Case Report
A 55-year-old woman presented with recurrent abdominal pain, a lump in her abdomen, and vomiting. In the previous 10 years, she required multiple hospital admissions for pain. Examination revealed pallor and a lump (20 cm × 15 cm) extending from left hypochondrium to left iliac region. Labs showed hemoglobin 7.8 g/dL, platelet count 5,100 cells/mm3, and serum protein/albumin 6.7/3.4 g/dL; the rest of her blood parameters were normal. Ultrasound showed heterogeneous liver echo-texture, ascites, and massive splenomegaly. Esophagoduodenoscopy showed grade 2 esophageal varices. Ascetic fluid examination showed high serum ascites albumin gradient (SAAG). Etiological evaluation for chronic liver disease (CLD) was negative. Computed tomography (CT) showed a homogeneously enhanced, massively enlarged spleen in the left lower abdomen. The vascular pedicle was long, stretched, and appeared coiled (whirl sign), suggestive of torsion (Figure 1). Features of CLD with portal hypertension (PHT) were seen, including diffuse atrophy of liver parenchyma, dilated portal vein, prominent perigastric collaterals, and ascites. The patient showed symptomatic improvement with conservative treatment.
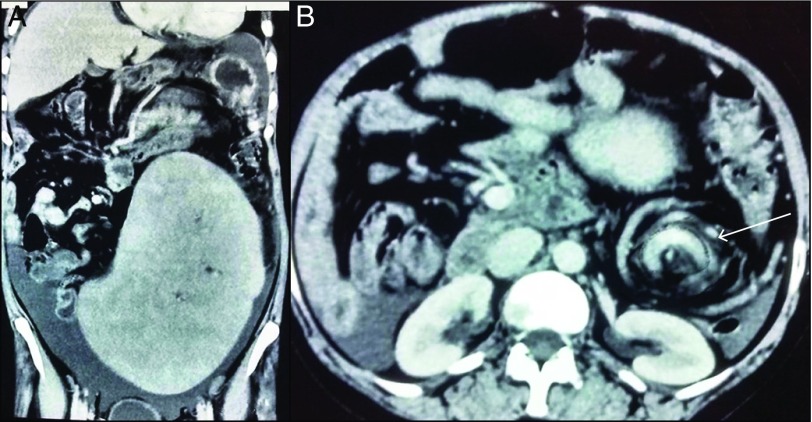
Figure 1.
CT scan showing (A) a homogeneously enhanced, massively enlarged spleen located in the left lower abdomen, and diffuse atrophy of liver parenchyma and ascites; and (B) a coiled splenic vascular pedicle (whirl sign), suggestive of torsion (arrow).
Wandering spleen is a rare clinical entity in which the spleen is attached by a long vascular pedicle. Wandering spleen is mainly caused by either laxity or absence of splenorenal and gastrosplenic ligaments (congenital or acquired). Acquired risk factors include pregnancy, abdominal wall laxity, multiparity, and splenomegaly.1 Wandering spleen is usually detected in the third or fourth decade of life, with a strong female preponderance. More than one risk factor is usually involved in wandering spleen cases, so it is difficult to determine the relative contribution of each risk factor. Our patient was a multiparous woman in her sixth decade of life. Her splenomegaly resulting from coexisting CLD appeared to be an additional risk factor for increased splenic mobility and torsion.
Wandering spleen can be complicated with torsion of pedicle, infarction, hypersplenism, pancreatitis, bowel obstruction, gastric volvulus, and gastric variceal bleeding due to left-sided (sinistral) PHT.2 Unlike gastric varices, esophageal varices have not been described in wandering spleen. Diagnosis of torsion is based on a whirled appearance of the splenic vessels on CT scan.3 Patchy hypoattenuating areas in the liver, secondary to compromised vascular supply, was described in a case of wandering spleen with torsion.4 Imaging in our patient showed heterogeneous echotexture and diffuse atrophy of liver parenchyma. The diagnosis of CLD and PHT was made on the basis of the presence of high SAAG ascites, esophageal varices, and imaging appearances suggestive of CLD. Splenectomy has been advocated in cases of torsion, infarction, splenic vessel thrombosis, and suspicion of cancer. Splenopexy is preferred in the presence of viable splenic tissue. This patient refused the splenectomy, and follow-up was continued without further complication.
Enlarged wandering spleen due to CLD and PHT is an extremely rare condition.5 CLD and wandering spleen can complicate each other. Repeated episodes of partial torsion and spontaneous detorsion of the splenic pedicle can cause recurrent pain, splenomegaly, and presinusoidal PHT. The massively enlarged spleen can also compress against the portal venous system during torsion, causing further PHT.2 A rapidly enlarging spleen due to underlying CLD and PHT is more prone to torsion in the ectopic location, where the spleen is already predisposed to torsion. Torsion further aggravates the left-sided PHT. To our knowledge, this is the second report of a massive splenomegaly in a patient with wandering spleen and cryptogenic CLD. After splenectomy, enlargement of an accessory spleen and recurrence of hypersplenism and variceal bleeding have been described in patients with CLD.6
Disclosures
Author contributions: All authors contributed equally to the manuscript. AK Jha is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Ho CL. Wandering spleen with chronic torsion in a patient with thalassaemia. Singapore Med J. 2014; 55:e198–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan HH, Ooi LL, Tan D, Tan CK. Recurrent abdominal pain in a woman with a wandering spleen. Singapore Med J. 2007; 48(4):e122.. [PubMed] [Google Scholar]
- 3.Priyadarshi RN, Anand U, Kumar B, Prakash V. Torsion in wandering spleen: CT demonstration of whirl sign. Abdom Imaging. 2013; 38:835–8. [DOI] [PubMed] [Google Scholar]
- 4.Maksoud SF, Swamy N, Khater NH. Tale of a wandering spleen: 1800 degree torsion with infarcted spleen and secondary involvement of liver. J Radiol Case Rep. 2014; 8:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Satpathi T, Mukhopadhyay S. Ectopic spleen with cirrhosis of liver. J Assoc Physicians India. 2008; 56:819–820. [PubMed] [Google Scholar]
- 6.Mishin I, Ghidirim G. Accessory splenectomy with gastroesophageal devascularization for recurrent hypersplenism and refractory bleeding varices in a patient with liver cirrhosis: Report of a case. Surg Today. 2004; 34:1044–8. [DOI] [PubMed] [Google Scholar]