Abstract
Objective
Sleep disturbance is a major consequence of hot flashes among breast cancer survivors. This study evaluated the effects of electro-acupuncture vs. gabapentin for sleep disturbances among breast cancer survivors experiencing daily hot flashes.
Methods
We analyzed data from a randomized controlled trial involving 58 breast cancer survivors experiencing bothersome hot flashes at least two times per day. Participants were randomly assigned to receive eight weeks of electro-acupuncture or daily gabapentin (total dose of 900 mg per day). The primary outcome was change in the total Pittsburgh Sleep Quality Index (PSQI) score between groups at Week 8. Secondary outcomes include specific PSQI domains.
Results
By the end of treatment at Week 8, the mean reduction in PSQI total score was significantly greater in the electro-acupuncture group as compared to the gabapentin group (−2.6 vs. −0.8, p=0.044). The electro-acupuncture also had improved sleep latency (−0.5 vs. 0.1, p=0.041) and sleep efficiency (−0.6 vs. 0.0, p=0.05) compared to the gabapentin group. By Week 8, the electro-acupuncture group improved sleep duration, sleep disturbance, sleep latency, daytime dysfunction, sleep efficiency, and sleep quality (p<0.05 for all) compared to baseline, whereas the gabapentin group improved in duration and sleep quality only (p<0.05).
Conclusions
Among women experiencing hot flashes, the effects of electro-acupuncture are comparable to gabapentin for improving sleep quality, specifically in the areas of sleep latency and efficiency. Larger randomized controlled trials with longer follow-ups are needed to confirm this preliminary finding.
Clinical Trial Registration
Keywords: Acupuncture, gabapentin, sleep, hot flashes, vasomotor, breast neoplasm
INTRODUCTION
Hot flashes are one of the most common and disruptive side effects experienced by breast cancer survivors.1,2 Studies suggest that approximately 30–40% of women with breast cancer report persistent moderate to severe hot flashes.3,4 Although precise definitions vary, hot flashes, or flushes, are episodic periods of intense heat beginning at the chest but moving to the neck and face, causing flushing, sweating, and heart palpitations, and lasting several seconds to minutes.5 Compared to women who undergo natural menopause, breast cancer survivors are at greater risk of experiencing problematic hot flashes for a number of reasons including, but not limited to, age at diagnosis, premature menopause resulting from chemotherapy and surgery, and estrogen deficiency caused by the use of hormonal treatments such as tamoxifen and aromatase inhibitors.6 Projections suggest that there will be close to 6 million breast cancer survivors in the United States by the year 2020,7 making symptom reduction and maintenance of quality of life a clinical priority.
Hot flashes can occur frequently throughout a 24-hour period; however, nocturnal hot flashes are among the most problematic because they can contribute to poor sleep.8 The construct of poor sleep is multi-faceted and can be characterized by insufficient sleep quantity and/or quantity, difficulty falling asleep or staying asleep, and/or non-restorative sleep. These can be singular symptoms but when combined they represent Insomnia Disorder, a more severe and pernicious condition.9 In one of the few studies to objectively measure hot flash frequency using 24-hour skin conductance monitoring in 21 postmenopausal breast cancer survivors, close to 50% exhibited three to seven nocturnal hot flashes.10 In a population-based cohort study of 255 midlife women undergoing natural menopause, women who experienced moderate to severe hot flashes were 1.8 times more likely to experience poor sleep than women who experience mild or no hot flashes.11 Hot flash frequency and severity in breast cancer survivors and healthy postmenopausal women has been associated with subjective and objective sleep disturbance, daytime fatigue, mood disturbances, and greater perceived interference with daily life activities.12–14 In a longitudinal study of 58 women receiving adjuvant treatment for breast cancer by Savard et al., hot flashes played a significant role in the development and worsening of insomnia symptoms.15 Considering that disrupted sleep has been associated with poorer overall psychological and physical health outcomes,16–19 effective interventions for disruptive nocturnal hot flashes will likely also improve sleep and a host of other downstream concerns.
Studies evaluating medication usage for sleep disturbances related to hot flashes in menopausal women indicate safety and effectiveness for drugs such as gabapentin and venlafaxine.20–23 However, women often choose to discontinue these medications due to side effects including dizziness/unsteadiness, fatigue/somnolence, and ataxia when taking gabapentin, and dry mouth, constipation, and headaches with venlafaxine, which, while often mild, are still undesirable.20,22,24 Several recent trials have shown that acupuncture, a therapy originating from Traditional Chinese Medicine, is an effective treatment for hot flashes in breast cancer survivors with few, if any, side effects.25–29 Compared to sham-acupuncture and no treatment control groups, acupuncture demonstrated a clear improvement in hot flash frequency in a double blind randomized controlled trial of 94 women post-treatment for breast cancer.30 Acupuncture has also been shown to be more effective than self-care alone for reducing hot flash frequency and intensity, an effect that was maintained at the 12 month follow-up assessment.31,32 The effectiveness of acupuncture compared to enhanced self-care was recently confirmed in a large pragmatic randomized controlled trial of 190 women with hot flashes secondary to breast cancer treatment.33 Several of the above trials also reported improved sleep as a secondary outcome.25,26,30,31 However, rigorously conducted trials with larger sample sizes and the inclusion of active comparison interventions are required before making definitive statements about the efficacy of acupuncture in improving sleep disturbance related to hot flashes.
While sleep is often a secondary outcome in interventions for hot flashes, little is known about the comparative effects of acupuncture to pharmacological interventions for sleep disturbances in women with hot flashes. We analyzed pre-specified secondary sleep outcomes in a recently completed Phase-II four arm randomized controlled trial (RCT) to evaluate the short term effects of electro-acupuncture (EA) compared to daily gabapentin (GP), sham acupuncture, and placebo pill in women with breast cancer experiencing bothersome hot flashes.35 We chose electro-acupuncture in particular because it has been shown to affect endorphins and other central neuropeptides offering biological plausibility for addressing hot flashes.36 We restricted the analyses to the two active treatment arms (EA and GP) to estimate the related effects of EA to an established pharmacological intervention on sleep quality in women who experience hot flashes. As a secondary aim, we also explored how acupuncture and gabapentin may impact sleep quality in specific domains. Comparative effectiveness research is an identified priority to assist in patient decision-making between available treatment options.34
METHODS
Participants
Participants were recruited from November 2009 through June 2013 by physician referral or in person clinic recruitment at the Abramson Cancer Center of the Hospital of the University of Pennsylvania, an academic medical center in Philadelphia. Eligible participants were women with a history of early stage breast cancer (stages 0–III), free of cancer as determined by an oncologist or primary care physician, with at least two hot flashes daily over the seven-day screening period. Hot flashes had to have been present for at least a month before study entry, and women had to be willing to use non-hormonal contraceptives during the duration of the study if premenopausal. We excluded individuals who had metastatic (stage IV) breast cancer, were currently in active treatment, had initiated or changed hormonal adjuvant therapy within the past four weeks or planned to initiate or change hormonal treatment in the coming 14 weeks, were pregnant or breast feeding, had a bleeding disorder or used warfarin/heparin, had an allergy to or prior use of gabapentin for hot flashes, were currently using an anti-convulsant, or had documented renal failure in the last 12 months. Participants were randomly assigned to treatment groups using computer-generated numbers sealed in opaque envelopes. Randomization was stratified by hormonal therapy status and included random block sizes of four or eight. All participants provided informed consent prior to randomization. The acupuncture treatments were delivered at medical clinics in the hospital. The Institutional Review Board of the University of Pennsylvania approved the study protocol.
Interventions
Electro-Acupuncture: Two licensed non-physician acupuncturists with 8 and 20 years of experience, respectively, administered interventions twice a week for two weeks, then weekly for six more weeks, for a total of ten treatments over eight weeks. The detailed protocol has been previously published.35 In brief, for EA, the acupuncturist chose standard points depending on the participant’s preferred positions. Additionally, up to four acupuncture points were chosen based on the participant’s other presenting symptoms (e.g. fatigue, insomnia). The needles (30 mm or 40mm and 0.25 mm gauge, Seirin-America Inc., Weymouth, MA) were inserted and manipulated until the participant reported “De Qi” (sensation of soreness, tingling, etc.).37 A bilateral two hertz current was connected between two acupuncture points using a TENS unit. The needles were left in place for 30 minutes with brief manipulation at the beginning, middle, and end of therapy.
Gabapentin: A total daily dose of 900 mg was chosen for GP as it was previously found to be effective in a prior placebo controlled trial in breast cancer survivors.5 There was a 6-day titration phase when participants took one pill (300 mg) at bedtime for three days, then twice daily for three days, and then three times daily for the remaining 50 days (a total of eight weeks). At the beginning of Week 9, the participants tapered the medication by taking one 300 mg pill twice daily for three days and once daily for three days before discontinuing. The Investigational Drug Services at the University of Pennsylvania purchased GP 300mg pills and masked the medication by placing the whole intact dose into a larger opaque gelatin capsule shell.
Outcome Measures
Sleep disturbance was assessed using the Pittsburgh Sleep Quality Index (PSQI) pre- and post-treatment. The 19-item PSQI instrument produces a global sleep quality score and seven specific component scores: quality, latency, duration, disturbance, habitual sleep efficiency, use of sleeping medications, and daytime dysfunction. Global scores range from 0–21 with higher scores indicating poor sleep quality and high sleep disturbance.38
The hot flash composite score (HFCS) is the weekly average of hot flashes reported on their Daily Hot Flash Diary39 for a one-week period before and after the 8-week study period. Each participant recorded how many hot flashes she experienced each day and how many were mild, moderate, severe, or very severe. The composite score for each day can be calculated by multiplying the number of mild, moderate, severe, or very severe hot flashes by 1, 2, 3, or 4, respectively, and adding the values. The Daily Hot Flash Diary is reliable, valid, and responsive to treatment effects.
Statistical Analysis
The primary outcome was mean change in the total Pittsburgh Sleep Quality Index (PSQI) score between the two groups from baseline to end of intervention (Week 8) between EA and GP. Secondary outcomes include specific PSQI domains. We used descriptive statistics to summarize data on demographics and cancer history variables. We calculated change scores by subtracting the pre scores from the post scores for each participant. We analyzed between and within group component and total scores on the PQSI for all participants using independent samples and paired t tests. We assessed associations between change on the PSQI total and component scores and the HFCS using Spearman’s rank order correlations to explore differences in mechanism of action of the two interventions. All statistical analyses were two-sided. Statistical significance was set at <0.05 level. Statistical analyses were performed using STATA.
RESULTS
As previously reported,35 between November 2009 and June 2013, we screened 498 women and randomized 120. Of these participants, 30 were randomized to EA and 28 to GP. All women remained in the study for the 8-week treatment. Among participants, 27 (90.0%) in the EA group received all ten acupuncture treatments and 21 (75.0%) in the GP group were adherent to medications based on pill count. The primary reason for non-adherence to EA was scheduling and time commitment versus the primary reason for non-adherence to gabapentin was intolerance of drug side effects.
As shown in Table 1, among all 58 participants, mean age was 51.7 (SD=8.5) with a range from 31.1 to 75.5 years. The women had been diagnosed with cancer 3.4 ± 3.9 years prior to study participation. The sample was primarily self-identified as White women (74.1%), with 22.4% describing themselves as Black. The majority of the women were married or in a partnered relationship (70.7%). Most of the women (86.0%) were post-menopausal and 63.8% were on hormonal treatments. Close to all of the women (93.1%) had attended college or above.
Table 1.
Baseline Demographic and Clinical Characteristics by Group
| Electro-Acupuncture (n=30) |
Gabapentin (n=28) |
|
|---|---|---|
| Demographic Characteristics | ||
| Age (years) | ||
| Mean ± SD | 52.9 ± 8.6 | 50.4 ± 8.4 |
| Age Range | 31.1–69.9 | 36.4–75.5 |
| BMI | ||
| Mean ± SD | 28.3 ± 5.9 | 29.3 ± 7.7 |
| Education: N (%) | ||
| High School or Less | 3 (10) | 1 (4) |
| College | 13 (43) | 18 (64) |
| Graduate or Higher | 14 (47) | 9 (32) |
| Marital Status: N (%) | ||
| Married/partnered | 20 (67) | 21 (75) |
| Single | 10 (33) | 7 (25) |
| Occupational Status: N (%) | ||
| Full Time | 19 (64) | 18 (64) |
| Part Time | 6 (20) | 5 (18) |
| Not employed | 4 (13) | 4 (14) |
| Retired | 1 (3) | 1 (4) |
| Race: N (%) | ||
| White | 26 (87) | 17 (61) |
| Black/African American | 3 (10) | 10 (36) |
| Other | 1 (3) | 1 (3) |
| Clinical Characteristics | ||
| Years since diagnosis | ||
| Mean± SD | 3.3 ± 3.7 | 3.5 ± 4.3 |
| Cancer Stage: N (%) | ||
| 0 and I | 14 (48) | 15 (55) |
| II | 11 (38) | 11 (41) |
| III | 4 (14) | 1 (4) |
| Menopausal status: N (%) | ||
| Pre-menopausal | 4 (13) | 4 (15) |
| Post-menopausal | 26 (87) | 23 (85) |
| Hormonal Therapy: N (%) | ||
| None | 9 (30) | 10 (36) |
| Tamoxifen | 15 (50) | 11 (39) |
| Aromatase inhibitors | 6 (20) | 7 (25) |
Between Group Change in Sleep
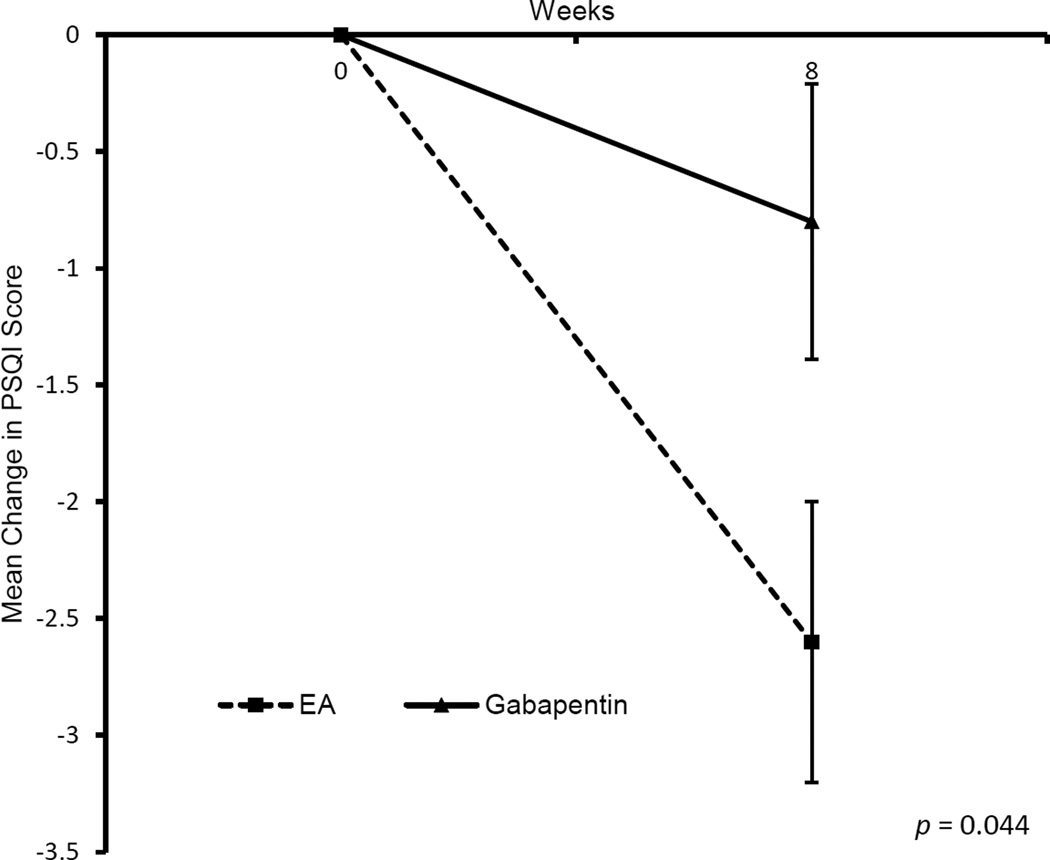
By Week 8, women in the EA group compared to the GP group, reported significantly better sleep as indicated by the reduction in PSQI global sleep quality score (−2.6 vs. −0.8; p=0.044) (Figure 1). From the PSQI subscales (Table 2), women in the EA group reported shorter sleep latency (−0.5 vs. 0.1; p=0.041) and higher sleep efficiency (−0.6 vs. 0.0; p=0.05).
Figure 1.
Impact of electro-acupuncture and gabapentin on total sleep disturbance
Table 2.
Within Group Changes in Sleep Quality
| Electro Acupuncture |
Gabapentin | Between Group P-value |
|
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| PSQI Total Score | 0.04 | ||
| Baseline | 9.1 (3.8) | 8.4 (3.9) | |
| Change from baseline at Wk 8 | −2.6 (3.2) | −0.8 (3.0) | |
| Pre-post P within group | 0.0003 | 0.18 | |
| Sleep Duration Subscale | 0.52 | ||
| Baseline | 1.0 (1.0) | 1.0 (1.2) | |
| Change from baseline at Wk8 | −0.4 (0.8) | −0.3 (0.8) | |
| Pre-post P within group | 0.008 | 0.048 | |
| Sleep Disturbance Subscale | 0.40 | ||
| Baseline | 1.7 (0.6) | 1.7 (0.6) | |
| Change from baseline at Wk8 | −0.2 (0.6) | −0.07 (0.8) | |
| Pre-post P within group | 0.032 | 0.62 | |
| Sleep Latency Subscale | 0.04 | ||
| Baseline | 1.3 (1.0) | 1.0 (0.9) | |
| Change from baseline at Wk8 | −0.5 (1.0) | 0.1 (1.0) | |
| Pre-post P within group | 0.025 | 0.12 | |
| Daytime Dysfunction Subscale | 0.60 | ||
| Baseline | 1.5 (1.0) | 1.4 (1.0) | |
| Change from baseline at Wk8 | −0.4 (1.0) | −0.2 (1.2) | |
| Pre-post P within group | 0.046 | 0.72 | |
| Sleep Efficiency Subscale | 0.05 | ||
| Baseline | 1.0 (1.1) | 0.9 (1.1) | |
| Change from baseline at Wk8 | −0.6 (1.0) | 0.0 (1.1) | |
| Pre-post P within group | 0.006 | 1.0 | |
| Sleep Quality Subscale | 0.93 | ||
| Baseline | 1.6 (0.8) | 1.5 (0.7) | |
| Change from baseline at Wk8 | −0.5 (0.9) | −0.5 (0.7) | |
| Pre-post P within group | 0.008 | 0.003 | |
| Use of Sleeping Medication Subscale | 0.67 | ||
| Baseline | 0.9 (1.1) | 1.0 (1.3) | |
| Change from baseline at Wk8 | −0.1 (0.9) | 0.0 (1.0) | |
| Pre-post P within group | 0.54 | 1.0 | |
Within Group Change in Specific domains of Sleep
Compared to baseline, by Week 8, EA improved sleep duration, sleep disturbance, sleep latency, daytime dysfunction, sleep efficiency, and sleep quality (p<0.05 for all); whereas GP improved duration and sleep quality (p<0.05). Refer to Table 2.
Associations between Changes in Hot Flashes And Sleep Disturbances
At baseline, 51 (87.9%) of the women met the clinical cutoff of 5 or higher for sleep disturbance. There were no significant baseline differences in sleep disturbances between conditions with 90% of the women in the EA group and 86% of the women in the GP group exceeding the PSQI cutoff. Women in both groups experienced a significant reduction in the hot flash composite score during treatment (EA: 15.5 to 8.1, Δ=7.4; GP: 13.2 to 8.0, Δ=5.2).
Significant associations were observed between a reduction in hot flash severity/frequency and improved sleep latency and sleep quality for the full sample. A trend was observed for the PSQI total score. When the groups were considered separately, only a trend towards a reduction in hot flash severity/frequency and improved sleep was seen for the indices of sleep disturbance (EA), sleep latency (GP) and sleep quality (EA and GP). See Table 3.
Table 3.
Association between Changes in Hot Flashes and Sleep Disturbance
| Hot Flash Composite Change Score | |||
|---|---|---|---|
| Electro Acupuncture |
Gabapentin | Both Groups | |
| Pre-Post Change Score | |||
| PSQI Total Score | ρ = 0.14; p = 0.49 | ρ = 0.18; p = 0.40 | ρ = 0.22; p = 0.13 |
| Sleep Duration | ρ = −0.18; p = 0.34 | ρ = 0.02; p = 0.93 | ρ = −0.09; p = 0.52 |
| Sleep Disturbance | ρ = 0.35; p =0.08 | ρ = −0.09; p = 0.67 | ρ = 0.14; p = 0.32 |
| Sleep Latency | ρ = 0.09; p = 0.67 | ρ = 0.30; p = 0.14 | ρ = 0.23; p = 0.01 |
| Daytime Dysfunction | ρ = 0.15; p = 0.45 | ρ = −0.19; p = 0.33 | ρ = 0.01; p = 0.96 |
| Sleep Efficiency | ρ = −0.04; p = 0.86 | ρ = −0.02; p = 0.93 | ρ = 0.06; p = 0.64 |
| Sleep Quality | ρ = 0.31; p = 0.10 | ρ = 0.35; p = 0.07 | ρ = 0.34; p = 0.01 |
| Use of Sleeping Medication | ρ = 0.20; p =0.30 | ρ = 0.08; p = 0.70 | ρ = 0.19; p = 0.17 |
DISCUSSION
Sleep disturbances are highly prevalent in breast cancer survivors who experience hot flashes.8 In our sample, close to 90% of women could be classified as having poor sleep quality at trial initiation. A recent review of the treatment of insomnia in women with menopausal symptoms by Attarian et al. gave gabapentin a level B rating, owing to its favorable safety profile, especially if vasomotor symptoms play a large role in contributing to the sleep disturbances.40 They also recommended head-to-head evaluations among promising treatments. This is the first study to demonstrate that acupuncture is as good as, if not better in some respects than, gabapentin for improving sleep parameters in women with breast cancer. We demonstrated that when compared with a daily dose of 900 mg of GP, an 8-week course of EA resulted in better self-reported overall sleep quality. Specifically, women receiving EA reported were able to fall asleep faster and spent more time in bed sleeping as opposed to lying awake in bed trying to sleep. Our results suggest that EA results in improved sleep in women with hot flashes and might be a viable treatment option in women who do not wish to take medication.
Despite a significant improvement in sleep for the women in the EA condition, it should be noted that the mean scores remained above the recommended clinical cutoff for sleep disturbance suggesting opportunities for further refining the intervention to optimize sleep outcomes in this population. Further research may need to examine the efficacy of acupuncture as an adjunctive treatment to another pharmacological or non-pharmacological intervention to achieve more complete symptom relief in women with disturbed sleep and hot flashes.
It is generally believed that hot flashes produce arousals and awakenings from sleep; however, the research on this has not been entirely consistent.24 It is more likely that the association between sleep and hot flashes is bi-directional. In a controlled laboratory study of 19 symptomatic and asymptomatic post- and pre-menopausal women between the ages of 46 and 51 years using sleep electroencephalograms and sternal skin conductance to record hot flashes, Freedman and Roehrs found that hot flashes tended to follow rather than precede arousals and awakenings.41 This means that the women woke up for a reason not related to hot flash activity (e.g. normal sleep stage transitions), at which time they experienced the hot flash. This suggests that improving sleep and reducing nocturnal arousals may lead to fewer hot flashes and similarly, reducing nocturnal hot flashes can improve overall sleep. In our study, the correlations between change in hot flash severity/frequency and sleep outcomes were generally small. The strongest associations (albeit still ~.30) were observed between a reduction in hot flash severity/frequency and improved sleep quality, regardless of treatment condition. This suggests that other factors may influence the association between sleep quality and hot flash severity/frequency including within night distribution of hot flashes, disruption caused by severity of sweating (e.g. needing to change bed clothes or sheets), and/or the psychological interpretation of distress caused by the awakening and the hot flash. Additional research with larger samples is needed to investigate potential differences in pathways and/or mechanisms of action for both treatments.
It is also not currently understood how exactly acupuncture might beneficially impact hot flash severity/frequency and sleep. Acupuncture has been shown to affect a number of neurotransmitters and hormonal factors associated with sleep, such as serotonin, melatonin, and gamma-aminobutyric acid (GABA).42 Evidence also suggests that acupuncture has the potential to repair fragmented sleep architecture and increase time spent in slow wave sleep,43 which would correspond to the perception of a deeper and more restorative sleep. A systematic review of 20 randomized controlled trials of acupuncture for insomnia suggested that traditional needle acupuncture was slightly more effective than benzodiazepines with response rates for acupuncture and benzodiazepines being 91% and 75%.44 Similarly, acupuncture was found to be equally as effective as zolpidem for improving sleep in 33 individuals with insomnia.45 The search for potential mechanisms of acupuncture is still in the early stages and work is currently ongoing to help researchers design trials to better understand its effect.46,47
Despite several strengths, including two active treatment groups, a well-defined sample, and excellent retention of participants, the following limitations deserve mention. First, there was no follow-up assessment after the end of treatment; therefore, it is not possible to evaluate any potential differences in the long-term effects of acupuncture versus gabapentin on sleep in women with hot flashes. Second, sleep and vasomotor activity were assessed with self-report measures. While this is standard in comparative trials because it allows for people to be assessed in their own environment, future research may want to include objective and/or in lab measurements such as actigraphy, electroencephalograms, and/or skin conductance to better understand the relationship between sleep and hot flashes and the effect of treatment. Third, sleep was a secondary outcome and we did not purposely select the sample for the presence of disturbed sleep or screen for the presence of sleep disorders (e.g. insomnia, sleep disordered breathing). This prevents us from specifically defining the nature of the sleep disturbances. Further research is needed to replicate this finding in studies with larger and more diverse samples and follow-up assessments to establish the durability of effect.
CONCLUSIONS
Sleep disturbances, including those that occur in conjunction with hot flashes, are especially problematic because of their negative relationship to psychological health and physical well-being. More often than not, poor sleep increases levels of pain, fatigue, depression, and anxiety, creating a positive feedback loop in which all symptoms are amplified and overall symptom burden is increased.48,49 The use of targeted interventions to treat difficulty sleeping and hot flashes would be expected to also positively impact other areas of functioning as well. We have demonstrated that electro-acupuncture produces comparable, if not better, improvements in sleep quality than gabapentin, a currently recommended pharmacological intervention. Comparative effectiveness studies such as this represent a step forward in providing clinicians and patients with information needed to make better and more informed treatment decisions.
Acknowledgments
Funding Source:
Dr. Mao is a recipient of the NCCAM K23 AT004112 award. This manuscript is also supported in part by a grant from the National Institutes of Health / National Cancer Institute Cancer Center (P30 CA008748).
We thank our acupuncturists, Lorna Lee and Adam Schreiber, for delivering the interventions.
Sincere thanks go to the participants, oncologists, nurse practitioners, and clinical staff for their support of this study.
Footnotes
Disclosure: The other co-authors have no conflicts of interest to declare.
Author Contributions: QL, CS, and JJM conceived of the study and participated in its design and coordination. SNG, SXX, QL, CB, and JJM performed the statistical analyses and interpretation. SNG, CS, and JJM drafted the manuscript. All authors read and approved the final manuscript. SNG and JJM are responsible for the overall content.
References
- 1.Carpenter JS, Andrykowski MA, Cordova M, et al. Hot flashes in postmenopausal women treated for breast carcinoma: Prevalence, severity, correlates, management, and relation to quality of life. Cancer. 1998;82(9):1682–1691. doi: 10.1002/(SICI)1097-0142(19980501)82:93.0.CO;2-0 [pii] [PubMed] [Google Scholar]
- 2.Carpenter JS, Johnson D, Wagner L, Andrykowski M. Hot flashes and related outcomes in breast cancer survivors and matched comparison women. Oncol Nurs Forum. 2002;29(3):E16–E25. doi: 10.1188/02.ONF.E16-E25. [doi] [DOI] [PubMed] [Google Scholar]
- 3.Mortimer J, Behrendt CE. Severe menopausal symptoms are widespread among survivors of breast cancer treatment regardless of time since diagnosis. J Palliat Med. 2013;16(9):1130–1134. doi: 10.1089/jpm.2012.0585. [doi] [DOI] [PubMed] [Google Scholar]
- 4.Gallicchio L, MacDonald R, Wood B, Rushovich E, Helzlsouer KJ. Menopausal-type symptoms among breast cancer patients on aromatase inhibitor therapy. Climacteric. 2012;15(4):339–349. doi: 10.3109/13697137.2011.620658. [doi] [DOI] [PubMed] [Google Scholar]
- 5.Pandya KJ, Morrow GR, Roscoe JA, et al. Gabapentin for hot flashes in 420 women with breast cancer: A randomised double-blind placebo-controlled trial. Lancet. 2005;366(9488):818–824. doi: 10.1016/S0140-6736(05)67215-7. doi: S0140-6736(05)67215-7 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bordeleau L, Pritchard KI, Loprinzi CL, et al. Multicenter, randomized, cross-over clinical trial of venlafaxine versus gabapentin for the management of hot flashes in breast cancer survivors. J Clin Oncol. 2010;28(35):5147–5152. doi: 10.1200/JCO.2010.29.9230. [doi] [DOI] [PubMed] [Google Scholar]
- 7.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the united states, 2010–2020. J Natl Cancer Inst. 2011;103(2):117–128. doi: 10.1093/jnci/djq495. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang HY, Jotwani AC, Lai YH, et al. Hot flashes in breast cancer survivors: Frequency, severity and impact. Breast. 2016;27:116–121. doi: 10.1016/j.breast.2016.02.013. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5) 5th. Washington, DC: Author; 2013. [Google Scholar]
- 10.Carpenter JS, Gautam S, Freedman RR, Andrykowski M. Circadian rhythm of objectively recorded hot flashes in postmenopausal breast cancer survivors. Menopause. 2001;8(3):181–188. doi: 10.1097/00042192-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Freeman EW, Sammel MD, Gross SA, Pien GW. Poor sleep in relation to natural menopause: A population-based 14-year follow-up of midlife women. Menopause. 2015;22(7):719–726. doi: 10.1097/GME.0000000000000392. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavigne JE, Griggs JJ, Tu XM, Lerner DJ. Hot flashes, fatigue, treatment exposures and work productivity in breast cancer survivors. J Cancer Surviv. 2008;2(4):296–302. doi: 10.1007/s11764-008-0072-z. [doi] [DOI] [PubMed] [Google Scholar]
- 13.Berger AM, Treat Marunda HA, Agrawal S. Influence of menopausal status on sleep and hot flashes throughout breast cancer adjuvant chemotherapy. J Obstet Gynecol Neonatal Nurs. 2009;38(3):353–366. doi: 10.1111/j.1552-6909.2009.01030.x. [DOI] [PubMed] [Google Scholar]
- 14.Carpenter JS, Gilchrist JM, Chen K, Gautam S, Freedman RR. Hot flashes, core body temperature, and metabolic parameters in breast cancer survivors. Menopause. 2004;11(4):375–381. doi: 10.1097/01.gme.0000113848.74835.1a. doi: 00042192-200411040-00003 [pii] [DOI] [PubMed] [Google Scholar]
- 15.Savard MH, Savard J, Trudel-Fitzgerald C, Ivers H, Quesnel C. Changes in self-reported hot flashes and their association with concurrent changes in insomnia symptoms among women with breast cancer. Menopause. 2011;18(9):985–993. doi: 10.1097/gme.0b013e31820db6a1. [doi] [DOI] [PubMed] [Google Scholar]
- 16.Kyle SD, Morgan K, Espie CA. Insomnia and health-related quality of life. Sleep Med Rev. 2010;14(1):69–82. doi: 10.1016/j.smrv.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64(4):409–415. doi: 10.1016/j.jpsychores.2007.11.008. [doi] [DOI] [PubMed] [Google Scholar]
- 18.Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65(1):63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 19.Simpson N, Dinges DF. Sleep and inflammation. Nutr Rev. 2007;65(12 Pt 2):S244–S252. doi: 10.1111/j.1753-4887.2007.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter JS, Storniolo AM, Johns S, et al. Randomized, double-blind, placebo-controlled crossover trials of venlafaxine for hot flashes after breast cancer. Oncologist. 2007;12(1):124–135. doi: 10.1634/theoncologist.12-1-124. doi: 12/1/124 [pii] [DOI] [PubMed] [Google Scholar]
- 21.Joffe H, Partridge A, Giobbie-Hurder A, et al. Augmentation of venlafaxine and selective serotonin reuptake inhibitors with zolpidem improves sleep and quality of life in breast cancer patients with hot flashes: A randomized, double-blind, placebo-controlled trial. Menopause. 2010;17(5):908–916. doi: 10.1097/gme.0b013e3181dbee1b. [doi] [DOI] [PubMed] [Google Scholar]
- 22.Toulis KA, Tzellos T, Kouvelas D, Goulis DG. Gabapentin for the treatment of hot flashes in women with natural or tamoxifen-induced menopause: A systematic review and meta-analysis. Clin Ther. 2009;31(2):221–235. doi: 10.1016/j.clinthera.2009.02.006. [doi] [DOI] [PubMed] [Google Scholar]
- 23.Yurcheshen ME, Guttuso T, Jr, McDermott M, Holloway RG, Perlis M. Effects of gabapentin on sleep in menopausal women with hot flashes as measured by a pittsburgh sleep quality index factor scoring model. J Womens Health (Larchmt) 2009;18(9):1355–1360. doi: 10.1089/jwh.2008.1257. [doi] [DOI] [PubMed] [Google Scholar]
- 24.Freedman RR. Menopausal hot flashes: Mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol. 2014;142:115–120. doi: 10.1016/j.jsbmb.2013.08.010. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frisk J, Kallstrom AC, Wall N, Fredrikson M, Hammar M. Acupuncture improves health-related quality-of-life (HRQoL) and sleep in women with breast cancer and hot flushes. Support Care Cancer. 2012;20(4):715–724. doi: 10.1007/s00520-011-1134-8. [doi] [DOI] [PubMed] [Google Scholar]
- 26.Otte JL, Carpenter JS, Zhong X, Johnstone PA. Feasibility study of acupuncture for reducing sleep disturbances and hot flashes in postmenopausal breast cancer survivors. Clin Nurse Spec. 2011;25(5):228–236. doi: 10.1097/NUR.0b013e318229950b. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Valois BA, Young TE, Robinson N, McCourt C, Maher EJ. Using traditional acupuncture for breast cancer-related hot flashes and night sweats. J Altern Complement Med. 2010;16(10):1047–1057. doi: 10.1089/acm.2009.0472. [doi] [DOI] [PubMed] [Google Scholar]
- 28.Painovich JM, Shufelt CL, Azziz R, et al. A pilot randomized, single-blind, placebo-controlled trial of traditional acupuncture for vasomotor symptoms and mechanistic pathways of menopause. Menopause. 2012;19(1):54–61. doi: 10.1097/gme.0b013e31821f9171. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baccetti S, Da Fre M, Becorpi A, et al. Acupuncture and traditional chinese medicine for hot flushes in menopause: A randomized trial. J Altern Complement Med. 2014;20(7):550–557. doi: 10.1089/acm.2012.0499. [doi] [DOI] [PubMed] [Google Scholar]
- 30.Bokmand S, Flyger H. Acupuncture relieves menopausal discomfort in breast cancer patients: A prospective, double blinded, randomized study. Breast. 2013;22(3):320–323. doi: 10.1016/j.breast.2012.07.015. [doi] [DOI] [PubMed] [Google Scholar]
- 31.Borud EK, Alraek T, White A, Grimsgaard S. The acupuncture treatment for postmenopausal hot flushes (acuflash) study: Traditional chinese medicine diagnoses and acupuncture points used, and their relation to the treatment response. Acupunct Med. 2009;27(3):101–108. doi: 10.1136/aim.2009.000612. [doi] [DOI] [PubMed] [Google Scholar]
- 32.Borud EK, Alraek T, White A, Grimsgaard S. The acupuncture on hot flashes among menopausal women study: Observational follow-up results at 6 and 12 months. Menopause. 2010;17(2):262–268. doi: 10.1097/gme.0b013e3181c07275. [doi] [DOI] [PubMed] [Google Scholar]
- 33.Lesi G, Razzini G, Musti MA, et al. Acupuncture as an integrative approach for the treatment of hot flashes in women with breast cancer: A prospective multicenter randomized controlled trial (AcCliMaT) J Clin Oncol. 2016 doi: 10.1200/JCO.2015.63.2893. doi: JCO632893 [pii] [DOI] [PubMed] [Google Scholar]
- 34.Frank L, Basch E, Selby JV. Patient-Centered Outcomes Research Institute. The PCORI perspective on patient-centered outcomes research. JAMA. 2014;312(15):1513–1514. doi: 10.1001/jama.2014.11100. [doi] [DOI] [PubMed] [Google Scholar]
- 35.Mao JJ, Bowman MA, Xie SX, Bruner D, DeMichele A, Farrar JT. Electroacupuncture versus gabapentin for hot flashes among breast cancer survivors: A randomized placebo-controlled trial. J Clin Oncol. 2015 doi: 10.1200/JCO.2015.60.9412. doi: JCO.2015.60.9412 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han JS. Acupuncture and endorphins. Neurosci Lett. 2004;361(1–3):258–261. doi: 10.1016/j.neulet.2003.12.019. [doi] [DOI] [PubMed] [Google Scholar]
- 37.Mao JJ, Farrar JT, Armstrong K, Donahue A, Ngo J, Bowman MA, De qi. Chinese acupuncture patients' experiences and beliefs regarding acupuncture needling sensation--an exploratory survey. Acupunct Med. 2007;25(4):158–165. doi: 10.1136/aim.25.4.158. [DOI] [PubMed] [Google Scholar]
- 38.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 39.Sloan JA, Loprinzi CL, Novotny PJ, Barton DL, Lavasseur BI, Windschitl H. Methodologic lessons learned from hot flash studies. J Clin Oncol. 2001;19(23):4280–4290. doi: 10.1200/JCO.2001.19.23.4280. [DOI] [PubMed] [Google Scholar]
- 40.Attarian H, Hachul H, Guttuso T, Phillips B. Treatment of chronic insomnia disorder in menopause: Evaluation of literature. Menopause. 2015;22(6):674–684. doi: 10.1097/GME.0000000000000348. [doi] [DOI] [PubMed] [Google Scholar]
- 41.Freedman RR, Roehrs TA. Lack of sleep disturbance from menopausal hot flashes. Fertil Steril. 2004;82(1):138–144. doi: 10.1016/j.fertnstert.2003.12.029. [doi] [DOI] [PubMed] [Google Scholar]
- 42.Huang W, Kutner N, Bliwise DL. Autonomic activation in insomnia: The case for acupuncture. J Clin Sleep Med. 2011;7(1):95–102. [PMC free article] [PubMed] [Google Scholar]
- 43.Ruan JW, Wang CH, Liao XX, et al. Electroacupuncture treatment of chronic insomniacs. Chin Med J (Engl) 2009;122(23):2869–2873. [PubMed] [Google Scholar]
- 44.Yeung WF, Chung KF, Leung YK, Zhang SP, Law AC. Traditional needle acupuncture treatment for insomnia: A systematic review of randomized controlled trials. Sleep Med. 2009;10(7):694–704. doi: 10.1016/j.sleep.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 45.Tu JH, Chung WC, Yang CY, Tzeng DS. A comparison between acupuncture versus zolpidem in the treatment of primary insomnia. Asian J Psychiatr. 2012;5(3):231–235. doi: 10.1016/j.ajp.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 46.Deng S, Zhao X, DU R, et al. Is acupuncture no more than a placebo? extensive discussion required about possible bias. Exp Ther Med. 2015;10(4):1247–1252. doi: 10.3892/etm.2015.2653. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haddad NE, Palesh O. Acupuncture in the treatment of cancer-related psychological symptoms. Integr Cancer Ther. 2014 doi: 10.1177/1534735413520181. [DOI] [PubMed] [Google Scholar]
- 48.Stepanski EJ, Walker MS, Schwartzberg LS, Blakely LJ, Ong JC, Houts AC. The relation of trouble sleeping, depressed mood, pain, and fatigue in patients with cancer. J Clin Sleep Med. 2009;5(2):132–136. [PMC free article] [PubMed] [Google Scholar]
- 49.Trudel-Fitzgerald C, Savard J, Ivers H. Longitudinal changes in clusters of cancer patients over an 18-month period. Health Psychol. 2013 doi: 10.1037/a0033497. [DOI] [PubMed] [Google Scholar]