Abstract
Background:
When performing follicular unit extraction (FUE), various types of minor hair follicle trauma unapparent during follicular unit strip surgery are likely to occur. However, no studies have examined such damage.
Methods:
In total, 100 grafts were randomly selected from each of 42 patients who underwent FUE with a 1-mm-diameter sharp punch. A ×5.5 magnifying loupe and a ×60 magnifying binocular microscope were used. The transection rate (TR), paring, fractures of and damage to the dermal papilla (DP) areas, and hair bulb partial injury were assessed.
Results:
Observation with the magnifying loupe revealed an average TR of 7.40%, and 4.31, 1.90, 1.52, and 0.43 hair follicles per 100 grafts exhibited paring, fracture, DP partial injury, and hair bulb partial injury, respectively. An average of 9.21 telogen hairs were observed. Microscopic examination revealed a TR of 6.34%, and 9.07, 1.95, 0.79, and 1.24 hair follicles per 100 grafts exhibited paring, fracture, DP injury, and hair bulb partial injury, respectively. An average of 16.62 telogen hairs were observed.
Conclusions:
Various types of minor hair follicle damage occur during FUE as shown by loupe and microscopic examination of the grafts. Especially paring and hair bulb injury were more apparent under microscopic examination. These minor hair follicle injuries should be considered when choosing operative method or surgical techniques.
INTRODUCTION
Since its first introduction in 2002, follicular unit extraction (FUE) has become an increasingly more popular method of obtaining donor hair.1
Despite the various advantages and disadvantages of FUE, it is likely that more patients choose to undergo hair transplantation by FUE than follicular unit strip surgery (FUSS) because less pain and scarring is associated with FUE. Nevertheless, the efficacy of FUE has been questioned with respect to whether its outcomes are equivalent to those of FUSS, the most commonly employed procedure by many hair surgeons.
Some expert hair surgeons have simultaneously performed FUSS and FUE in the same patient. Long-term comparisons of the 2 methods have revealed much lower follicle survival rates in FUE than FUSS (53.9% versus 85.2%, respectively).2 FUE-harvested grafts contain less perifollicular tissue than do FUSS-harvested grafts, and many physicians evidently believe this to be the main cause of the lower survival rate of harvested follicles in FUE than FUSS. Nonetheless, the same expert surgeons have found that there is a tendency toward a larger deviation of surgical outcomes of FUE than FUSS. In cases in which the same surgeon consistently harvested the follicles by the same method, both excellent and poor results were observed. This raises 2 important clinical questions: What characteristics of FUE-obtained grafts, other than the smaller amount of perifollicular tissue compared with FUSS-obtained grafts, contribute to this variation in outcomes? How does the appearance of FUE- and FUSS-obtained grafts differ under a microscopic and high-magnification loupe?
Microscopic dissection is generally chosen for FUSS. However, although an approximately ×5 magnifying loupe is recommended for FUE, some surgeons perform this procedure with the naked eye or by wearing a simple ×1.5 or ×2.0 magnifying glass. The grafts harvested in this way might then be inspected by the naked eye, a ×1.5 to ×2.0 magnifying glass, and a ×5 magnifying loupe to confirm whether they are intact or properly transected.
Until now, we have only considered either the occurrence of transection or the presence of intact grafts to assess the quality of follicles harvested by either FUE or FUSS. We believe that the transection rate (TR) provides valuable information about the quality of FUE surgery. However, in addition to simple transection, the occurrence of other types of minor trauma to the follicles harvested by FUE is probable, and these types of trauma are rarely seen in FUSS.
FUSS lacks various potentially traumatic processes such as dissection using a rotating or oscillating punch and extraction using aid-to-extraction forceps or jeweler’s forceps. Hence, in the present study, we aimed to identify other types of hair follicle injuries that can occur in addition to transection.
To the best of our knowledge, no reports have addressed the nature and extent of these types of minor hair follicle trauma. Therefore, we conducted the present study to determine the frequency and nature of minor trauma that occurs during FUE surgery.
MATERIALS AND METHODS
This study included 42 patients (38 males and 4 females) at the authors’ clinic. Using a 1-mm-diameter sharp punch, 100 follicles were randomly selected from each patient. In total, 4200 grafts were analyzed.
Patients with a history of hair transplant surgery, infectious disease, or trauma in the donor area were excluded from the study. The patients’ age distribution ranged from 28 to 52 years, and the mean age was 32.6 years. All male patients exhibited Norwood stage 3 to 5 male pattern baldness. All female patients were undergoing female hairline correction without female pattern hair loss. The donor area of all patients was shaved in the form of a total or partial patch for FUE. This study was approved by the internal institutional review board of the Korea National Institute of Bioethics Policy.
FUE Procedure
All punching was performed by 1 expert hair surgeon (Dr. Park). A 1-mm sharp punch of the Folligraft system (LeadM Corp., Seoul, Korea) was used. The surgical procedure was implemented in the same manner as routinely performed during a normal FUE operation. A FOX test was conducted at the beginning and in the middle of the surgery, while the punching depth was modified. The punching depth achieved was within 2.5 to 3.5 mm (mean, 2.9 mm).
All injuries were divided into 5 types: transection, paring, fracture, dermal papilla (DP) injury, and hair bulb partial injury. The presence or absence of such injuries was confirmed in all patients. A ×5.5 magnifying loupe and ×60 magnifying binocular microscope were employed for analysis. If none of the above-described 5 types of injury was present, the hair follicle was considered intact.
Statistical Analysis
An independent-samples t test was conducted to determine the differences in the types of partial injuries in all patients.
RESULTS
The TR was 7.40% based on microscopic observation and 6.34% based on loupe observation. The difference in these rates was not significantly different (P > 0.05). However, the 2 observation methods showed significantly different numbers of telogen hairs: an average of 9.21 follicles based on loupe observation and an average of 16.62 follicles based on microscopic observation (P < 0.001; Table 1).
Table 1.
Comparative Analysis of FUE-extracted Grafts Using a Loupe and Microscope
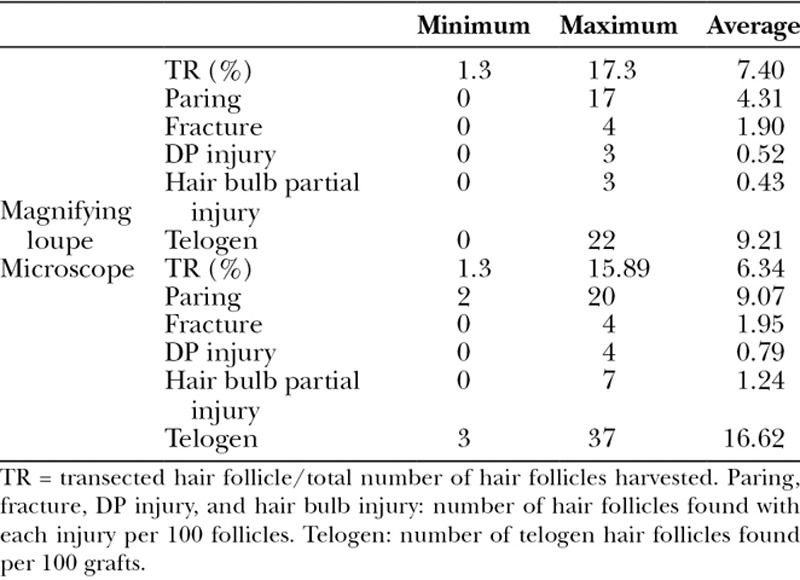
Paring was present in approximately 4.31 follicles based on loupe observation and 9.07 follicles based on microscopic observation; microscopic observation showed a 2-fold higher number of affected follicles, and the difference was statistically significant (P < 0.000).
DP partial injury affected an average of 0.52 follicles based on loupe observation and 0.79 follicles based on microscopic observation with no significant difference (P > 0.243).
Bulb injury affected an average of 0.43 and 1.24 follicles based on loupe and microscopic observation, respectively, with a significant difference (P < 0.003).
Finally, an average of 1.90 follicles were fractured based on loupe observation and an average of 1.95 follicles were fractured based on microscopic observation, with no significant difference between the 2 methods (P > 0.858).
Trauma was more frequently found in association with all types of damage under microscopic examination. However, a statistically significant difference appeared only for paring and bulb injury (Fig. 1).
Fig. 1.
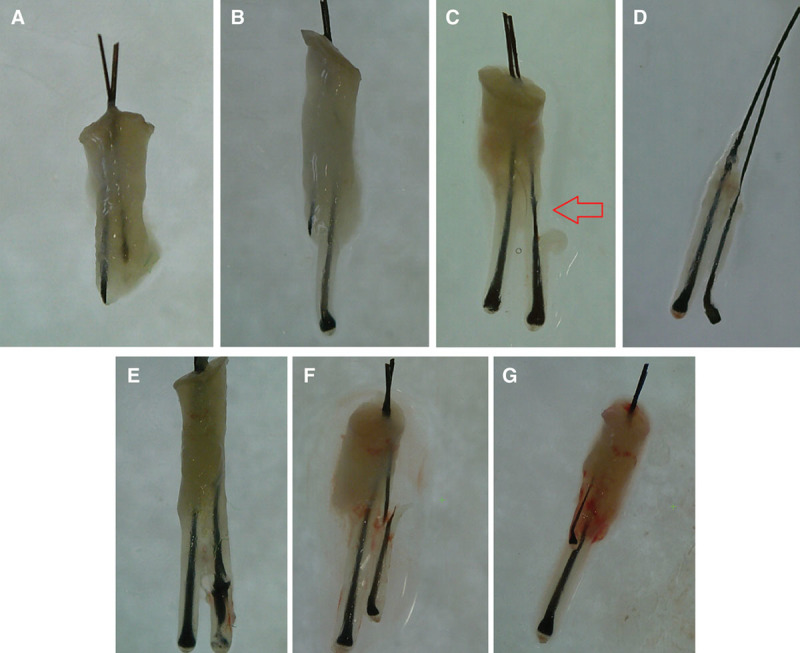
Various types of follicle injury that are likely to occur during FUE (×60 magnification). A, Total transection. B, Partial transection. C, Paring. D, DP injury. E, Bulb injury. F, Fracture. G, Telogen.
DISCUSSION
Generally, patients prefer FUE to FUSS for obtaining donor hair, although the follicle survival rate remains controversial because of less postoperative pain and to avoid linear donor scar.3
Despite the fact that FUSS can have phenomenal results with respect to minimal scarring when the trichophytic closure strategy is used, this is a benefit generally seen from the doctor’s point of view and may differ from the patient’s perspective. From the patient’s point of view, FUE is a more minimally invasive and patient-friendly method.4,5
Regardless, successful and consistent results of FUE are still being demanded. The type of surgery that would be considered a successful FUE surgery remains unclear. When comparing FUE with FUSS, the TR and calculated density are often compared, and the TR is often examined by itself.5–7 The TR is undoubtedly a very important factor that must be considered during surgery, but a lower TR in association with a high follicle survival rate is also an imperative factor to be considered. Fewer studies have evaluated the follicle survival rate in FUE. Beehner8 performed FUE and FUSS simultaneously in the same patient and reported an 85.2% follicle survival rate in FUSS and a 53.9% follicle survival rate in FUE.
Many researchers and hair surgeons believe that the reason for the difference in the survival rate between FUE and FUSS is the difference in the amount of perifollicular tissue between the 2 types of grafts. A thicker graft is associated with a higher follicle survival rate; this fact is recognized as the most basic concept of hair transplantation. Many other factors may also affect the follicle survival rate, such as the out-of-body time, dryness, physical trauma, and surgeon’s implantation skills.9
In the present study, no paring, fracture, DP injury, or bulb damage was observed while affirming the randomly selected follicles under a microscope; all of these follicles were arbitrarily acquired by FUSS and analyzed as a follicular unit by a highly experienced surgical assistant.
How specifically and practically hair follicle trauma affects the survival rate remains unknown. However, based on our literature review, it is possible to infer that the minor trauma described in this report has more negative effects on hair follicles than intact and perfectly conditioned grafts with no minor trauma.
Hair follicle stem cells are not a single multipotent entity given that a pilosebaceous unit contains numerous stem cell populations and subpopulations ranging from epithelial to mesenchymal and melanocyte stem cells. The epithelium comprises the hair shaft, inner root sheath, and outer root sheath (ORS). The isthmus is the region between the entry of the sebaceous duct and the insertion of the arrector pili muscle. The isthmus includes the “bulge” region (otherwise known as the basal, outermost ORS layer of the distal hair follicle epithelium at the proximal end of the isthmus), which contains the epithelial hair follicle stem cells. The DP and dermal sheath of the follicle are mesenchymal in origin and have been shown to harbor multipotent stem cell subpopulations distinct from epithelial hair follicle stem cells, such as skin-derived precursors, NESTIN+ cells, or SOX2+ cells.10–12
Hair follicle morphogenesis and regeneration depend on intensive but well-orchestrated interactions between epithelial (bulge stem cells, their descendent secondary hair germ cells, and hair matrix cells) and mesenchymal (DP and dermal sheath) components.10–13 Thus, both DP stem cells and epithelial stem cells are important, and hair growth is reportedly degraded if either is missing.
Each type of trauma described in this study is shown in detail in Figure 1. First and foremost is transection, which can occur not only during the strip incision process of FUSS but also during dissection in FUE. The transected donor hair follicle obtained by FUE remains in the donor scalp tissue; in FUSS, however, it completely dissipates.
The second type of injury is paring. Paring refers to laceration or avulsion of the ORS by the punch tip (Fig. 2).14
Fig. 2.
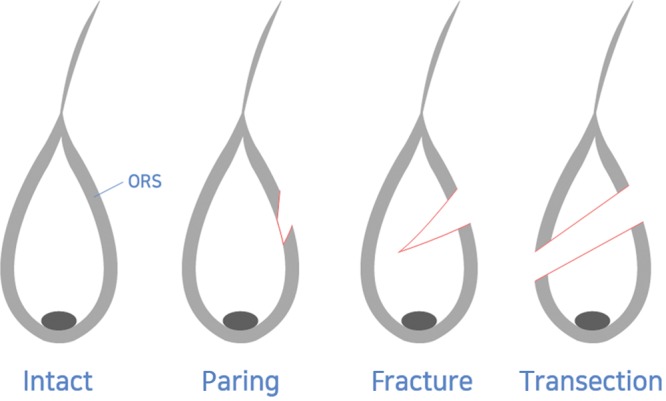
Concept schema for easy understanding of paring, fracture, and transection.
The third injury is fracture. A fracture is defined as separation of either end of the hair follicle into 2 or more pieces due to stress at some point along the length of the follicle.14 The cause of a fracture is rotation of the punch tip, which partially traumatizes the hair follicle like a laceration, resulting in injury to the ORS and the hair shaft on one side; the ORS and partial hair shaft on the other side remain intact, maintaining the overall continuity of the follicle (Fig. 2). Theoretically, fractures occur more frequently under circumstances of increased axial force such as rubbery skin; long, thick hair follicles; hyperelastic skin; and use of a blunt punch tip.15
The fourth type of trauma is DP injury. This occurs due to an insufficient punching depth when considering the adhesion between the perifollicular tissue and the hair follicle. When the depth is too superficial for extraction, the tissues of the ORS encompassing the hair bulb and DP can likewise be detached or torn out. Therefore, from a clinical perspective, when conducting the extraction, the surrounding scalp tissues can be elevated by tagging along the graft, which can suddenly break off later, resulting in frequent DP injuries. If the punch tip enters even deeper than the minimal punching depth, it can reach a segment where extraction of the hair follicles can be conducted in a smoother, easier manner without having to increase the TR. The authors refer to this as the safe punching depth.
The fifth type of trauma is bulb partial damage. This is another very important factor that may be overlooked. A partially damaged hair follicle will be considered intact if it does not contribute to the TR, which we have recognized. However, it is highly likely to affect the survival rate. An important fact that matters in the present study is that such types of damage to the hair bulb frequently occur in many cases and that they can usually be visualized only under a ×60 magnifying microscope and not through a ×5 to ×6 magnifying loupe, which is routinely used during FUE. Trauma to the hair bulb such as damage, crushing, or partial avulsion are thought to profoundly affect the survival of hair follicles. From a comprehensive viewpoint, not only are a too superficial punching depth and inadequate extraction undesirable, but a too deep punching depth should be avoided as well.
The main limitation of this study is that transection and other types of minor trauma were dependent upon the operators’ skill levels and variations in techniques. We consider that a further study is required to gain a better understanding of the effects of various types of trauma on the survival rate of damaged follicles. We also believe that an additional study should be conducted to determine how these types of trauma vary depending on various FUE techniques and skin and hair characteristics.
This study confirms the existence of diverse types of damage to hair follicles obtained through FUE. Such graft damage was less often detected by a ×5 to ×6 magnifying loupe, which is routinely used during FUE, than with a ×60 microscope. The present study will serve as a baseline for additional studies on this topic, enabling researchers to discover better surgical techniques that ensure satisfactory results for both the doctor and the patient.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Rassman WR, Bernstein RM, McClellan R, et al. Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28:720–728.. [DOI] [PubMed] [Google Scholar]
- 2.Beehner M. A comparative study of FUE and FUT survival in four patients. 2015Chicago, 23rd Annual Scientific Meeting, ISHRS. [Google Scholar]
- 3.Harris JA. Follicular unit extraction. Facial Plast Surg Clin North Am. 2013;21:375–384.. [DOI] [PubMed] [Google Scholar]
- 4.Dua A, Dua K. Follicular unit extraction hair transplant. J Cutan Aesthet Surg. 2010;3:76–81.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ors S, Ozkose M, Ors S. Follicular unit extraction hair transplantation with micromotor: eight years experience. Aesthetic Plast Surg. 2015;39:589–596.. [DOI] [PubMed] [Google Scholar]
- 6.Shin JW, Kwon SH, Kim SA, et al. Characteristics of robotically harvested hair follicles in Koreans. J Am Acad Dermatol. 2015;72:146–150.. [DOI] [PubMed] [Google Scholar]
- 7.Cole J. Status of individual follicular group harvesting. Hair Tranplant Forum Int’l. 2009;19:20–24.. [Google Scholar]
- 8.Beehner M. MFU grafts and strip harvesting – we hardly know yet. Hair Transplant Forum Int’l. 2014;24:125–126.. [Google Scholar]
- 9.Parsley WM, Perez-Meza D. Review of factors affecting the growth and survival of follicular grafts. J Cutan Aesthet Surg. 2010;3:69–75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohyama M, Veraitch O. Strategies to enhance epithelial-mesenchymal interactions for human hair follicle bioengineering. J Dermatol Sci. 2013;70:78–87.. [DOI] [PubMed] [Google Scholar]
- 11.Ohyama M, Zheng Y, Paus R, et al. The mesenchymal component of hair follicle neogenesis: background, methods and molecular characterization. Exp Dermatol. 2010;19:89–99.. [DOI] [PubMed] [Google Scholar]
- 12.Commo S, Gaillard O, Bernard BA. The human hair follicle contains two distinct K19 positive compartments in the outer root sheath: a unifying hypothesis for stem cell reservoir? Differentiation. 2000;66:157–164.. [DOI] [PubMed] [Google Scholar]
- 13.Yang CC, Cotsarelis G. Review of hair follicle dermal cells. J Dermatol Sci. 2010;57:2–11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lorenzo J, Devorye JM, True RH, et al. Standardization of the terminology used in FUE: part I. Hair Transplant Forum Int’l. 2013;23:165–168.. [Google Scholar]
- 15.Cole JP. An analysis of follicular punches, mechanics, and dynamics in follicular unit extraction. Facial Plast Surg Clin North Am. 2013;21:437–447.. [DOI] [PubMed] [Google Scholar]


