Abstract
In patients with chronic myelomonocytic leukemia (CMML), age>65 years is an adverse prognostic factor. Our objective in the current study was to examine risk factors for survival and treatment outcome in 261 ‘young' adults with CMML, as defined by age ⩽65 years. In multivariable analysis, lower HB (P=0.01), higher circulating blast % (P=0.002), ASXL1 (P=0.0007) and SRSF2 mutations (P=0.008) and Mayo-French cytogenetic stratification (P=0.04) negatively impacted survival. Similarly, leukemia-free survival was independently affected by higher circulating blast % (P<0.0001), higher bone marrow blast % (P=0.0007) and the presence of circulating immature myeloid cells (P=0.0002). Seventy-five (29%) patients received hypomethylating agents (HMA), with the median number of cycles being 5, and the median duration of therapy being 5 months. The over-all response rate was 40% for azacitidine and 30% for decitabine. Fifty-three (24%) patients underwent an allogeneic hematopoietic stem cell transplant (AHSCT), with a response rate of 56% and a non-relapse mortality of 19%. Survival in young adults with CMML, although higher than in older patients, is poor and even worse in the presence of ASXL1 and SRSF2 mutations. Treatment outcome was more impressive with AHSCT than with HMA and neither was influenced by ASXL1/SRSF2 mutations or karyotype.
Introduction
Chronic myelomonocytic leukemia (CMML) is a clonal hematopoietic stem cell disorder, with overlapping features of myelodysplastic syndromes and myeloproliferative neoplasms, and is associated with an inherent risk of transformation to acute myeloid leukemia.1 The median age of presentation ranges between 71–74 years, with a male predilection.2, 3, 4 In fact, age >65 years has been shown to be an adverse prognosticator, impacting over-all survival (OS).2 There, however, are a fair number of patients that present earlier than the seventh decade of life. In two large studies the age ranges of disease presentation were; 20–93 years for the Mayo Clinic study,3 and 40–91 years for the Groupe Francophone des Myelodysplasies (GFM) study.2
Cytogenetic abnormalities are seen in 20–30% of patients, whereas gene mutations, especially those causing epigenetic dysregulation (TET2, IHD1, IDH2 and DNMT3A), abnormalities in chromatin dynamics (ASXL1 and EZH2), affecting the spliceosome component machinery (SRSF2, SF3B1 and U2AF1) and the signal transduction pathways (JAK2, KRAS, NRAS and CBL) can be seen in every patient (1, 3, 5 and our unpublished data). Of these, mutations involving TET2 (~60%), SRSF2 (~50%), ASXL1 (~40%) and the RAS pathway (~30%) are most common, with only frame-shift and non-sense mutations of ASXL1 independently impacting OS.2, 3
Contemporary prognostic models, incorporating molecular information, include the Mayo Molecular Model (MMM) and the GFM model. The MMM includes; hemoglobin (HB)<10 gm/dl, absolute monocyte count (AMC) >10 × 10(9)/l, circulating immature myeloid cells (IMCs), platelet count<100 × 10(9)/l and the presence of ASXL1 mutations, risk stratifying patients into four categories: low, intermediate-1/2 and high risk, with median OS of 97 months, 59 months, 37 months and 16 months, respectively.3 The GFM includes; age >65 years, anemia (HB<11 gm/dl in males and 10 gm/dl in females), white blood count (WBC)>15 × 10(9)/l, platelets<100 × 10(9)/l and ASXL1 mutations, risk stratifying patients into three categories; low, intermediate and high risk, with median OS of not reached, 38.5 months and 14.4 months, respectively.2 In addition, recently, the Mayo-French cytogenetic risk stratification system was developed, stratifying patients into three groups; high (complex and monosomal karyotype), intermediate (all karyotypes not belonging to high and low risk groups) and low risk (normal, −Y and der(3q)), with median OS of 3 months, 20 months and 41 months, respectively.5 In this study, advanced age was significantly associated with the presence of an abnormal karyotype (P=0.03).
Treatment options for CMML are limited, and include therapy with hypomethylating agents (HMA) or allogeneic hematopoietic stem cell transplant (AHSCT). There is no phase III data supporting the use of HMA in CMML, however, several phase II studies have been completed with overall response rates ranging from 25–70%, and median OS ranging from 12 to 37 months.6, 7, 8, 9, 10, 11, 12 Unfortunately, the retrospective nature of the vast majority of the studies along with the lack of a comparator arm makes it difficult to draw cross-study conclusions. While AHSCT is a curative strategy, it is currently not widely utilized given issues with donor eligibility (advanced age), limited donor pools and the risk of complications such as graft rejection, acute and chronic graft versus host disease (GVHD) and non-relapse mortality (NRM). Most AHSCT studies have been retrospective, with a mix of myeloablative (MA) and reduced intensity conditioning (RIC) regimens, with NRM ranging from 12–40% and relapse rates ranging from 25–40%, making it very difficult to draw concrete conclusions.1, 13, 14
While there is a modest pool of clinical, prognostic and therapeutic information on patients with CMML, not much is known about those that present prior to the seventh decade of life. In a large study on primary myelofibrosis (n=1000), patients with age <60 years (n=299) had a dynamic international prognostic scoring system (DIPSS-plus) stratified survival that was better than that of the overall cohort, with median OS of 20.0 years, 14.3 years, 5.3 years and 1.7 years for low, intermediate-1/2 and high risk disease, respectively, compared with 15.6 years, 5.6 years, 2.5 years and 1.4 years for the entire cohort.15 Similarly, the clinical characteristics, karyotypic and molecular abnormalities, and outcomes of ‘young' adults with CMML are not well-defined. These patients are more likely to be offered therapies impacting survival, such as, HMA and AHSCT. Given that the median age of presentation for CMML is in the seventh decade of life and since age >65 years was found to be an adverse prognosticator, for the purposes of this study, we defined ‘young' CMML as age ⩽65 years. We carried out this international collaborative effort to define the molecular and cytogenetic predictors of survival and treatment outcomes in ‘young' adults with CMML.
Materials and methods
The current study was an international collaborative effort between the Mayo Clinic, MN, USA the Moffitt Cancer Center, FL, USA, the GFM and the University of Milan in Italy, and was duly approved by the respective institutional review boards. Study eligibility criteria included availability of peripheral blood (PB) smear, bone marrow (BM) cytology or histology, and cytogenetic information at the time of referral to the respective institutions. As mentioned above, ‘young' CMML was defined as age ⩽65 years. The diagnoses of CMML, including sub-classification into CMML-1 or CMML-2 and documentation regarding the presence or absence of ring sideroblasts and leukemic transformation (LT) were according to the 2008 WHO (World Health Organization) criteria.16 All complete blood count differentials and PB smears were evaluated for presence of circulating IMCs, defined by the presence of any of the following cells in circulation; myeloblasts, myelocytes, metamyelocytes and promyelocytes.17
At the time of CMML diagnosis, DNA from BM or PB, was extracted using conventional methods. JAK2, ASXL1, SF3B1, SRSF2, U2AF1 and SETBP1 mutation analysis was performed according to previously published methods.2, 18, 19, 20, 21 Based on prior observations, only frame-shift and non-sense ASXL1 mutations were considered bona fide mutations.3, 4 In the French CMML cohort a sub-group of patients did have DNA analysis for TET2 and RAS mutations, while these were not done on the remainder.2
Karyotype risk designation and CMML risk stratification were according to the Spanish cytogenetic risk stratification system,22 the Mayo-French cytogenetic classification,5 the MD Anderson prognostic system (MDAPS),17 the GFM model,2 the Mayo Prognostic Model4 and the MMM.3 In the analysis of prognostic factors, variables included were: gender, HB, WBC, absolute neutrophil count, AMC, absolute lymphocyte count, platelet count, PB and BM blasts, circulating IMC, BM cellularity, WHO morphological subcategories (CMML-1 versus CMML-2), karyotype groups based on the Spanish cytogenetic risk stratification system and the Mayo-French cytogenetic classification, MDAPS, Mayo prognostic model, GFM model, MMM, ASXL1 mutations, spliceosome component mutations (SF3B1, SRSF2 and U2AF1) and SETBP1 mutations.
Treatment data collected included: best supportive care options (blood transfusions, hydroxyurea and erythropoiesis stimulating agents), the use of HMA (5-Azacitidine (AZA) and/or decitabine (DAC), either as single agents or in the setting of a clinic trial) and the use of AHSCT. Responses to HMA were graded according to the International Working Group (IWG) response criteria.23 For AHSCT, data collected included: donor source (matched related donor, matched unrelated donor (MUD), double umbilical cord blood units or haploidentical donors), graft type (PB versus BM), conditioning regimen (MA versus RIC) and transplant outcomes such as engraftment rates, acute and chronic GVHD, relapse free survival, NRM and OS.
All statistical analyses considered clinical and laboratory parameters obtained at the time of referral to the participating institutions, which in most instances coincided with the time of BM aspiration or biopsy and study sample collection. Differences in the distribution of continuous variables between categories were analyzed by either Mann–Whitney (for comparison of two groups) or Kruskal–Wallis (comparison of three or more groups) tests. Patient groups with nominal variables were compared by χ2-test. Overall survival was calculated from the date of first referral to the date of death (uncensored) or last contact (censored). Leukemia-free survival (LFS) was calculated from the date of first referral to date of LT (uncensored) or death/last contact (censored). Overall and LFS curves were prepared by the Kaplan–Meier method and compared by the log-rank test. Cox proportional hazard regression model was used for multivariable analysis. P-values <0.05 were considered significant. The Stat View (SAS Institute, Cary, NC, USA) statistical package was used for all calculations.
Results
Two hundred and sixty-one patients with WHO-defined CMML were included in the current international study: 105 (40%) were from the GFM cohort, 86 (33%) from Mayo Clinic Minnesota, 47 (18%) from the Moffitt Cancer Center Florida and 23 (9%) from the University of Milan. There were no statistically significant demographic, clinical or laboratory differences between patients from the four participating centers. Two hundred and nineteen (84%) patients had CMML-1 and 42 (16%) had CMML-2, with median OS of 59 months and 24 months, respectively. The median age of the cohort was 59 years (range, 18–65 years) and 73% (n=192) were males. Table 1 outlines the presenting clinical and laboratory features and subsequent events in the 261 study patients with CMML, stratified by their AHSCT status. At a median follow-up of 26 months, 126 (48%) deaths and 72 (28%) LTs were documented. Of 220 evaluable patients, 53 (24%) did undergo AHSCT and in this group at last follow-up 8 (19%) deaths were documented.
Table 1. Clinical and laboratory features and subsequent events in 261 ‘young' (age⩽65 years) adults with WHO-defined chronic myelomonocytic leukemia, stratified by allogenic stem cell transplant status.
| Variable | All patients n=261 | Transplanted patents n=53 (24%) | Non-transplant patients n=167 (76%) | P-value |
|---|---|---|---|---|
| Age in years; median (range) | 59 (18–65) | 52 (18–65) | 60 (20–65) | <0.0001 |
| Males; n (%) | 192 (73%) | 32 (60%) | 128 (77%) | 0.02 |
| Hemoglobin g/dl; median (range) | 11.0 (4.2–17.7) | 10.1 (4.2–15.5) | 10.9 (4.9–17.7) | 0.006 |
| WBC × 109/l; median (range) | 12.4 (1.8–180.0) | 14.8 (2.5–133.0) | 11.4 (1.8–180) | 0.08 |
| ANC × 109/l; median (range) | 5.7 (0.2–151) | 5.9 (0.3–92.6) | 5.3 (0.2–151) | 0.5 |
| AMC × 109/l; median (range) | 2.6 (0.3–62.8) | 3.1 (0.6–62.8) | 2.6 (0.3–44) | 0.3 |
| ALC × 109/l; median (range) | 2.1 (0–12.5) | 2.6 (0.3–12.5) | 2.0 (0–8.1) | 0.01 |
| Platelets × 109/l; median (range) | 99 (6–1427) | 72 (6–1064) | 107 (10–1427) | 0.1 |
| PB blast % median (range) | 0 (0–16) | 0 (0–16) | 0 (0–16) | 0.1 |
| BM blast % median (range) | 4 (0–18) | 6 (0–18) | 4 (0–16) | 0.001 |
| Circulating immature myeloid cells; n (%) ‘N' evaluable=258 | 141 (55%) | 29 (55%) | 86 (52%) | 0.8 |
| WHO morphological subtype; n (%) | ||||
| CMML-1 | 219 (84%) | 36 (68%) | 146 (87%) | 0.001 |
| CMML-2 | 42 (16%) | 17 (32%) | 21 (13%) | — |
| ASXL1 mutations; ‘N' evaluable=174 | 58 (33%) | 7 (28%) | 37 (34%) | 0.6 |
| SETBP1 mutations; ‘N' evaluable=164; n (%) | 7 (4%) | 0 (0%) | 4 (4%) | 0.3 |
| Spliceosome component mutations; | ||||
| SF3B1 ‘N' evaluable=113 | 9 (8%) | 1 (6%) | 5 (9%) | 0.7 |
| SRSF2 ‘N' evaluable=161 | 72 (45%) | 8 (33%) | 47 (48%) | 0.2 |
| U2AF1 ‘N' evaluable=111 | 5 (4%) | 1 (6%) | 3 (5%) | 0.9 |
| Spanish cytogenetic risk stratification; ‘N' evaluable=246 n (%) | ||||
| Low | 196 (80%) | 40 (75%) | 124 (78%) | 0.7 |
| Intermediate | 28 (11%) | 6 (11%) | 20 (13%) | — |
| High | 22 (9%) | 7 (13%) | 15 (9%) | — |
| Mayo-French cytogenetic risk stratification; ‘N' evaluable=246, n(%) | ||||
| Low | 200 (81%) | 40 (75%) | 126 (79%) | 0.6 |
| Intermediate | 39 (16%) | 12 (23%) | 27 (17%) | — |
| High | 7 (3%) | 1 (2%) | 6 (4%) | — |
| MD Anderson prognostic risk categories; n (%) ‘N' evaluable=254 | ||||
| Low | 111 (44%) | 17 (33%) | 74 (46%) | 0.02 |
| Intermediate-1 | 51 (20%) | 17 (33%) | 50 (31%) | — |
| Intermediate-2 | 85 (33%) | 13 (25%) | 35 (67%) | — |
| High | 7 (3%) | 5 (10%) | 2 (1%) | — |
| Mayo Model prognostic risk categories; n (%) ‘N' evaluable=259 | ||||
| Low | 65 (25%) | 9 (17%) | 48 (29%) | 0.1 |
| Intermediate | 92 (36%) | 18 (34%) | 58 (35%) | — |
| High | 102 (39%) | 26 (49%) | 59 (36%) | — |
| Mayo Molecular Model ‘N' evaluable=171 | ||||
| Low | 20 (12%) | 1 (4%) | 13 (12%) | — |
| Intermediate-1 | 46 (26%) | 5 (20%) | 31 (29%) | 0.1 |
| Intermediate-2 | 61 (36%) | 8 (32%) | 39 (37%) | — |
| High | 44 (26%) | 11 (44%) | 23 (22%) | — |
| GFM prognostic risk categories; n (%) ‘N' evaluable=171 | ||||
| Low | 106 (62%) | 12 (48%) | 68 (64%) | 0.2 |
| Intermediate | 61 (36%) | 13 (52%) | 35 (33%) | — |
| High | 4 (2%) | 0 (0%) | 3 (3%) | — |
| — | — | — | — | |
| Leukemic transformations; n (%) ‘N' evaluable=258 | 72 (28%) | — | — | — |
| Before transplant | — | 19 (36%) | 41 (24%) | — |
| After transplant | — | 5 (9%) | — | — |
| Deaths; n (%) | 126 (48%) | 25 (47%) | 92 (55%) | 0.3 |
Abbreviations: ALC, absolute lymphocyte count; AMC, absolute monocyte count; ANC, absolute neutrophil count; ASXL1, additional sex combs 1 gene; BM, bone marrow; CMML, chronic myelomonocytic leukemia; GFM, Groupe Francais des Myelodsyplasies; PB, peripheral blood; SF3B1, splicing factor 3B, subunit 1; SRSF2, serine/arginine-rich splicing factor 2; U2AF1, U2 small nuclear RNA auxiliary factor 1; WBC, white blood cell count; WHO, World Health Organization.
Mayo-French cytogenetic risk stratification: Low risk, normal karyotype, −Y and sole der (3q); high risk, complex and monosomal karyotype; intermediate all other karyotype abnormalities; Spanish cytogenetic risk stratification: Low risk, −Y and normal karyotype; high risk, +8, −chromosome 7 abnormalities and complex karyotype: intermediate risk, all other abnormalities. Bold entries signify statistically significant P-values (i.e. P<0.05).
Cytogenetic information was available in 246 (94%) patients; 60 (23%) displayed an abnormal karyotype and the Mayo-French cytogenetic risk designations included 200 (81%) low, 39 (16%) intermediate and 7 (3%) high risk. The common cytogenetic abnormalities included: −7(18%), +8 (16%), −Y (14%), der(3q) (13%) and 20q-(9%). Forty-five (80%) of the 60 patients had a sole abnormality, while 4 (7%) had two, 7 (13%) had a complex karyotype and 6 (11%) had a monosomal karyotype.
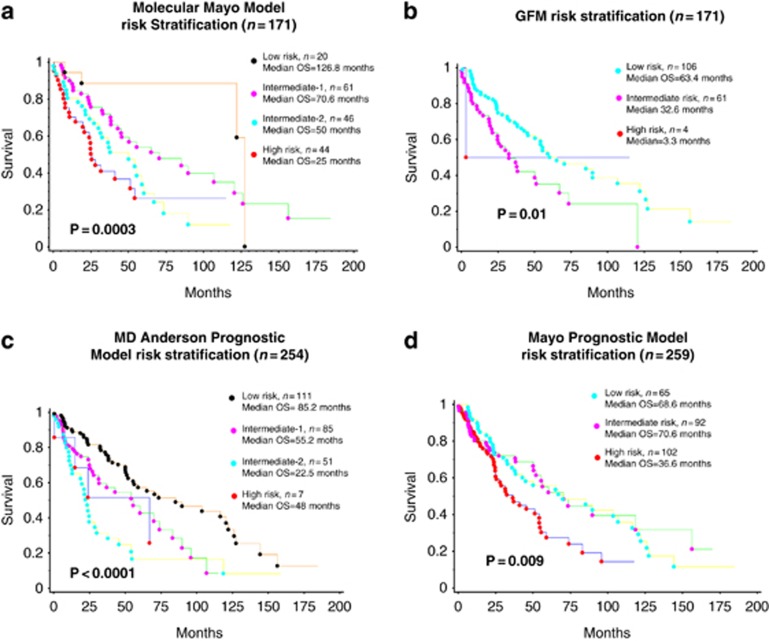
Mutational frequencies were 45% (72/161) for SRSF2, 33% (58/174) for ASXL1, 8% (9/113) for SF3B1, 4% (7/164) for SETBP1 and 4% (5/111) for U2AF1. The most common ASXL1 mutation was the c.1934dupG; p.G646WfsX12 variant (40%), followed by the 1900_1922_ del (11%). The most common SRSF2 mutations were P95H (33%) and P95L (33%), while K700E (90%) was the most common SF3B1 mutation. In the French CMML cohort, of the 53 evaluable patients 29(53%) had TET2 mutations, while of the 59 evaluable patients 13 (22%) had RAS mutations (NRAS-10 and KRAS-3). The distribution according to the four studied risk stratification algorithms is shown in Figure 1. For example, the distribution according to the MMM was: 20 (12%) low, 46 (26%) intermediate-1, 61 (36%) intermediate-2 and 44 (26%) high risk.
Figure 1.
Overall survival of ‘young' adults with chronic myelomonocytic leukemia stratified by contemporary prognostic models. (a) Overall survival of 171 ‘young' adults with chronic myelomonocytic leukemia stratified by the Molecular Mayo Model. (b) Overall survival of 171 ‘young' adults with chronic myelomonocytic leukemia stratified by the GFM model. (c) Overall survival of 254 ‘young' adults with chronic myelomonocytic leukemia stratified by the MD Anderson prognostic model. (d) Overall survival of 257 ‘young' adults with chronic myelomonocytic leukemia stratified by the Mayo prognostic model.
Survival
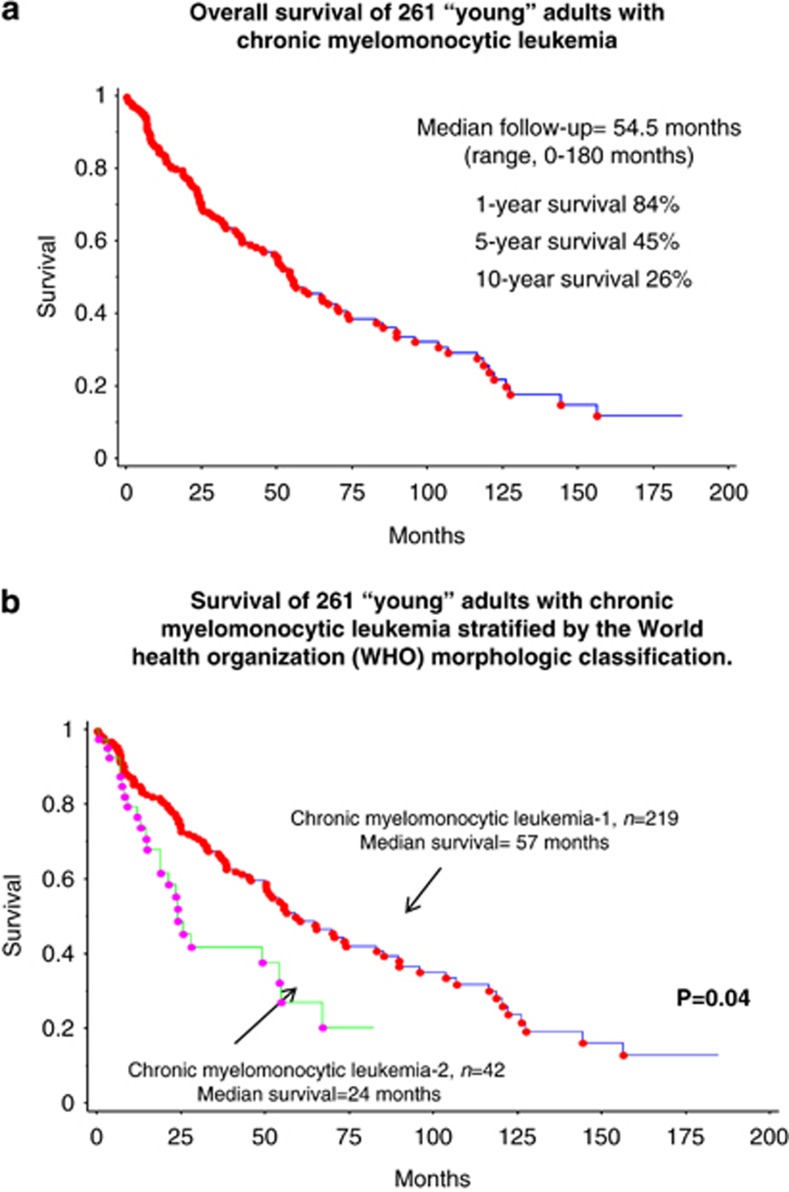
Figure 2a demonstrates the OS of 261 ‘young' adults with CMML. With a median follow-up of 54.5 months, overall survival was 84% at 1 year, 45% at 5 years, and 26% at 10 years, with a median survival of 55 months. The median OS for CMML-1 and CMML-2 were 59 months and 24 months, respectively (Figure 2b). In an univariate OS analysis, after censoring for AHSCT lower HB (P<0.0001), higher WBC (P=0.0002), higher absolute neutrophil count (P=0.001), higher AMC (P=0.0004), higher circulating blast % (P<0.0001), higher BM blast % (P=0.02), presence of circulating IMC (P<0.0001), ASXL1 mutations (P=0.003), SRSF2 mutations (P=0.04), the Mayo-French cytogenetic risk stratification (P<0.0001) and the Spanish cytogenetic risk stratification system (P=0.0002) predicted shortened survival (Table 2). In multivariable analysis, lower HB (P=0.01), higher circulating blast % (P=0.002), ASXL1 mutations (P=0.0007), SRSF2 mutations (P=0.008) and the Mayo-French cytogenetic risk stratification system (P=0.04) retained their negative prognostic impact. Interestingly, without censoring for AHSCT, on a multivariable analysis OS was independently affected by lower HB (P=0.01), lower platelets (P=0.03), higher circulating blast % (P=0.001), SRSF2 mutations (P=0.04) and the high risk stratification of the Mayo-French cytogenetic stratification (P=0.02; Table 2). SETBP1 mutations had no impact on OS.
Figure 2.
(a) Overall survival of 261 ‘young' adults with chronic myelomonocytic leukemia. (b) Survival of 261 ‘young' adults with chronic myelomonocytic leukemia stratified by the World health organization (WHO) morphologic classification.
Table 2. Univariate and multi-variable analysis of survival and leukemic transformation in 261 ‘young' adults with chronic myelomonocytic leukemia.
| Variable | Censor survival univariate | Censor survival multivariate | Censor transplant univariate | Censor transplant multivariate | Censor leukemic transformation univariate | Censor leukemic transformation multivariate |
|---|---|---|---|---|---|---|
| Older age | 0.99 | — | 0.89 | — | 0.1 | — |
| Males | 0.5 | — | 0.8 | — | 0.5 | — |
| Lower hemoglobin g/dl | <0.0001 | 0.01 | <0.0001 | 0.01 | <0.0001 | — |
| Higher WBC × 109/l | 0.002 | — | 0.0002 | — | 0.2 | — |
| Higher ANC × 109/l | 0.005 | — | 0.001 | — | 0.7 | — |
| Higher AMC × 109/l) | 0.02 | — | 0.0004 | — | 0.01 | — |
| Higher ALC × 109/l | 0.9 | — | 0.3 | — | 0.07 | — |
| Lower platelets × 109/l | 0.004 | 0.03 | 0.2 | — | 0.1 | — |
| Higher PB blast % | <0.0001 | 0.001 | <0.0001 | 0.002 | <0.0001 | <0.0001 |
| Higher BM blast % | 0.007 | — | 0.02 | — | <0.0001 | 0.0007 |
| Presence of circulating immature myeloid cells | 0.007 | — | <0.0001 | — | <0.0001 | 0.0002 |
| ASXL1 mutations | 0.06 | — | 0.003 | 0.007 | 0.8 | — |
| SETBP1 mutations | 0.07 | — | 0.05 | — | 0.4 | — |
| SF3B1 | 0.5 | — | 0.2 | 0.7 | — | |
| SRSF2 | 0.03 | 0.04 | 0.04 | 0.008 | 0.7 | — |
| U2AF1 | 0.2 | — | 0.5 | — | — | — |
| Mayo-French cytogenetic risk stratification | <0.0001 | HOLDS for high risk 0.02 | <0.0001 | 0.04 | <0.0001 | — |
| Spanish cytogenetic risk stratification; | <0.0001 | — | 0.0002 | — | <0.0001 | — |
Abbreviations: ALC, absolute lymphocyte count; AMC, absolute monocyte count; ANC, absolute neutrophil count; ASXL1, additional sex combs 1 gene; BM, bone marrow; PB, peripheral blood; SETBP1, SET binding protein 1; SF3B1, splicing factor 3B, subunit 1; SRSF2, serine/arginine-rich splicing factor 2; U2AF1, U2 small nuclear RNA auxiliary factor 1; WBC, white blood cell count.
Mayo-French cytogenetic risk stratification; Low risk, normal karyotype, −Y and sole der (3q), High risk, complex and monosomal karyotype, Intermediate all other karyotype abnormalities, Spanish cytogenetic risk stratification; Low risk, −Y and normal karyotype, High risk, +8, −chromosome 7abnormalities and complex karyotype, Intermediate risk, all other abnormalities. Bold entries signify statistically significant P-values (i.e. P<0.05).
Similarly, in a univariate analysis for LFS lower HB (P<0.0001), higher AMC (P=0.01), higher circulating blast% (P<0.0001), higher BM blast % (P<0.0001), presence of circulating IMC (P<0.0001), the Mayo-French cytogenetic risk stratification (P<0.0001) and the Spanish cytogenetic risk stratification (P<0.0001) predicted shortened survival (Table 2). In multivariable analysis, LFS was independently affected by higher circulating blast % (P<0.0001), higher BM blast % (P=0.0007) and the presence of circulating IMC (P=0.0002). Karyotype risk designation, ASXL1, SETBP1 and SRSF2 mutations had no impact on LFS.
Response to HMAs
Seventy-five (29%) patients received HMA, of which, 45 (60%) received 5-AZA, 30 (40%) received DAC and 7 (9%) received both. Table 3 outlines the treatment characteristics and outcomes of ‘young' CMML patients that received HMA. In the 5-AZA group, the median age was 56 years and 78% (n=35) were male. Thirty-five (78%) had CMML-1, while 10 (22%) had CMML-2. Of 20 evaluable patients, 9 (45%) had ASXL1 mutations. The risk designations according to the MMM were: 3 (16%) high, 7 (37%) intermediate-2, 8 (42%) intermediate-1 and 1 (5%) low risk (evaluable n=19). The median number of cycles was 5 (range, 1–44), median duration of therapy 4.6 months (range, 0.1–32.2), with 5 (11%) receiving DAC on progression and 20 (39%) proceeding with AHSCT. The over-all response rate was 40% (n=18/45) and included complete response (CR) in 3 (7%), partial response in 10 (25%) and hematological improvement (HI) in 5 (12%). Of 30 evaluable patients, reasons for 5-AZA discontinuation included patient choice-1 (3%), 5-AZA intolerance-3 (10%), disease progression-14 (47%), death-4 (13%) and bridge to AHSCT-8 (27%).
Table 3. Treatment of ‘young' CMML patients (age⩽65) with hypomethylating agents and their outcome stratified by their allogenic stem cell transplant status.
| Variables | All n=75 | CMML patients that underwent Allogenic transplant n=29 (39%) | CMML patients without transplant n=45 (61%) | P-value |
|---|---|---|---|---|
| 1. 5-Azacitidine n (%) | 45 (60%) | 20 (71%) | 25 (56%) | — |
| Age | 56 (30–65) | 52 (30–63) | 59 (44–65) | 0.0009 |
| Male (%) | 35 (78%) | 14 (70%) | 21 (84%) | 0.3 |
| WHO morphological subtype; n (%) | ||||
| CMML-1 | 35 (78%) | 16 (80%) | 19 (76%) | 0.7 |
| CMML-2 | 10 (22%) | 4 (20%) | 6 (24%) | — |
| ASXL1 mutated ‘N' evaluable=20 | 9 (45%) | 4 (50%) | 5 (42%) | 0.7 |
| SRSF2 mutated ‘N' evaluable=19 | 9 (47%) | 2 (22%) | 7 (70%) | 0.04 |
| Mayo Molecular Model risk categorization ‘N' evaluable=19 | ||||
| Low | 1 (5%) | 0 (0%) | 1 (9%) | — |
| Intermediate-1 | 8 (42%) | 4 (50%) | 4 (36%) | 0.3 |
| Intermediate-2 | 7 (37%) | 0 (0%) | 3 (27%) | — |
| High | 3 (16%) | 4 (50%) | 3 (27%) | — |
| Mayo-French cytogenetic stratification ‘N' evaluable=74 | ||||
| Low | 33 (73%) | 14 (70%) | 19 (76%) | 0.5 |
| Intermediate | 11 (24%) | 6 (30%) | 5 (20%) | — |
| High | 1 (2%) | 0 (0%) | 1 (4%) | — |
| Median cycles (range) | 5 (1–44) | 4 (2–44) | 6 (1–36) | 0.3 |
| Median duration of therapy in months (range) | 4.6 (0.1–32) | 3.8 (0.1–18) | 4.6 (0.1–32) | 0.6 |
| Best response ‘N' evaluable=40 | ||||
| HI | 5 (13%) | 2 (10%) | 3 (14%) | 0.4 |
| PR | 10 (25%) | 6 (32%) | 4 (19%) | — |
| CR | 3 (7%) | 0 (0%) | 3 (14%) | — |
| No response | 22 (55%) | 11 (58%) | 7 (33%) | — |
| Reason for discontinuation of therapy ‘N' evaluable=30 | ||||
| Patient choice | 1 (3%) | 0 (0%) | 1 (6%) | — |
| Intolerance | 3 (10%) | 0 (0%) | 3 (18%) | 0.01 |
| Progression | 14 (47%) | 7 (47%) | 7 (41%) | — |
| Bridge to transplant | 8 (27%) | 8 (53%) | 0 (0%) | — |
| Death | 4 (13%) | 0 (0%) | 4 (23%) | — |
| Second HMA n (%) | 5 (11%) | 3 (15%) | 2 (8%) | — |
| 2. Decitabine | 30 (40%) | 9 (31%) | 20 (68%) | — |
| Age | 58 (33–65) | 57 (43–65) | 59 (33–65) | 0.7 |
| Male (%) | 18 (60%) | 3 (37%) | 15 (75%) | 0.6 |
| WHO morphological subtype; n (%) | ||||
| CMML-1 | 21 (70%) | 5 (56%) | 16 (76%) | 0.3 |
| CMML-2 | 9 (30%) | 4 (44%) | 5 (24%) | — |
| ASXL1 mutated ‘N' evaluable=21 | 6 (28%) | 1 (20%) | 5 (31%) | 0.6 |
| SRSF2 mutated ‘N' evaluable=15 | 7 (47%) | 1 (33%) | 6 (54%) | 0.5 |
| Mayo Molecular Model risk categorization ‘N' evaluable=19 | ||||
| Low | 2 (10%) | 0 (0%) | 2 (14%) | 0.5 |
| Intermediate-1 | 6 (32%) | 1 (20%) | 5 (36%) | — |
| Intermediate-2 | 7 (37%) | 2 (40%) | 5 (36%) | — |
| High | 4 (21%) | 2 (40%) | 2 (14%) | — |
| Mayo-French cytogenetic risk stratification ‘N' evaluable=29 | ||||
| Low | 22 (76%) | 7 (78%) | 14 (74%) | 0.8 |
| Intermediate | 6 (21%) | 2 (22%) | 4 (21%) | — |
| High | 1 (3%) | 0 (0%) | 1 (5%) | — |
| Median number of cycles (range) | 6 (1–30) | 4 (1–12) | 7 (2–25) | 0.4 |
| Median duration of therapy in months (range) | 5.0 (0.1–49) | 4.2 (0.1–13) | 5.0 (1.0–49) | 0.1 |
| Best response ‘N' evaluable=20 | ||||
| HI | 2 (10%) | 1 (14%) | 1 (8%) | — |
| PR | 1 (5%) | 0 (0%) | 1 (8%) | 0.3 |
| CR | 6 (32%) | 1 (14%) | 5 (38%) | — |
| No response | 11 (55%) | 5 (71%) | 6 (46%) | — |
| Reason for discontinuation of therapy ‘n' evaluable=15 | ||||
| Progression | 9 (60%) | 2 (40%) | 7 (70%) | 0.03 |
| Bridge to transplant | 3 (20%) | 3 (60%) | 0 (0%) | — |
| Death | 3 (20%) | 0 (0%) | 3 (30%) | — |
| Second HMA n (%) | 2 (7%) | 0 (0%) | 2 (10%) | — |
Abbreviations: ASXL1, additional sex combs 1 gene; CMML, chronic myelomonocytic leukemia; CR, complete remission; HI, hematologic improvement; HMA, hypomethylating agent; PR, partial remission; SRSF2, serine/arginine-rich splicing factor 2; WHO, World Health Organization. Bold entries signify statistically significant P-values (i.e. P<0.05).
Thirty (40%) patients received DAC; with the median age being 58 years (range, 33–65), with a male predilection (60%) (Table 3). Twenty-one (70%) had CMML-1, while 9 (30%) had CMML-2. Of 21 evaluable patients, 6 (28%) had ASXL1 mutations and the risk designations according to the MMM were: 4 (21%) high risk, 7 (37%) intermediate-2, 6 (32%) intermediate-1 and 2 (10%) low risk. The median number of cycles was 6 (range, 1–30), median duration of therapy 5 months (range, 0.1–49), with two (7%) receiving DAC on progression and nine (31%) proceeding with AHSCT. The over-all response rate was 30% (n=9/30) and included CR in 6 (32%), partial response in one (5%) and HI in two (10%). Of 15 evaluable patients, reasons for DAC discontinuation included disease progression-9 (60%), death-3(20%) and bridge to AHSCT-3 (20%). Neither did ASXL1 (P=0.4) and SRSF2 (P=0.7) mutational status, nor karyotype (P=0.3 for Mayo-French cytogenetic stratification and 0.5 for the Spanish stratification) correlate with response to HMA. In 53 evaluable patients in the French cohort, TET2 mutations demonstrated a trend toward predicting HMA response (P=0.5), but this did not reach statistical significance.
Outcomes of AHSCT
Fifty-three patients (20%) underwent AHSCT. Conditioning regimen was reported in 42 patients and included MA in 14 (33%) and reduced intensity in 28 (67%) (Table 4). Donor source was documented in 40 patients and included: matched related donor in 20 (50% MA-7 and RIC-13), MUD in 13 (32% MA-4, RIC-9), 9/10 mismatched unrelated donor in 4 (10% MA-1, RIC-3), double umbilical cord blood units in 1 (3% MA-1) and RIC haploidentical transplants in 2 (8%). In the MA group, the median age was 51 years (range, 27–62), 32 (60%) were males and 36 (68%) had CMML-1, while the remaining 17 (32%) had CMML-2. In the RIC group, the median age was 48 years (range, 18–65), 8 (57%) were males, 21 (75%) had CMML-1, while the remaining 7 (25%) had CMML-2. Of 25 evaluable patients, 7 (28%) had ASXL1 mutations (MA-3, RIC-4) and the risk designation according to the MMM was: high-11 (44%), intermediate-2-5 (20%), intermediate-1-8 (32%) and low risk-1 (4%). Nineteen patients (47%) developed grade II–IV acute GVHD, 7 (54%) with a MA regimen and 12 (46%) with RIC, while 29 (67%) developed chronic GVHD, 8 (57%) with a MA regimen and 21 (75%) with RIC. Of 43 evaluable patients, 1 (2%) had primary engraftment failure, 8 died secondary to treatment related causes (NRM-19%), 10 (25%) had disease relapse and 24 (56%) achieved a CR. Neither did ASXL1 (P=0.9) and SRSF2 (P=0.5) mutational status, nor karyotype (P=0.3 for Mayo-French cytogenetic stratification and 0.2 for the Spanish stratification) correlate with response to AHSCT.
Table 4. Clinical and laboratory features of 53 ‘young' adults (age⩽65 years) with chronic myelomonocytic leukemia that underwent allogeneic stem cell transplantation and their outcomes.
| Variables | All N=53 | Myeloablative conditioning N=14 (33%) | Reduced intensity conditioning N=28 (67%) | P-value |
|---|---|---|---|---|
| Age | 52 (18–65) | 51 (27–62) | 48 (18–65) | 0.7 |
| Sex | 32 (60%) | 8 (57%) | 8 (57%) | 1.0 |
| WHO morphological subtype; n (%) | ||||
| CMML-1 | 36 (68%) | 8 (57%) | 21 (75%) | 0.2 |
| CMML-2 | 17 (32%) | 6 (43%) | 7 (25%) | — |
| ASXL1 ‘N' evaluable= 25 | 7 (28%) | 3 (33%) | 1 (14%) | 0.4 |
| SRSF2 ‘N' evaluable=24 | 8 (33%) | 4 (44%) | 2 (29%) | 0.5 |
| Mayo-French cytogenetic risk stratification | — | — | — | 0.7 |
| Low | 40 (75%) | 11 (79%) | 19 (68%) | — |
| Intermediate | 12 (23%) | 3 (21%) | 8 (29%) | — |
| High | 1 (2%) | — | 1 (3%) | — |
| Mayo Molecular Model risk categorization ‘N' evaluable=25 | ||||
| Low | 1 (4%) | 0 (0%) | 1 (14%) | 0.5 |
| Intermediate-1 | 8 (32%) | 2 (22%) | 1 (14%) | — |
| Intermediate-2 | 5 (20%) | 3 (33%) | 1 (14%) | — |
| High | 11 (44%) | 4 (44%) | 4 (57%) | — |
| Mayo-French cytogenetic risk stratification ‘N' evaluable=53 | ||||
| Low | 40(75%) | 11 (79%) | 19 (68%) | 0.7 |
| Intermediate | 12 (23%) | 3 (21%) | 8 (29%) | — |
| High | 1 (2%) | 0 (0%) | 1 (3%) | — |
| Graft source ‘N' evaluable=40 | ||||
| Matched sibling donor | 20 (50%) | 7 (54%) | 12 (46%) | 0.5 |
| Matched unrelated donor | 13 (32%) | 4 (31%) | 9 (35%) | — |
| Mismatched unrelated donor | 4 (10%) | 1 (8%) | 3 (11%) | — |
| Umbilical cord blood units | 1 (3%) | 1 (8%) | 0 (0%) | — |
| Haploidentical donor | 2 (5%) | 0 (0%) | 2 (8%) | — |
| Acute GVHD ‘N' evaluable=40 | 19 (47%) | 10 (76%) | 9 (35%) | 0.01 |
| Chronic GVHD ‘N' evaluable=43 | 29 (67%) | 8 (57%) | 21 (75%) | 0.2 |
| Outcome of transplant ‘N' evaluable=43 | ||||
| CR | 24 (56%) | 8 (61%) | 15 (55%) | 0.4 |
| Relapse | 10 (23%) | 1 (8%) | 7 (26%) | — |
| Death | 8 (19%) | 4 (31%) | 4 (15%) | — |
| Failure | 1 (2%) | 0 (0%) | 1 (4%) | — |
Abbreviations: ASXL1, additional sex combs 1 gene; CMML, chronic myelomonocytic leukemia; CR, complete remission; GVHD, graft versus host disease; SRSF2, serine/arginine-rich splicing factor 2; WHO, World Health Organization. Bold entries signify statistically significant P-values (i.e. P<0.05).
Discussion
CMML is uncommon in ‘young' adults and is often associated with significant morbidity and mortality. Ours is the first comprehensive study evaluating presenting features, risk stratification and treatment outcomes in ‘young' CMML patients, defined by age ⩽65 years. The male predilection (73%), distribution across WHO morphological sub-categories (CMML-1 84%) and presenting laboratory features were similar to larger CMML studies analyzing all age groups.2, 3, 4 Cytogenetic abnormalities were seen in 23% of patients, with a lower frequency of +8 (16% versus 23%) and –Y (14% versus 20%) in comparison to the Mayo-French cytogenetic study cohort.5 On the other hand there was a higher frequency of der(3q) (13% versus 8%) and −7/del7q (18% versus 14%). None of the patients with der(3q) had the classical t(3;3)(q21;q26) or inv3(q21;q26), and fluorescence in situ hybridization studies for EVI1 were negative. This abnormality (der(3q)) has been associated with favorable outcomes in patients with CMML.5
ASXL1 mutations were seen in 33% of the patients (compared with 39% and 40% in the Mayo Clinic and GFM studies, respectively), while SRSF2 mutations were seen in 45% of the patients (compared with 43% and 46% in the Mayo Clinic and GFM studies, respectively).2, 4 The median OS for CMML-1 and CMML-2 were 59 months and 24 months, respectively (compared with 38 months and 24 months in the combined Mayo-French study of 466 patients).3 The risk designations based on the Spanish cytogenetic risk stratification, Mayo Prognostic model, MDAPS and the MMM were similar, with the only exception being that there were no ‘young' patients with high risk GFM disease stratification, as age >65 years is considered an adverse prognosticator in the GFM model.2
Contemporary prognostic models have identified anemia, thrombocytopenia, circulating IMC, high WBC/AMC and ASXL1 mutations to be negatively prognostic for OS.2, 3 In the current study, platelet count, WBC/AMC and circulating IMC did not impact OS. In addition to anemia and ASXL1 mutations, circulating blast %, SRSF2 mutations and risk stratification by the Mayo-French cytogenetic classification were independently prognostic. SRSF2 mutations affect pre-messenger RNA splicing and have been shown to exert a negative prognostic impact in myelodysplastic syndrome24 and primary myelofibrosis,19 but not in CMML.3, 20 Their negative prognostic impact in ‘young' adults with CMML needs further elucidation. The LT rate in ‘young' patients was slightly higher at 28%, compared with 22% in the GFM study and 17% in the Mayo-French study. Factors impacting LFS included circulating and BM blast% and the presence of IMC. Notably, karyotypic risk designation, ASXL1 and SRSF2 mutations did not impact LFS.
While prospective phase III data with HMA is lacking in CMML, these agents are often used for the management of symptomatic patients. Currently 5-AZA and DAC are approved for patients with myelodysplastic syndrome in the USA, while in Europe DAC has only been approved for elderly patients with de novo acute myeloid leukemia, potentially explaining the higher number of ‘young' patients who received 5-AZA (60%). In this study, patients received a median of five cycles of 5-AZA and six cycles of DAC, for a median duration of 5 months, with an over-all response rate of 40% for 5-AZA and 30% for DAC; once again similar to other observational studies.6, 7, 8, 9, 10, 11, 12 Response prediction to HMA has been challenging. Braun et al.8 demonstrated that ASXL1, NRAS, KRAS, CBL, FLT3 and JAK2 mutations did not predict response or survival in 39 CMML patients treated with DAC. However, lower CJUN and CMYB gene expression levels independently predicted improved OS. There was a trend toward higher response rate in patients with TET2 mutations (when not associated with an ASXL1 mutation).8 Recently, in myelodysplastic syndrome, clonal TET2 mutations were shown to predict HMA responses (odds ratio 1.99, P=0.036), especially when they occurred independent of clonal ASXL1 mutations.25 In our study, neither ASXL1 nor SRSF2 mutations predicted HMA response. In a smaller sub-set of ‘young' French patients (n=53), while there was a trend toward better HMA responses in TET2 mutated patients (P=0.5), this did not reach statistical significance.
AHSCT is the only potentially curative option, and is more likely to be offered to ‘young' adults with CMML. Eissa et al.13 reported outcomes on 85 patients with CMML (median age 52 years) that underwent AHSCT (32% RIC). After a median follow-up of 5.2 years 49 (58%) had died; 20 from disease relapse and 29 from non-relapse causes. About 26% developed grade II–IV acute GVHD and 40% developed chronic GVHD. A multivariable model identified increasing age, high SCT comorbidity index and poor risk cytogenetics as independent prognosticators for poor survival. A recent European study, evaluated AHSCT in 73 patients (median age 53 years) with CMML (61% CMML-1, 43 RIC).26 The three year OS was 32%, NRM 36% and the cumulative incidence of relapse was 35%. Survival was not influenced by the CR status, BM blast% at AHSCT, prior treatments and chronic GVHD. In our study, 53 (24%) patients underwent an AHSCT, with 67% receiving a RIC. About 44% had high risk disease according to the MMM and 50% received stem cells from a matched related donor. Alternative donor sources used included: MUDs (32%), mismatched unrelated donors (10%), double umbilical cord blood units (3%) and haploidentical transplants (5%). Acute GVHD was seen in 47%, while chronic GVHD was seen in 67% of patients. There was one case of engraftment failure, involving a patient who received an umbilical cord blood transplant. The response rate (CR) was 56%, NRM 19% and relapse rate 23%. Once again, ASXL1, SRSF2 mutational status and karyotype designations did not affect transplant outcomes.
In summary, this is the largest study analyzing survival and treatment outcomes in ‘young' adults with CMML. Survival in these patients, although higher than in older patients, is poor and is even worse in the setting of ASXL1 and SRSF2 mutations. These mutations, however, did not predict HMA response or impact transplant outcomes, suggesting that these treatments could erase the poor prognostic impact of these mutations in patients receiving only supportive care.
Acknowledgments
This study is supported in part by grants from the Myeloproliferative Disorders Foundation, Chicago, IL, USA and The Henry J. Predolin Foundation for Research in Leukemia, Mayo Clinic, Rochester, MN, USA.
Footnotes
The authors declare no conflict of interest.
References
- Patnaik MM, Parikh SA, Hanson CA, Tefferi A. Chronic myelomonocytic leukaemia: a concise clinical and pathophysiological review. Br J Haematol 2014; 165: 273–286. [DOI] [PubMed] [Google Scholar]
- Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol 2013; 31: 2428–2436. [DOI] [PubMed] [Google Scholar]
- Patnaik MM, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia 2014; 28: 2206–2212. [DOI] [PubMed] [Google Scholar]
- Patnaik MM, Padron E, LaBorde RR, Lasho TL, Finke CM, Hanson CA et al. Mayo prognostic model for WHO-defined chronic myelomonocytic leukemia: ASXL1 and spliceosome component mutations and outcomes. Leukemia 2013; 27: 1504–1510. [DOI] [PubMed] [Google Scholar]
- Wassie EA, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA et al. Molecular and prognostic correlates of cytogenetic abnormalities in chronic myelomonocytic leukemia: a Mayo Clinic-French Consortium Study. Am J Hematol 2014; 89: 1111–1115. [DOI] [PubMed] [Google Scholar]
- Ades L, Sekeres MA, Wolfromm A, Teichman ML, Tiu RV, Itzykson R et al. Predictive factors of response and survival among chronic myelomonocytic leukemia patients treated with azacitidine. Leuk Res 2013; 37: 609–613. [DOI] [PubMed] [Google Scholar]
- Aribi A, Borthakur G, Ravandi F, Shan J, Davisson J, Cortes J et al. Activity of decitabine, a hypomethylating agent, in chronic myelomonocytic leukemia. Cancer 2007; 109: 713–717. [DOI] [PubMed] [Google Scholar]
- Braun T, Itzykson R, Renneville A, de Renzis B, Dreyfus F, Laribi K et al. Molecular predictors of response to decitabine in advanced chronic myelomonocytic leukemia: a phase 2 trial. Blood 2011; 118: 3824–3831. [DOI] [PubMed] [Google Scholar]
- Costa R, Abdulhaq H, Haq B, Shadduck RK, Latsko J, Zenati M et al. Activity of azacitidine in chronic myelomonocytic leukemia. Cancer 2011; 117: 2690–2696. [DOI] [PubMed] [Google Scholar]
- Fianchi L, Criscuolo M, Breccia M, Maurillo L, Salvi F, Musto P et al. High rate of remissions in chronic myelomonocytic leukemia treated with 5-azacytidine: results of an Italian retrospective study. Leuk Lymphoma 2013; 54: 658–661. [DOI] [PubMed] [Google Scholar]
- Garcia-Manero G, Gore SD, Cogle C, Ward R, Shi T. Macbeth KJ, et al. Phase I study of oral azacitidine in myelodysplastic syndromes, chronic myelomonocytic leukemia, and acute myeloid leukemia. J Clin Oncol 2011; 29: 2521–2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe M, Montalvao A, Pierdomenico F, Moita F, Almeida A. Treatment of chronic myelomonocytic leukemia with 5-Azacitidine: a case series and literature review. Leuk Res 2012; 36: 1071–1073. [DOI] [PubMed] [Google Scholar]
- Eissa H, Gooley TA, Sorror ML, Nguyen F, Scott BL, Doney K et al. Allogeneic hematopoietic cell transplantation for chronic myelomonocytic leukemia: relapse-free survival is determined by karyotype and comorbidities. Biol Blood Marrow Transplant 2011; 17: 908–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Labopin M, Yakoub-Agha I, Delaunay J, Dhedin N, Deconinck E et al. Allogeneic stem cell transplantation for chronic myelomonocytic leukemia: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Eur J Haematol 2013; 90: 355–364. [DOI] [PubMed] [Google Scholar]
- Tefferi A, Lasho TL, Jimma T, Finke CM, Gangat N, Vaidya R et al. One thousand patients with primary myelofibrosis: the mayo clinic experience. Mayo Clinic Proc 2012; 87: 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swederlow S, Camp E, Harris NL, Jaffe ES, Stefano PA, Stein H (ed) WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer: Lyon, France, 2008. [Google Scholar]
- Onida F, Kantarjian HM, Smith TL, Ball G, Keating MJ, Estey EH et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood 2002; 99: 840–849. [DOI] [PubMed] [Google Scholar]
- Laborde R, Patnaik M, Lasho T, Finke C, Hanson C, Knudson R et al. SETBP1 mutations in 415 patients with primary myelofibrosis or chronic myelomonocytic leukemia: independent prognostic impact in CMML. Leukemia 2013; 27: 2100–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasho TL, Jimma T, Finke CM, Patnaik M, Hanson CA, Ketterling RP et al. SRSF2 mutations in primary myelofibrosis: significant clustering with IDH mutations and independent association with inferior overall and leukemia-free survival. Blood 2012; 120: 4168–4171. [DOI] [PubMed] [Google Scholar]
- Patnaik MM, Lasho TL, Finke CM, Hanson CA, Hodnefield JM, Knudson RA et al. Spliceosome mutations involving SRSF2, SF3B1, and U2AF35 in chronic myelomonocytic leukemia: prevalence, clinical correlates, and prognostic relevance. Am J Hematol 2013; 88: 201–206. [DOI] [PubMed] [Google Scholar]
- Patnaik MM, Lasho TL, Hodnefield JM, Knudson RA, Ketterling RP, Garcia-Manero G et al. SF3B1 mutations are prevalent in myelodysplastic syndromes with ring sideroblasts but do not hold independent prognostic value. Blood 2012; 119: 569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Such E, Cervera J, Costa D, Sole F, Vallespi T, Luno E et al. Cytogenetic risk stratification in chronic myelomonocytic leukemia. Haematologica 2011; 96: 375–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 2006; 108: 419–425. [DOI] [PubMed] [Google Scholar]
- Thol F, Kade S, Schlarmann C, Loffeld P, Morgan M, Krauter J et al. Frequency and prognostic impact of mutations in SRSF2, U2AF1, and ZRSR2 in patients with myelodysplastic syndromes. Blood 2012; 119: 3578–3584. [DOI] [PubMed] [Google Scholar]
- Bejar R, Lord A, Stevenson K, Bar-Natan M, Perez-Ladaga A, Zaneveld J et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood 2014; 124: 2705–2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Labopin M, Yakoub-Agha I, Delaunay J, Dhedin N, Deconinck E et al. Allogeneic stem cell transplantation for chronic myelomonocytic leukemia (CMML): A report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire (SFGM-TC). Eur J Haematol 2013; 90: 355–364. [DOI] [PubMed] [Google Scholar]