STRUCTURED ABSTRACT
OBJECTIVE AND SUMMARY BACKGROUND DATA
For pancreatectomy patients, mortality increases with increasing age. Our study evaluated the relative contribution of overall postoperative complications and failure to rescue rates on the observed increased mortality in older patients undergoing pancreatic resection at specialized centers.
METHODS
We identified 2,694 patients who underwent pancreatic resection from the ACS-NSQIP Pancreatectomy Demonstration Project at 37 high volume centers. Overall morbidity and in-hospital mortality were determined in patients <80 (N=2,496) and ≥80 (N=198) years old. Failure to rescue was the number of deaths in patients with complications divided by the total number of patients with postoperative complications.
RESULTS
No significant differences were observed between patients <80 and ≥80 in the rates of overall complications (41.4% vs. 39.4%, p=0.58). In-hospital mortality increased in patients ≥80 compared to patients <80 (3.0% vs. 1.1%, p=0.02). Failure to rescue rates were higher in patients ≥80 (7.7% vs. 2.7%, p=0.01). Across 37 high volume centers, unadjusted complication rates ranged from 25.0%–72.2% and failure to rescue rates ranged from 0.0%–25.0%. Among patients with postoperative complications, comorbidities associated with failure to rescue were ascites, COPD, and diabetes. Complications associated with failure to rescue included acute renal failure, septic shock, and postoperative pulmonary complications.
CONCLUSION
In experienced hands, the rates of complications after pancreatectomy in patients ≥80 compared to patients <80 were similar. However, when complications occurred, older patients were more likely to die. Interventions to identify and aggressively treat complications are necessary to decrease mortality in vulnerable older patients.
Keywords: Failure to rescue, pancreatectomy, complications, mortality
INTRODUCTION
Failure to rescue is defined as the number of patients who die from their postsurgical complications divided by the total number of patients who experience complications.1 Failure to rescue is a measure of a hospital’s ability to recognize and manage postoperative complications.2 In-hospital mortality can be considered a function of both postoperative complications and failure to rescue rates. A retrospective cohort study using the American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) data demonstrated that failure to rescue, after non-emergent general surgery operations increased with increasing age.3 When compared to younger patients, the observed increased mortality in older patients could be due to increased complication rates, increased failure to rescue rates, or a combination of both.
While mortality rates in pancreatectomy have improved over time, the complication rates remain in excess of 30% in most series.4–6 Two recent, large, population based studies demonstrated that advanced age was independently associated with longer lengths of stay and higher mortality rates following pancreatic surgery.7,8 Previous studies have focused solely on mortality following pancreatectomy in older patients7,9–11 or failure to rescue for all patients undergoing pancreatectomy.12 However, for older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of post-surgical complications, higher failure to rescue from these post-surgical complications, or both.
We used data from the ACS-NSQIP Pancreatectomy Demonstration Project to determine the relative contribution of overall postoperative complications and failure to rescue rates on mortality in older patients undergoing pancreatic resection. We hypothesized that older patients undergoing pancreatectomy at high volume centers would experience both higher complication rates and higher failure to rescue rates when compared to younger patients, with both contributing to the observed increase in mortality.
METHODS
As the study involved secondary data analysis of de-identified data, the study was deemed not human subjects research and was designated exempt from review by the Institutional Review Board at the University of Texas Medical Branch.
Data Source
The ACS-NSQIP was established in 2005 to prospectively collect data on 30-day perioperative morbidity and mortality for patients undergoing surgery at participating hospitals. The details of data reporting, acquisition, and reliability have been published previously.13–15 The ACS-NSQIP Pancreatectomy Demonstration Project is a collaborative of 43 institutions that prospectively collected pancreatectomy-specific variables in addition to standard NSQIP variables for patients undergoing pancreatic resection.
Cohort Selection
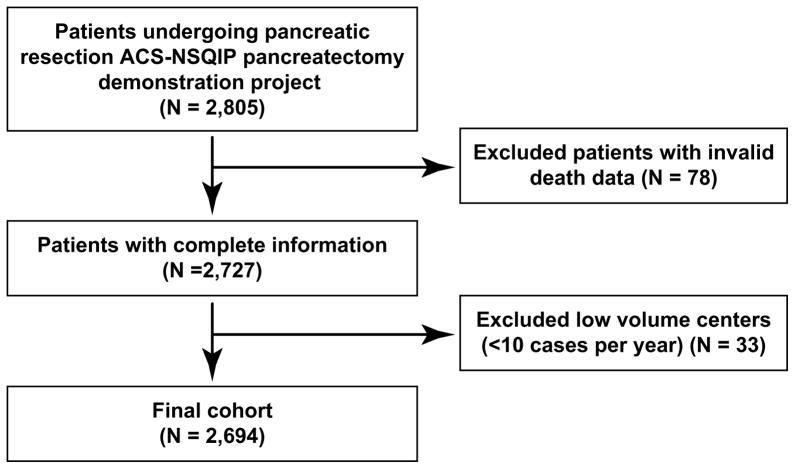
We identified 2,805 patients undergoing pancreatic resection (pancreaticoduodenectomy, distal pancreatectomy, total pancreatectomy, enucleation) from November 2011 through December 2012 at 43 participating institutions. Patients with missing information on 30-day mortality were excluded. We also excluded all institutions with fewer than 10 cases (N=5). One additional institution lacked mortality data and was excluded. Our final cohort consisted of 2,694 patients from 37 high volume centers (Figure 1).
Figure 1.
Cohort Selection. 2,805 patients undergoing pancreatic resection from 2011–2012 were identified. Patients with invalid death data and patients from low volume institutions were excluded. The final cohort included 2,694 patients.
Variables
The Pancreatectomy Demonstration Project includes pancreas-specific variables in addition to the standard 240 Health Insurance Portability and Accountability Act (HIPPA) compliant variables recorded on patient demographics, preoperative risk factors, intraoperative variables, and 30-day postoperative morbidity and mortality in ACS NSQIP. Morbidity and mortality data do not extend beyond the 30 day postoperative period in the NSQIP dataset. This could potentially underestimate the calculated failure to rescue rates if death from complications occurred outside the 30-day observational period. The list and definitions of variables collected in the database can be found at the American College of Surgeons NSQIP website and have been described previously.16,17
Age was analyzed as a categorical variable with groups categorized as either less than 80 years old or equal to/greater than 80 years old.
Outcome
Overall postoperative morbidity was defined as any one or more of the following: delayed gastric emptying, postoperative pancreatic fistula, any surgical site infection (SSI), postoperative sepsis or septic shock, wound disruption, urinary tract infection, acute renal failure, progressive renal insufficiency, postoperative pneumonia, postoperative ventilator dependence, need for cardiopulmonary resuscitation, postoperative myocardial infarction, postoperative coma or stroke, pulmonary embolism, deep venous thrombosis, and reoperation, all within 30 days of operation and as defined within ACS NSQIP.
Serious morbidity was derived from a previous algorithm for pancreatectomy patients15 as any one or more of the following in the absence of preoperative pneumonia, preoperative surgical site infection (SSI), or preoperative ventilator dependence: pancreatic fistula, acute renal failure, organ space surgical site infection, postoperative sepsis or septic shock, wound disruption, reoperation, pulmonary embolism, deep venous thrombosis, need for cardiopulmonary resuscitation, postoperative myocardial infarction, postoperative stroke, and postoperative coma.
In-hospital mortality was defined as occurring in any patient with a discharge destination of “Expired,” as recorded by the Pancreatectomy Demonstration Project. Failure to rescue was defined as the number of patients who experienced in-hospital mortality from these complications divided by the number of patients who experienced complications.
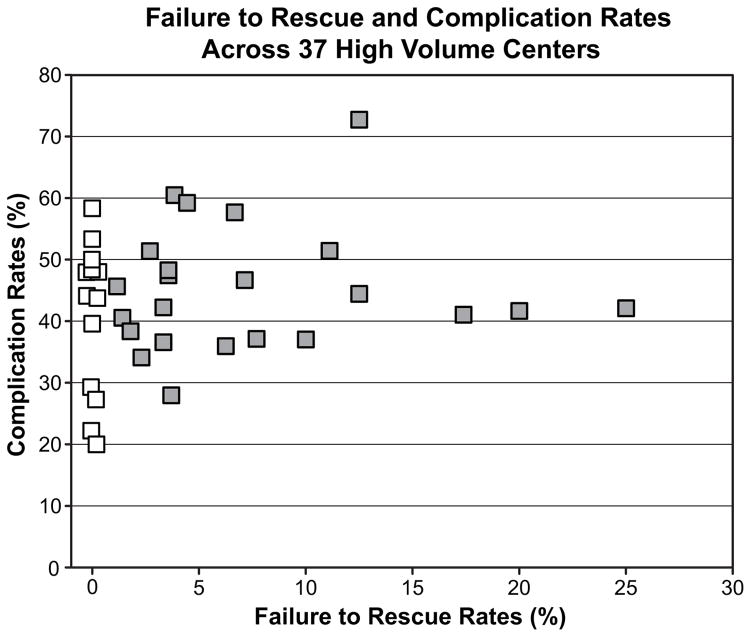
Unadjusted complication rates and failure to rescue rates were calculated across the 37 included participating institutions.
Statistical Analysis
Summary statistics were calculated for the overall cohort. Chi square tests and t-tests were used to test significant differences in patient and treatment characteristics for patients <80 years old and patients ≥ 80 years old. The mortality, complication, and failure to rescue rates were also calculated for each age group. Complication rates and failure to rescue rates were calculated for each of the high volume centers, and are represented graphically in Figure 2. For the patients with complications (N=1,111), chi square tests and t-tests were used to compare the characteristics and complications of patients who failed to rescue to those who did not. Fisher’s exact test was performed where appropriate. For these patients with complications we reported the unadjusted odds ratio and 95% confidence intervals (CI) relative to a chosen reference group. Statistical significance was accepted at the p<0.05 level. All analyses were performed using SAS 9.2 (SAS, Inc., Cary, NC).
Figure 2.
Failure to Rescue Rates and Complication Rates for 37 High Volume Centers. Each data point represents a hospital among the 37 high volume centers. The x axis represents the failure to rescue rate and the y axis represents the complication rate for each hospital. Complication rates ranged from 20.0% to 72.2% and failure to rescue rates ranged from 0.0% to 25.0%. The white data points represent those hospitals with 0.0% failure to rescue rates and the gray data points represent those hospitals with > 0.0% failure to rescue rates.
RESULTS
Our final cohort included 2,694 patients who underwent pancreatic resection at 37 high-volume institutions (median=48 cases per institution, range 11 to 379). Patient characteristics are summarized in Table 1. The mean age for our cohort was 62.3 ± 13.0. The majority of the patients were white (89.1%), male (50.7%), and 67.3% of patients underwent pancreatic head resection (pancreaticoduodenectomy or total pancreatectomy). The diagnosis was adenocarcinoma in 58.9% of patients.
Table 1.
Patient Characteristics of Patients Undergoing Pancreatic Resection in ≥ 80 and < 80 age groups, ACS-NSQIP Pancreatectomy Demonstration Project, 2011–2012 (N=2,694)
| Overall Cohort (%) | Patients ≥ 80 (%) | Patients < 80 (%) | p value* | |
|---|---|---|---|---|
| Patient Characteristics | N=2,694 | N=198 | N=2,496 | |
| Age (Mean, SD) | 62.3 ± 13.0 | 82.9 ± 2.8 | 60.8 ± 12.1 | <0.0001 |
| Sex | 0.84 | |||
| Male | 1366 (50.7%) | 99 (50.0%) | 1267 (50.8%) | |
| Race | 0.03 | |||
| White | 2124 (89.1%) | 180(94.7%) | 2124 (88.7%) | |
| Black | 201 (7.8%) | 7 (3.7%) | 194 (8.1%) | |
| Other | 201 (3.1%) | 3 (1.6%) | 78 (3.3%) | |
| ASA Class | 0.003 | |||
| I | 24 (0.9%) | 1 (0.5%) | 23 (0.9%) | |
| II | 762 (28.5%) | 34 (17.3%) | 728 (29.4%) | |
| III | 1789 (66.9%) | 154 (78.1%) | 1635 (66.0%) | |
| IV | 98 (3.7%) | 8 (4.1%) | 90 (3.6%) | |
| Preoperative Weight Loss | 422 (15.7%) | 37 (18.7%) | 385 (15.4%) | 0.22 |
| BMI | <0.0001 | |||
| Underweight | 59 (2.2%) | 2 (1.0%) | 57 (2.3%) | |
| Normal | 994 (37.0%) | 94 (47.5%) | 900 (36.1%) | |
| Overweight | 917 (34.1%) | 77 (38.9%) | 840 (33.7%) | |
| Obese | 719 (26.7%) | 25 (12.6%) | 694 (27.9%) | |
| Diabetes | 637 (23.7%) | 42 (21.2%) | 595 (23.8%) | 0.40 |
| Smoker | 577 (21.4%) | 4 (2.0%) | 573 (23.0%) | <0.0001 |
| Dyspnea | 213 (7.9%) | 20 (10.1%) | 193 (7.7%) | 0.23 |
| Hypertension | 1380 (51.2%) | 137(69.2%) | 1243 (49.8%) | <0.0001 |
| Obstructive Jaundice | 836 (31.6%) | 75 (38.1%) | 761 (31.0%) | 0.04 |
| Steroid Use | 69 (2.6%) | 6 (3.0%) | 63 (2.5%) | 0.66 |
| COPD | 121 (4.5%) | 7 (3.5%) | 114 (4.6%) | 0.50 |
| Preoperative Biliary Stent | 862 (32.2%) | 65 (33.2%) | 797 (32.1%) | 0.77 |
| Diagnosis | <0.0001 | |||
| Adenocarcinoma | 1586 (58.9%) | 160 (80.8%) | 1426 (57.1%) | |
| Pancreatitis | 401 (14.9%) | 9 (4.5%) | 392 (15.7%) | |
| Neuroendocrine/Carcinoid | 242 (9.0%) | 11 (5.6%) | 231 (9.3%) | |
| Other | 465 (17.2%) | 18 (9.1%) | 447 (17.9%) | |
| Type of Operation | 0.05 | |||
| Pancreaticoduodenectomy | 1720 (64.4%) | 142 (72.5%) | 1578 (63.7%) | |
| Distal Pancreatectomy | 821 (30.7%) | 50 (25.5%) | 771 (31.1%) | |
| Total Pancreatectomy | 80 (3.0%) | 3 (1.5%) | 77 (3.1%) | |
| Enucleation | 52 (2.0%) | 1 (0.5%) | 51 (2.1%) | |
| Laparoscopy (Yes) | 359 (13.4%) | 23 (11.7%) | 336 (13.5%) | 0.47 |
| Intraoperative Drain | 0.09 | |||
| Yes | 2014 (74.8%) | 156 (78.8%) | 1858 (74.4%) | |
| No | 446 (16.6%) | 22 (11.1%) | 424 (17.0%) | |
| Unknown | 234 (8.7%) | 20 (10.1%) | 214 (8.6%) | |
| Vascular Resection (Yes) | 437 (17.9%) | 35 (19.2%) | 402 (17.8%) | 0.63 |
p values represent differences between subgroups for each category
Patient Characteristics Stratified by Age
When compared to patients <80 (N=2,496), patients who were ≥ 80 (N=198) were more likely to be white, non-smokers, have higher ASA class, hypertension, and present with obstructive jaundice (Table 1). While adenocarcinoma was the most common diagnosis in both age groups, pancreatectomy was more commonly performed for pancreatic cancer in the older patients (80.8% vs 57.1%, p=<0.0001). Pancreaticoduodenectomy was more commonly performed in patients ≥80 compared to patients < 80 (72.5% vs 63.7%, p=0.05, Table 1).
Complications and Failure to Rescue Across Participating Hospitals
For the 2,694 patients, the overall mortality rate was 1.3% and the complication rate was 41.2%. Of the 1,111 patients with complications, the overall failure to rescue rate was 3.1%. Across the 37 high-volume hospitals, unadjusted complications ranged from 20.0% to 72.2% (Figure 2). Likewise, failure to rescue rates varied across hospitals, from 0% to 25.0% (Figure 2). Complication rates for each hospital varied across failure to rescue rates. For hospitals with 0.0% failure to rescue rates, complication rates ranged from 20.0% to 58.3% whereas for hospitals with the higher failure to rescue rates, complication rates ranged from 27.9% to 72.2% (Figure 2).
Morbidity, Mortality, and Failure to Rescue by Age Groups (Table 2)
Table 2.
Overall Complications, Major Complications, and Mortality for Patients Undergoing Pancreatic Resection Stratified by Age, ACS-NSQIP Pancreatectomy Demonstration Project, 2011–2012 (N=2,694)
| Overall Rates N=2,694 |
Patients ≥ 80 N=198 |
Patients < 80 N=2,496 |
p value* | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| In hospital Mortality | 34 (1.3%) | 6 (3.0%) | 28 (1.1%) | 0.02 |
| Overall Complications | 1,111 (41.2%) | 78 (39.4%) | 1,033 (41.4%) | 0.58 |
| Major Complicationsa | 768 (28.5%) | 58 (29.3%) | 710 (28.5%) | 0.79 |
| Specific Complications | ||||
| Perioperative Bleeding | 579 (21.5%) | 63 (31.8%) | 516 (20.7%) | 0.0002 |
| SSI | 513 (19.0%) | 35 (17.7%) | 478 (19.2%) | 0.61 |
| Pancreatic Fistula | 402 (14.9%) | 27 (14.3%) | 375 (15.6%) | 0.62 |
| Delayed Gastric Emptying | 344 (12.8%) | 25 (13.4%) | 319 (13.3%) | 0.98 |
| Organ Space SSI | 258 (9.6%) | 24 (12.1%) | 234 (9.4%) | 0.21 |
| Superficial SSI | 226 (8.4%) | 10 (5.1%) | 216 (8.7%) | 0.08 |
| Postoperative Sepsis | 208 (7.7%) | 9 (4.6%) | 199 (8.0%) | 0.08 |
| DVT and Pulmonary Embolism | 110 (4.1%) | 11 (5.6%) | 99 (4.0%) | 0.30 |
| UTI | 103 (3.8%) | 5 (2.5%) | 98 (3.9%) | 0.32 |
| Postoperative Pneumonia | 101 (3.7%) | 11 (5.6%) | 90 (3.6%) | 0.16 |
| Reoperation | 93 (3.5%) | 10 (5.1%) | 83 (3.4%) | 0.20 |
| Septic Shock | 92 (3.4%) | 12 (6.1%) | 80 (3.2%) | 0.03 |
| Unplanned Intubation | 87 (3.2%) | 13 (6.6%) | 74 (3.0%) | 0.006 |
| Ventilator >48 Hours | 80 (2.9%) | 9 (4.6%) | 71 (2.8%) | 0.17 |
| Deep SSI | 56 (2.1%) | 2 (1.0%) | 54 (2.2%) | 0.27 |
| Acute Renal Failure and Renal Insufficiency | 45 (1.7%) | 3 (1.5%) | 42 (1.7%) | 0.86 |
| Wound Disruption | 40 (1.5%) | 4 (2.0%) | 36 (1.4%) | 0.52 |
| MI | 26 (0.9%) | 4 (2.0%) | 22 (0.9%) | 0.11 |
| CPR | 19 (0.7%) | 2 (1.0%) | 17 (0.7%) | 0.59 |
| CVA | 9 (0.3%) | 0 | 9 (0.4%) | 0.40 |
| Failure to Rescue Overall | 34 (3.1%) | 6 (7.7%) | 28 (2.7%) | 0.01 |
Major complications defined as one or more of the following in the absence of preoperative pneumonia, preoperative surgical site infection (SSI), or preoperative ventilator dependence: organ space surgical site infection, postoperative sepsis or septic shock, wound disruption, reoperation, pulmonary embolism, deep venous thrombosis, need for cardiopulmonary resuscitation, postoperative myocardial infarction
p values represent differences between subgroups for each category
The denominator for failure to rescue is the number of patients with postoperative complications
In-hospital mortality rates increased in patients ≥ 80 compared to patients < 80 (3.0% vs. 1.1%, p=0.03). However, across high volume centers, there was no significant difference in the rate of overall complications between patients ≥ 80 years old and < 80 years (41.4% vs. 39.4%, p=0.59). Also, no significant difference existed in the rate of major complications between patients ≥ 80 and < 80 (28.5 % vs. 29.3%, p=0.79). The increased mortality in older patients was attributed to higher failure to rescue rates in patients ≥ 80 compared to patients < 80 (7.7% vs. 2.6%, p=0.01).
Morbidity, Mortality, and Failure to Rescue by Volume (Table 3)
Table 3.
Overall Complications, Major Complications, and Mortality for Patients Undergoing Pancreatic Resection Stratified by Hospital Volume, ACS-NSQIP Pancreatectomy Demonstration Project, 2011–2012 (N=2,694)
| Overall N=2,694 |
High Volume N=2,229 |
Low Volume N=465 |
P Value | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| In hospital Mortality | 34/2,694 (1.3%) | 23/2,229 (1.0%) | 11/465 (2.4%) | 0.02 |
| Overall Complications | 1,111/2,694 (41.2%) | 907/2,229 (40.7%) | 204/465 (43.9%) | 0.21 |
| Major Complications | 768 (28.5%) | 639/2,229 (28.7%) | 129/465 (27.7%) | 0.69 |
| Failure to Rescue | 34 (3.1%) | 23/907 (2.5%) | 11/204 (5.4%) | 0.03 |
The denominator for failure to rescue is the total number of patients with complications
The median number of cases performed across high volume centers was 48 (range 11 to 379). Among the 37 high volume centers, we used a cutoff of 50 cases performed annually to distinguish between higher versus lower volume centers. There were 19 lower volume institutions that performed 465 cases and 18 higher volume institutions that performed 2,229 cases. Compared to lower volume centers, higher volume centers had lower in hospital mortality rates (2.4% vs 1.0%, p=0.02). However, there was no significant difference in complication rates between higher and lower volume centers (43.9% vs 40.7%, p=0.21). The increased mortality in lower volume centers compared to higher volume centers was attributed to higher failure to rescue rates (5.4% vs 2.5%, p=0.03).
Other Factors Associated with Failure to Rescue
In a bivariate analysis, we identified additional factors associated with failure to rescue in the 1,111 patients who experienced complications. Table 4 shows the rates of failure to rescue and unadjusted odds ratios comparing patients with and without specific preoperative comorbidities and postoperative complications. Comorbidities significantly associated with increased failure to rescue rates were ascites, COPD, and diabetes. Complications associated with failure to rescue were acute renal failure, CVA, postoperative cardiopulmonary resuscitation, unplanned intubation, septic shock, progressive renal insufficiency, reoperation, postoperative pneumonia, and postoperative bleeding.
Table 4.
Preoperative Factors and Complications Associated with Failure to Rescue* In Patients Who Experienced Postoperative Complications (N=1,111)
| Preoperative Factors | |||
|---|---|---|---|
| % Failure to Rescue with Factor | % Failure to Rescue without Factor | Odds Ratio (95% CI) | |
| Ascites (N=10) | 40.0% | 2.7% | 23.8 (6.38–88.75) |
| COPD (N=58) | 10.3% | 2.7% | 4.2 (1.68–10.65) |
| Diabetes (N=251) | 5.2% | 2.4% | 2.2 (1.08–4.42) |
| Postoperative Complications | |||
| % Failure to Rescue with Complication | % Failure to Rescue w/out Complication | Odds Ratio (95% CI) | |
| Acute Renal Failure (N=24) | 50.0% | 2.0% | 48.41 (19.59–119.63) |
| CVA (N=9) | 44.4% | 2.7% | 28.6 (7.31–111.82) |
| CPR (N=19) | 36.8% | 2.5% | 23.0 (8.40–63.01) |
| Unplanned intubation (N=87) | 27.6% | 0.9% | 38.6 (7.70–84.29) |
| Septic Shock (N=92) | 23.9% | 1.2% | 26.4 (12.53–55.49) |
| Ventilator >48hrs (N=80) | 21.3% | 1.7% | 16.1 (7.84–33.03) |
| Progressive Renal Insufficiency (N=24) | 16.7% | 2.7% | 7.0 (2.27–21.88) |
| Reoperation (N=93) | 11.8% | 2.2% | 5.9 (2.81–12.79) |
| DVT (N=76) | 10.5% | 2.5% | 4.6 (1.99–10.47) |
| Postoperative Pneumonia (N=101) | 7.9% | 2.6% | 3.3 (1.43–7.39) |
| Postoperative Bleeding (N=298) | 5.0% | 2.3% | 2.2 (1.11–4.42) |
Failure to rescue defined as death from complications divided by the total number of complications
DISCUSSION
We used a multi-institutional, prospectively collected database to identify in-hospital mortality, complications, and failure to rescue rates for patients undergoing pancreatectomy. When stratified by age, older patients had a higher ASA class compared to their younger counterparts, but no significant difference was observed in the overall rate of postoperative complications between these groups. However, older patients still had higher in hospital mortality rates. Our study could implicate higher failure to rescue rates as a potential contributor to the observed increased mortality rates in older patients undergoing pancreatectomy at high volume institutions.
Considerable debate exists in the literature regarding the safety of pancreatectomy in older patients.18,19 In population-based studies of patients undergoing pancreatectomy, advancing age was identified among others as an independent predictor of increased perioperative mortality.7,20 To explain the observed increased mortality in older patients undergoing major surgery, several studies have evaluated the impact of postoperative complications on patient survival.6,20,21 A population based study by Finlayson et al. demonstrated higher complication rates in older patients undergoing pancreatic resection for cancer.8 Likewise, in a retrospective cohort study by Haigh et al. using NSQIP data, age > 70 years was found to be an independent prognostic factor for increased postoperative complications following pancreaticoduodenectomy.4 A prospective multicenter study using the NSQIP database demonstrated that 30-day postoperative complications were the most important determinant of survival in patients undergoing major general surgery operations.21 In contrast, our study, which included only patients operated on at high volume centers, found no difference in overall complication rates between patients ≥80 and <80 (41.4% vs. 39.4%, p=0.58). This finding suggests that at high volume centers both careful patient selection and improved operative technique related to surgeon experience led to fewer complications in older patients.
A volume-outcome relationship in pancreatic surgery is well established.22–24 In evaluating high volume centers only, our findings have significant implications regarding postoperative management of complications. Previous studies have demonstrated improved postoperative outcomes for high volume compared to low volume centers.12 A population based study from Texas evaluated outcomes for pancreatectomy patients at high volume centers only and identified significant variability in mortality, length of stay, and total hospital charges.25 In our study, complication rates and failure to rescue rates varied widely. We found that even across high-volume centers, the very high volume centers (>50 cases per year) had lower mortality rates but similar complications rates compared to lower volume centers. At lower volume centers, the observed increased mortality rates were attributed to higher failure rescue rates.
These data suggest that identification of preoperative risk factors early recognition and timely management of complications strongly associated with failure to rescue, especially in older patients, could decrease mortality rates for patients undergoing pancreatectomy in high volume centers. The inciting events that lead to failure to rescue likely originate in complications such as pancreatic fistula. Cardiopulmonary resuscitation, acute renal failure, and reintubation are often downstream events of such complications. While the NSQIP data describes the presence or absence of abscess, infection, fistula, and other complications, the temporal relations of these complications are unknown. Given that these are downstream complications, our data suggest that early and aggressive management can prevent the cascade of complications leading to cardiopulmonary resuscitation, acute renal failure, and reintubation.
In a study using a nationwide database, Ghaferi et al identified teaching hospitals, high volume centers, increased nurse to patient ratios, and increased hospital technology as hospital characteristics significantly associated with lower failure to rescue rates following pancreatectomy for all patients.12 In a qualitative study by Johnston et al., escalation of care was identified as the common initial factor in the recognition and management of the deteriorating patient. Barriers to escalating care in patients with complications were lack of an established protocol and lack of support from senior team members.26 In an effort to improve failure to rescue rates, Johnston et al created a guide for the development of technology-based communication interventions to address issues with barriers to escalation of care.27 In various institutions, the increase in failure to rescue rates for elderly patients may also be explained by unmeasured factors such as resource and provider factors that impact the recognition and management of complications. In addition, clarifying physician, patient, and caregiver goals of care by qualitative techniques can provide insight into differences in management of complications within the aging population.
Several limitations are inherent to this study. As with all observational data sets, it is difficult to assess whether the population included in the study is a truly representative sample for most patients undergoing pancreatectomy. During the ACS-NSQIP pancreatectomy demonstration project, there was a learning curve for the pancreas specific variables. This learning curve could have lead to inaccuracy in capturing complications. Any hospital participating in ACS-NSQIP employs Surgical Clinical Reviewers (SCRs) who are trained through a standardized process to systematically abstract clinical data at an institutional level throughout the 30-day postoperative period. All pancreatectomy specific variables were clearly defined and collected by trained ACS-NSQIP SCRs. All SCRs were trained in the new variable collection and support was available for questions during the demonstration project. As such, we expect reasonable accuracy of the collected data. The ACS-NSQIP data collection process has been shown to have high inter-rater reliability and high accuracy in capturing complications.28–30 In addition, all patients in our study underwent surgery at high volume institutions defined by Leapfrog criteria as > 10 cases per year. In hospitals only performing 10 or 20 cases during the period of the demonstration project, one or two complications could lead to large changes in the percentage of complications. Overtime, as more data are collected, we expect regression some regression to the mean. Across these high volume institutions, some hospitals contributed a much smaller number of cases when compared to others between 2011 and 2012. A larger sample size from such institutions could yield large differences in outcomes. In this study, the number of patients undergoing pancreatectomy who were 80 years or older is a small subset of the population (N=198) and this study is likely underpowered to detect significant factors associated with failure to rescue between age groups. Older patients had more comorbid illness and were more likely to undergo higher-risk pancreatic resections, including pancreaticoduodenectomy and total pancreatectomy, than younger patients. In addition, assessment of patient motivation for treatment choices which can result in a selection bias is difficult. Patients ≥80 could have had a DNR status precluding escalation of care in the event of a serious complication. These individual characteristics are not captured in this observational data set. However, for those patients who agreed to undergo pancreatectomy and are included in the data set, it is assumed that by signing consent, patients agreed to pursue surgical intervention with a clear understanding of the potential complications. In addition, unmeasured intraoperative variables such as the difficulty of the operation may not have been captured. Our study identifies preoperative comorbidities and postoperative complications associated with failure to rescue, the incidence of many of these were low, with resulting large confidence intervals around our unadjusted estimates. While postoperative complications can occur within 30 days, for pancreatectomy patients, the risk of mortality extends beyond 30 days and death from these complications can occur much later. In a study using SEER-Medicare data to evaluate mortality after pancreatic resection, in hospital and 30-day mortality were similar, but mortality increased significantly within 60 days post resection.31 Given that NSQIP data only includes 30-day postoperative morbidity and mortality data, the failure to rescue from postoperative complications could potentially be underestimated in this study.
It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy. Complication rates are also included in the failure to rescue pathway. Therefore, complications can be addressed before they occur (avoiding complications) or once they occur by addressing those complications that are associated with higher rates of failure to rescue. Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy.
We used a multi-institutional database to identify the relative contributions of failure to rescue and complications on the observed increased mortality rates for older patients undergoing pancreatic resection. We found that patients 80 years of age and older had no difference in complication rates but higher failure to rescue rates compared to patients less than 80 years old. Especially with regards to the variation in failure to rescue rates even at high-volume hospitals, earlier recognition and more effective management of postoperative complications is key to improving outcomes. Protocols to escalate care based on timely recognition and treatment of the complications strongly associated with failure to rescue can improve outcomes in older patients undergoing pancreatectomy.
Acknowledgments
Funding: Cancer Prevention Research Institute of Texas Grant # # RP140020, UTMB Clinical and Translational Science Award #UL1TR000071, NIH T-32 Grant # T32DK007639, AHRQ Grant # 1R24HS022134.
This study would not have been possible without the collaboration of the following institutions: Albany Medical Center, Baptist Memorial Healthcare – Memphis, Baylor University Hospital, Baystate Medical Center, Beth Israel Deaconess Medical Center, Boston Medical Center, Brigham & Women’s Hospital, California Pacific Medical Center, Cleveland Clinic Hospital, Emory University Hospital, Hospital of the University of Pennsylvania, Indiana University Health - Methodist Hospital, Indiana University Health - University Hospital, Intermountain Medical Center, Johns Hopkins Hospital, Kaiser Permanente - San Francisco, Kaiser Permanente – Walnut Creek, Lehigh Valley Hospital, Massachusetts General Hospital, Mayo Clinic – Methodist Hospital, Mayo Clinic - St. Mary’s Hospital, Northwestern University Hospital, Oregon Health and Science University, Penn State Milton S. Hershey Medical Center, Providence Portland Medical Center, Sacred Heart Medical Center, Stanford Hospital and Clinics, Tampa General Hospital, The Ohio State University Medical Center, Thomas Jefferson University Hospital, University of Alabama Medical Center, University of California Irvine, University of California San Diego Medical Center, University of Iowa Hospital and Clinics, University of Kentucky Chandler Medical Center, University of Texas Medical Branch, University of Virginia Medical Center University of Wisconsin Hospital and Clinics, Vanderbilt University Medical Center, Wake Forest University Baptist Medical Center, Washington University/Barnes Jewish Hospital, and Winthrop University.
Footnotes
Author Disclosures: Bruce L. Hall is a paid consulting director of the ACS NSQIP
References
- 1.Silber JH, Williams SV, Krakauer H, et al. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care. 1992;30:615–629. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Needleman J, Buerhaus PI, Vanderboom C, et al. Using present-on-admission coding to improve exclusion rules for quality metrics: the case of failure-to-rescue. Med Care. 2013;51:722–730. doi: 10.1097/MLR.0b013e31829808de. [DOI] [PubMed] [Google Scholar]
- 3.Gajdos C, Kile D, Hawn MT, et al. Advancing age and 30-day adverse outcomes after nonemergent general surgeries. J Am Geriatr Soc. 2013;61:1608–1614. doi: 10.1111/jgs.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haigh PI, Bilimoria KY, DiFronzo LA. Early postoperative outcomes after pancreaticoduodenectomy in the elderly. Arch Surg. 2011;146:715–723. doi: 10.1001/archsurg.2011.115. [DOI] [PubMed] [Google Scholar]
- 5.Simons JP, Shah SA, Ng SC, et al. National complication rates after pancreatectomy: beyond mere mortality. J Gastrointest Surg. 2009;13:1798–1805. doi: 10.1007/s11605-009-0936-1. [DOI] [PubMed] [Google Scholar]
- 6.Spanheimer PM, Cyr AR, Liao J, et al. Complications and survival associated with operative procedures in patients with unresectable pancreatic head adenocarcinoma. J Surg Oncol. 2014;109:697–701. doi: 10.1002/jso.23560. [DOI] [PubMed] [Google Scholar]
- 7.Riall TS, Reddy DM, Nealon WH, et al. The effect of age on short-term outcomes after pancreatic resection: a population-based study. Ann Surg. 2008;248:459–467. doi: 10.1097/SLA.0b013e318185e1b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007;205:729–734. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 9.Makary MA, Winter JM, Cameron JL, et al. Pancreaticoduodenectomy in the very elderly. J Gastrointest Surg. 2006;10:347–356. doi: 10.1016/j.gassur.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Tani M, Kawai M, Hirono S, et al. A pancreaticoduodenectomy is acceptable for periampullary tumors in the elderly, even in patients over 80 years of age. J Hepatobiliary Pancreat Surg. 2009;16:675–680. doi: 10.1007/s00534-009-0106-6. [DOI] [PubMed] [Google Scholar]
- 11.McPhee JT, Hill JS, Whalen GF, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246:246–253. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghaferi AA, Osborne NH, Birkmeyer JD, et al. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–330. doi: 10.1016/j.jamcollsurg.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 13.American College of Surgeons-National Surgical Quality Improvement Program. [Accessed January, 2013];ACSNSQIP Key Studies Fact Sheet. web site. 2013 Available at: http://site.acsnsqip.org/downloads/
- 14.Pitt HA, Kilbane M, Strasberg SM, et al. ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB (Oxford) 2009;11:405–413. doi: 10.1111/j.1477-2574.2009.00074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parikh P, Shiloach M, Cohen ME, et al. Pancreatectomy risk calculator: an ACS-NSQIP resource. HPB (Oxford) 2010;12:488–497. doi: 10.1111/j.1477-2574.2010.00216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parmar AD, Sheffield KM, Vargas GM, et al. Factors associated with delayed gastric emptying after pancreaticoduodenectomy. HPB (Oxford) 2013;15:763–772. doi: 10.1111/hpb.12129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. [Accessed January, 2013]; http://site.acsnsqip.org/wp-content/uploads/2012/03/ACS-NSQIP-Participant-User-Data-File-User-Guide_06.pdf. UGftPUDFACoSNSQIPwsSAa.
- 18.Kow AW, Sadayan NA, Ernest A, et al. Is pancreaticoduodenectomy justified in elderly patients? Surgeon. 2012;10:128–136. doi: 10.1016/j.surge.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Sulpice L, Rayar M, D’Halluin PN, et al. Impact of age over 75 years on outcomes after pancreaticoduodenectomy. J Surg Res. 2012;178:181–187. doi: 10.1016/j.jss.2012.03.075. [DOI] [PubMed] [Google Scholar]
- 20.Teh SH, Diggs BS, Deveney CW, et al. Patient and hospital characteristics on the variance of perioperative outcomes for pancreatic resection in the United States: a plea for outcome-based and not volume-based referral guidelines. Arch Surg. 2009;144:713–721. doi: 10.1001/archsurg.2009.67. [DOI] [PubMed] [Google Scholar]
- 21.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–341. doi: 10.1097/01.sla.0000179621.33268.83. discussion 341–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eppsteiner RW, Csikesz NG, McPhee JT, et al. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009;249:635–640. doi: 10.1097/SLA.0b013e31819ed958. [DOI] [PubMed] [Google Scholar]
- 23.Nathan H, Cameron JL, Choti MA, et al. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg. 2009;208:528–538. doi: 10.1016/j.jamcollsurg.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Pecorelli N, Balzano G, Capretti G, et al. Effect of surgeon volume on outcome following pancreaticoduodenectomy in a high-volume hospital. J Gastrointest Surg. 2012;16:518–523. doi: 10.1007/s11605-011-1777-2. [DOI] [PubMed] [Google Scholar]
- 25.Riall T, Nealon W, Goodwin J, et al. Outcomes following pancreatic resection: variability among high volume providers. Surgery. 2008;144:133–140. doi: 10.1016/j.surg.2008.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnston M, Arora S, King D, et al. Escalation of care and failure to rescue: A multicenter, multiprofessional qualitative study. Surgery. 2014 doi: 10.1016/j.surg.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 27.Johnston MJ, King D, Arora S, et al. Requirements of a new communication technology for handover and the escalation of patient care: a multi-stakeholder analysis. J Eval Clin Pract. 2014 doi: 10.1111/jep.12186. [DOI] [PubMed] [Google Scholar]
- 28.Shiloach M, Frencher SK, Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210:6–16. doi: 10.1016/j.jamcollsurg.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 29.Lawson EH, Louie R, Zingmond DS, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg. 2012;256:973–981. doi: 10.1097/SLA.0b013e31826b4c4f. [DOI] [PubMed] [Google Scholar]
- 30.Cima RR, Lackore KA, Nehring SA, et al. How best to measure surgical quality? Comparison of the Agency for Healthcare Research and Quality Patient Safety Indicators (AHRQ-PSI) and the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) postoperative adverse events at a single institution. Surgery. 2011;150:943–949. doi: 10.1016/j.surg.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 31.Carroll JE, Smith JK, Simons JP, et al. Redefining mortality after pancreatic cancer resection. J Gastrointest Surg. 2010;14:1701–1708. doi: 10.1007/s11605-010-1326-4. [DOI] [PubMed] [Google Scholar]