Abstract
AIM
To explore the association between Helicobacter pylori (H. pylori) infection and obesity/weight gain in a Chinese population.
METHODS
Our primary outcome was the change in body mass index (BMI). The generalized linear models were used to explore the association between H. pylori infection and the change of BMI, and the logistic regression models were used to explore the association between H. pylori infection and obesity.
RESULTS
A total of 3039 subjects were recruited and analyzed, of which 12.8% were obese. The prevalence of H. pylori infection was 53.9% (1639/3039) overall and 54.6% (212/388) in the obese subjects. The change of BMI in the H. pylori (+) group was not significantly higher than that in the H. pylori (-) group after adjustment for potential confounding factors [RR = 0.988, 95%CI: 0.924-1.057, P = 0.729]. The prevalence of obesity decreased 1.1% in the H. pylori (+) group and 0.5% in the H. pylori (-) group. The RR of H. pylori infection for obesity was 0.831 (95%CI: 0.577-1.197, P = 0.321) after the adjustment.
CONCLUSION
H. pylori infection was not associated with overweight/obesity observed from the retrospective study in this Chinese population.
Keywords: Obesity, Helicobacter pylori, Retrospective study, China
Core tip: The association between Helicobacter pylori (H. pylori) infection and obesity/weight gain is still unclear and controversial. We performed this retrospective study with a large sample size to explore the association between H. pylori infection and obesity/weight gain in Chinese people. The change in body mass index and the prevalence of obesity over two years in the H. pylori (+) group were not significantly higher than those in the H. pylori (-) group. We concluded that H. pylori infection was not associated with overweight/obesity observed from this study of Chinese people.
INTRODUCTION
Obesity is defined as excessive fat accumulation that may impair health. The World Health Organization estimated that over 600 million people in the world were obese in the year 2014. The worldwide prevalence of obesity more than doubled between 1980 and 2014. Obesity is associated with infectious diseases, such that certain infections may trigger an increase in adiposity, such as human adenovirus 36, H1N1/influenza virus, human immunodeficiency virus, and Helicobacter pylori (H. pylori)[1].
H. pylori is one of the most common human infections, and it is estimated that more than half of the world’s population are infected[2]. H. pylori has been linked to gastritis, gastric ulcers and gastric cancer[3-5]. The association between H. pylori and obesity/weight gain remains unclear and controversial.
The prevalence of H. pylori infection was reported to be from 8.7% to 85.5%[6]. A lower prevalence of H. pylori infection was found in obese patients than in the general population[6]. Other studies have reported a higher H. pylori prevalence in obese patients[7,8]. The systematic review by Dhurandhar et al[1] reported an increase in weight gain or an increase in the biomarkers associated with weight gain after H. pylori eradication, and most cross-sectional studies found evidence of a higher prevalence of H. pylori infection in obese individuals or metabolic impairment in the presence of the infection.
One study indicated an inverse relationship between morbid obesity and H. pylori seropositivity, leading to the hypothesis that the absence of H. pylori infection during childhood may enhance the risk of developing morbid obesity[9]. The significant increase in body mass index (BMI) observed after eradication of H. pylori highlights a possible inverse correlation between H. pylori infection and obesity[10,11]. Several studies did not find any influence of bacterial eradication on body weight[12,13]. In a large randomized controlled study, Lane and colleagues found a significant increase in body mass following eradication of H. pylori in a European population[10]. A meta-analysis of 18 observational studies including 10000 subjects found a higher body mass index among H. pylori-positive subjects compared with H. pylori-negative subjects[14]. A cross-sectional study showed that H. pylori infection was significantly and positively associated with overweight/obesity in a Chinese population[15]. Reports from different areas and countries were not consistent with each other, and most were cross-sectional studies. It is therefore necessary to further explore the true association between H. pylori infection and obesity.
Therefore, we performed this retrospective study to explore the association between H. pylori infection and obesity/weight gain in a Chinese population.
MATERIALS AND METHODS
Study design and participants
This observational retrospective study was performed at the Aerospace Center Hospital in Beijing, China. The data of all the subjects from a certain unit who underwent health examination in 2012 were retrieved from the registration system. The subjects without H. pylori detection results or data regarding height/weight were excluded. We then searched the data regarding height and weight of the same patient population in 2013.
We performed a chart review of all recruited subjects to collect the information regarding demographic characteristics, underlying diseases (diabetes, hypertension and coronary heart disease), and laboratory test results, including low density lipoprotein (LDL), high density lipoprotein (HDL), triglycerides (TG), total cholesterol (TC) and fasting blood-glucose (FBG). The height and weight of all the subjects were measured at baseline and at 1-year follow-up. H. pylori status was estimated by enzyme linked immunosorbent assay (ELISA) for anti-H. pylori IgG and IgM. This study was performed with the approval of the Ethical Committees of the hospital. The methods were carried out in accordance with the approved guidelines. At recruitment, written informed consent was obtained from all subjects.
Outcomes
Our primary outcome was the change in BMI. The secondary outcome was the prevalence of obesity.
Statistical analysis
BMI was calculated as the weight (kg) divided by the square of the height (m). Obesity was defined as BMI equal to or greater than 28 kg/m2, and overweight was defined as BMI equal to or greater than 24 kg/m2 and less than 28 kg/m2, as recommended by the Working Group on Obesity in China[16]. Descriptive statistics were performed, with continuous variables summarized as median and range and categorical variables as frequencies and proportions. The statistical significance between groups was tested using the χ2-test or Fisher’s exact test for categorical variables and the independent t test for continuous variables. Generalized linear models were used to explore the association between H. pylori infection and the change in BMI. Logistic regression models were used to explore the association between H. pylori infection and obesity. The variables of age, sex, marital status, underlying disease, LDL, HDL, TGs, TC and FBG were adjusted in the above models. Risk ratios (RRs) and their 95%CIs were estimated. A two-sided P value < 0.05 was considered statistically significant. All analyses were performed using Stata 12.0 (Stata Corp LP, College Station, TX, United States).
RESULTS
Subjects
A total of 16462 subjects participated in the health examination at the hospital. The diagram of the selection of subjects in the study is shown in Figure 1. Among all the subjects, 13390 were excluded due to the absence of H. pylori detection results or BMI data, and 33 (1.1%) subjects were lost to follow-up. Finally, 3039 subjects were recruited and analyzed.
Figure 1.
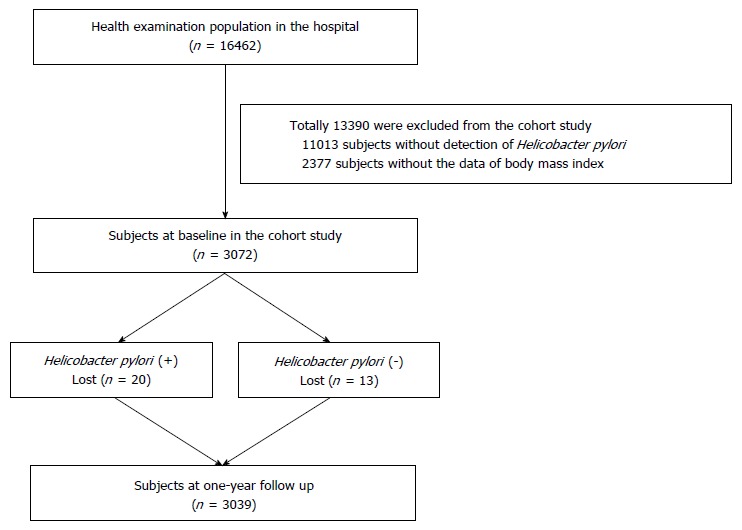
The flow diagram of the subject selection in the study.
The characteristics of the subjects in this study are shown in Table 1. The mean (SD) age of all the subjects was 49 (19) years, and 248 (8.2%) were female. A total of 770 (22.5%) subjects had underlying diseases, including 21.1% with hypertension, 6.8% with diabetes and 5.8% with coronary heart disease. The mean (standard deviation) BMI was 24.5 (3.3) kg/m2. Most (44.2%) of the subjects had normal weight, 41.0% were overweight and 12.8% were obese.
Table 1.
The characteristics of subjects at study baseline n (%)
| Variable | Total (n = 3039) |
Baseline data |
||
| H. pylori (+) | H. pylori (-) | P value | ||
| Age (yr), mean ± SD | 49 ± 19 | 50 ± 19 | 47 ± 19 | < 0.001 |
| ≤ 45 | 1513 (49.8) | 737 (48.7) | 776 (51.3) | < 0.001 |
| 45-60 | 523 (17.2) | 319 (61.0) | 204 (39.0) | |
| > 60 | 1003 (33.0) | 583 (58.1) | 420 (41.9) | |
| Sex, female | 248 (8.2) | 137 (55.4) | 111 (44.6) | 0.662 |
| Marriage, single | 734 (24.2) | 358 (48.8) | 376 (51.2) | 0.001 |
| Underlying disease | 770 (25.4) | 446 (57.9) | 324 (42.1) | 0.010 |
| Diabetes | 207 (6.8) | 121 (58.5) | 86 (41.6) | 0.175 |
| Hypertension | 642 (21.1) | 369 (57.5) | 273 (42.5) | 0.042 |
| Coronary heart disease | 177 (5.8) | 99 (55.9) | 78 (44.1) | 0.579 |
| LDL > 3.1 mmol/L | 816 (28.1) | 465 (57.0) | 351 (43.0) | 0.092 |
| HDL < 0.83 mmol/L | 823 (28.4) | 469 (57.0) | 354 (43.0) | 0.090 |
| TG > 1.71 mmol/L | 861 (28.3) | 488 (56.7) | 373 (43.3) | 0.056 |
| TC > 5.7 mmol/L | 614 (20.2) | 336 (54.7) | 278 (45.3) | 0.660 |
| FBG > 6.1 mmol/L | 439 (14.5) | 258 (58.8) | 181 (41.2) | 0.028 |
| BMI, kg/m2 | 24.5 ± 3.3 | 24.5 ± 3.2 | 24.4 ± 3.3 | 0.221 |
| Underweight | 62 (2.0) | 34 (54.8) | 28 (45.2) | 0.146 |
| Normal | 1342 (44.2) | 693 (51.6) | 649 (48.4) | |
| Overweight | 1247 (41.0) | 700 (56.1) | 547 (43.9) | |
| Obese | 388 (12.8) | 212 (54.6) | 176 (45.4) | |
BMI: Body mass index; LDL: Low density lipoprotein; HDL: High density lipoprotein; FBG: Fasting blood glucose; TG: Triglycerides; TC: Total cholesterol; H. pylori: Helicobacter pylori.
H. pylori distribution
The overall prevalence of H. pylori infection was 53.9% (1639/3039), and the prevalence was 54.6% (212/388) in the obese subjects. Higher rates of seroprevalence were demonstrated in the subjects who were older, married, had underlying diseases, hypertension or higher FBG (all P < 0.05), as shown in Table 1. No significant associations were found between H. pylori and BMI/obesity at the baseline survey (P > 0.05).
Association between H. pylori and BMI
Observed from all the subjects, the BMI decreased from the baseline to the 1-year follow-up in both the H. pylori (+) group (r = -0.169, Figure 2A) and the H. pylori (-) group (r = -0.189, Figure 2B). However, the change in BMI in the H. pylori (+) group was not significantly higher than that in the H. pylori (-) group after adjusting for age, sex, marriage, underlying disease, LDL, HDL, TGs, TC and FBG (RR = 0.988, 95%CI: 0.924-1.057, P = 0.729), as shown in Table 2. BMI significantly decreased in the overweight and obese subjects at the 1-year follow-up, while it was non-significantly increased in the underweight and normal weight subjects (Table 2 and Figure 3). Differences were not found between H. pylori infection and BMI change in different BMI groups (P > 0.05 for all).
Figure 2.
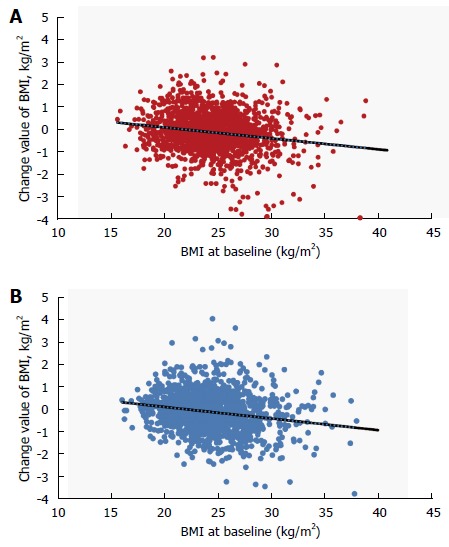
The scatter plots of change in body mass index along with body mass index at baseline in the Helicobacter pylori (+) and Helicobacter pylori (-) groups. The trend lines are added in the two plots. A: Helicobacter pylori (H. pylori) (+) group; B: H. pylori (-) group. BMI: Body mass index.
Table 2.
The association between Helicobacter pylori and body mass index in the study
| Group |
Change in BMI |
Crude |
Adjusted |
|||
| Value | P value | RR (95%CI) | P value | RR (95%CI) | P value | |
| Model 1 in all the subjects | ||||||
| H. pylori (+) | -0.118 | < 0.001 | 0.963 (0.901-1.029) | 0.264 | 0.988 (0.924-1.057) | 0.729 |
| H. pylori (-) | -0.080 | < 0.001 | 1.000 | 1.000 | ||
| Model 2 in the subjects with obesity | ||||||
| H. pylori (+) | -0.431 | < 0.001 | 1.020 (0.791-1.317) | 0.876 | 1.038 (0.794-1.357) | 0.786 |
| H. pylori (-) | -0.411 | < 0.001 | 1.000 | 1.000 | ||
| Model 3 in the subjects with overweight | ||||||
| H. pylori (+) | -0.136 | < 0.001 | 0.942 (0.852-1.042) | 0.245 | 0.968 (0.874, 1.072) | 0.529 |
| H. pylori (-) | -0.196 | < 0.001 | 1.000 | 1.000 | ||
| Model 4 in the subjects with normal and underweight | ||||||
| H. pylori (+) | 0.0563 | 0.159 | 0.987 (0.908-1.074) | 0.764 | 1.009 (0.926-1.1) | 0.835 |
| H. pylori (-) | 0.0435 | 0.057 | 1.000 | 1.000 | ||
H. pylori: Helicobacter pylori.
Figure 3.
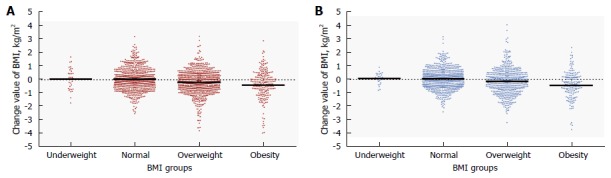
The scatter plots of change in body mass index in the underweight, normal, overweight and obese subjects at baseline in the Helicobacter pylori (+) and Helicobacter pylori (-) groups. The means are added in the two plots. A: Helicobacter pylori (H. pylori) (+) group; B: H. pylori (-) group. BMI: Body mass index.
Association between H. pylori and obesity
The prevalence of obesity decreased 1.1% in the H. pylori (+) group and 0.5% in the H. pylori (-) group (Table 3). The RR of H. pylori infection for obesity was 0.831 (95%CI: 0.577-1.197; P = 0.321) after the adjustment. In the obese subjects, the decreased prevalence of obesity was 19.9% and 19.1% in the H. pylori (+) and the H. pylori (-) group, respectively. Compared with the H. pylori (-) group, the subjects in the H. pylori (+) group lost weight more easily (RR = 0.931; 95%CI: 0.574-1.585; P = 0.972). In the non-obese subjects, the prevalence of obesity in the H. pylori (+) group was lower than that in the H. pylori (-) group (RR = 0.673; 95%CI: 0.382-1.186; P = 0.170).
Table 3.
The association between Helicobacter pylori and obesity in the study
| Group |
Event |
Crude |
Adjusted |
||||
| Baseline | 1 yr | Incidence (%) | RR (95%CI) | P value | RR (95%CI) | P value | |
| Model 1 in all the subjects | |||||||
| H. pylori (+) | 212 (12.9) | 194 (11.8) | 18 (1.1) | 0.890 (0.626-1.267) | 0.519 | 0.831 (0.577-1.197) | 0.321 |
| H. pylori (-) | 176 (12.6) | 169 (12.1) | 7 (0.5) | 1.000 | 1.000 | ||
| Model 2 in the obese subjects | |||||||
| H. pylori (+) | 212 (100) | 170 (80.2) | 42 (19.8) | 0.995 (0.603-1.642) | 0.985 | 0.931 (0.547-1.585) | 0.792 |
| H. pylori (-) | 176 (100) | 141 (80.1) | 35 (19.1) | 1.000 | 1.000 | ||
| Model 3 in the non-obese subjects | |||||||
| H. pylori (+) | 0 | 24 (1.7) | 24 (1.7) | 0.731 (0.422-1.268) | 0.265 | 0.673 (0.382-1.186) | 0.170 |
| H. pylori (-) | 0 | 28 (2.3) | 28 (2.3) | 1.000 | 1.000 | ||
Note: The population is the same as that in Table 2. H. pylori: Helicobacter pylori.
DISCUSSION
We evaluated the relationship between H. pylori infection and obesity/weight gain in the population using a retrospective study. No significant differences were found during the analysis. Despite the lack of significant differences, we found a trend toward weight loss in conjunction with H. pylori infection.
The prevalence of H. pylori in the overall population was 53.9%, which was similar to those in other Asian countries (Japan and Taiwan), lower than those in most European and South American countries and higher than those in North America and Australia[6]. These discrepancies might be related to both small sample size and variability in diagnostic testing. Different methods were used to diagnose H. pylori infection. Serology had a low diagnostic accuracy of only 80%-84%, which is only useful to exclude H. pylori, while the urea breath test (UBT) performed better with a sensitivity of 88%-95% and a specificity of 95%-100%[6]. Therefore, in order to give a correct diagnosis, positive serology and UBT should be performed together before treatment.
Some studies reported that eradication of H. pylori was associated with metabolic disturbances including weight gain[17-19]. Some studies have given an explanation about the effect of H. pylori eradication; one was that H. pylori eradication increases the gastric secretion of ghrelin, which leads to increased appetite and weight gain[20,21]. The precise effect of gastric secretion of ghrelin on circulating ghrelin levels is not straightforward. Another explanation was that the eradication of H. pylori decreases gastric leptin expression, and this decrease was accompanied by an increase in BMI[22]. The effects of H. pylori on ghrelin and leptin strongly suggest that the bacterium “protects” against obesity. The decreasing incidence of this infection may be contributing to an increase in appetite and food intake. Unfortunately, these mechanisms were not invariably confirmed. Epidemiological studies have failed to show any association between H. pylori infection and BMI, although a meta-analysis of 18 observational studies reported a slightly higher BMI in H. pylori positive patients[14]. In our study, the H. pylori infection appeared to be a protective factor for obesity. The H. pylori (+) subjects had decreased BMI more than H. pylori (-) subjects, although the differences were not significant, which is opposite to the result of the cross-sectional study by Zhang et al[15]. This contrary finding may be attributed to different populations being analyzed and/or the different methods used to make the diagnosis. Another reason may be the increase in intestinal permeability and the role of gut microbiota to induce insulin resistance and liver steatosis[23,24]. Based on that, we think that H. pylori infection may have a limited effect in losing weight, and the eradication of H. pylori may have a limited effect in gaining weight. The primary cause of weight gain is changes in lifestyle. The intake of fat and carbohydrates increases, while physical activity clearly decreases. H. pylori infection was associated with decreased gastric expression of leptin and ghrelin and correlated negatively with patient energy intake and body mass index[25]. It can be postulated that H. pylori infection due to effects on leptin and ghrelin protects against the intake of a large amount of calories in these patients.
Our study had several important limitations. The primary limitation is that our study had a short-term follow-up (only one year), and we could not achieve a significant outcome from the portion of the subjects who attended follow-up. Another limitation is that we did not consider the effect of the treatment on the H. pylori infection during the follow-up time, which may influence the association between H. pylori infection and weight gain. We did not analyze the effect of insulin resistance on the association between H. pylori and obesity. Serological testing for the presence of anti-H. pylori IgG and IgM does not indicate a current infection and only shows exposure to these bacteria, which may have biased the detection of H. pylori infection. The last limitation is that the ratio of males to females was high due to the characteristics of the unit from which the subjected came. These above limitations may have biased certain outcomes of the results.
In conclusion, H. pylori infection was not associated with overweight/obesity observed in the retrospective study in this Chinese population.
ACKNOWLEDGMENTS
We would like to thank Lai-Lai Yan from the School of Public Health, Peking University for his support and assistance in this study.
COMMENTS
Background
The World Health Organization estimated that over 600 million people were obese in the world in year 2014. Obesity is interlinked with infectious diseases, such that certain infections may trigger an increase in adiposity, such as Helicobacter pylori (H. pylori). H. pylori has been linked with gastritis, gastric ulcers and gastric cancer. The association between H. pylori and obesity/weight gain is still unclear and controversial. Reports from different areas and countries are not consistent with each other, and most were cross-sectional studies. It was therefore necessary to further explore the true association between H. pylori and obesity. Therefore, we performed this retrospective study to explore the association between H. pylori infection and obesity/weight gain in a population in China.
Research frontiers
Some studies reported that the eradication of H. pylori was associated with metabolic disturbances including weight gain, but the mechanisms were not invariably confirmed. Epidemiological studies have failed to show any association between H. pylori infection and body mass index.
Innovations and breakthroughs
No significant differences were found between H. pylori infection and obesity/weight gain during the analysis. In spite of this, the authors also found a trend toward weight loss with H. pylori infection.
Applications
These results provide evidence that H. pylori infection may be not associated with obesity or weight gain, which means that H. pylori infection may have a limited effect in weight loss; that is, eradication of H. pylori may have a limited effect in gaining weight.
Terminology
BMI, body mass index, is used to quantify the amount of tissue mass (muscle, fat, and bone) in an individual and then categorize that person as underweight, normal weight, overweight, or obese based on that value.
Peer-review
This is a well-designed, performed and written retrospective clinical study for the evaluation of the association between H. pylori infection and obesity in a population in China.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Institutional review board statement: This study was reviewed and approved by the Research Ethics Committee of Aerospace Center Hospital.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: We have no financial relationships to disclose.
Data sharing statement: No additional data are available in this manuscript.
Peer-review started: December 14, 2016
First decision: December 29, 2016
Article in press: March 15, 2017
P- Reviewer: Abenavoli L, Chmiela M, Tovey FI, Vorobjova T, Yamaoka Y S- Editor: Gong ZM L- Editor: Wang TQ E- Editor: Wang CH
References
- 1.Dhurandhar NV, Bailey D, Thomas D. Interaction of obesity and infections. Obes Rev. 2015;16:1017–1029. doi: 10.1111/obr.12320. [DOI] [PubMed] [Google Scholar]
- 2.Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T, et al. Management of Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084. [DOI] [PubMed] [Google Scholar]
- 3.Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991;338:1175–1176. doi: 10.1016/0140-6736(91)92035-z. [DOI] [PubMed] [Google Scholar]
- 4.Khatoon J, Rai RP, Prasad KN. Role of Helicobacter pylori in gastric cancer: Updates. World J Gastrointest Oncol. 2016;8:147–158. doi: 10.4251/wjgo.v8.i2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang SS, Hu HY. Helicobacter pylori: Effect of coexisting diseases and update on treatment regimens. World J Gastrointest Pharmacol Ther. 2015;6:127–136. doi: 10.4292/wjgpt.v6.i4.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carabotti M, D’Ercole C, Iossa A, Corazziari E, Silecchia G, Severi C. Helicobacter pylori infection in obesity and its clinical outcome after bariatric surgery. World J Gastroenterol. 2014;20:647–653. doi: 10.3748/wjg.v20.i3.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arslan E, Atilgan H, Yavaşoğlu I. The prevalence of Helicobacter pylori in obese subjects. Eur J Intern Med. 2009;20:695–697. doi: 10.1016/j.ejim.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Dutta SK, Arora M, Kireet A, Bashandy H, Gandsas A. Upper gastrointestinal symptoms and associated disorders in morbidly obese patients: a prospective study. Dig Dis Sci. 2009;54:1243–1246. doi: 10.1007/s10620-008-0485-6. [DOI] [PubMed] [Google Scholar]
- 9.Wu MS, Lee WJ, Wang HH, Huang SP, Lin JT. A case-control study of association of Helicobacter pylori infection with morbid obesity in Taiwan. Arch Intern Med. 2005;165:1552–1555. doi: 10.1001/archinte.165.13.1552. [DOI] [PubMed] [Google Scholar]
- 10.Lane JA, Murray LJ, Harvey IM, Donovan JL, Nair P, Harvey RF. Randomised clinical trial: Helicobacter pylori eradication is associated with a significantly increased body mass index in a placebo-controlled study. Aliment Pharmacol Ther. 2011;33:922–929. doi: 10.1111/j.1365-2036.2011.04610.x. [DOI] [PubMed] [Google Scholar]
- 11.Yang YJ, Sheu BS, Yang HB, Lu CC, Chuang CC. Eradication of Helicobacter pylori increases childhood growth and serum acylated ghrelin levels. World J Gastroenterol. 2012;18:2674–2681. doi: 10.3748/wjg.v18.i21.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang EJ, Park SW, Park JS, Park SJ, Hahm KB, Paik SY, Sin MK, Lee ES, Oh SW, Park CY, et al. The influence of the eradication of Helicobacter pylori on gastric ghrelin, appetite, and body mass index in patients with peptic ulcer disease. J Gastroenterol Hepatol. 2008;23 Suppl 2:S278–S285. doi: 10.1111/j.1440-1746.2008.05415.x. [DOI] [PubMed] [Google Scholar]
- 13.Kawano S, Kawahara A, Nakai R, Fu HY, Tsuji S, Tsujii M. Helicobacter pylori infection does not affect serum leptin concentration and body mass index (BMI) in asymptomatic subjects. J Gastroenterol. 2001;36:579–580. doi: 10.1007/s005350170064. [DOI] [PubMed] [Google Scholar]
- 14.Danesh J, Peto R. Risk factors for coronary heart disease and infection with Helicobacter pylori: meta-analysis of 18 studies. BMJ. 1998;316:1130–1132. doi: 10.1136/bmj.316.7138.1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Du T, Chen X, Yu X, Tu L, Zhang C. Association between Helicobacter pylori infection and overweight or obesity in a Chinese population. J Infect Dev Ctries. 2015;9:945–953. doi: 10.3855/jidc.6035. [DOI] [PubMed] [Google Scholar]
- 16.Zhou BF; Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 17.Al-Nozha M, Al-Khadra A, Arafah MR, Al-Maatouq MA, Khalil MZ, Khan NB, Al-Mazrou YY, Al-Marzouki K, Al-Harthi SS, Abdullah M, et al. Metabolic syndrome in Saudi Arabia. Saudi Med J. 2005;26:1918–1925. [PubMed] [Google Scholar]
- 18.Scharnagl H, Kist M, Grawitz AB, Koenig W, Wieland H, März W. Effect of Helicobacter pylori eradication on high-density lipoprotein cholesterol. Am J Cardiol. 2004;93:219–220. doi: 10.1016/j.amjcard.2003.09.045. [DOI] [PubMed] [Google Scholar]
- 19.Albaker WI. Helicobacter pylori infection and its relationship to metabolic syndrome: is it a myth or fact? Saudi J Gastroenterol. 2011;17:165–169. doi: 10.4103/1319-3767.80377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osawa H, Nakazato M, Date Y, Kita H, Ohnishi H, Ueno H, Shiiya T, Satoh K, Ishino Y, Sugano K. Impaired production of gastric ghrelin in chronic gastritis associated with Helicobacter pylori. J Clin Endocrinol Metab. 2005;90:10–16. doi: 10.1210/jc.2004-1330. [DOI] [PubMed] [Google Scholar]
- 21.Tatsuguchi A, Miyake K, Gudis K, Futagami S, Tsukui T, Wada K, Kishida T, Fukuda Y, Sugisaki Y, Sakamoto C. Effect of Helicobacter pylori infection on ghrelin expression in human gastric mucosa. Am J Gastroenterol. 2004;99:2121–2127. doi: 10.1111/j.1572-0241.2004.30291.x. [DOI] [PubMed] [Google Scholar]
- 22.Azuma T, Suto H, Ito Y, Ohtani M, Dojo M, Kuriyama M, Kato T. Gastric leptin and Helicobacter pylori infection. Gut. 2001;49:324–329. doi: 10.1136/gut.49.3.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abenavoli L, Milic N, Masarone M, Persico M. Association between non-alcoholic fatty liver disease, insulin resistance and Helicobacter pylori. Med Hypotheses. 2013;81:913–915. doi: 10.1016/j.mehy.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Upala S, Sanguankeo A, Saleem SA, Jaruvongvanich V. Effects of Helicobacter pylori eradication on insulin resistance and metabolic parameters: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017;29:153–159. doi: 10.1097/MEG.0000000000000774. [DOI] [PubMed] [Google Scholar]
- 25.Salles N, Ménard A, Georges A, Salzmann M, de Ledinghen V, de Mascarel A, Emeriau JP, Lamouliatte H, Mégraud F. Effects of Helicobacter pylori infection on gut appetite peptide (leptin, ghrelin) expression in elderly inpatients. J Gerontol A Biol Sci Med Sci. 2006;61:1144–1150. doi: 10.1093/gerona/61.11.1144. [DOI] [PubMed] [Google Scholar]


