Abstract
Heat-shock factor 1 (HSF1) is the primary regulator of the response to various stressors. A previous study showed that HSF1 expression is associated with a poor prognosis in breast cancer and hepatocellular carcinoma; however, the prognostic significance of HSF1 in esophageal squamous cell carcinoma (ESCC) is unknown. Therefore, the present study investigated the association between HSF1 expression and the clinicopathological parameters of patients, as well as the association between HSF1 expression, and heat shock protein (Hsp)27, Hsp70 and Hsp90 expression induced by HSF1, by cDNA microarray and immunohistochemistry analyses. HSF1 protein and mRNA expression were assessed in resected specimens from 270 patients with ESCC in two independent cohorts. Hsp27, Hsp70 and Hsp90 expression were also assessed in 55/270 patients. Patients with high HSF1 expression had a significantly worse OS than those with low HSF1 expression in both cohorts. In multivariate analyses, pathological T stage [hazard ratio (HR), 2.21; 95% confidence interval (CI), 1.38–3.65; P=0.0008], pathological N stage (HR, 1.73; 95% CI, 1.04–3.02; P=0.03) and HSF1 expression (HR, 2.29; 95% CI, 1.48–3.64; P=0.0002) were statistically significant independent prognostic factors. Furthermore, Hsp27 and Hsp90 expression were significantly correlated with HSF1 expression (P<0.0001), but Hsp70 expression was not (P=0.38). These results indicate that HSF1 is a prognostic factor for patients with ESCC, and that Hsp27 and Hsp90, but not Hsp70, may be the downstream targets of HSF1 in ESCC.
Keywords: heat-shock factor 1, prognosis, esophageal squamous cell carcinoma
Introduction
Esophageal squamous cell carcinoma (ESCC) is the major histological type of esophageal cancer in East Asian countries, and is the eighth most common malignancy, and the sixth leading cause of cancer death worldwide (1). Despite improvements in surgical procedures, multidisciplinary therapies and perioperative management, the prognosis of patients with ESCC remains unsatisfactory (2). A staging system for ESCC based on clinicopathological features that can provide an accurate prediction of survival in patients aids clinicians in selecting the best treatment approach. Currently, the TNM classification is widely used to stage patients and to select treatment strategies (3). However, the assessment of prognosis using this system remains inadequate due to the considerable biological heterogeneity within the same stage of ESCC. Therefore, novel biological markers are required that provide a more accurate prognosis of patients and that facilitate in selecting the appropriate treatment strategy for individual patients.
Heat-shock transcription factor 1 (HSF1) is a transcription factor that induces the expression of heat shock proteins (Hsp) in response to various stressors (4,5). These Hsps act as molecular chaperones to maintain cellular homeostasis by restoring protein folding and stability. HSF1 facilitates survival in response stressors by regulating various cellular processes, such as cell-cycle control, protein translation and glucose metabolism (6,7). The expression of HSF1 is reportedly upregulated in cancer cell lines and cancer tissues of hepatocellular carcinoma, and high expression of HSF1 is associated with a poor prognosis in breast cancer and hepatocellular carcinoma (8,9). However, the role of HSF1 as a prognostic biomarker in ESCC has not been well investigated. Therefore, the present study analyzed HSF1 mRNA and protein expression in resected ESCC tissues to determine if the expression of HSF1 could be used as a prognostic biomarker in ESCC.
Materials and methods
Sample collection
Samples of resected ESCC and normal squamous epithelium were obtained from two independent cohorts, and assayed for HSF1 mRNA and protein expression. Cohort 1 was composed of 58 ESCC samples, which were collected during subtotal esophagectomy between February 2005 and March 2009 after obtaining written informed consent. All patients underwent subtotal esophagectomy at one of five hospitals (Juntendo University Hospital, Tokyo, Japan; National Cancer Center Hospital, Tokyo, Japan; Kurume University Hospital, Fukuoka, Japan; Saitama Cancer Center, Saitama, Japan; Kagoshima University Hospital, Kagoshima, Japan). The clinicopathological characteristics of patients are indicated in Table I. All patients underwent curative resection and no patients received neoadjuvant therapy. The tumor samples were submitted for cDNA microarray analysis.
Table I.
Correlation between HSF1 mRNA expression and clinicopathological parameters in cohort 1.
| Parameter | Low (n=29) | High (n=29) | P-value |
|---|---|---|---|
| Age, yearsa | 66 (52–82) | 66 (52–79) | 0.72 |
| Gender, n | |||
| Male | 24 | 18 | 0.08 |
| Female | 5 | 1 | |
| Location, n | |||
| Ut | 3 | 8 | 0.24 |
| Mt | 16 | 13 | |
| Lt | 10 | 8 | |
| Histological grade, n | |||
| G1 | 12 | 8 | 0.49 |
| G2 | 14 | 16 | |
| G3 | 3 | 5 | |
| pT stage, n | |||
| 1 | 4 | 4 | 0.69 |
| 2 | 3 | 5 | |
| 3 | 19 | 15 | |
| 4 | 3 | 5 | |
| pN stage, n | |||
| 0 | 15 | 9 | 0.61 |
| 1 | 5 | 6 | |
| 2 | 6 | 5 | |
| 3 | 3 | 9 |
Data are presented as median (range). HSF1, heat-shock factor 1; pT/N, pathological T/N; Ut, upper thoracic esophagus; Mt, mid-thoracic esophagus; Lt, lower thoracic esophagus.
Cohort 2 consisted of 212 ECC samples collected during subtotal esophagectomy at Osaka University Hospital (Osaka, Japan) between June 2000 and February 2013, following receipt of written informed consent. Patient characteristics, including the number of patients that underwent neoadjuvant therapy, are indicated in Table II. These specimens were submitted for immunohistochemical analysis. The present study was approved by the Ethics Committee of Osaka University Hospital (Osaka, Japan) and the written consent of all the patients was obtained. Pathological tumor stage was evaluated using the seventh edition of the TNM classification established by the Union for International Cancer Control (3).
Table II.
Correlation between HSF1 protein expression and clinicopathological parameters in cohort 2.
| Parameter | Low expression (n=103) | High expression (n=109) | P-value |
|---|---|---|---|
| Age, yearsa | 64 (47–79) | 65 (39–80) | 0.43 |
| Gender, n | |||
| Male | 89 | 95 | 0.87 |
| Female | 14 | 14 | |
| Histological grade, n | |||
| G1 | 27 | 22 | 0.14 |
| G2 | 43 | 62 | |
| G3 | 24 | 16 | |
| Gx | 9 | 9 | |
| Location, n | |||
| Ut | 11 | 18 | 0.03 |
| Mt | 65 | 47 | |
| Lt | 27 | 44 | |
| pT stage, n | |||
| T1 | 33 | 24 | 0.41 |
| T2 | 16 | 19 | |
| T3 | 51 | 61 | |
| T4 | 3 | 5 | |
| pN stage, n | |||
| N0 | 41 | 31 | 0.12 |
| N1 | 37 | 35 | |
| N2 | 16 | 29 | |
| N3 | 9 | 13 | |
| pStage, n | |||
| I | 22 | 18 | 0.10 |
| II | 34 | 24 | |
| III | 31 | 49 | |
| IV | 16 | 18 | |
| Neoadjuvant therapy | |||
| None | 39 | 46 | 0.52 |
| Chemotherapy | 64 | 63 |
Data are presented as median (range). HSF1, heat-shock factor 1; pT/N/Stage, pathological T/N/Stage; Ut, upper thoracic esophagus; Mt, mid-thoracic esophagus; Lt, lower thoracic esophagus.
Extraction of RNA and cDNA microarray analysis
Resected tumor tissues in cohort 1 were immediately cut (5 mm thickness), and embedded in Tissue-Tek OCT medium (Sakura Finetek Europe B.V., Alphen aan den Rijn, The Netherlands), frozen in liquid nitrogen and maintained at −80°C until RNA extraction. Following isolation of RNA and DNA using the QIAamp DNA Micro kit (Qiagen, Valencia, CA, USA) and the RNeasy Micro kit (Qiagen), cDNA was synthesized from 8.0 µg of total RNA (10) using the commercially available Whole Human Genome Oligo DNA Microarray kit (Agilent Technologies, Inc., Santa Clara, CA, USA). Cyanine-labeled cRNA was prepared using T7 linear amplification as described in the Agilent Low RNA Input Fluorescent Linear Amplification kit manual (Agilent Technologies, Inc.). Labeled cRNA was then fragmented (with fragmentation buffer from the Agilent Low RNA Input Fluorescent Amplification kit, according to the manufacturer's protocol; Agilent Technologies, Inc.) and hybridized to an oligonucleotide microarray (Whole Human Genome Microarray kit, 4×44K; product no. G4112F; Agilent Technologies, Inc.). Fluorescence intensities were determined with a DNA microarray scanner (G2565BA/DB; Agilent Technologies, Inc.) and analyzed using G2567AA Feature Extraction Software (version A7.5.1; Agilent Technologies, Inc.), which used the locally weighted linear regression curve fit normalization method (11). This microarray study followed Minimum Information About a Microarray Experiment guidelines issued by the Microarray Gene Expression Data group (12). Further analyses were performed using GeneSpring (version 7.3; Agilent Technologies, Inc.). mRNA expression level in cancer tissue by microarray was categorised by the median expression level into high and low expression groups.
Immunohistochemistry
Tumor specimens in cohort 2 were fixed in 10% formalin (Wako Pure Chemical Industries, Ltd., Osaka, Japan) and embedded in paraffin (Wako Pure Chemical Industries, Ltd.). The expression of proteins was evaluated by immunohistochemistry in 4-µm-thick sections following deparaffinization with xylene (Wako Pure Chemical Industries, Ltd.) and dehydration in graded ethanol solutions. For antigen retrieval, the sections were autoclaved in 10 mM citrate buffer (pH 6.0) at 115°C for 20 min. After blocking with hydrogen peroxide (Wako Pure Chemical Industries, Ltd.), the sections were incubated with specific antibodies overnight at 4°C in a moist chamber. Rat monoclonal antibody against HSF1 (10H8; Enzo Life Sciences, Inc., Farmingdale, NY, USA), mouse monoclonal antibody against Hsp27 (G3.1; Enzo Life Sciences, Inc.), mouse monoclonal antibody against Hsp70 (C92F3A-5; Santa Cruz Biotechnology, Inc., Dallas, TX, USA) and mouse monoclonal antibody against Hsp90 (ADI-SPA-830-D; Enzo Life Sciences, Inc.), were used at dilutions of 1:100, 1:1,000, 1:500 and 1:300, respectively. Sites of antibody binding were visualized with the ABC peroxidase detection system according to the manufacturer's protocol (catalog nos., PK-4004 and PK-4010; Vector Laboratories, Inc., Burlingame, CA, USA) using a fluorescence microscope (BZ-X700; Keyence Corporation, Osaka, Japan). The intensity of antibody-stained nuclei in cancer cells was evaluated by two independent pathologists, who were blinded to the clinicopathological parameters. The intensity of HSF1, Hsp27, Hsp70 and Hsp90 immunoreactions in the cells were scored as follows: 0, not stained; 1+, weak staining; 2+, moderate staining; and 3+, intense staining. Finally, the expression of these proteins in ESCC specimens was classified into a HSF1 low expression group (0 or 1+) and a HSF1 high expression group (2+ or 3+).
Statistical analysis
The association between HSF1 protein expression and various clinicopathological factors was analyzed using the χ2 test and Fisher's exact probability test. The overall survival (OS) was assessed by performing the Kaplan-Meier method and compared using the log-rank test. OS was defined as the period from the date of surgery to the date of death from any cause. All parameters with a P<0.10 in univariate analysis by the Cox proportional hazard model were entered into multivariate survival analysis. P<0.05 was considered to indicate a statistically significant difference. Statistical analysis was performed with JMP Pro software (version 10.0.2; SAS Institute, Cary, NC, USA). Each test was repeated six times.
Results
Correlation between HSF1 mRNA expression and clinicopathological characteristics in cohort 1
The 58 ESCC cases were classified into two groups using the median HSF1 mRNA expression level in cancer tissue as determined by microarray. Table I shows the correlation between HSF1 expression and various clinicopathological parameters. No significant association was observed with age, gender, tumor location, histological grade, pathological T (pT) stage or pathological N (pN) stage (P<0.05).
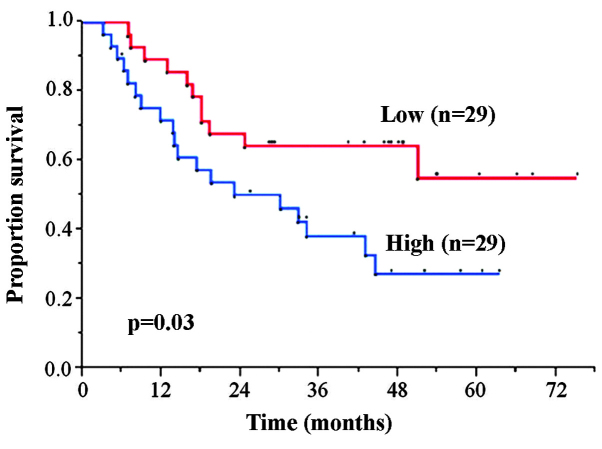
Correlation between HSF1 mRNA expression and OS in cohort 1
The 5-year OS rates in the HSF1 high and low expression groups was 27.3 and 55.1%, respectively. The HSF1 high expression group exhibited significantly worse OS rate compared with the low expression group (P=0.03) (Fig. 1).
Figure 1.
Kaplan-Meier overall survival curves based on the heat-shock factor 1 mRNA expression status of patients with esophageal squamous cell carcinoma in cohort 1.
HSF1 protein expression in cohort 2
A total of 212 cancerous lesion samples were evaluated for HSF1 protein expression by immunohistochemical analysis. Of these, 109 (51.4%) exhibited high HSF1 expression (Table II), predominantly in the nuclei of the tumor cells, with faint cytoplasmic staining (Fig. 2A), while the remaining 103 (48.6%) samples showed low HSF1 expression (Fig. 2B). The staining was almost homogenous among different areas of the cancerous lesions, including the surface, central and deep areas. None of the normal squamous epithelium samples showed significant levels of HSF1 expression, although faint immunostaining was observed in the nuclei of a small number of basal cells (Fig. 2C). Scoring of the immunostained sections was almost identical by the two pathologists, with interobserver variation of <5%.
Figure 2.
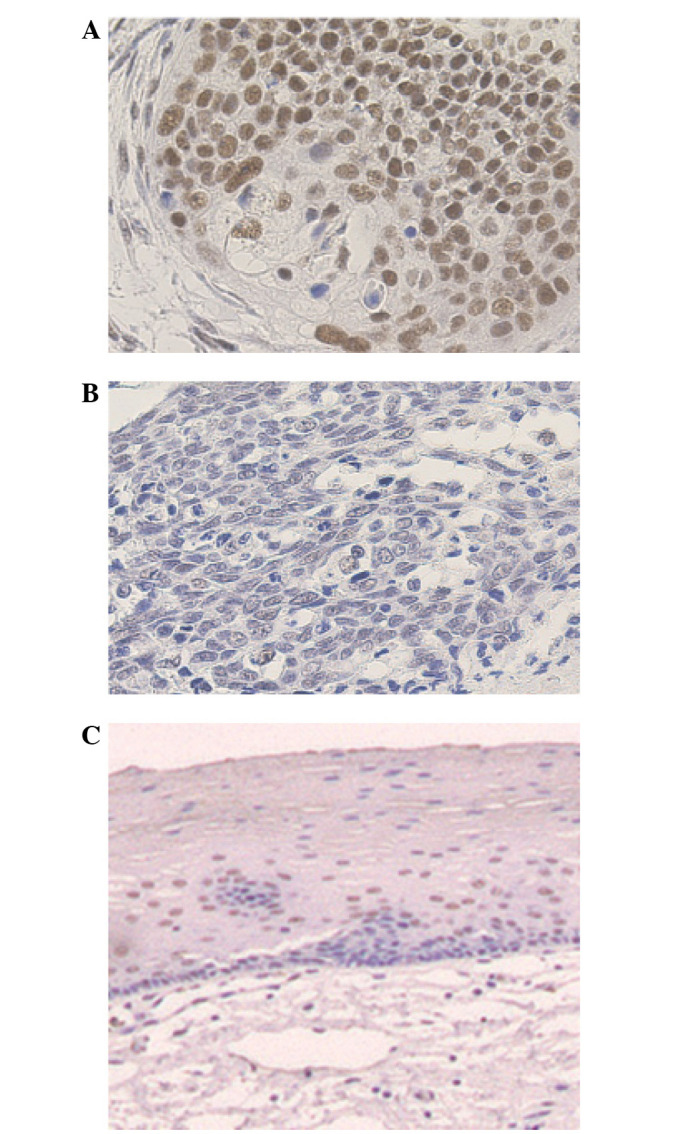
Immunohistochemical staining showing the expression of heat-shock factor 1 (HSF1) in esophageal squamous cell carcinoma (ESCC) tumor samples from cohort 2. Representative images of (A) high HSF1 expression in ESCC, showing staining predominantly in the nuclei of tumor cells (magnification, ×200); (B) low HSF1 expression ESCC, showing almost no appreciable staining of the tumor cells (magnification, ×200); and (C) normal squamous epithelium, which is negative for HSF1 expression except for a few basal cells (magnification, ×100).
Correlation between HSF1 protein expression and clinicopathological parameters in cohort 2
Table II indicates the correlations between HSF1 protein expression and various clinicopathological parameters. In comparison to primary tumors with low HSF1 expression, primary tumors with high HSF1 expression were significantly more likely to be in the upper location (P=0.03). All other parameters, including age, gender, pT, pN, pathological stage and preoperative therapy, did not significantly correlate with HSF1 protein expression.
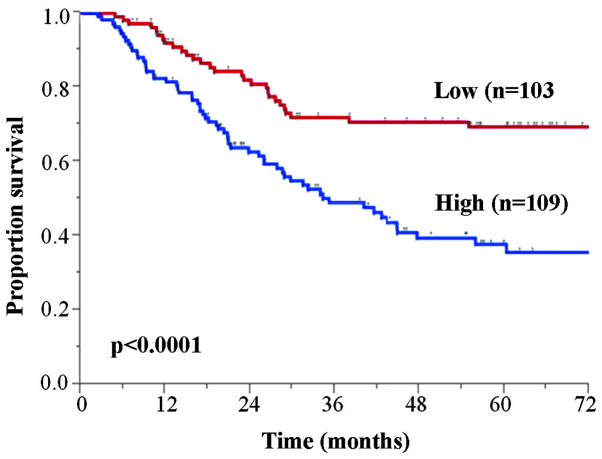
Correlation between HSF1 protein expression and clinical outcome in cohort 2
The 5-year OS rates for patients with low and high HSF1 expression tumors were 69.4 and 37.8%, respectively (Fig. 3). The high HSF1 expression group exhibited significantly poorer OS than those in the low HSF1 expression group (P<0.0001). Furthermore, univariate analysis revealed that the OS significantly correlated with age, pT, pN and HSF1 protein expression (Table III). Multivariate analysis using the five parameters with P<0.10 on univariate analysis identified high HSF1 expression [hazard ratio (HR), 2.29; 95% confidence interval (CI), 1.48–3.64; P=0.0002] as an independent OS prognostic factor, in addition to pT (HR, 2.21; 95% CI, 1.38–3.65; P=0.0008) and pN (HR, 1.73; 95% CI, 1.04–3.02; P=0.03).
Figure 3.
Kaplan-Meier overall survival curves based on the heat-shock factor 1 protein expression status of esophageal squamous cell carcinoma patients in cohort 2.
Table III.
Univariate and multivariate survival analyses of overall survival rate by Cox's proportional hazard model.
| Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|
| Parameter | Patients, n | HR | 95% CI | P-value | HR | 95% CI | P-value |
| Age, years (65≤/≤64) | 106/106 | 1.64 | 1.08–2.50 | 0.02 | 1.51 | 0.99–2.32 | 0.06 |
| Gender (male/female) | 184/28 | 1.36 | 0.74–2.8 | 0.34 | |||
| Histological grade (G1/G2, G3, Gx) | 49/163 | 0.81 | 0.51–1.32 | 0.39 | |||
| Location (Ut, Mt/Lt) | 141/71 | 0.66 | 0.44–1.02 | 0.06 | 1.36 | 0.88–2.07 | 0.16 |
| pT (T3, T4/T1, T2) | 92/120 | 2.66 | 1.69–4.34 | <0.0001 | 2.22 | 1.39–3.65 | 0.0007 |
| pN (N1, N2, N3/N0) | 72/140 | 2.42 | 1.49–4.14 | 0.0002 | 1.76 | 1.06–3.06 | 0.03 |
| Neoadjuvant therapy (none/chemotherapy) | 85/127 | 0.91 | 0.59–1.38 | 0.65 | |||
| HSF1 expression (high/low) | 109/103 | 2.53 | 1.64–4.0 | <0.0001 | 2.24 | 1.44–3.56 | 0.0003 |
HR, hazard ratio; CI, confidence interval; pT/N, pathological T/N; HSF1, heat-shock factor 1; Ut, upper thoracic esophagus; Mt, mid-thoracic esophagus; Lt, lower thoracic esophagus.
Correlation between HSF1 protein expression and expression of Hsps in cohort 2
To determine whether the expression of Hsps correlated with HSF1 tumor expression in ESCC tumor specimens, 55/212 ESCC randomly selected samples in cohort 2 were immunohistochemically evaluated for Hsp27, Hsp70 and Hsp90 expression. High expression of HSF1 and Hsp27 was observed in 24 ESCC samples, 18 samples showed low expression of HSF1 and Hsp27, 7 samples exhibited high expression of HSF1 but low expression of Hsp27, and 6 samples exhibited low HSF1 expression but high Hsp27 expression (Table IV). The results indicate that HSF1 expression is significantly correlated with Hsp27 expression (P<0.0001). Hsp90 expression was also significantly correlated with HSF1 expression (P<0.0001), but Hsp70 expression was not (P=0.38).
Table IV.
Correlation between HSF1, and Hsp27, Hsp70 and Hsp90 expression.
| HSF1 | ||||
|---|---|---|---|---|
| Expression | + | − | Total | P-value |
| Hsp27 | ||||
| + | 24 | 6 | 30 | <0.0001 |
| − | 7 | 18 | 25 | |
| Hsp70 | ||||
| + | 7 | 8 | 15 | 0.38 |
| − | 24 | 16 | 40 | |
| Hsp90 | ||||
| + | 28 | 7 | 35 | <0.0001 |
| − | 3 | 17 | 20 | |
| Total | 31 | 24 | 55 | |
HSF1, heat-shock factor 1; Hsp, heat-shock protein.
These results indicate that the expression of HSF1 is closely correlated with poor prognosis in ESCC. The results also indicate that Hsp27 and Hsp90 expression, but not Hsp70 expression, are possible downstream targets of HSF1 in ESCC.
Thus, the correlation between the Hsp27, Hsp70 and Hsp90 expression, and OS were investigated. The high Hsp27 and Hsp90 expression groups showed significantly poorer OS compared with those in the low Hsp27 and Hsp90 expression groups (P=0.04 and P=0.03, respectively) (Fig. 4A and B, respectively), while there were no significant differences in OS between high and low Hsp70 expression (P=0.91) (Fig. 4C).
Figure 4.
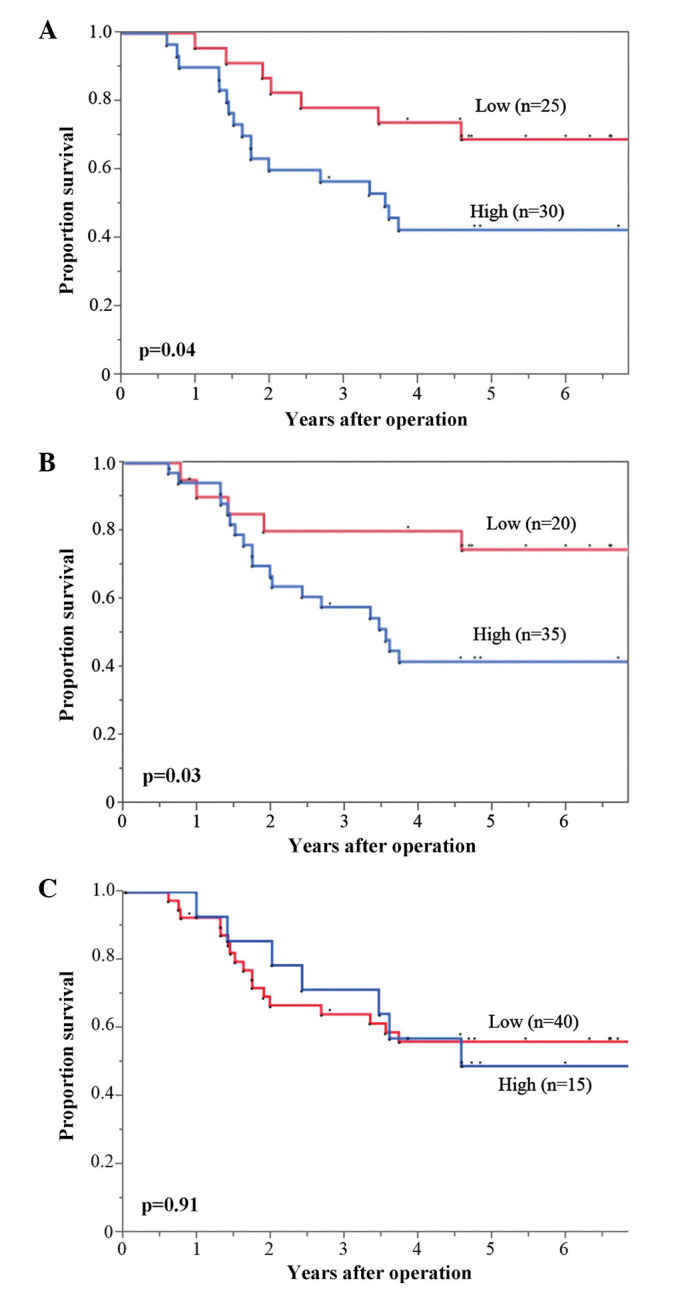
Overall survival curves based on (A) heat-shock protein 27 (Hsp27), (B) Hsp90 and (C) Hsp70 expression status of patients with esophageal squamous cell carcinoma.
Discussion
Hsps are overexpressed in numerous types of cancer (including hepatocellular carcinoma, colorectal carcinoma, bladder cancer and neuroblastoma), and are correlated with tumor proliferation, invasion and metastasis (13,14). Various studies report that Hsp levels are useful biomarkers of carcinogenesis and aggressiveness in specific types of cancer, including hepatocellular carcinoma, colorectal carcinoma, breast cancer, primary oral squamous cell carcinoma and gastric adenocarcinoma (15–18). Hsp expression is regulated by HSF1, which can bind to the 5′ promoter regions of all Hsp genes, and trigger their immediate and massive transcription (19,20). HSF1 expression itself is also involved in numerous crucial steps of carcinogenesis and tumor development (7). Its expression is closely correlated with invasion, metastasis and angiogenesis (21,22), and has been identified as a prognostic factor in breast cancer and hepatocellular carcinoma.
The present study demonstrated that high HSF1 expression is associated with poor prognosis in two independent patient cohorts, and appears to be an independent prognostic factor for patients undergoing curative resection for ESCC. The prediction of prognosis following curative surgical resection will enable clinicians to determine the necessity for intensive follow-up and adjuvant therapy (23,24). Furthermore, if HSF1 expression can be measured in pretreated biopsy samples it may yield useful information for determining the treatment strategy for individual patients.
Additionally, the present study revealed that the expression of Hsp27 and Hsp90 are closely correlated with HSF1 expression in ESCC tumor specimens. This suggests that the HSF1/Hsp27 and HSF1/Hsp90 pathways may be involved in the progression of ESCC. A number of studies previously reported that Hsp27 and Hsp90 were associated with survival and could be potential molecular targets in various types of cancer (23,25–29).
Recently, Hsp90 inhibitors have been developed, and used as preclinical and clinical anticancer therapies (30,31). The present study indicates that Hsp27 and Hsp90 may be potential therapeutic targets in patients with ESCC, as HSF1 is a regulator of Hsps. Therefore, inhibiting HSF leads to inhibition of not only Hsp27, but also Hsp90. However, the results suggest that HSF1, which regulates the transcription of Hsp27 and Hsp90, may be a more effective and stronger therapeutic target. HSF1 may, therefore, be a valid prognostic marker in ESCC and a candidate for novel approaches to ESCC treatment.
Prospective studies are required to further clarify the significance of HSF1 in the clinical setting. Additionally, it will be important to investigate the molecular mechanisms underlying the effect of HSF1 expression on prognosis. The present findings may mark a new step for the exploration of appropriate treatment strategies and the development of novel therapeutic approaches for ESCC.
In conclusion, the results of the present study indicate that HSF1 is a prognostic factor for patients with ESCC, and that Hsp27 and Hsp90, but not Hsp70, may be the downstream targets of HSF1 in ESCC.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Fujita H. The history of lymphadenectomy for esophageal cancer and the future prospects for esophageal cancer surgery. Surg Today. 2015;45:140–149. doi: 10.1007/s00595-014-0841-4. [DOI] [PubMed] [Google Scholar]
- 3.Sobin LH, Gospodarowicz MK, Wittekind Ch, editors. TNM Classification of Malignant Tumors. 7th. Wiley-Blackwell; Oxford: 2009. Oesophagus including oesophagogastric junction; pp. 65–72. [Google Scholar]
- 4.Sorger PK. Heat shock factor and the heat shock response. Cell. 1991;65:363–366. doi: 10.1016/0092-8674(91)90452-5. [DOI] [PubMed] [Google Scholar]
- 5.Qian SB, McDonough H, Boellmann F, Cyr DM, Patterson C. CHIP-mediated stress recovery by sequential ubiquitination of substrates and Hsp70. Nature. 2006;440:551–555. doi: 10.1038/nature04600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page TJ, Sikder D, Yang L, Pluta L, Wolfinger RD, Kodadek T, Thomas RS. Genome-wide analysis of human HSF1 signaling reveals a transcriptional program linked to cellular adaptation and survival. Mol Biosyst. 2006;2:627–639. doi: 10.1039/b606129j. [DOI] [PubMed] [Google Scholar]
- 7.Dai C, Whitesell L, Rogers AB, Lindquist S. Heat shock factor 1 is a powerful multifaceted modifier of carcinogenesis. Cell. 2007;130:1005–1018. doi: 10.1016/j.cell.2007.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li S, Ma W, Fei T, Lou Q, Zhang Y, Cui X, Qin X, Zhang J, Liu G, Dong Z, et al. Upregulation of heat shock factor 1 transcription activity is associated with hepatocellular carcinoma progression. Mol Med Rep. 2014;10:2313–2321. doi: 10.3892/mmr.2014.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santagata S, Hu R, Lin NU, Mendillo ML, Collins LC, Hankinson SE, Schnitt SJ, Whitesell L, Tamimi RM, Lindquist S, Ince TA. High levels of nuclear heat-shock factor 1 (HSF1) are associated with poor prognosis in breast cancer. Proc Natl Acad Sci USA. 2011;108:18378–18383. doi: 10.1073/pnas.1115031108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enders GH. Cyclins in breast cancer: Too much of a good thing. Breast Cancer Res. 2002;4:145–147. doi: 10.1186/bcr439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quackenbush J. Microarray data normalization and transformation. Nat Genet. 2002;32:S496–S501. doi: 10.1038/ng1032. (Suppl) [DOI] [PubMed] [Google Scholar]
- 12.Brazma A, Hingamp P, Quackenbush J, Sherlock G, Spellman P, Stoeckert C, Aach J, Ansorge W, Ball CA, Causton HC, et al. Minimum information about a microarray experiment (MIAME)-toward standards for microarray data. Nat Genet. 2001;29:365–371. doi: 10.1038/ng1201-365. [DOI] [PubMed] [Google Scholar]
- 13.Khalil AA, Kabapy NF, Deraz SF, Smith C. Heat shock proteins in oncology: Diagnostic biomarkers or therapeutic targets? Biochim Biophys Acta. 2011;1816:89–104. doi: 10.1016/j.bbcan.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Ciocca DR, Calderwood SK. Heat shock proteins in cancer: Diagnostic, prognostic, predictive and treatment implications. Cell Stress Chaperones. 2005;10:86–103. doi: 10.1379/CSC-99r.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaigorodova EV, Bogatyuk MV. Heat shock proteins as prognostic markers of cancer. Curr Cancer Drug Targets. 2014;14:713–726. doi: 10.2174/1568009614666140926122846. [DOI] [PubMed] [Google Scholar]
- 16.Ciocca DR, Vargas-Roig LM. Hsp27 as a prognostic and predictive factor in cancer. Prog Mol Subcell Biol. 2002;28:205–218. doi: 10.1007/978-3-642-56348-5_11. [DOI] [PubMed] [Google Scholar]
- 17.Kim KK, Jang TJ, Kim JR. HSP70 and ER expression in cervical intraepithelial neoplasia and cervical cancer. J Korean Med Sci. 1998;13:383–388. doi: 10.3346/jkms.1998.13.4.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chuma M, Sakamoto M, Yamazaki K, Ohta T, Ohki M, Asaka M, Hirohashi S. Expression profiling in multistage hepatocarcinogenesis: Identification of HSP70 as a molecular marker of early hepatocellular carcinoma. Hepatology. 2003;37:198–207. doi: 10.1053/jhep.2003.50022. [DOI] [PubMed] [Google Scholar]
- 19.Wu C. Heat shock transcription factors: Structure and regulation. Annu Rev Cell Dev Biol. 1995;11:441–469. doi: 10.1146/annurev.cellbio.11.1.441. [DOI] [PubMed] [Google Scholar]
- 20.Calderwood SK, Xie Y, Wang X, Khaleque MA, Chou SD, Murshid A, Prince T, Zhang Y. Signal transduction pathways leading to heat shock transcription. Sign Transduct Insights. 2010;2:13–24. doi: 10.4137/STI.S3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khaleque MA, Bharti A, Gong J, Gray PJ, Sachdev V, Ciocca DR, Stati A, Fanelli M, Calderwood SK. Heat shock factor 1 represses estrogen-dependent transcription through association with MTA1. Oncogene. 2008;27:1886–1893. doi: 10.1038/sj.onc.1210834. [DOI] [PubMed] [Google Scholar]
- 22.Gabai VL, Meng L, Kim G, Mills TA, Benjamin IJ, Sherman MY. Heat shock transcription factor Hsf1 is involved in tumor progression via regulation of hypoxia-inducible factor 1 and RNA-binding protein HuR. Mol Cell Biol. 2012;32:929–940. doi: 10.1128/MCB.05921-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyu X, Huang J, Mao Y, Liu Y, Feng Q, Shao K, Gao S, Jiang Y, Wang J, He J. Adjuvant chemotherapy after esophagectomy: Is there a role in the treatment of the lymph node positive thoracic esophageal squamous cell carcinoma? J Surg Oncol. 2014;110:864–868. doi: 10.1002/jso.23716. [DOI] [PubMed] [Google Scholar]
- 24.Ruiz MI Gallegos, Floor K, Roepman P, Rodriguez JA, Meijer GA, Mooi WJ, Jassem E, Niklinski J, Muley T, van Zandwijk N, et al. Integration of gene dosage and gene expression in non-small cell lung cancer, identification of HSP90 as potential target. PLoS One. 2008;3:e0001722. doi: 10.1371/journal.pone.0001722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakamura M, Iwahashi M, Nakamori M, Ojima T, Katsuda M, Iida T, Hayata K, Kato T, Yamaue H. New prognostic score for the survival of patients with esophageal squamous cell carcinoma. Surg Today. 2014;44:875–883. doi: 10.1007/s00595-013-0628-z. [DOI] [PubMed] [Google Scholar]
- 26.Pick E, Kluger Y, Giltnane JM, Moeder C, Camp RL, Rimm DL, Kluger HM. High HSP90 expression is associated with decreased survival in breast cancer. Cancer Res. 2007;67:2932–2937. doi: 10.1158/0008-5472.CAN-06-4511. [DOI] [PubMed] [Google Scholar]
- 27.Solit DB, Scher HI, Rosen N. Hsp90 as a therapeutic target in prostate cancer. Semin Oncol. 2003;30:709–716. doi: 10.1016/S0093-7754(03)00346-4. [DOI] [PubMed] [Google Scholar]
- 28.Romani AA, Crafa P, Desenzani S, Graiani G, Lagrasta C, Sianesi M, Soliani P, Borghetti AF. The expression of HSP27 is associated with poor clinical outcome in intrahepatic cholangiocarcinoma. BMC Cancer. 2007;7:232. doi: 10.1186/1471-2407-7-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bauer K, Nitsche U, Slotta-Huspenina J, Drecoll E, von Weyhern CH, Rosenberg R, Höfler H, Langer R. High HSP27 and HSP70 expression levels are independent adverse prognostic factors in primary resected colon cancer. Cell Oncol (Dordr) 2012;35:197–205. doi: 10.1007/s13402-012-0079-3. [DOI] [PubMed] [Google Scholar]
- 30.Smyth T, Van Looy T, Curry JE, Rodriguez-Lopez AM, Wozniak A, Zhu M, Donsky R, Morgan JG, Mayeda M, Fletcher JA, et al. The HSP90 inhibitor, AT13387, is effective against imatinib-sensitive and -resistant gastrointestinal stromal tumor models. Mot Cancer Ther. 2012;11:1799–1808. doi: 10.1158/1535-7163.MCT-11-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagner AJ, Agulnik M, Heinrich MC, Mahadevan D, Riedel RF, von Mehren M, Trent J, Demetri GD, Corless CL, Yule M. Dose-escalation study of a second-generation non-ansamycin HSP90 inhibitor, onalespib (AT13387), in combination with imatinib in patients with metastatic gastrointestinal stromal tumour. Eur J Cancer. 2016;61:94–101. doi: 10.1016/j.ejca.2016.03.076. [DOI] [PubMed] [Google Scholar]