Abstract
Introduction
We studied the effect of long-term storage at −80°C on cerebrospinal fluid (CSF) biomarker levels. Our approach assumed consistency of mean biomarker levels in a homogenous Alzheimer's disease patient cohort over time.
Methods
We selected 148 Alzheimer's disease samples that had inclusion dates equally distributed over the years 2001 to 2013 from our biobank. The concentrations of CSF biomarkers, amyloid β1–42 (Aβ1–42), total tau (T-tau), and phosphorylated tau181 (P-tau), were measured with one enzyme-linked immunosorbent assay lot. Results were compared with historical results obtained at biobank inclusion.
Results
Linear regression analyses showed that the levels of CSF biomarkers, Aβ1–42, T-tau, and P-tau, were not related to storage time at −80°C (β = 0.015, 0.048, and 0.0016 pg/mL per day, not significant). However, the differences between remeasured concentrations of Aβ1–42 and concentrations at biobank inclusion measured for more than 30 assay batches increased with increasing time difference.
Discussion
The levels of CSF biomarkers, Aβ1–42, T-tau, and P-tau, did not significantly change during the maximum period of 12 years of storage at −80°C. Batch variation for Aβ1–42 is a factor that should be controlled for when using historical cohorts.
Keywords: Alzheimer's disease, Cerebrospinal fluid, Biomarkers, Amyloid β1–42, Total tau, Phosphorylated tau181, Long-term storage, Preanalytical variation, Batch variation, ELISA
1. Introduction
Cerebrospinal fluid (CSF) biomarkers, amyloid β1–42 (Aβ1–42), total tau (T-tau), and phosphorylated tau181 (P-tau), support the diagnosis of Alzheimer's disease (AD) [1]. Unfortunately, susceptibility to preanalytical/analytical variation has hampered clinical implementation [2], [3], [4], [5], [6], [7], [8], [9]. The effect of long-term storage on CSF biomarkers is relevant because historical cohorts are needed to establish universal cutoff values. Evaporation during biobank storage is not an issue [10], [11], but the long-term stability of biomarkers has been poorly studied. The first study on this topic monitored Aβ1–42 and T-tau for 22 days and extrapolated these results using Arrhenius equations showing long-term stability at −80°C [12]. Next, a study reported on a repetitive measurement of a quality control CSF sample for more than 2 years, resulting in stable Aβ1–42 concentrations [13]. Another study compared aliquots of clinical samples for more than 0 to 6 years and reported stable Aβ1–42 and T-tau concentrations [14]. In both the latter studies, however, analysis was done in different assay batches, which could have interfered with the potential effects of long-term storage.
We studied the levels of CSF biomarkers, Aβ1–42, T-tau, and P-tau, in relation to storage duration, starting from the assumption that mean biomarker levels of the average AD patient will not change over time. Similar collection procedures and assay batches thus precluded any preanalytical bias other than the length of biobank storage.
2. Methods
2.1. Sample collection
Patients underwent a standard clinical assessment and were diagnosed as probable AD according to the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA) criteria [15]. We assumed that the average biomarker concentrations in AD patients within a narrow age range and equal apolipoprotein E (APOE) genotype and gender distribution on a group level will remain similar, regardless of the inclusion year. CSF was collected by lumbar puncture in 10 mL polypropylene tubes (Sarstedt, Nümbrecht, Germany). CSF samples were centrifuged at 1800 to 2100g for 10 minutes at 4°C within 2 hours and a small amount, 0.35 to 2.5 mL, was transferred to 5 mL polypropylene tubes (Sarstedt) and used for routine analysis and biomarker measurement (Innotest β-AMYLOID (1–42), hTAU-Ag, and PHOSPHO-TAU (181p); Innogenetics, Belgium). The remaining CSF was divided into polypropylene tubes (1.5 or 2.0 mL; Sarstedt) in 0.5 mL volumes and stored in the biobank at −80°C [16]. The protocol was approved by the institutional review board and subjects gave written consent.
2.2. Cohort selection
We selected 148 patients diagnosed with probable AD included between September 2001 and October 2013: aged 64 to 72 years, MMSE score from 14 to 27, APOE genotypes ε3/ε3 (n = 41), ε3/ε4 (n = 69), and ε4/ε4 (n = 38), and a gender distribution of 78 females and 70 males. We aimed for an equally scattered distribution of these clinical characteristics of the samples over the inclusion years. The biobank collection protocol remained unchanged during this period, apart from a small change as follows: from 2008 to 2011 biobank vials of 0.5 mL (Brand, ref. 211-3211) were used.
2.3. Enzyme-linked immunosorbent assays
We determined Aβ1–42, T-tau, and P-tau concentrations in fresh biobank aliquots using one batch of sandwich Enzyme-linked immunosorbent assays (Innotest β-AMYLOID (1–42), Innotest hTAU-Ag, and Innotest PHOSPHO-TAU (181p); Fujirebio, Ghent, Belgium, former Innogenetics) between November 2015 and February 2016.
2.4. Statistical analysis
Linear regression analyses were performed to assess the effect of storage time in days on (1) biomarker levels (all reassessed in one batch) and (2) differences between new and old biomarker measurements. “β” expresses the slope of the linear regressions in picograms per milliliter per day ± standard error of the mean (SEM). To compare the remeasured values with the old values, Spearman correlation and Passing-Bablok regression were performed. P value <.05 was considered significant. Analyses were done in R version 3.3.1.
3. Results
3.1. Levels of CSF biomarkers Aβ1–42, T-tau, and P-tau are not related to storage time at −80°C
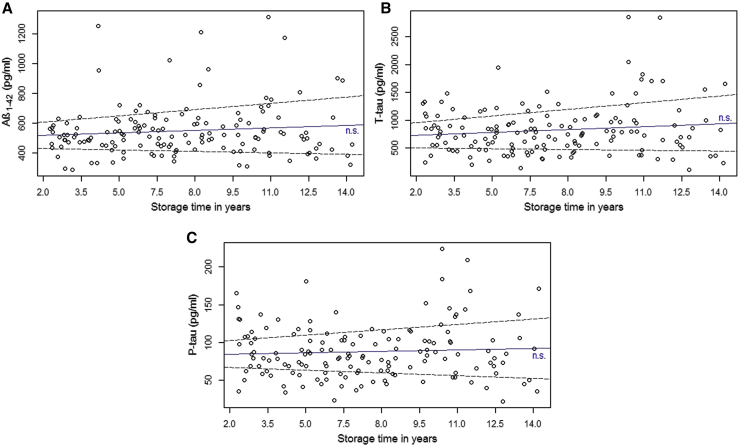
Biomarker values (median + range) were 516 (287–1314) pg/mL for Aβ1–42, 769 (112–2856) pg/mL for T-tau, and 83 (22–224) pg/mL for P-tau; these values were not part of the selection criteria. Linear regression analysis showed that there was no relation between storage time and biomarker value (β[slope ± SEM] = 0.015 ± 0.012 pg/mL per day for Aβ1–42, β = 0.048 ± 0.031 pg/mL per day for T-tau, and β = 0.0016 ± 0.0025 pg/mL per day for P-tau, all P > .05) (Fig. 1). Confidence intervals (95%; CIs) of the linear regression model fit show that the yearly concentration changes for Aβ1–42, T-tau, and P-tau were between −3.2 and 14.2, −4.7 and 39.7, and between −1.2 and 2.4 pg/mL, respectively.
Fig. 1.
CSF biomarker (A) Aβ1–42, (B) T-tau, and (C) P-tau concentrations over storage years at −80°C. Aβ1–42, T-tau, and P-tau concentrations were measured in biobanked samples of a homogenous AD patient cohort (n = 148) in a single assay batch. Linear regression analyses showed no significant effects of storage time on biomarker concentrations. Solid lines represent regression fit and dotted lines represent the 95% confidence intervals of the regression models. Abbreviations: Aβ1–42, amyloid β1–42; AD, Alzheimer's disease; CSF, cerebrospinal fluid; n.s., not significant; T-tau, total tau; P-tau, phosphorylated tau181.
3.2. Comparison of old and new biomarker measurements
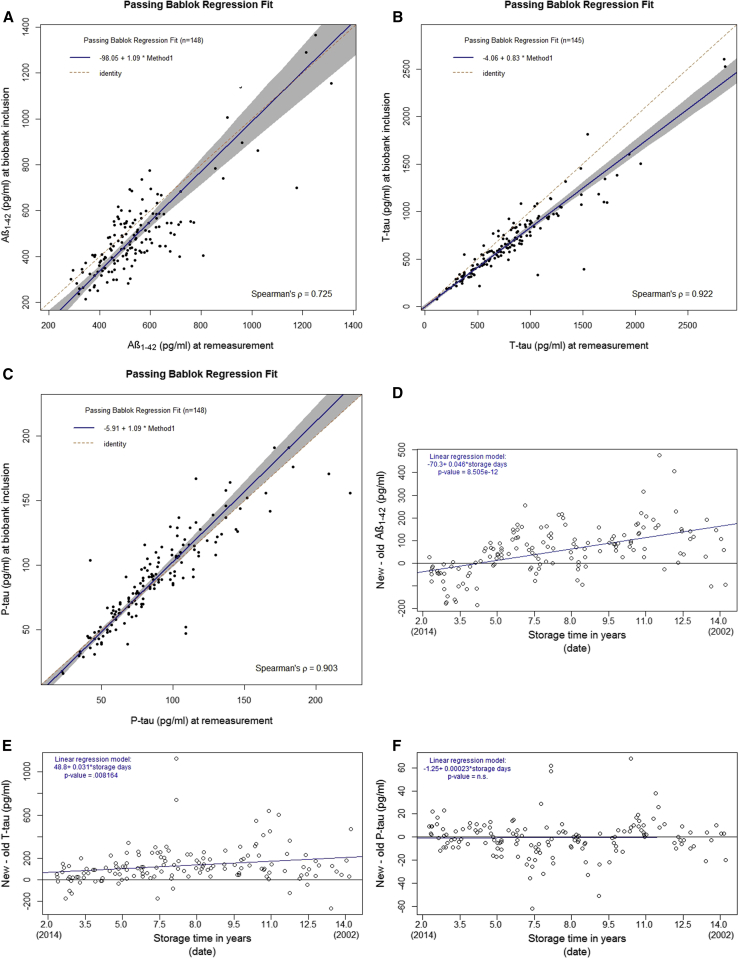
We compared the remeasured Aβ1–42, T-tau, and P-tau concentrations with those measured at the time of inclusion in the biobank, showing strong correlations: ρ = 0.725 for Aβ1–42, ρ = 0.922 for T-tau, and ρ = 0.903 for P-tau (Fig. 2A–C). However, Passing-Bablok regression analyses showed systematic differences, indicated by the intercept of regression line, for Aβ1–42 (intercept = −98.0 [95% CI = −171 to −24.0], β = 1.09 [95% CI = 0.92–1.24]), proportional differences, indicated by the slope of the regression line, for T-tau (intercept = −4.06 [95% = −28.9 to 22.5], β = 0.83 [95% CI = 0.79–0.89]) but no difference for P-tau levels (intercept = −5.91 [95% CI = −11.6 to 0.00], β = 1.09 [95% CI = 1.00–1.17]) (Fig. 2A–C).
Fig. 2.
Comparison of remeasured biomarker values with biomarker values at the time of biobank inclusion. Passing-Bablok regression fit and Spearman's correlation of old and new values showing a systematic difference for Aβ1–42 (A), a proportional difference for T-tau (B), and no difference for P-tau (C). Differences in new and old Aβ1–42, T-tau, and P-tau concentrations in relation to storage time are given in (D), (E), and (F), respectively. For Aβ1–42 (D) and T-tau (E), differences between new and old concentrations increased with longer storage times. Gray areas indicate the 95% confidence interval of the regression fit. Abbreviations: Aβ1–42, amyloid β1–42; AD, Alzheimer's disease; CSF, cerebrospinal fluid; T-tau, total tau; P-tau, phosphorylated tau181.
3.3. Differences between new and old values is related to batch changes
Differences between new and old measurements of Aβ1–42 were strongly related to storage time (β ± SEM = 0.046 ± 0.0062 pg/mL per day; P < .001) (Fig. 2D), where the more recent measurements were consistently higher. For T-tau, a similar trend was observed (β ± SEM = 0.031 ± 0.011 pg/mL per day; P < .01) (Fig. 2E), although not as strong as for Aβ1–42. For P-tau, no trend was observed (β ± SEM = 0.00023 ± 0.0011 pg/mL per day, n.s.) (Fig. 2F).
From 2004 to 2015, 30 batches of Aβ1–42 kits were sequentially used in our laboratory. Before 2004, biomarker measurements were too infrequent to consider batch shifts. Internal quality control samples, measured over the years, confirmed that there was an upward drift in Aβ1–42 concentrations (data not shown) [17].
3.4. Preanalytical biobank protocol
From 2001 to 2013, the only change in our biobank collection protocol was the type of tube used for sample storage, which did not affect biomarker concentrations: values for Sarstedt 1.5/2.0 mL versus Brand 0.5 mL tubes were (median + interquartile range) 504 (158) versus 541 (161) pg/mL for Aβ1–42, 788 (525) versus 747 (422) pg/mL for T-tau, and 84 (49) versus 80 (40) pg/mL for P-tau (all n.s.).
4. Discussion
Our study shows that storage time up to 12 years does not significantly affect the levels of CSF biomarkers Aβ1–42, T-tau, and P-tau. Our novel approach was to measure biomarker concentrations in biobanked samples of a homogenous AD cohort using single batches of Aβ1–42, T-tau, and P-tau enzyme-linked immunosorbent assays.
We observed differences in Aβ1–42 and T-tau levels originally measured in 2001 versus 2013 but did not find significant effects of storage time when biomarkers were measured in the same assay batch. The recently established increase in the cutoff level for Aβ1–42 in AD diagnostics [18] and the increase in internal quality control sample concentrations over time (data not shown) [17] support our findings and indicate that batch variation is a factor impeding AD biomarker studies [5]. The development of automated platforms [19] and calibration against reference methods and reference material [20], [21] for biomarker measurement can strongly reduce this variation.
Potential preanalytical processing factors were controlled for as much as possible in this study. To illustrate, the same technician performed the biomarker analyses for this study and for the routine diagnostics since 2009. Moreover, the same routine and biobanking protocols were used throughout the whole period, although we cannot exclude influence of as yet unidentified preanalytical factors. One identified factor in this study was a difference in aliquot volumes between the remeasurements (0.5 mL) and a broader range of volumes for the samples used for routine biomarker measurements at the time of biobank inclusion (between 0.35 and 2.5 mL). However, a potential effect of this difference was not observed as a visual systematic difference between the new and the old biomarker measurements. Another limitation of this study was the large variance in biomarker concentrations in our cohort, which is an inevitable risk in this type of study design, where biomarker concentrations were not part of the selection criteria.
The guidelines for the preanalytical protocol of CSF biomarkers [11] can be updated following this study to include the currently presented stability of CSF biomarkers and the long-term resistance of CSF samples to evaporation [10]. Assay drift over the years is a secondary outcome of the present study and a phenomenon that will be thoroughly addressed in other reports. There are various potential approaches to resolve the consequences of assay drift when using historically measured biomarker levels: (1) remeasurement of the biomarker values in one assay batch, (2) development of statistical models that correct for assay batch as a confounding factor, and (3) more complex statistical models that level out the drift in biomarker concentrations over time. Future studies should carefully consider these solutions.
To conclude, AD biomarker levels prove to be stable on long-term storage. Historically measured Aβ1–42 and T-tau concentrations should be applied with caution, because absolute values have increased over time due to analytical assay changes. Statistical correction for an assay batch or remeasurement of the biomarkers provides plausible solutions for this assay drift. Our results encourage the growth of CSF biobanks for dementia biomarker research because historical samples retain their value for AD research over years.
Research in Context.
-
1.
Systematic review: Literature on the topic was identified by searching PubMed for “AD biomarkers” AND “long-term storage” OR “stability.” The methods used to assess long-term storage effects in the identified reports were evaluated in detail.
-
2.
Interpretation: Our data confirm that the Alzheimer's disease (AD) cerebrospinal fluid biomarkers Aβ1–42, T-tau, and P-tau are not affected by long-term storage up to 12 years. Stability of these biomarkers has been reported earlier but has not been empirically proven using a design that covers a period of 12 years and precludes effects of batch variation.
-
3.
Future directions: The AD biomarkers are stable during biobank storage, which reassures the value of historical patient cohorts for biomarker studies. Long-term stability of other analytes should be assessed. Guidelines should be generated to handle differences in biomarker values caused by batch variation. Potential solutions are (1) remeasurement of the AD biomarkers within one batch and (2) including batch number as a confounding factor in future statistical models.
References
- 1.Scheltens P., Blennow K., Breteler M.M., de Strooper B., Frisoni G.B., Salloway S. Alzheimer's disease. Lancet. 2016;388:505–517. doi: 10.1016/S0140-6736(15)01124-1. [DOI] [PubMed] [Google Scholar]
- 2.Fourier A., Portelius E., Zetterberg H., Blennow K., Quadrio I., Perret-Liaudet A. Pre-analytical and analytical factors influencing Alzheimer's disease cerebrospinal fluid biomarkers variability. Clin Chim Acta. 2015;449:9–15. doi: 10.1016/j.cca.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 3.Le Bastard N., De Deyn P.P., Engelborghs S. Importance and impact of preanalytical variables on Alzheimer disease biomarker concentrations in cerebrospinal fluid. Clin Chem. 2015;61:734–743. doi: 10.1373/clinchem.2014.236679. [DOI] [PubMed] [Google Scholar]
- 4.Willemse E.A., Teunissen C.E. Importance of pre-analytical stability for CSF biomarker testing. In: Deisenhammer F., Sellebjerg F., Teunissen C.E., Tumani H., editors. Cerebrospinal Fluid in Clinical Neurology. Springer International Publishing Switzerland; Cham, Switzerland: 2015. pp. 59–77. [Google Scholar]
- 5.Mattsson N., Andreasson U., Persson S., Carrillo M.C., Collins S., Chalbot S. CSF biomarker variability in the Alzheimer's association quality control program. Alzheimers Dement. 2013;9:251–261. doi: 10.1016/j.jalz.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leitão M.J., Baldeiras I., Herukka S.K., Pikkarainen M., Leinonen V., Simonsen A.H. Chasing the effects of pre-analytical confounders—a multicenter study on CSF-AD biomarkers. Front Neurol. 2015;6:1–8. doi: 10.3389/fneur.2015.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuhlmann J., Andreasson U., Pannee J., Bjerke M., Portelius E., Leinenbach A. CSF Aβ1–42—an excellent but complicated Alzheimer's biomarker—a route to standardisation. Clin Chim Acta. 2017;467:27–33. doi: 10.1016/j.cca.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Perret-Liaudet A., Pelpel M., Tholance Y., Dumont B., Vanderstichele H., Zorzi W. Cerebrospinal fluid collection tubes: a critical issue for Alzheimer disease diagnosis. Clin Chem. 2012;795:787–789. doi: 10.1373/clinchem.2011.178368. [DOI] [PubMed] [Google Scholar]
- 9.Vanderstichele H.M., Janelidze S., Demeyer L., Coart E., Stoops E., Herbst V. Optimized standard operating procedures for the analysis of cerebrospinal fluid Aβ42 and the ratios of Aβ isoforms using low protein binding tubes. J Alzheimers Dis. 2016;53:1121–1132. doi: 10.3233/JAD-160286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willemse E.A., Koel-Simmelink M.J., Durieux-lu S., Van der Flier W.M., Teunissen C.E. Standard biobanking conditions prevent evaporation of body fluid samples. Clin Chim Acta. 2015;442:141–145. doi: 10.1016/j.cca.2015.01.036. [DOI] [PubMed] [Google Scholar]
- 11.del Campo M., Mollenhauer B., Bertolotto A., Engelborghs S., Hampel H., Simonsen A.H. Recommendations to standardize preanalytical confounding factors in Alzheimer's and Parkinson's disease cerebrospinal fluid biomarkers: an update. Biomark Med. 2012;6:419–430. doi: 10.2217/bmm.12.46. [DOI] [PubMed] [Google Scholar]
- 12.Schoonenboom N.S., Mulder C., Vanderstichele H., Van Elk E.J., Kok A., Van Kamp G.J. Effects of processing and storage conditions on amyloid beta (1-42) and tau concentrations in cerebrospinal fluid: implications for use in clinical practice. Clin Chem. 2005;51:189–195. doi: 10.1373/clinchem.2004.039735. [DOI] [PubMed] [Google Scholar]
- 13.Bjerke M., Portelius E., Minthon L., Wallin A., Anckarsäter H., Anckarsäter R. Confounding factors influencing amyloid beta concentration in cerebrospinal fluid. Int J Alzheimers Dis. 2010;2010:1–12. doi: 10.4061/2010/986310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schipke C.G., Jessen F., Teipel S., Luckhaus C., Wiltfang J., Esselmann H. Long-term stability of Alzheimer's disease biomarker proteins in cerebrospinal fluid. J Alzheimers Dis. 2011;26:255–262. doi: 10.3233/JAD-2011-110329. [DOI] [PubMed] [Google Scholar]
- 15.McKhann G., Drachman D., Folstein M., Katzman R., Price D., Stadlan E.M. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 16.Mulder C., Verwey N.A., van der Flier W.M., Bouwman F.H., Kok A., van Elk E.J. Amyloid-beta(1-42), total tau, and phosphorylated tau as cerebrospinal fluid biomarkers for the diagnosis of Alzheimer disease. Clin Chem. 2010;56:248–253. doi: 10.1373/clinchem.2009.130518. [DOI] [PubMed] [Google Scholar]
- 17.Vos S.J., Visser P.J., Verhey F., Aalten P., Knol D., Ramakers I. Variability of CSF Alzheimer's disease biomarkers: implications for clinical practice. PLoS One. 2014;9:e100784. doi: 10.1371/journal.pone.0100784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zwan M.D., Rinne J.O., Hasselbalch S.G., Nordberg A., Lleó A., Herukka S.K. Use of amyloid-PET to determine cutpoints for CSF markers: a multicenter study. Neurology. 2016;86:50–58. doi: 10.1212/WNL.0000000000002081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiasserini D., Biscetti L., Farotti L., Eusebi P., Salvadori N., Lisetti V. Performance evaluation of an automated ELISA system for Alzheimer's disease detection in clinical routine. J Alzheimers Dis. 2016;54:55–67. doi: 10.3233/JAD-160298. [DOI] [PubMed] [Google Scholar]
- 20.Bjerke M., Andreasson U., Kuhlmann J., Portelius E., Pannee J., Lewczuk P. Assessing the commutability of reference material formats for the harmonization of amyloid beta measurements. Clin Chem Lab Med. 2015;54:1177–1191. doi: 10.1515/cclm-2015-0733. [DOI] [PubMed] [Google Scholar]
- 21.Leinenbach A., Pannee J., Dülffer T., Huber A., Bittner T., Andreasson U. Mass spectrometry-based candidate reference measurement procedure for quantification of amyloid-β in cerebrospinal fluid. Clin Chem. 2014;60:987–994. doi: 10.1373/clinchem.2013.220392. [DOI] [PubMed] [Google Scholar]