Abstract
Background
Clinical care for children and adults living with sickle cell disease (SCD) is often provided in the emergency department (ED). Population-based surveillance data can be used to describe the ED utilization patterns of this patient population.
Procedure
A cohort of pediatric and adult California patients with SCD was identified from multiple data sources, and 10 years (2005–2014) of their treat-and-release ED utilization data were analyzed.
Results
Among a cohort of 4,636 patients with SCD, 4,100 (88%) had one or more treat-and-release ED visits. There were 2.1 mean annual visits per person for the cohort (median 0.7; range 0–185). In a single year (2005), 53% had 0 treat-and-release ED visits, 35% had 1–3 visits, 9% had 4–10 visits, and 3% had 11 or more visits; this highest utilization group accounted for 45% of all patients’ ED visits. ED utilization in this cohort was highest among young adults and also higher among older adults than pediatric patients.
Conclusion
The majority of identified patients in each of the 10 years did not go to the ED, but nearly all had one or more such visits over the full span of time. This study highlights the power and utility of a multisource longitudinal data collection effort for SCD. Further study of the segment of the population with highest ED utilization may highlight areas where changes in health-care and health policy could improve and extend the lives of patients with SCD.
Keywords: emergency department, healthcare utilization, sickle cell disease
1 | INTRODUCTION
Sickle cell disease (SCD) affects 70,000–100,000 individuals in the United States.1,2 The acute painful vaso occlusive events that are the hallmark of SCD, along with other clinical manifestations of the disease, may result in visits to the emergency department (ED) when the events cannot be successfully managed at home or during an outpatient visit.3 Frequency of ED visits may also be associated with factors related to the healthcare system, such as lack of access to care, few or no SCD clinical care experts located nearby, or inadequate coverage for the payment of medical services.4–6 Between 47% and 67% of patients’ ED visits end in a discharge, termed as a treat-and-release visit; the remainder result in an inpatient admission to a hospital or other treatment facility.7,8
The information that is currently available about ED visits by patients with SCD is the result of analyses of data from either a single clinical institution or a consortium of institutions, or from a dataset based on a single source of administrative data (i.e., hospital discharge or Medicaid). Each type of data source has advantages and disadvantages for these types of epidemiologic studies. Clinical centers can accurately identify patients with laboratory-confirmed SCD and have access to detailed medical information about them, although drawing additional information from clinical electronic health records may be challenging. Further, even in regions with excellent clinical care centers, a sizeable portion of patients with SCD receive care in other settings. Therefore, data from clinical care centers alone may not accurately reflect the general SCD population. By contrast, administrative data rely on International Classification of Disease (ICD) codes to identify patients with SCD. Administrative data allow for the inclusion of a larger number of patients, including those who receive care outside of SCD clinical centers, but the correlation between SCD ICD codes and laboratory-confirmed diagnosis of SCD has been demonstrated to be unsatisfactory.9–11
These limitations were among the factors that led to the development of the Registry and Surveillance System for Hemoglobinopathies (RuSH) project and the subsequent Public Health Research, Epidemiology, and Surveillance for Hemoglobinopathies (PHRESH; www.cdc.gov/ncbddd/hemoglobinopathies/phresh.html) project.12 These programs were designed to conduct statewide public health surveillance for children and adults with SCD. Following on these efforts, the current Sickle Cell Data Collection (SCDC; http://www.cdc.gov/ncbddd/hemoglobinopathies/scdc.html) Program was developed to continue and expand state-based SCD surveillance. These programs have resulted in the identification of pediatric and adult patients with SCD and description of their healthcare utilization patterns, including utilization of the ED. The objectives of this descriptive analysis were to use these longitudinal data to: (i) describe California’s SCD population’s utilization of the ED for treat-and-release visits and (ii) compare and contrast these results with previous publications that were based on single-source administrative data.3,8,13
2 | METHODS
Data were collected for the years 2004–2008 from newborn screening, hospital inpatient discharge, ED treat-and-release visits, Medicaid, and vital records files as well as case reports from six SCD clinical centers of care. Once patients with SCD were identified in one or more of these datasets, their data from all sources were linked using social security numbers (SSN) and date of birth (DOB). Probabilistic linking methods using variables such as diagnosis, DOB, sex, and facility were used to determine the correct SSN for those identified through newborn screening or who were reported without an SSN by clinics. The data collection and linkage details and methods used are described in detail in a prior publication.14
Only patients with complete and consistent SSN and DOB were used in the present analyses. Furthermore, patients were included only if they met one of these criteria: (i) a laboratory-confirmed SCD diagnosis from newborn screening or one of the six SCD clinical centers (“confirmed”) or (ii) three or more separate clinical encounters during 2004–2008 with an SCD ICD 9 code (282.41, 282.42, 282.6, 282.60, 282.61, 282.62, 282.63, 282.64, 282.68, 282.69; “probable”). This cohort of patients with SCD was then linked (using SSN and DOB) to hospital discharge and ED data for subsequent years 2009–2014, providing a total of 10 years of ED data (2005–2014; ED data were not collected by the state prior to 2005). The inclusion criteria for those patients identified only in administrative data (“probable”) as well as data linking methodologies were previously validated in reports by other RuSH researchers.14,15 Demographics and other characteristics of this cohort have been described previously.12,14
The analyses presented here include treat-and-release ED visits only, except where noted. Mean and median annual rates of utilization across multiple years were calculated using the number of ED visits and person years for the subgroup of interest (e.g., 10-year age group, sex). Person years were calculated based on an entrance to the study on January 1, 2005, or DOB if later, and study exit on December 31, 2014, or date of death if prior. Deaths were identified using hospital and ED “disposition” codes only, with the date of death recorded as the last date of service in the record. If there was subsequent care utilization by a patient, the disposition code indicating death was assumed to be erroneous and was ignored. The utilization of person years was necessary in order to accurately calculate mean and median annual rates.
A separate analysis examined treat-and-release ED visits in index year 2005 only, the year most likely to have complete data and that allowed for the comparison of utilization patterns in subsequent years. Furthermore, 2005 was the earliest year California released ED data, and the closest in time to two of the studies previously published and used here for comparison. Patients with SCD who were born in 2005 or later and those who died in 2005 were excluded from this single-year analysis.
The RuSH and PHRESH projects were declared exempt from review by the California Committee for the Protection of Human Subjects as public health surveillance and the SCDC project protocol was approved by the committee, and each project protocol was reviewed and approved or exempted as public health surveillance by the institutional review boards at the clinical centers that reported data. The use of state administrative, newborn screening, and Medicaid claims data was also approved by the privacy committee at each agency.
3 | RESULTS
There were 4,636 patients with SCD identified in California during 2004–2008 who met the inclusion criteria for this study (Table 1). SCD genotype was known for 1,624 (35%) of these patients (“confirmed”) via laboratory results from an SCD clinical center and/or newborn screening results. The remaining 3,012 patients were found in the administrative data sources (“probable”) and SCD genotype was unknown. The cohort of 4,636 patients contributed a total of 43,416.5 person years, an average of 9.4 years per person between 2005, when ED data collection began, and 2014, the most recent year of data. There were 4,328 (93%) patients in this cohort with one or more encounters (for any diagnosis) in the hospital discharge and/or ED data during the years 2005–2014, and 4,100 (88%) had one or more treat-and-release ED visits during that period. This group of 4,100 had 90,904 treat-and-release ED visits (with or without an SCD diagnosis code), which are the focus of these analyses. Patients under the age of 20 and the oldest patients with SCD were less likely to receive treat-and-release care in the ED compared to patients aged 20–79 at the time of visit (77% vs. 93%). The greatest change in mean annual ED visits across consecutive age groups was an increase from 0.9 visits for the 10- to 19.9-year-olds to 2.8 visits among the 20- to 29.9-year-olds, a threefold increase, and median utilization doubled across these two age groups.
TABLE 1.
Description of individuals with sickle cell disease (SCD) and their treat-and-release emergency department (ED) utilization, California, 2005–2014
| Individuals with SCD | Individuals with SCD and at least 1 treat-and-release ED visit, 2005–2014 | |||||
|---|---|---|---|---|---|---|
| N | N | Row (%) | Mean annual visits | Median annual visits | Range of annual visits | |
| Total | 4,636 | 4,100 | 88 | 2.1 | 0.7 | 0–185 |
| Sex | ||||||
| Female | 2,564 | 2,300 | 90 | 2.3 | 0.8 | 0–171 |
| Male | 2,072 | 1,800 | 87 | 1.9 | 0.6 | 0–185 |
| Age at the close of 2014, years | ||||||
| 0–9.9 | 299 | 203 | 68 | 0.7 | 0.3 | 0–15 |
| 10–19.9 | 930 | 746 | 80 | 0.9 | 0.4 | 0–46 |
| 20–29.9 | 1,045 | 961 | 92 | 2.8 | 0.9 | 0–179 |
| 30–39.9 | 853 | 806 | 94 | 3.4 | 0.9 | 0–161 |
| 40–49.9 | 624 | 583 | 93 | 3.1 | 0.8 | 0–185 |
| 50–59.9 | 544 | 499 | 92 | 2.8 | 0.6 | 0–182 |
| 60–69.9 | 241 | 221 | 92 | 2.1 | 0.5 | 0–91 |
| 70–79.9 | 67 | 57 | 85 | 1.1 | 0.3 | 0–8 |
| 80 and older | 33 | 24 | 73 | 0.5 | 0.0 | 0–3 |
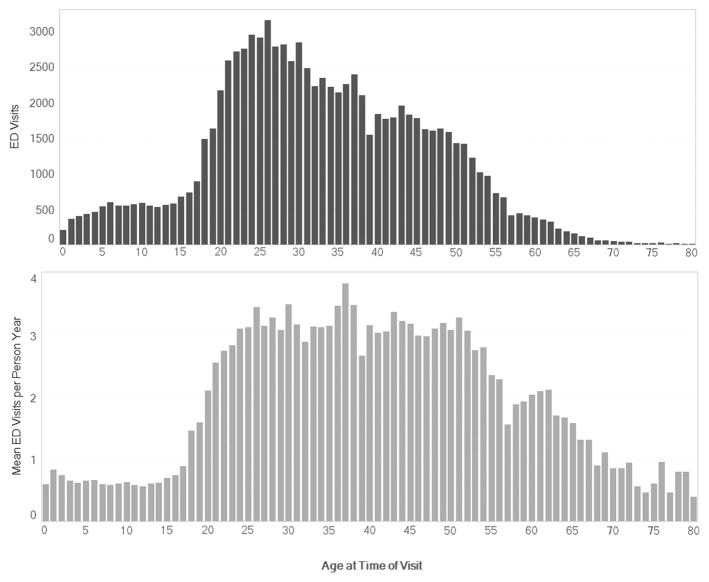
Figure 1 depicts the change in ED utilization by age; the upper, dark gray histogram shows the total count of ED treat-and-release visits during 2005–2014 for each 1-year increment of age. The bottom, light gray histogram shows the mean number of annual ED treat-and-release visits per person for the same time period. For instance, during the 10-year study period, there were 599 treat-and-release ED visits, with an annual mean of 0.7 visits, by children with SCD who were 6 years of age at the time of their visit. By contrast, there were a total of 2,583 such visits by those with SCD who were 21-year-old at the time of visit, with an annual mean of 2.6 visits. The mean annual number of visits showed a consistent pattern of ED utilization across age groups from early adulthood to the late 50s in comparison to the count of visits by age, which showed a sharp increase in early adulthood followed by a steady decline over older age groups. The number of patients with SCD and ED treat-and-release visits over the age of 80 was very small, making interpretation of mean annual visits difficult in graphic form; the figure therefore includes data from individuals aged 80 and younger only.
FIGURE 1.
Comparison of total treat-and-release emergency department utilization and mean annual emergency department utilization for individuals with sickle cell disease, by age at the time of visit (0–80 years of age), California, 2005–2014
The data from this study were compared using matching age groups to earlier published work describing ED treat-and-release utilization for SCD (Table 2). Compared to Epstein, the California data showed similar utilization in the 20- to 30-year and 41- to 50-year age groups, but lower in the 31- to 40-year age group and higher in the oldest age group.7 California data showed markedly higher utilization among those aged 18 and older compared to Brousseau.8 When 2005 ED treat-and-release utilization data were compared to Shankar’s prior work, results were similar.13
TABLE 2.
Comparison of mean annual treat-and-release emergency department (ED) visits for individuals with sickle cell disease (SCD) (California, 2005–2014) to previously published SCD ED utilization reports
| Epstein7 | Previous estimates Mean annual visits (1997–2001) |
California Mean annual visits (2005–2014) |
|---|---|---|
| 20–30 years | 2.9 | 3.3 |
| 31–40 years | 8.5 | 3.8 |
| 41–50 years | 4.3 | 3.8 |
| 51 years and older | 1.0 | 2.5 |
| Brousseau8 | Mean annual visits (2005–2006) | Mean annual visits (2005–2014) |
| 1–9 years | 0.6 | 0.5 |
| 10–17 years | 0.7 | 0.8 |
| 18–30 years | 1.6 | 3.0 |
| 31–45 years | 1.3 | 3.7 |
| 46–64 years | 0.9 | 3.2 |
| 65 years and older | 0.3 | 1.1 |
| Shankar13 | Proportion (1995–2002) | Proportion (2005 only) |
| 0 visits per year (all ages) | 50–60% | 53% |
| 1 visit per year (all ages) | 15–25% | 19% |
| 2 or more visits per year (all ages) | 8–32% | 28% |
The proportion of patients with an ED treat-and-release visit in 2005 was calculated across four frequency-of-visit categories: none (0 visits), low (1–3 visits), medium (4–10 visits), and high (11 or more visits) (Table 3). These proportions were very similar in subsequent years, with less than 2% variation across categories of utilization by year. Chi-square tests of observed (individual years) versus expected (sum of all 10 years) distribution across no, low, medium, and high utilization categories were not statistically significant, with all P values >0.8.
TABLE 3.
Treat-and-release emergency department (ED) visits for individuals with sickle cell disease (SCD) by sex and age, California, 2005
| Patients, n (row, %) | ||||
|---|---|---|---|---|
| 0 visits | 1–3 visits | 4–10 visits | 11 or more visits | |
| Total (n = 4,297) | 2,275 (53) | 1,499 (35) | 401 (9) | 122 (3) |
| Sex | ||||
| Female (n = 2,409) | 1,230 (51) | 877 (36) | 227 (9) | 75 (3) |
| Male (n = 1,888) | 1,045 (55) | 622 (33) | 174 (9) | 47 (2) |
| Age at the close of 2005, years | ||||
| 0–9.9 (n = 841) | 540 (64) | 255 (30) | 45 (5) | 1 (<1) |
| 10–19.9 (n = 1,028) | 648 (63) | 335 (33) | 43 (4) | 2 (<1) |
| 20–29.9 (n = 881) | 391 (44) | 315 (36) | 133 (15) | 42 (5) |
| 30–39.9 (n = 630) | 263 (42) | 256 (41) | 84 (13) | 27 (4) |
| 40–49.9 (n = 553) | 254 (46) | 198 (36) | 65 (12) | 36 (7) |
| 50–59.9 (n = 260) | 122 (47) | 99 (38) | 28 (11) | 11 (4) |
| 60–69.9 (n = 70) | 37 (53) | 29 (41) | 1 (1) | 3 (4) |
| 70–79.9 (n = 24) | 15 (63) | 7 (29) | 2 (8) | 0 (0) |
| 80 and older (n = 10) | 5 (50) | 5 (50) | 0 (0) | 0 (0) |
Total row percentage may not equal 100, due to rounding.
4 | DISCUSSION
Tracking a population-based cohort of patients living with SCD in California over a 10-year period offers a unique perspective on patterns of ED utilization. While the exact number of patients living with SCD in the state is not currently known, these analyses provide information on over 70% of the total number estimated by previous studies.1,2 Nearly half of the identified population living with SCD had one or more treat-and-release visits in any given year, and 88% had one or more such visits during the 10-year period. As other research has shown, the total number of ED visits was highest among young adults. These analyses show that when normalized for person years and diminished denominator in older age groups, mean number of visits per year was high among those up to age 60 as well.
Previous studies found that 47–67% of ED visits among those with SCD were treat-and-release.7,8 The analyses described here yielded similar results: 66% of ED visits were treat-and-release. The dramatic rise in ED visits during the young adult period is also consistent with the trends of increased utilization during this age, which have been described by others.6,8 In comparison to previous publications that have reported mean annual ED treat-and-release visits ranging from as few as 1.1 visits to as many as 4.9 visits, these data show an average of 2.1 ED treat-and-release visits per year for all included patients with SCD.7,8,16
Finally, while treat-and-release ED utilization is high among this group of patients with SCD overall, these data yielded a small number of individuals (3%) in any given year who were very high utilizers. In 2005, this group comprised just 122 patients. More analyses of these very high utilizers are currently underway, including descriptions of periods of very high utilization versus lower utilization within individuals, and triggers or risk factors for high utilization episodes.
This study highlights the power and utility of a multisource longitudinal data collection effort for SCD. Individuals described here were identified using population-based surveillance methods, rather than relying on data from a small number of clinical institutions or from a single administrative dataset. This method of patient identification and tracking, along with the inclusion criteria that were employed, ensured that these analyses included patients with SCD who spanned the spectrum of disease severity. The difference in data sources and breadth of data collection may explain some of the differences between mean annual number of visits in this study and those reported by others. For example, a study that identifies patients with SCD using ICD-9-CM codes in a single-source dataset3,5,8,11,13,16–21 may include an excess number of individuals without a true SCD diagnosis, as the code could have been used to indicate a rule-out diagnosis or may be the result of miscoding.9 Such an error would increase the total number of patients with SCD (denominator), resulting in a lower mean number of visits. Alternatively, a study that collects information from an SCD specialty clinic or clinics may contain a greater number of patients with severe illness and consequently, greater ED utilization than the general SCD population.4,7,22
There are limitations to this work. Because this was a closed cohort with no new patients born or identified after 2008, most of the patients were aged 10 or older by the close of 2014. The count of ED visits for those in the youngest decade age group will therefore be low, although the normalized mean number of visits per year by age at the time of visit will not be biased. The study included data for ED visits that took place in California only and may not be generalizable to other states. If the patients with SCD were cared for in locations outside of the state, either due to travel or a permanent move, the data were not available for these analyses. Loss to follow-up, either due to a patient moving to another state or death outside of the ED or hospital, could not be determined using these data, so the inclusion of all known patients with SCD for the full 10 years may underestimate ED utilization by inflating the denominator person years. Although 70% of the estimated cases in California are included here, our cohort is not complete. Patients included in this cohort are only those for whom complete, reliable data with SSN and DOB were available, and this may bias results toward those more severely affected with SCD, as they are likely to appear more often in the data. Additionally, the SCD genotype for a large number of patients was unknown and confounded by age in this cohort (the majority of patients with known genotype were under age 20); therefore, subanalyses by genotype were not included. Further analyses of these data to identify risk factors associated with very frequent ED utilization are planned.
These data indicate that most identified SCD patients had at least one treat-and-release visit over the 10-year study period, and nearly half have one or more such visits in any given year. Treat-and-release ED utilization among patients with SCD is highest among young and middle-aged adults. They also show that a substantial portion of those living with this disease do not have such visits in a single year. The similarities and differences among the analyses of these data and related prior publications highlight the importance of a population-based data collection system that captures information on healthcare utilization, access to care, and health outcomes for all patients with SCD.
Acknowledgments
Grant sponsor: Pfizer, Inc.; Grant sponsor: Biogen; Grant sponsor: CDC Foundation.
This work was supported by funding from Pfizer Inc., Biogen, and the CDC Foundation. The authors wish to thank the staff from Children’s Hospital Los Angeles, University of California (UC) San Francisco Benioff Children’s Hospital Oakland, UC San Francisco Medical Center, UC San Diego Rady Medical Center, UC Davis Medical Center, and UC Irvine Medical Center for their contributions to the data collection effort of these projects. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
Abbreviations
- ED
emergency department
- ICD
International Classification of Disease
- PHRESH
Public Health Research, Surveillance, and Epidemiology for Hemoglobinopathies
- RuSH
Registry and Surveillance System for Hemoglobinopathies
- SCD
sickle cell disease
- SCDC
Sickle Cell Data Collection Program
- SSN
social security number
Footnotes
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
References
- 1.Brousseau DC, Panepinto JA, Nimmer M, et al. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hematol. 2010;85(1):77–78. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 2.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38(4 Suppl):S512–S521. doi: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Blinder MA, Duh MS, Sasane M, et al. Age-related emergency department reliance in patients with sickle cell disease. J Emerg Med. 2015;49(4):513–522. doi: 10.1016/j.jemermed.2014.12.080. [DOI] [PubMed] [Google Scholar]
- 4.Hand R, Koshy M, Dorn L, et al. Health insurance status and the use of emergency and other outpatient services by adults with sickle cell disease. Ann Emerg Med. 1995;25(2):224–229. doi: 10.1016/s0196-0644(95)70328-4. [DOI] [PubMed] [Google Scholar]
- 5.Hemker BG, Brousseau DC, Yan K, et al. When children with sickle-cell disease become adults: lack of outpatient care leads to increased use of the emergency department. Am J Hematol. 2011;86(10):863–865. doi: 10.1002/ajh.22106. [DOI] [PubMed] [Google Scholar]
- 6.Panepinto JA, Owens PL, Mosso AL, et al. Concentration of hospital care for acute sickle cell disease-related visits. Pediatr Blood Cancer. 2012;59(4):685–689. doi: 10.1002/pbc.24028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epstein K, Yuen E, Riggio JM, et al. Utilization of the office, hospital and emergency department for adult sickle cell patients: a five-year study. J Natl Med Assoc. 2006;98(7):1109–1113. [PMC free article] [PubMed] [Google Scholar]
- 8.Brousseau DC, Owens PL, Mosso AL, et al. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 9.Grosse SD, Boulet SL, Amendah DD, et al. Administrative data sets and health services research on hemoglobinopathies: a review of the literature. Am J Prev Med. 2010;38(4 Suppl):S557–S567. doi: 10.1016/j.amepre.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Reeves S, Garcia E, Kleyn M, et al. Identifying sickle cell disease cases using administrative claims. Acad Pediatr. 2014;14(5 Suppl):S61–S67. doi: 10.1016/j.acap.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Claster S, Termuhlen A, Schrager SM, et al. Pitfalls of using administrative data sets to describe clinical outcomes in sickle cell disease. Pediatr Blood Cancer. 2013;60(12):1936–1939. doi: 10.1002/pbc.24747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hulihan MM, Feuchtbaum L, Jordan L, et al. State-based surveillance for selected hemoglobinopathies. Genet Med. 2015;17(2):125–130. doi: 10.1038/gim.2014.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shankar SM, Arbogast PG, Mitchel E, et al. Medical care utilization and mortality in sickle cell disease: a population-based study. Am J Hematol. 2005;80(4):262–270. doi: 10.1002/ajh.20485. [DOI] [PubMed] [Google Scholar]
- 14.Paulukonis ST, Harris WT, Coates TD, et al. Population based surveillance in sickle cell disease: methods, findings and implications from the California Registry and Surveillance System in Hemoglobinopathies project (RuSH) Pediatr Blood Cancer. 2014;61(12):2271–2276. doi: 10.1002/pbc.25208. [DOI] [PubMed] [Google Scholar]
- 15.Lane PA, Theodore R, Zhou M, et al. Accuracy of ICD-9 coding for sickle cell disease (SCD) in children and adolescents: results from the Georgia (GA) RuSH Surveillance Project. Poster Session Presented at the Meeting of the Academy Health Research Conference; June, 2016; Boston, MA. [Accessed July 1, 2016]. http://ghpc.gsu.edu/download/accuracy-icd-9-coding-sickle-cell-disease-scd-children-adolescents/ [Google Scholar]
- 16.Kauf TL, Coates TD, Huazhi L, et al. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84(6):323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- 17.Lanzkron S, Carroll CP, Haywood C., Jr The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database. Am J Hematol. 2010;85(10):797–799. doi: 10.1002/ajh.21807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mvundura M, Amendah D, Kavanagh PL, et al. Health care utilization and expenditures for privately and publicly insured children with sickle cell disease in the United States. Pediatr Blood Cancer. 2009;53(4):642–646. doi: 10.1002/pbc.22069. [DOI] [PubMed] [Google Scholar]
- 19.Raphael JL, Dietrich CL, Whitmire D, et al. Healthcare utilization and expenditures for low income children with sickle cell disease. Pediatr Blood Cancer. 2009;52(2):263–267. doi: 10.1002/pbc.21781. [DOI] [PubMed] [Google Scholar]
- 20.Wolfson JA, Schrager SM, Coates TD, et al. Sickle-cell disease in California: a population-based description of emergency department utilization. Pediatr Blood Cancer. 2011;56(3):413–419. doi: 10.1002/pbc.22792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yusuf HR, Atrash HK, Grosse SD, et al. Emergency department visits made by patients with sickle cell disease: a descriptive study, 1999–2007. Am J Prev Med. 2010;38(4 Suppl):S536–S541. doi: 10.1016/j.amepre.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nimmer M, Hoffmann RG, Dasgupta M, et al. The proportion of potentially preventable emergency department visits by patients with sickle cell disease. J Pediatr Hematol Oncol. 2015;37(1):48–53. doi: 10.1097/MPH.0000000000000124. [DOI] [PubMed] [Google Scholar]