Abstract
Background
Despite being diagnostically associated uniquely with schizophrenia, negative symptoms are also observed in bipolar disorder (BD). Genome-wide association studies (GWAS) have uncovered a number of shared risk genes between schizophrenia and BD. The objectives of this study were to examine whether previously identified risk genes for BD are associated with negative symptom severity within a first-episode schizophrenia (FES) cohort and to examine whether such genes influence brain morphology.
Methods
Patients experiencing FES were genotyped for 21 previously identified BD risk genes; a series of univariate analyses of covariance examined the association between negative symptom severity, as measured using the Scale for the Assessment of Negative Symptoms (SANS), and genotype. A subset of participants underwent a structural 1.5 T MRI T1 scan, analyzed for surface area and cortical thickness changes via the CIVET pipeline and LPBA40 atlas.
Results
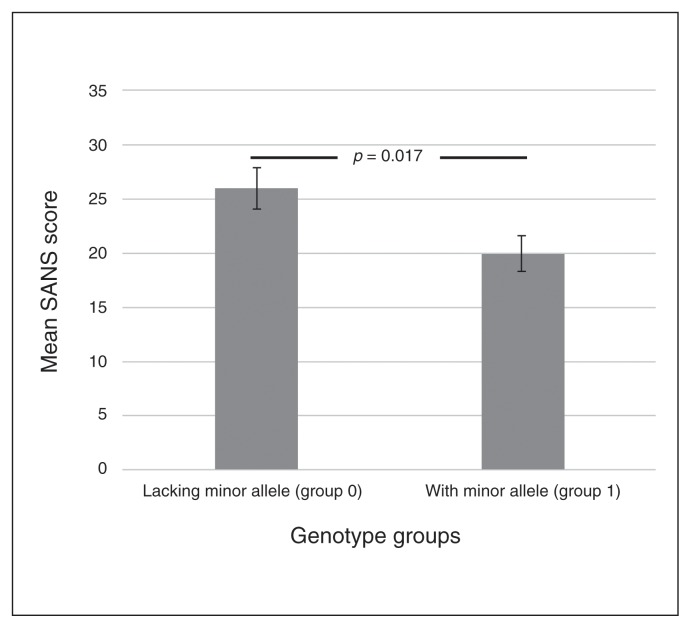
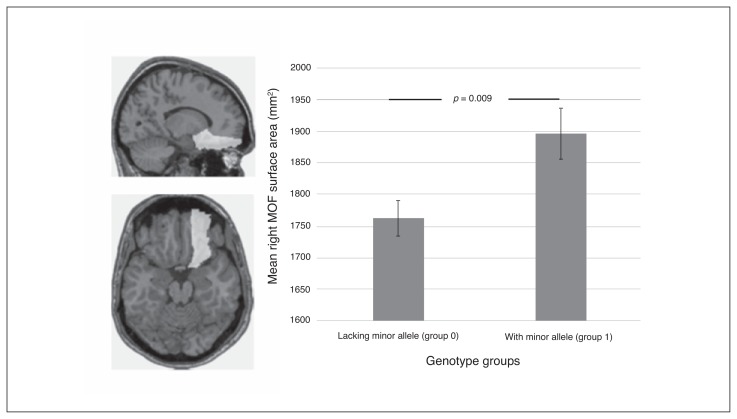
We included 133 patients with FES in our analysis; 61 of them underwent structural MRI. We observed a significant association between negative symptom severity and the BD risk gene FOXO6 (rs4660531). Individuals with the CC genotype presented significantly higher negative symptoms (Cohen d = 0.46, F = 5.854, p = 0.017) and significantly smaller surface area within the right middle orbitofrontal gyrus (Cohen d = 0.69, F = 7.289, p = 0.009) than carriers of allele A.
Limitations
Limitations of this study include its modest sample size and lack of a control sample.
Conclusion
Lacking the FOXO6 risk allele was associated with an increase in negative symptoms and surface area reduction in the right orbitofrontal gyrus — an area previously associated with negative symptoms —– suggesting that presence of the FOXO6 risk allele confers resistance against negative symptoms and associated neuroanatomical changes in individuals with FES.
Introduction
Despite significant attention, schizophrenia continues to be a prevalent and debilitating disorder. Although positive symptoms, such as hallucinations and delusions, can typically be treated with medication, patients often continue to experience negative symptoms, such as affective flattening, apathy, avolition and amotivation. Negative symptoms typically show only mild (if any) response to antipsychotic medications, and about one-third of patients with first-episode psychosis (FEP) will experience persistent negative symptoms, which represent significant impediments on the path to recovery.1,2 In addition, there is mounting evidence that negative symptoms are not unique to schizophrenia but may be present in other forms of psychosis (e.g., bipolar disorder [BD]).3,4 Understanding the underlying mechanisms of negative symptoms is, therefore, crucial in discovering interventions to improve outcomes for schizophrenia.
In addition to being an important obstacle on the path to recovery, familial studies have shown negative symptoms to be one of the more heritable traits of schizophrenia. One study found that patients with schizophrenia who also had affected relatives were more likely to present severe and treatment-resistant negative symptoms, whereas positive and cognitive symptoms were unrelated to family history.5 Another study recruited individuals with schizophrenia and their unaffected sibling(s) as well as pairs of healthy control siblings in order to investigate heritability of positive and negative symptoms as well as cognitive deficits associated with the disorder. That study found that negative symptoms coaggregated with 3 out of 4 neurocognitive measures (working memory, episodic memory and executive function, but not attention), which were also deficient in unaffected siblings, whereas positive and disorganization symptoms showed no such association. These findings suggest the heritability of negative symptoms, and the authors posit that there may be common genetic components that influence both negative symptoms and select neurocognitive impairments.6
Although schizophrenia and BD are diagnostically distinct, there is increasing evidence of the overlap between the 2 disorders. One comprehensive review found that when comparing schizophrenia and BD along genetic, neurophysiological and cognitive biomarkers rather than classical clinical expression, the 2 disorders shared important aspects of psychopathology, neurobiology and mechanisms of treatment.7 Familial heritability studies bolster this notion, with many studies uncovering coaggregation of schizophrenia and BD. One study found that risk for BD was associated with familial history of BD or schizophrenia, quantifying the risk of schizophrenia and BD developing in relatives of patients with schizophrenia at 10% and 8%, respectively.8
Genome-wide association studies (GWAS) have identified a large number of specific risk variants conferring risk for schizophrenia, BD and major depressive disorder (MDD).9 Although many single-nucleotide polymorphisms (SNPs) are associated with risk for a single disorder, many SNPs confer risk toward multiple neuropsychiatric disorders. A recent GWAS investigating risk loci within a range of psychiatric disorders found that a broad set of common genetic variants were associated with schizophrenia, BD and MDD; the authors additionally noted the parallels between this finding and those in other medical specialties, such as the overlap in genetic variants associated with a wide range of autoimmune disorders.9 A subsequent study by the same group examined the sharing of genetic risk factors across pairs of psychiatric disorders, including schizophrenia, BD, MDD, autism-spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). Although each pair of disorders was shown to share some common genetic risk factors, schizophrenia and BD were found to share as much as 17% of their underlying genetic contribution, more than any other pair of disorders examined.10 Further genetic linkage studies reported that, owing to shared genetic susceptibility, separating schizophrenia and BD into 2 genetically distinct disorders is impossible.7 This group also performed an analysis of risk prediction for schizophrenia, BD and MDD based on correlated traits and determined that, although polygenic traits make accurate risk prediction difficult, the pleiotropy between these disorders “implies that a SNP contributing risk of 1 disease will, on average, also be informative of the risk of the correlated disease.”11
The disparity between these findings and current diagnostic criteria has encouraged a number of new initiatives, such as the National Institute of Mental Health’s Research Domain Criteria (RDoC) campaign, to reclassify mental disorders based on underlying behavioural dimensions and neurobiological pathways rather than observable symptoms.12
Although negative symptoms are diagnostically associated with schizophrenia, studies suggest that negative symptoms are not unique to this disorder. Recent discussions of the overlap among psychotic disorders focus on common dimensions of psychosis, including positive, negative, disorganization and affective symptoms, rather than the more classical categorical separation.13 A number of studies have suggested a 3-factor model of symptomatology in schizophrenia involving negative symptoms, psychoticism (hallucinations and delusions) and disorganization,14–16 and this same 3-factor model has been shown by numerous studies to apply also to BD.17,18 A subsequent comprehensive analysis of symptomatology in schizophrenia, MDD and BD revealed that all 3 disorders share an underlying negative symptom factor, suggesting that negative symptoms represent a common dimension underlying the major affective and psychotic disorders.4 One study investigating negative symptoms in a group of patients with remitted BD found that about 27% of participants exhibited clinically significant negative symptoms and found that negative symptom severity was inversely correlated with participants’ current socio-occupational functioning.3 Finally, a number of genes associated with negative symptoms in schizophrenia have also been identified as BD risk genes. ST3GAL1 has been associated with risk for BD,19,20 while variants of BCL9 have been associated with risk for BD and schizophrenia;21 both genes were later associated with the presence of negative symptoms in patients with schizophrenia.22
The above evidence suggests a common biological basis for negative symptoms, regardless of diagnosis — a finding that is perhaps unsurprising, given that negative symptoms, such as flattened affect, social withdrawal, amotivation and apathy can closely resemble symptoms of an episode of depression. Given that negative symptoms are not unique to schizophrenia, and considering the shared genetic contributions between schizophrenia and BD, it is possible that risk alleles for BD may modulate the severity of negative symptoms in patients with schizophrenia. Despite this, cross-disorder phenotypes are rarely considered. We therefore undertook this exploratory study in order to examine possible associations between previously identified risk alleles for BD and the severity of negative symptoms in a first-episode schizophrenia (FES) cohort. Additionally, the inclusion of a neuroimaging component allowed us to investigate any associated neuroanatomical differences.
Previous schizophrenia GWAS have identified dozens of independent risk variants consistent with a polygenic inheritance model.23 However, few studies have investigated the association between specific SNPs and the negative symptom phenotype. A recent meta-analysis of GWAS identified a number of SNPs significantly associated with negative symptoms in schizophrenia, including multiple variants of BCL9 and 2 SNPs in the C9orf5 gene, among others.22 Other studies have implicated additional genes: a study on multiple variants of the DRD2 gene found weak associations between rs1236428 and negative symptoms,24 and another study including cognitive variables associated the MIR137 variant rs1625579 with severe negative symptoms and cognitive deficits.25
Although GWAS have provided invaluable insight into genetic risk for schizophrenia and other neuropsychiatric conditions, the power required to undertake such studies demands enormous sample sizes, and disease populations are typically heterogeneous, ignoring more nuanced clinical presentations.26 Evidence suggests that the risk for schizophrenia involves many genetic variants, each with small effects,27 and the size of cohorts required to identify individual SNPs with such small effects is prohibitive.28 Recent evidence, however, suggests that better homogeneity among cohorts could be more important than increasing sample sizes.29 In an effort to mitigate heterogeneity related to symptom trajectory and course of illness, a first-episode cohort is favourable. Negative symptoms can be reliably assessed during FEP, at which point factors known to influence negative symptoms, such as long-term medication use, extrapyramidal symptoms and lack of environmental stimulation, are less likely to play a role.30,31
The objective of this exploratory study was to assess whether previously identified risk genes for BD might have a phenotypic effect on patients with schizophrenia. Specifically, we sought to examine the potential effects of genotype on the severity of negative symptoms and to identify any associated neuroanatomical differences. We hypothesized that any risk genes associated with increased negative symptoms would also be associated with neuroanatomical abnormalities consistent with negative symptom severity.
Methods
Participants
Participants were part of a longitudinal outcome study of FEP treated in a specialized early intervention service, the Prevention and Early Intervention Program for Psychosis (PEPP-Montréal) at the Douglas Mental Health University Institute in Montreal, Canada. Individuals from the local catchment area presenting with affective or nonaffective psychosis were admitted to the program, provided they met the following inclusion criteria: age 18–35 years, no anti-psychotic medication taken in the past month or longer, and IQ higher than 70.32 Participants’ diagnoses were confirmed through clinical evaluations with experienced psychiatrists, and diagnoses were corroborated using the Structured Clinical Interview for DSM-IV (SCID-IV);33 only participants with diagnoses of schizophrenia or related spectrum disorders were included in this study. The Douglas Institute Human Ethics Review Board approved research protocols, and all patients who chose to participate in the study gave their written informed consent.
Instruments and assessment
All participants underwent full neuropsychological and symptom assessments. We used the Scale for the Assessment of Negative Symptoms (SANS) as a measure of negative symptom severity, and it was administered at 6 months from program entry, as per previous studies from our group.2,34 We also performed symptom evaluations at program entry; however, previous studies have noted that symptoms during the first 6 months after start of treatment can fluctuate due to introduction of medication and that negative symptoms in particular can fluctuate due to high levels of depression and acute positive symptoms at baseline.2 Negative symptoms measured at the 6-month time point are less likely to be influenced by these factors and therefore represent a more accurate measure of primary negative symptoms. Severity of negative symptoms was defined as total score on the SANS, excluding global items. The domain of attention on the SANS was also excluded from our analysis, as factor analyses from previous studies have shown that this domain, unlike others, loads on both negative and disorganization dimensions.35,36 We assessed depressive symptoms using the Calgary Depression Scale (CDS).37
Genetics
Prior to our analysis, participants included in this study were genotyped for a large number of SNPs associated with a myriad of factors and comorbidities (risk for schizophrenia, BD, or MDD; smoking behaviours; alcoholism; obesity). The DNA extraction was performed via blood and/or saliva sample, and genotyping was performed at the McGill University and Génome Québec Innovation Centre using Sequenom iPlex Gold Technology. For the purpose of this study, only those SNPs identified in previous GWAS as contributing significant risk for BD were considered (n = 21).38–41 The SNPs included in this analysis, including their associated gene(s) and GWAS reference, are listed in Table 1.
Table 1.
Single-nucleotide polymorphisms included in the analysis, and results of analysis of covariance with Scale for the Assessment of Negative Symptoms scores
| SNP | Chromosome | Position | Gene | Risk allele | Reference | F statistic | p value |
|---|---|---|---|---|---|---|---|
| rs4765913 | 12 | 2310730 | CACNA1C | A | Perlis et al.19 | 0.111 | 0.74 |
| rs10896135 | 11 | 66783531 | C11orf80 | G | 0.869 | 0.35 | |
| rs10994336 | 10 | 60420054 | ANK3 | T | 2.061 | 0.15 | |
| rs10994397 | 10 | 60519366 | ANK3 | T | 3.008 | 0.09 | |
| rs12576775 | 11 | 79366149 | TENM4 | G | 1.162 | 0.28 | |
| rs1006737 | 12 | 2236129 | CACNA1C | A | 0.054 | 0.82 | |
| rs1938526 | 10 | 60540625 | ANK3 | G | Zhang et al.20 | 0.49 | 0.49 |
| rs736408 | 3 | 52801338 | ITIH3 | C | Li et al.21 | 2.491 | 0.12 |
| rs2070615 | 12 | 48824388 | CACNB3 | G | 6.202 | 0.014 | |
| rs2175420 | 11 | 79412839 | TENM4 | T | 2.354 | 0.13 | |
| rs2176528 | 2 | 1.94E+08 | N/A | G | 1.388 | 0.24 | |
| rs3774609 | 3 | 53798876 | CACNA1D | T | 0.064 | 0.80 | |
| rs3845817 | 2 | 65531391 | N/A | T | 1.67 | 0.20 | |
| rs4660531 | 1 | 41374150 | FOXO6 | T | 5.854 | 0.017 | |
| rs6746896 | 2 | 96745212 | N/A | G | 0.53 | 0.47 | |
| rs7296288 | 12 | 49086185 | N/A | C | 0.157 | 0.69 | |
| rs7578035 | 2 | 98766429 | N/A | G | 1.363 | 0.25 | |
| rs9804190 | 10 | 60080073 | ANK3 | C | 0.015 | 0.90 | |
| rs11168751 | 12 | 48825355 | CACNB3 | G | 0.473 | 0.49 | |
| rs9371601 | 6 | 1.52E+08 | SYNE1 | T | 0.118 | 0.73 | |
| rs11030101 | 11 | 27659197 | BDNF, BDNF-AS | T | Xu et al.22 | 0.424 | 0.52 |
N/A = not applicable; SNP = single-nucleotide polymorphism.
Image processing
A subset of participants underwent a T1 structural MRI scan acquired using a 1.5 T Siemens MRI scanner at the Montreal Neurological Institute under the following parameters: repetition time (TR) 22 ms, echo time (TE) 9.2 ms, flip angle 30°, field of view (FOV) 256 mm × 204 mm, 180 sagittal slices, voxel size 1 mm3. Images were acquired on average 4.8 months after program entry. Following a visual inspection, 5 scans were rejected owing to blurring and/or motion artifacts. The MRI images were converted to MINC and preprocessed via the CIVET pipeline, version 1.1.10.42 Using the LONI Probabilistic Brain Atlas (LPBA40), MRI images were automatically segmented into 24 bilateral regions of interest, with mean cortical thickness and total surface area calculated at each region.43 Regions were subsequently grouped by lobe, with each hemisphere analyzed individually; regions and lobe groupings can be found in Table 2.
Table 2.
Neuroanatomical regions grouped by lobe
| Lobe; region |
|---|
| Frontal lobe |
| Superior frontal gyrus |
| Middle frontal gyrus |
| Inferior frontal gyrus |
| Precentral gyrus |
| Middle orbitofrontal gyrus |
| Lateral orbitofrontal gyrus |
| Gyrus rectus |
| Parietal lobe |
| Postcentral gyrus |
| Superior parietal gyrus |
| Supramarginal gyrus |
| Angular gyrus |
| Precuneus |
| Limbic lobe |
| Cingulate gyrus |
| Hippocampus |
| Occipital lobe |
| Superior occipital gyrus |
| Middle occipital gyrus |
| Inferior occipital gyrus |
| Cuneus |
| Temporal lobe |
| Superior temporal gyrus |
| Middle temporal gyrus |
| Inferior temporal gyrus |
| Parahippocampal gyrus |
| Lingual gyrus |
| Fusiform gyrus |
Statistical analysis
Participants were coded for each SNP as 1 or 0, with 1 indicating the presence of the risk allele (i.e., risk allele heterozygous or homozygous) and 0 representing lack of the risk allele. In order to assess whether genotype had an impact on negative symptom severity, we performed an analysis of covariance (ANCOVA) for each SNP, with genotype as the independent variable, total SANS score as the dependent variable, and age and sex as covariates.
We performed an additional analysis on 61 structural MRI T1 scans to examine associations between genotype and neuroanatomical differences for those SNPs that achieved significance (p < 0.05) on the previous ANCOVA (SANS × genotype). To examine structural differences by genotype, a series of multivariate ANCOVAs (MANCOVAs) were performed for all regions within each lobe, with genotype as the independent variable and mean cortical thickness and total surface area as the dependent variables, covaried with age and sex. Regions within any lobe whose MANCOVA test achieved significance (p < 0.05) were subsequently tested in a series of univariate ANCOVAs, which we corrected for multiple comparisons using the Bonferroni method.
Results
Sample
We included 133 patients with FES in our analyses; 66 of them underwent structural MRI. The demographic and clinical characteristics of all participants are summarized in Table 3.
Table 3.
Clinical and demographic characteristics of participants
| Group; mean ± SD or no. | ||
|---|---|---|
|
|
||
| Characteristic* | All participants n = 133 | Subset with MRI scan n = 61 |
| Age, yr | 22.5 ± 3.9 | 22.9 ± 3.8 |
| Sex, male:female | 105:28 | 47:14 |
| SANS total score, excluding attention† | 23.62 ± 13.7 | 21.49 ± 12.7 |
| CDS total score† | 2.07 ± 2.9 | 2.08 ± 2.9 |
| Duration of illness, mo† (n = 131) | 6.86 ± 1.67 | 6.87 ± 1.86 |
| Completed education, yr (n = 130) | 11 ± 2.3 | 10.69 ± 2.04 |
| Antipsychotic dosage, CPZ equivalent† (n = 127) | 319.42 ± 249.96 | 325.63 ± 262.69 |
| Taking antidepressants, yes:no (n = 127) | 20:107 | 11:50 |
| Taking benzodiazepine, yes:no (n = 127) | 7:120 | 4:57 |
| Taking anticholinergics, yes:no (n = 127) | 8:119 | 2:59 |
| Socioeconomic status‡ (n = 104) | 4.13 ± 0.89 | 4.14 ± 0.9 |
CDS = Calgary Depression Scale; CPZ = chlorpromazine; SANS = Scale for the Assessment of Negative Symptoms; SD = standard deviation.
Data were limited owing to missing questionnaires, and per-item n is shown.
Measured at 6 mo from program entry.
Calculated according to the Hollingshead Four Factor Index for Socioeconomic Status.
Genotype and negative symptoms
The full results of this analysis are presented in Table 1. Although 2 SNPs achieved significance, rs2070615 was excluded owing to heavily unbalanced group sizes (only 24 of 133 participants lacked the risk allele). A significant association was observed between rs4660531 (FOXO6) genotype and SANS scores (Cohen d = 0.46, F = 5.854, p = 0.017), indicating that participants with the CC genotype (n = 72) presented significantly higher negative symptoms than carriers of the risk allele A (n = 61; Fig. 1). Participant groups did not significantly differ in age, sex, or level of depression (all p > 0.05; Table 4).
Fig. 1.
Mean Scale for the Assessment of Negative Symptoms (SANS) scores per FOX06 genotype group. Total scores on the SANS can range from 0 to 90, where a higher score denotes more severe negative symptoms.
Table 4.
Clinical and demographic characteristics, by FOXO6 rs4660531 genotype distribution
| Group; mean ± SD or no. | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | With risk allele, n = 61 | Without risk allele, n = 72 | Statistic | p value |
| Age, yr | 22.3 ± 4.08 | 22.6 ± 3.9 | F = 0.191 | 0.66 |
| Sex, male:female | 49:12 | 56:16 | χ2 = 0.129 | 0.72 |
| CDS total score | 2.16 ± 3.05 | 1.98 ± 2.8 | F = 0.094 | 0.76 |
| Duration of illness, mo* | 6.8 ± 1.33 | 6.91 ± 1.93 | F = 0.151 | 0.70 |
| Completed education, yr | 11.41 ± 2.45 | 10.64 ± 2.11 | F = 3.714 | 0.06 |
| Antipsychotic dosage, CPZ equivalents* | 333.63 ± 265.97 | 306.29 ± 235.49 | F = 0.377 | 0.54 |
| Socioeconomic status† | 4.02 ± 0.95 | 4.23 ± 0.83 | χ2 = 2.885 | 0.41 |
CDS = Calgary Depression Scale; CPZ = chlorpromazine; F = female; M = male; SD = standard deviation.
Measured 6 mo from program entry.
Socioeconomic status calculated according to the Hollingshead Four Factor Index for Socioeconomic Status.
Genotype and neuroanatomy
The FOXO6 rs4660531 genotype showed a significant effect on right frontal lobe surface area (F = 1.727, p = 0.049). Subsequent univariate ANCOVA tests localized the effect to the right middle orbitofrontal gyrus (MOF), part of the orbitofrontal cortex (OFC; Cohen d = 0.69, F = 7.289, p = 0.009, Bonferroni-corrected), indicating that participants with the CC genotype (n = 29) had significantly smaller surface area within the right MOF than carriers of the risk allele A (n = 32; Fig. 2).
Fig. 2.
(Left) Example sagittal and transverse plane of an MRI of 1 participant, on which the right middle orbitofrontal gyrus (MOF; as defined by the LPBA40 atlas) has been labelled. (Right) Mean right MOF surface area per genotype group.
Discussion
Our analysis revealed a significant effect of the FOXO6 major allele C on both negative symptoms and surface area of the right MOF in a sample of young people with FES. Participants with the CC genotype — those lacking the risk allele A — exhibited higher negative symptoms and reduced MOF surface area. Although the mechanism by which the FOXO6 genotype affects patients with schizophrenia is unclear, our analyses indicate that the FOXO6 risk allele appears to protect patients with schizophrenia from more severe negative symptoms and associated MOF surface area reduction. It is curious that the risk allele would confer a positive effect; however, since our interest in FOXO6 comes from a GWAS examining risk for BD, it is possible that the risk allele would be associated with a negative phenotype (e.g., mania) in that population. In addition, the effects of FOXO6 in schizophrenia may be limited to modulating symptom profile; it may not confer risk for the disorder.
FOXO6 is not a particularly well-studied gene and has rarely been included in studies on neuropsychiatric disorders. The gene was included in our analysis owing to its significance in a recent GWAS of BD;40 however, to our knowledge no candidate gene studies on BD including FOXO6 have been conducted to date. FOXO6 codes for the Fox-O6 transcription factor, a member of the O-group of the forkhead (Fox) transcription factor family.44 Fox-O transcription factors are mediated by protein kinase B (PKB)/Akt and phosphoinositide 3-kinase (PI3K) pathways, suggesting potential associations between Fox-O and cellular metabolism, apoptosis and other cellular processes.44 The Akt signalling pathway has been associated with schizophrenia in a number of studies, showing response to antipsychotic agents45 and abnormalities in the brains of patients with schizophrenia.46 A handful of studies suggest that Fox-O6 is enriched in areas of the nucleus accumbens, cingulate cortex, parts of the amygdala44 and the hippocampus;47 however, as one of the more recently discovered Fox-O isoforms, the specific functions of Fox-O6 are not well researched.
The Fox family has diverse functions throughout the body, and certain isoforms have been previously associated with mental illness. A study by Spaniel and colleagues48 investigated the potential link between FOXP2 — a Fox family gene previously associated with the development of speech and language — and schizophrenia, hypothesizing a connection between Fox-P2 and schizophrenia owing to the underlying deficits in language processing inherent to the disease.48 These investigators identified reductions in grey matter concentrations in patients with schizophrenia carrying the C risk allele of rs2396753 (FOXP2); however, the clinical presentation of the disease, as measured by the Positive And Negative Syndrome Scale (PANSS), did not differ between genotype groups.
A more recent study by Zheng and colleagues49 established an association between lithium, primarily used in the treatment of BD, and the Fox-O isoform Fox-O1.49 As a model of neuropsychiatric disorders, such as schizophrenia and BD, Zheng’s group treated mice with amphetamine and subsequently with lithium. Mice treated with amphetamine exhibited hyperactivity and impaired prepulse inhibition (PPI) of startle — an effect often seen in BD and schizophrenia populations — as well as decreased levels of Fox-O1 in the striatum; subsequent treatment with lithium reversed this effect. Additionally, pretreatment of mice with lithium prevented the amphetamine-induced Fox-O1 reduction and associated hyperactivity and PPI deficits. The association between the increase of bipolar-like behaviour and decreased levels of Fox-O1 suggests an association between the Fox family of transcription factors and BD.
Multiple studies have investigated the role of FOXO6 in oxidative stress, and this may be a potential mechanism by which the gene modulates negative symptoms in patients with schizophrenia. In their 2003 study, Burgering and Medema50 noted that activation of Fox-O transcription factors via protein kinase B produced an increase in manganese superoxide dismutase (MnSOD), one of the antioxidant enzymes critical in protecting cells from the effects of oxidative stress by reducing superoxide anions. A recent study by Kim and colleagues51 elaborated on this finding, noting that the upregulation of P13K/Akt signalling triggered by increased oxidative stress led to reduced levels of both Fox-O6 and MnSOD. Multiple studies have identified negative correlations between symptom severity in patients with schizophrenia and MnSOD levels,52–54 whereas Sirota and colleagues55 found a positive correlation between increased superoxide anion levels and negative symptoms in a group of patients with schizophrenia. It is important to note, however, that a candidate gene study investigating the role of the FOXO6 genotype on oxidative stress has not been conducted.
The association uncovered in our analysis between negative symptom severity and the OFC is consistent with previous findings from our research group. Two studies on FEP cohorts with persistent negative symptoms (PNS) — a clinical subgroup of schizophrenia defined by enduring negative symptoms — identified deficits in this region. The first, a voxel-based morphometry (VBM) study, found that patients with PNS had smaller grey matter volume in the right frontal medial-orbital gyrus.56 A subsequent study looking at cortical thickness noted that patients with PNS exhibited cortical thinning in the left orbitofrontal gyrus compared with non-PNS patients.57 Additionally, frontal lobe impairment associated with oxidative stress has been shown to affect negative symptoms in patients with schizophrenia. One study found reduced cerebral blood flow in the right OFC within a group of deficit syndrome patients (a subtype of schizophrenia characterized by enduring negative symptoms),58 and another study using a mouse model for schizophrenia noted dysfunctional behaviours consistent with negative symptoms in response to prefrontal oxidative stress.59
Limitations
An important limitation to this study is the lack of appropriate corrections for multiple comparisons. Unfortunately, without substantially increasing our sample size, there is no acceptable way to enhance the statistical rigor of our results. The results of a power calculation revealed that with a power value of 0.8 and 21 SNPs included in the analysis, the required sample size to achieve significance after properly correcting for multiple comparisons would be roughly 300 participants, which is more than double our actual sample size. To undertake such a study with as many participants would likely require multisite collaboration, which would reduce the quality and homogeneity of our participants. A great strength of this study is the high-quality sample; hailing from a single first-episode clinic, limited medication exposure, detailed symptom evaluations and a well-defined sample is arguably more valuable than greater numbers.29
Additionally, this multimodal study produced significant results associating the FOXO6 SNP with both negative symptoms (via the SANS scale) and neuroanatomical abnormalities, reducing the likelihood of a spurious result. In the broader context of the results, the SNPs in consideration have passed the rigorous requirements of GWAS, and the brain regions implicated have a strong history with negative symptoms.
Finally, our analysis relates FOXO6 to SANS scores and to surface area, but the direct association between SANS scores and surface area was not discussed. This association was in fact examined, but did not yield significant results. This is not surprising, however, since previous studies have suggested that negative symptoms do not represent a single homogeneous symptom, but perhaps multiple psychopathological constructs influenced by a variety of systems and genetic variants.60 This suggests that what manifests as behaviourally similar negative symptoms may be caused by abnormalities in disparate underlying pathways.
As discussed, the statistical results presented are uncorrected for multiple comparisons, as the exploratory nature of this study — lacking a priori hypotheses about the effects of these specific risk genes — required considering a large number of variables and made appropriate corrections for multiple comparison impossible. Although we cannot exclude the possibility that this is a false positive, FOXO6 emerges from a robust GWAS as a BD risk gene and is shown here to be strongly associated with neuroanatomical differences in a region highly associated with negative symptoms. This study is also limited by the lack of a control group, which would be necessary to examine whether the observed neuroanatomical differences associated with FOXO6 genotype are unique to this clinical population. Finally, the proposed mechanism of FOXO6 related to oxidative stress, while plausible, is merely theoretical. Subsequent studies on FOXO6 would benefit from measuring MnSOD levels and other metabolic indicators of oxidative stress.
Conclusion
Although the specific mechanisms by which FOXO6 may be modulating negative symptoms are unclear, associations between this BD risk gene and negative symptoms in schizophrenia are apparent, adding mounting evidence to the notion that negative symptoms represent an important underlying dimension of psychotic disorders. The association between FOXO6 and the Akt/P13K signalling pathway is of particular interest owing to its downstream effects on cAMP response element binding protein and brain-derived neurotrophic factor61 and prior associations with schizophrenia,45 depression62 and oxidative stress.63 Additionally, many antipsychotic drugs increase phosphorylation of Akt as well as the associated GSK-3b,45 whose phosphorylation is mediated by the Wnt signalling pathway, associated with negative symptom risk gene BCL9.22 The Akt/P13K and Wnt signalling pathways are already exciting avenues for exploring the mechanisms behind negative symptoms, and future studies might benefit from examining the role of Fox-O isoforms in these chains. Finally, although previous research has provided a number of potential genetic variants associated with negative symptoms, future studies are needed to identify and understand additional bio-markers — genetic and other — that may associate with negative symptoms across psychotic disorders.
Acknowledgements
The authors thank Kathleen MacDonald and members of the Lepage and Chakravarty laboratories, notably Raihaan Patel and Gabriel Devenyi. The study was supported by operating grants from the Canadian Institutes of Health Research (CIHR; #68961) and the Sackler Foundation to M. Lepage, R. Joober and A. Malla. M. Chakravarty is supported by CIHR, the Natural Sciences and Engineering Research Council of Canada (NSERC), and the Weston Brain Institute. Salary awards include Fonds de la Recherche en Santé du Québec (M. Lepage, R. Joober, M. Chakravarty), James McGill Professorship (M. Lepage) and Canada Research Chairs Program (A. Malla). The funding sources had no role in study design; the collection, analysis, or interpretation of data; the writing of the paper; or in the decision for publication.
Footnotes
Competing interests: See jpn.ca/about for R. Joober. M. Lepage reports grants and personal fees from Otsuka Canada, Lundbeck and Janssen-Ortho, outside the submitted work. No other competing interests declared.
Contributors: R. Joober, M. Chakravarty and M. Lepage designed the study. S. Sengupta, R. Joober, A. Malla and M. Lepage acquired the data, which all authors analyzed. J. Shenker, A. Malla and M. Chakravarty wrote the article, which all authors reviewed and approved for publication.
References
- 1.Chang WC, Hui CL, Tang JY, et al. Persistent negative symptoms in first-episode schizophrenia: a prospective three-year follow-up study. Schizophr Res. 2011;133:22–8. doi: 10.1016/j.schres.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Hovington CL, Bodnar M, Joober R, et al. Identifying persistent negative symptoms in first episode psychosis. BMC Psychiatry. 2012;12:224. doi: 10.1186/1471-244X-12-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ameen S, Ram D. Negative symptoms in the remission phase of bipolar disorder. German Journal of Psychiatry. 2007;10:1–7. [Google Scholar]
- 4.Toomey R, Faraone SV, Simpson JC, et al. Negative, positive, and disorganized symptom dimensions in schizophrenia, major depression, and bipolar disorder. J Nerv Ment Dis. 1998;186:470–6. doi: 10.1097/00005053-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Malaspina D, Goetz RR, Yale S, et al. Relation of familial schizophrenia to negative symptoms but not to the deficit syndrome. Am J Psychiatry. 2000;157:994–1003. doi: 10.1176/appi.ajp.157.6.994. [DOI] [PubMed] [Google Scholar]
- 6.Chen LS, Rice TK, Thompson PA, et al. Familial aggregation of clinical and neurocognitive features in sibling pairs with and without schizophrenia. Schizophr Res. 2009;111:159–66. doi: 10.1016/j.schres.2009.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellivier F, Geoffroy PA, Scott J, et al. Biomarkers of bipolar disorder: Specific or shared with schizophrenia? Front Biosci (Elite Ed) 2013;5:845–63. doi: 10.2741/e665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mortensen PB, Pedersen CB, Melbye M, et al. Individual and familial risk factors for bipolar affective disorders in Denmark. Arch Gen Psychiatry. 2003;60:1209–15. doi: 10.1001/archpsyc.60.12.1209. [DOI] [PubMed] [Google Scholar]
- 9.Cross-Disorder Group of the Psychiatric Genomics. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9. doi: 10.1016/S0140-6736(12)62129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross-Disorder Group of the Psychiatric Genomics. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45:984–94. doi: 10.1038/ng.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maier R, Moser G, Chen GB, et al. Joint analysis of psychiatric disorders increases accuracy of risk prediction for schizophrenia, bipolar disorder, and major depressive disorder. Am J Hum Genet. 2015;96:283–94. doi: 10.1016/j.ajhg.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Potuzak M, Ravichandran C, Lewandowski KE, et al. Categorical vs dimensional classifications of psychotic disorders. Compr Psychiatry. 2012;53:1118–29. doi: 10.1016/j.comppsych.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arndt S, Alliger RJ, Andreasen NC. The distinction of positive and negative symptoms. The failure of a two-dimensional model. Br J Psychiatry. 1991;158:317–22. doi: 10.1192/bjp.158.3.317. [DOI] [PubMed] [Google Scholar]
- 15.Silver H, David D, Kaplan M, et al. Factor analysis of schizophrenic symptoms and comparison of different rating scales. Schizophr Res. 1993;10:67–75. doi: 10.1016/0920-9964(93)90078-w. [DOI] [PubMed] [Google Scholar]
- 16.Klimidis S, Stuart GW, Minas IH, et al. Positive and negative symptoms in the psychoses. Re-analysis of published SAPS and SANS global ratings. Schizophr Res. 1993;9:11–8. doi: 10.1016/0920-9964(93)90003-2. [DOI] [PubMed] [Google Scholar]
- 17.Maziade M, Roy MA, Martinez M, et al. Negative, psychoticism, and disorganized dimensions in patients with familial schizophrenia or bipolar disorder: continuity and discontinuity between the major psychoses. Am J Psychiatry. 1995;152:1458–63. doi: 10.1176/ajp.152.10.1458. [DOI] [PubMed] [Google Scholar]
- 18.Minas IH, Stuart GW, Klimidis S, et al. Positive and negative symptoms in the psychoses: multidimensional scaling of SAPS and SANS items. Schizophr Res. 1992;8:143–56. doi: 10.1016/0920-9964(92)90031-y. [DOI] [PubMed] [Google Scholar]
- 19.Perlis RH, Purcell S, Fagerness J, et al. Family-based association study of lithium-related and other candidate genes in bipolar disorder. Arch Gen Psychiatry. 2008;65:53–61. doi: 10.1001/archgenpsychiatry.2007.15. [DOI] [PubMed] [Google Scholar]
- 20.Zhang P, Xiang N, Chen Y, et al. Family-based association analysis to finemap bipolar linkage peak on chromosome 8q24 using 2,500 genotyped SNPs and 15,000 imputed SNPs. Bipolar Disord. 2010;12:786–92. doi: 10.1111/j.1399-5618.2010.00883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J, Zhou G, Ji W, et al. Common variants in the BCL9 gene conferring risk of schizophrenia. Arch Gen Psychiatry. 2011;68:232–40. doi: 10.1001/archgenpsychiatry.2011.1. [DOI] [PubMed] [Google Scholar]
- 22.Xu C, Aragam N, Li X, et al. BCL9 and C9orf5 are associated with negative symptoms in schizophrenia: meta-analysis of two genome-wide association studies. PLoS One. 2013;8:e51674. doi: 10.1371/journal.pone.0051674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertolino A, Fazio L, Caforio G, et al. Functional variants of the dopamine receptor D2 gene modulate prefronto-striatal phenotypes in schizophrenia. Brain. 2009;132:417–25. doi: 10.1093/brain/awn248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Green MJ, Cairns MJ, Wu J, et al. Genome-wide supported variant MIR137 and severe negative symptoms predict membership of an impaired cognitive subtype of schizophrenia. Mol Psychiatry. 2013;18:774–80. doi: 10.1038/mp.2012.84. [DOI] [PubMed] [Google Scholar]
- 26.Wang Q, Xiang B, Deng W, et al. Genome-wide association analysis with gray matter volume as a quantitative phenotype in first-episode treatment-naive patients with schizophrenia. PLoS One. 2013;8:e75083. doi: 10.1371/journal.pone.0075083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.International Schizophrenia Consortium. Purcell SM, Wray NR, et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460:748–52. doi: 10.1038/nature08185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lencz T, Guha S, Liu C, et al. Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat Commun. 2013;4:2739. doi: 10.1038/ncomms3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manchia M, Cullis J, Turecki G, et al. The impact of phenotypic and genetic heterogeneity on results of genome wide association studies of complex diseases. PLoS One. 2013;8:e76295. doi: 10.1371/journal.pone.0076295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galderisi S, Mucci A, Bitter I, et al. Persistent negative symptoms in first episode patients with schizophrenia: results from the European First Episode Schizophrenia Trial. Eur Neuropsychopharmacol. 2013;23:196–204. doi: 10.1016/j.euroneuro.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 31.Malla AK, Norman RM, Takhar J, et al. Can patients at risk for persistent negative symptoms be identified during their first episode of psychosis? J Nerv Ment Dis. 2004;192:455–63. doi: 10.1097/01.nmd.0000131804.34977.c1. [DOI] [PubMed] [Google Scholar]
- 32.Iyer S, Jordan G, MacDonald K, et al. Early intervention for psychosis: a Canadian perspective. J Nerv Ment Dis. 2015;203:356–64. doi: 10.1097/NMD.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 33.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P & SCID-I/NP), Version 2. New York: New York Psychiatric Institute, Biometrics Research; 1998. [Google Scholar]
- 34.Buchy L, Bodnar M, Malla A, et al. A 12-month outcome study of insight and symptom change in first-episode psychosis. Early Interv Psychiatry. 2010;4:79–88. doi: 10.1111/j.1751-7893.2010.00166.x. [DOI] [PubMed] [Google Scholar]
- 35.Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: an item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res. 1999;38:13–26. doi: 10.1016/s0920-9964(99)00003-1. [DOI] [PubMed] [Google Scholar]
- 36.Malla AK, Jatinder J, Takhar R, et al. Negative symptoms in first episode non-affective psychosis. Acta Psychiatr Scand. 2002;105:431–9. doi: 10.1034/j.1600-0447.2002.02139.x. [DOI] [PubMed] [Google Scholar]
- 37.Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res. 1990;3:247–51. doi: 10.1016/0920-9964(90)90005-r. [DOI] [PubMed] [Google Scholar]
- 38.Psychosis Endophenotypes International. A genome-wide association analysis of a broad psychosis phenotype identifies three loci for further investigation. Biol Psychiatry. 2014;75:386–97. doi: 10.1016/j.biopsych.2013.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferreira MA, O’Donovan MC, Meng YA, et al. Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet. 2008;40:1056–8. doi: 10.1038/ng.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Psychiatric GWAS Consortium Bipolar Disorder Working Group. Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nat Genet. 2011;43:977–83. doi: 10.1038/ng.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pae CU, Chisea A, Porcelli S, et al. Influence of BDNF variants on diagnosis and response to treatment in patients with major depression, bipolar disorder and schizophrenia. Neuropsychobiology. 2012;65:1–11. doi: 10.1159/000327605. [DOI] [PubMed] [Google Scholar]
- 42.Ad-Dab’bagh Y, Einarson D, Lyttelton O, et al. The CIVET image-processing environment: a fully automated comprehensive pipeline for anatomical neuroimaging research. 12th Annual Meeting of the Organization for Human Brain Mapping; 2006; Florence, Italy. [Google Scholar]
- 43.Shattuck DW, Mirza M, Adisetiyo V, et al. Construction of a 3D probabilistic atlas of human cortical structures. Neuroimage. 2008;39:1064–80. doi: 10.1016/j.neuroimage.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jacobs FM, Van der Heide LP, Wijchers PJ, et al. FoxO6, a novel member of the FoxO class of transcription factors with distinct shuttling dynamics. J Biol Chem. 2003;278:35959–67. doi: 10.1074/jbc.M302804200. [DOI] [PubMed] [Google Scholar]
- 45.Zheng W, Wang H, Zeng Z, et al. The possible role of the Akt signaling pathway in schizophrenia. Brain Res. 2012;1470:145–58. doi: 10.1016/j.brainres.2012.06.032. [DOI] [PubMed] [Google Scholar]
- 46.Emamian ES. AKT/GSK3 signaling pathway and schizophrenia. Front Mol Neurosci. 2012;5:33. doi: 10.3389/fnmol.2012.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salih DA, Rashid AJ, Colas D, et al. FoxO6 regulates memory consolidation and synaptic function. Genes Dev. 2012;26:2780–801. doi: 10.1101/gad.208926.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spaniel F, Horácek J, Tintera J, et al. Genetic variation in FOXP2 alters grey matter concentrations in schizophrenia patients. Neurosci Lett. 2011;493:131–5. doi: 10.1016/j.neulet.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 49.Zheng W, Zeng Z, Bhardwaj SK, et al. Lithium normalizes amphetamine-induced changes in striatal FoxO1 phosphorylation and behaviors in rats. Neuroreport. 2013;24:560–5. doi: 10.1097/WNR.0b013e3283623725. [DOI] [PubMed] [Google Scholar]
- 50.Burgering BM, Medema RH. Decisions on life and death: FOXO forkhead transcription factors are in command when PKB/Akt is off duty. J Leukoc Biol. 2003;73:689–701. doi: 10.1189/jlb.1202629. [DOI] [PubMed] [Google Scholar]
- 51.Kim DH, Park MH, Chung KW, et al. The essential role of FoxO6 phosphorylation in aging and calorie restriction. Age (Dordr) 2014;36:9679. doi: 10.1007/s11357-014-9679-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Michel TM, Thome J, Martin D, et al. Cu, Zn- and Mn-superoxide dismutase levels in brains of patients with schizophrenic psychosis. J Neural Transm (Vienna) 2004;111:1191–201. doi: 10.1007/s00702-004-0160-9. [DOI] [PubMed] [Google Scholar]
- 53.Zhang XY, Chen DC, Xiu MH, et al. Clinical symptoms and cognitive impairment associated with male schizophrenia relate to plasma manganese superoxide dismutase activity: a case-control study. J Psychiatr Res. 2013;47:1049–53. doi: 10.1016/j.jpsychires.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 54.Zhang XY, Chen DC, Xiu MH, et al. Cognitive function, plasma MnSOD activity, and MnSOD Ala-9Val polymorphism in patients with schizophrenia and normal controls. Schizophr Bull. 2014;40:592–601. doi: 10.1093/schbul/sbt045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sirota PR, Gavrieli R, Wolach B. Overproduction of neutrophil radical oxygen species correlates with negative symptoms in schizophrenic patients: parallel studies on neutrophil chemotaxis, superoxide production and bactericidal activity. Psychiatry Res. 2003;121:123–32. doi: 10.1016/s0165-1781(03)00222-1. [DOI] [PubMed] [Google Scholar]
- 56.Benoit A, Bodnar M, Malla AK, et al. The structural neural substrates of persistent negative symptoms in first-episode of non-affective psychosis: a voxel-based morphometry study. Front Psychiatry. 2012;3:42. doi: 10.3389/fpsyt.2012.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bodnar M, Hovington CL, Buchy L, et al. Cortical thinning in temporo-parietal junction (TPJ) in non-affective first-episode of psychosis patients with persistent negative symptoms. PLoS One. 2014;9:e101372. doi: 10.1371/journal.pone.0101372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kanahara N, Sekine Y, Haraquchi T, et al. Orbitofrontal cortex abnormality and deficit schizophrenia. Schizophr Res. 2013;143:246–52. doi: 10.1016/j.schres.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 59.Johnson AW, Jaaro-Peled H, Shahani N, et al. Cognitive and motivational deficits together with prefrontal oxidative stress in a mouse model for neuropsychiatric illness. Proc Natl Acad Sci U S A. 2013;110:12462–7. doi: 10.1073/pnas.1307925110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Galderisi S, Merlotti E, Mucci A. Neurobiological background of negative symptoms. Eur Arch Psychiatry Clin Neurosci. 2015;265:543–58. doi: 10.1007/s00406-015-0590-4. [DOI] [PubMed] [Google Scholar]
- 61.Du K, Montminy M. CREB is a regulatory target for the protein kinase Akt/PKB. J Biol Chem. 1998;273:32377–9. doi: 10.1074/jbc.273.49.32377. [DOI] [PubMed] [Google Scholar]
- 62.Yu H, Chen ZY. The role of BDNF in depression on the basis of its location in the neural circuitry. Acta Pharmacol Sin. 2011;32:3–11. doi: 10.1038/aps.2010.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang X, McCullough KD, Franke TF, et al. Epidermal growth factor receptor-dependent Akt activation by oxidative stress enhances cell survival. J Biol Chem. 2000;275:14624–31. doi: 10.1074/jbc.275.19.14624. [DOI] [PubMed] [Google Scholar]