar]
- Waugh MH. The PDLT-C. Oak Ridge: Tennessee; 2014. Unpublished manuscript. [Google Scholar]
- Westen D, Lohr N, Silk KR, Gold L, Kerber K. Object relations and social cognition in borderlines, major depressives, and normals: A Thematic Apperception Test analysis. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2:355–364. [Google Scholar]
- Weiner IB. Assessing explicit and implicit processes in personality pathology. In: Huprich S, editor. Personality Disorders: Toward Theoretical and Empirical Integration in Diagnosis and Assessment. Washington, DC: American Psychological Association; 2015. pp. 253–270. [Google Scholar]
- Widiger TA. Assessment of DSM-5 personality disorder. Journal of Personality Assessment. 2015;97:456–466. doi: 10.1080/00223891.2015.1041142. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Crego C. The process and content of DSM-5. Psychopathology Review. 2015;2:162–176. [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. American Psychologist. 2007;62:71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. Paradigms of personality assessment. New York: Guilford Press; 2003. [Google Scholar]
- Wright AGC, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychological Medicine. 2015;45:2309–2319. doi: 10.1017/S0033291715000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Calabrese WR, Rudick MM, Yam WH, Zelazny K, Rotterman J, Simms LJ. Stability of the DSM-5 Section III pathological personality traits and their longitudinal associations with functioning in personality disordered individuals. Journal of Abnormal Psychology. 2015;124:199–207. doi: 10.1037/abn0000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Thomas KM, Hopwood CJ, Markon KE, Krueger RF. Conceptions of Narcissism and the DSM-5 Pathological Personality Traits. Assessment. 2013;20:339–352. doi: 10.1177/1073191113486692. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment. 2014;5:43–54. doi: 10.1037/per0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology. 2012;121:951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachar P, First MB. Transitioning to a dimensional model of personality disorders in DSM-5.1 and beyond. Current Opinion-Psychiatry. 2014;28:66–72. doi: 10.1097/YCO.0000000000000115. [DOI] [PubMed] [Google Scholar]
- Zachar P, Krueger RF, Kendler K. Personality disorders in the DSM-5: An oral history. Psychological Medicine. 2015 doi: 10.1017/S0033291715001543. [DOI] [PubMed] [Google Scholar]
- Zimmermann J, Altenstein D, Krieger T, Grosse Holtforth M, Pretsch J, Alexopoulos J, Leising D. The structure and correlates of self-reported DSM-5 maladaptive personality traits: Findings from two German-speaking samples. Journal of Personality Disorders. 2014;28:518–540. doi: 10.1521/pedi_2014_28_130. [DOI] [PubMed] [Google Scholar]
- Zimmermann J, Benecke C, Bender DS, Skodol AE, Schauenburg H, Cierpka M, Leising D. Assessing DSM-5 Level of Personality Functioning from videotaped clinical interviews: A pilot study with untrained and clinically inexperienced students. Journal of Personality Assessment. 2014;96:397–409. doi: 10.1080/00223891.2013.852563. [DOI] [PubMed] [Google Scholar]
- Zimmermann J, Böhnke JR, Eschstruth R, Mathews A, Wenzel K, Leising D. The latent structure of personality functioning: Investigating criterion A from the alternative model for personality disorders in DSM–5. Journal of Abnormal Psychology. 2015;124:532–548. doi: 10.1037/abn0000059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.