The intervention improved the performance of key FCR elements, which were associated with significant changes in engagement and improvements in parent perceptions of safety.
Abstract
BACKGROUND AND OBJECTIVES:
Family-centered rounds (FCRs) have become standard of care, despite the limited evaluation of FCRs’ benefits or interventions to support high-quality FCR delivery. This work examines the impact of the FCR checklist intervention, a checklist and associated provider training, on performance of FCR elements, family engagement, and patient safety.
METHODS:
This cluster randomized trial involved 298 families. Two hospital services were randomized to use the checklist; 2 others delivered usual care. We evaluated the performance of 8 FCR checklist elements and family engagement from 673 pre- and postintervention FCR videos and assessed the safety climate with the Children’s Hospital Safety Climate Questionnaire. Random effects regression models were used to assess intervention impact.
RESULTS:
The intervention significantly increased the number of FCR checklist elements performed (β = 1.2, P < .001). Intervention rounds were significantly more likely to include asking the family (odds ratio [OR] = 2.43, P < .05) or health care team (OR = 4.28, P = .002) for questions and reading back orders (OR = 12.43, P < .001). Intervention families’ engagement and reports of safety climate were no different from usual care. However, performance of specific checklist elements was associated with changes in these outcomes. For example, order read-back was associated with significantly more family engagement. Asking families for questions was associated with significantly better ratings of staff’s communication openness and safety of handoffs and transitions.
CONCLUSIONS:
The performance of FCR checklist elements was enhanced by checklist implementation and associated with changes in family engagement and more positive perceptions of safety climate. Implementing the checklist improves delivery of FCRs, impacting quality and safety of care.
What’s Known on This Subject:
Family-centered rounds (FCRs) are suggested to improve the quality and safety of pediatric inpatient care. FCRs have become standard practice, despite limited evidence to support consistent high-quality FCR delivery or rigorous evaluation of their benefit.
What This Study Adds:
Implementing the FCR checklist significantly improved the performance of 3 key FCR elements. In addition, performance of specific FCR elements was associated with significant changes in family engagement during FCRs and improvements in parent perceptions of safety.
Family-centered care has been recommended by the Institute of Medicine as a key to improving the quality and safety of health care.1 To achieve this type of care, experts suggest family-centered rounds (FCRs) as the standard for hospitalized children.2–4 Although FCRs are being performed at most children’s hospitals and many community hospitals,5 great variability exists in the elements that constitute FCRs.6 Implementing effective FCRs requires the development and assessment of tools supporting standardized FCR delivery.5 To address this need, we developed the FCR checklist intervention, a checklist and associated provider training, to standardize delivery of high-quality FCR (www.hipxchange.org/FamilyRounds).7–9
Despite suggested benefits of FCRs,3,10–12 rigorous trials of the impact of FCRs are lacking. Only 2 trials have assessed the impact of family presence during rounds, 1 of which is now nearly 30 years old13 and the other randomized only 27 families, finding greater parental satisfaction when rounding with the team at the bedside.10 Other qualitative, quality improvement, or pre–postintervention studies suggest that health care providers and families believe that FCR supports building relationships,13–15 sharing information,13,16–19 and engaging in decision-making.11,20 However, additional work is needed to assess whether FCR can influence the quality and safety of care for hospitalized children. In this cluster randomized trial, we assessed the impact of our FCR checklist intervention on: (1) performance of checklist elements, (2) family engagement in talk that builds relationships, shares information, or facilitates decision-making, and (3) parent perceptions of the patient safety climate in our children’s hospital.
Methods
Study Design, Setting, and Participants
To represent children’s hospital patients broadly, including both acute and chronic disease admissions, we collected data from 4 services: 2 general pediatric hospitalist services, the pulmonary service, and the hematology/oncology service. The hospitalist services admit many children with acute concerns (eg, respiratory distress), whereas the other services mostly admit children with ongoing or chronic illnesses (eg, cystic fibrosis or cancer). To strengthen our ability to determine causality, our study used a pre–post cluster randomized design,21,22 randomizing 2 services to use the intervention with all their patients, whereas 2 others delivered usual care. Services were aware of their designation as intervention or usual care. One research team member (R.L.B.) used a computer algorithm to randomly designate intervention (1 hospitalist service and the hematology/oncology service) and usual care services (the other hospitalist service and the pulmonary service). The attending, a senior resident, 2 interns, ∼4 medical students, and the patient’s nurse typically participated in FCRs, with other team members joining as appropriate. We collected preintervention data at our 61-bed children’s hospital from October 2010 to May 2011; the postintervention data collection occurred from October 2012 to May 2013.
During the recruitment periods, the family of each child (aged 0–17 years) admitted to a participating service was approached to participate. Children with stigmatizing reasons for hospitalization (eg, suspected nonaccidental trauma or mental health concerns), new cancer diagnoses, or whose parent(s) were unavailable to consent (absent or sleeping during recruitment) or could not speak or read English did not meet inclusion criteria and were excluded. Written consent was obtained from parents and children ages 15 to 17 years, with children ages 7 to 14 years providing written assent. The University of Wisconsin Health Sciences Institutional Review Board approved this study.
The FCR Checklist Intervention
The FCR checklist intervention was developed through stakeholder engagement, including parents, health care team members, institutional leadership, and patient advocates. To identify suggestions to optimize family engagement in FCRs, stimulated recall methods were used with 11 parents, 4 children, and 22 health care team members.8,9,23,24 Suggestions from these interviews were aggregated into 21 possible improvements. These were then prioritized by stakeholders, including 42 parents, based on feasibility and potential impact,8 ultimately resulting in 8 “best practices” for FCRs, organized in a checklist format (Supplemental Fig 2). Checklist elements (Table 1) were arranged in the order they typically occur during rounds, beginning with ensuring the nurse is present and ending with reading back orders, but they could be performed in any order. To optimize implementation, the checklist was bundled with a 1-hour interactive training, a brief refresher training, tools to monitor implementation, and laminated checklists for use as prompts, constituting the FCR checklist intervention (toolkit available at www.hipxchange.org/familyrounds).8
TABLE 1.
Descriptive Characteristics of the Participants and Study Outcomes for Usual Care and Intervention Services, Pre- and Postintervention
| Participant Characteristics | Usual Care Admissionsa | Intervention Admissionsb | ||
|---|---|---|---|---|
| Pre (n = 70) | Post (n = 76) | Pre (n = 74) | Post (n = 78) | |
| Child | ||||
| Female child, % (n) | 46 (32) | 57.9 (44) | 50 (37) | 44 (34) |
| Child age, mean (SD), y | 6.0 (5.7) | 5.7 (5.3) | 5.6 (5.6) | 5.0 (5.2) |
| Child health status, % (n) | ||||
| Good to excellent | 86 (60) | 87 (66) | 85 (63) | 87 (68) |
| Parent | ||||
| Mother, % (n) | 81 (57) | 83 (63) | 88 (65) | 82 (64) |
| White, non-Hispanic, % (n) | 84 (59) | 89 (68) | 84 (62) | 91 (71) |
| Parent education, % (n) | ||||
| High school or less | 21 (15) | 8 (6) | 15 (11) | 26 (20) |
| Some college | 31 (22) | 38 (29) | 39 (29) | 27 (21) |
| Bachelor's degree or more | 46 (32) | 54 (41) | 46 (34) | 47 (37) |
| Parent age, mean (SD), y | 35.0 (7.6) | 35.4 (6.7) | 34.6 (7.9) | 33.9 (6.9) |
| Length of stay, % (n) | ||||
| 1 d | 46 (32) | 43 (33) | 34 (25) | 40 (31) |
| 2–3 d | 31 (22) | 33 (25) | 45 (33) | 38 (30) |
| 4–7 d | 4 (3) | 16 (12) | 18 (13) | 14 (11) |
| >1 wk | 19 (13) | 8 (6) | 4 (3) | 8 (6) |
| FCR length, mean (SD), min | 10.2 (4.6) | 10.4 (3.4) | 9.9 (3.6) | 11.2 (4.6) |
| Checklist elements | ||||
| Total checklist elements performed, mean (SD) | 4.6 (1.0) | 4.9 (1.0) | 4.3 (1.0) | 5.9 (1.2) |
| Nurse present, mean % (SD)c | 86 (29.8) | 88 (27.7) | 88 (23.8) | 88 (26.5) |
| Introductions made, mean % (SD) | 29 (41.6) | 39 (41.1) | 21 (34.1) | 47 (42.9) |
| Assessment provided, mean % (SD) | 58 (42.5) | 64 (40.5) | 48 (40.9) | 69 (41.9) |
| Plan summarized, mean % (SD) | 97 (11.5) | 100 (2.8) | 96 (18.2) | 98 (8.6) |
| Family was asked for questions, mean % (SD) | 71 (37.2) | 73 (36.2) | 67 (37.9) | 88 (26.1) |
| Health care team was asked for questions, mean % (SD) | 24 (35.2) | 28 (35.4) | 23 (33.8) | 59 (41.3) |
| Discharge goals discussed, mean % (SD) | 82 (26.9) | 85 (24.8) | 76 (33.8) | 83 (31.1) |
| Orders were read back, mean % (SD) | 9 (20.9) | 17 (29.7) | 7 (20.1) | 52 (42.8) |
| Family engagementd | ||||
| Relationship building, mean (SD) | 43.7 (31.1) | 42.6 (18.7) | 36.0 (22.5) | 41.6 (24.1) |
| Information giving, mean (SD) | 32.1 (34.4) | 23.4 (19.2) | 33.1 (28.8) | 28.3 (23.6) |
| Information gathering, mean (SD) | 3.3 (3.3) | 3.0 (2.5) | 3.1 (3.2) | 3.3 (3.6) |
| Decision-making, mean (SD) | 3.2 (3.0) | 4.0 (3.2) | 2.9 (2.2) | 4.4 (4.2) |
| Parent perceptions of safety climatee | ||||
| Overall safety, mean (SD) | 4.1 (0.7) | 4.1 (0.7) | 4.2 (0.8) | 4.1 (0.7) |
| Staff communication openness, mean (SD) | 3.9 (0.7) | 3.9 (0.7) | 4.0 (0.6) | 4.0 (0.8) |
| Family communication openness, mean (SD) | 4.5 (0.6) | 4.5 (0.6) | 4.5 (0.6) | 4.6 (0.6) |
| Handoffs and transitions, mean (SD) | 3.9 (0.8) | 3.9 (0.9) | 4.0 (0.9) | 4.0 (1.0) |
Values may not add to 100% due to rounding.
Includes admissions to general pediatrics 1 (hospitalist) and pulmonary services.
Includes admissions to general pediatrics 2 (hospitalist) and hematology/oncology services.
For each checklist element, the mean and SD of the average percent of rounds during which the element was performed during a patient’s stay.
Mean and SD of the number of utterances or decision-making events that families engaged in during FCRs.
Mean and SD of parents’ safety climate domain scores, in which all of the domains’ elements were rated on a 5-point scale (1, strongly disagree to 5, strongly agree) with higher scores indicating more favorable perceptions.
Data Collection
Before the consented families’ first FCR, parents completed surveys of demographics, comorbidities, and previous hospitalizations (see Table 1). Child characteristics included child age, sex, and health status (single item, 5-point Likert scale).25 Parent characteristics included age, sex, race/ethnicity, and education (eighth grade or less; 9th to 12th grade but not high school graduate; high school graduate or equivalent; some college; bachelor’s degree; graduate or professional degree). Length of stay was calculated based on admit and discharge dates. A researcher video-recorded each FCR during the child’s stay.
Outcome Measures
Checklist Element Performance
Pairs of trained coders evaluated videos for performance of checklist elements, except for the element “Assess family preference for rounds,” which was not evaluated because this often occurred before rounds and therefore was not always captured on video. Coders received 23 hours of training over 6 weeks, using a training manual and pilot videos, and then met monthly over 8 months to resolve areas of disagreement by consensus. Coders were blinded to intervention or usual care status. For stays >7 days, 7 videos were coded (admit day, day after admission, day before discharge, discharge day, and the 3 days marking one-quarter, half, and three-quarters of the duration of the stay).
Family Engagement in Rounds
Family engagement in communication tasks that support family-centeredness was assessed from FCR videos by using 2 reliable, validated coding schemes. Videos were assessed for family engagement in relationship building, information giving, and information gathering, by using the Roter Interaction Analysis System. This widely used system for coding clinical communication provides a mechanism for categorizing each speaker’s talk at the level of the utterance (the smallest discernable speech segment to which a category may be assigned [eg, a word, phrase, or sentence with a single intent]) into 1 of 34 mutually exclusive categories.26,27 To evaluate family engagement in decision-making (proposing a plan, raising risks or benefits of a possible plan, or disagreeing with a proposed plan), coders applied a validated coding scheme developed by one of the authors.28,29 Talk was coded only for periods in which the health care team was present during the round. Child and parent talk was summed to reflect family engagement. As with checklist element performance, 7 representative videos were coded for stays >7 days. To represent family engagement over the entire hospital stay, counts of categorized utterances or events for each communication task were averaged across all of the patient’s FCRs.
Family engagement was assessed by a team of 20 trained, blinded coders. Each coder received a minimum of 20 hours of training, using a training manual and pilot videos. Subsequently, coders met at least monthly over 9 months to review areas of disagreement. Intercoder reliability was assessed by double-coding a random sample of videos (93 videos [13%] for Roter Interaction Analysis System and 84 videos [12%] for engagement in decision-making). Reliabilities were near perfect for relationship building, information giving, and information gathering (intraclass correlation coefficient >0.8), which were treated as continuous variables, and substantial for family engagement in decision-making (κ > 0.6), treated as a count.30,31
Parent Perceptions of Children’s Hospital Safety Climate
Because patients and parents are at the front lines of care, their perceptions of hospital safety are highly relevant indicators of the safety of care relating to outcomes, such as posthospitalization treatment adherence or readmissions.32–38 For instance, parents are first-hand witnesses to medication errors, adherence to safety procedures (eg, hand hygiene), and information handoffs during shift changes.39,40 Therefore, the Children’s Hospital Safety Climate Survey was administered at discharge to assess parent perspectives of safety during the stay.38 Domains included overall perceptions of safety (4 items), staff communication openness (3 items), family communication openness (3 items), and handoffs and transitions (4 items). Domain scores were created by averaging item responses, which were on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree), with negatively worded items reverse-scored.
Analyses
Descriptive analyses were performed, including proportions or means and SDs. All analyses of intervention effects were performed by the originally assigned arm. To strengthen our ability to infer causality, our random effects linear or logistic regression models of intervention impact included an arm indicator (intervention or usual care, reflecting whether the service eventually received the intervention), an indicator for the intervention period (preintervention or postintervention, regardless of arm), and an intervention-by-arm interaction representing the intervention effect (allowing the pre–post differences for each study arm to differ). This assessment of intervention effect and also the association of family engagement with the performance of each checklist element were assessed with random effects regression models. These models included a patient-level random intercept to account for repeated measures across the stay for a given patient. The association of parent perceptions of the hospital’s safety climate at discharge with average checklist element performance across all FCRs during the admission was assessed with linear regression by using pre- and postintervention data. All models were adjusted for child age and health status, parent education, and length of stay. Results are presented as odds ratios (ORs) or regression coefficients with 95% confidence intervals (CIs). Significance was assessed at P < .05. All analyses were performed by using Stata version 13 (Stata Corp, College Station, TX).
This study was powered a priori to detect small to moderate effect sizes (0.2–0.3 σ) in family engagement, based on previous work, leading to a goal of 300 participants.28,29 At trial inception, there were no previous data on which to base power calculations for the domains of the Children’s Hospital Safety Climate Survey. However, based on data collected before the intervention’s delivery, our sample size provided 80% power to detect a 10% change in safety climate domain means.
Results
Trial Recruitment and Participant Characteristics
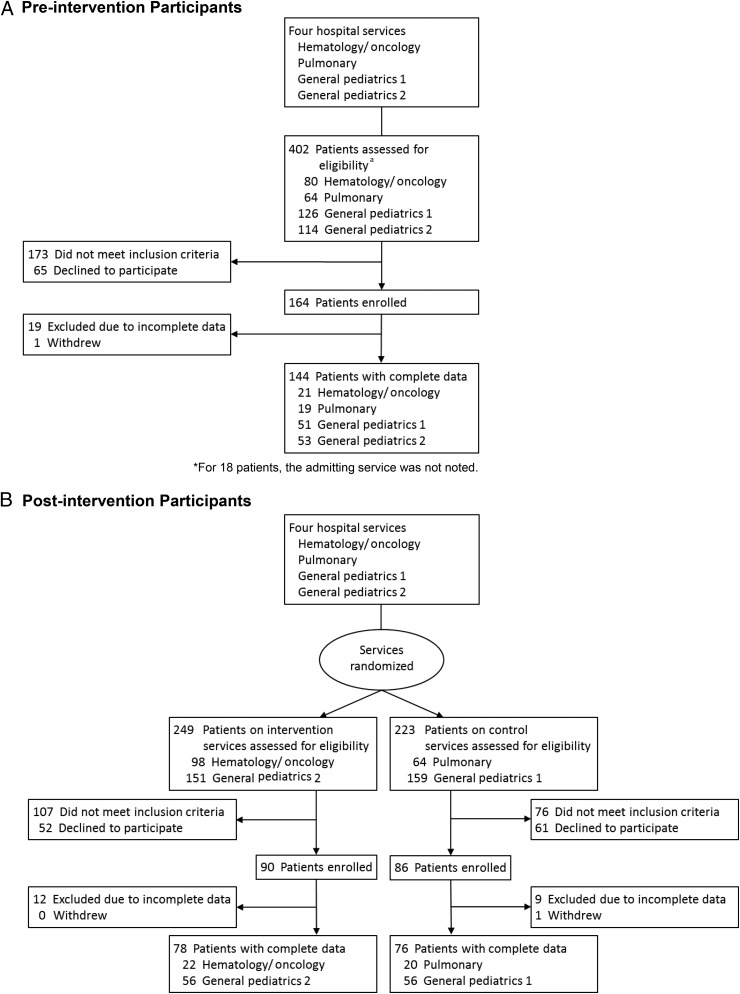
A total of 874 potential participant admissions (402 preintervention; 472 postintervention) were identified (Fig 1). Common reasons for exclusion were inability to consent before initial FCR (eg, parent was asleep or not present) (44%), stigmatizing or traumatic reasons for admission, such as suspected nonaccidental trauma or a new cancer diagnosis (15%), previous participation in the study (12%), and limited English proficiency (6%). Of 518 eligible admissions approached, 340 (66%) agreed to participate, with 164 families participating in the preintervention period and 176 in the postintervention period. Our final sample was 298 families: 144 preintervention (19 families were excluded due to incomplete data; 1 withdrew due to stress of a new diagnosis) and 154 postintervention (21 families were excluded due to incomplete data; 1 withdrew due to stress of a new diagnosis).
FIGURE 1.
Flow of participants in trial of FCR checklist intervention. A, Preintervention participants. B, Postintervention participants. a For 18 patients, the admitting service was not noted.
On average, children were young (5–6 years of age), and most were in good to excellent health. Parents were predominantly white, non-Hispanic mothers with a wide range of educational attainment. Common reasons for hospitalization were breathing problems, gastrointestinal problems, and fever. Hospital stays were typically >3 days, although ∼20% of children stayed longer. Rounds were ∼10 to 11 minutes in length. Usual care and intervention arms were comparable across numerous patient and parent characteristics. The only significantly different characteristic was length of stay (χ2, P = .04) (Table 1).
From the hospital stays of 298 children in the study, 673 FCR videos were evaluated. Usual care services contributed 348 videos (164 preintervention videos from 70 families; 184 postintervention videos from 76 families); intervention services contributed 325 videos (155 preintervention videos from 74 families; 170 postintervention videos from 78 families).
Descriptive Data for Main Outcomes
Checklist Element Performance
On average across services during the study period, ∼4.3 to 5.9 of the 8 checklist elements were performed during rounds (Table 1). Three elements were performed frequently (nurse present, plan summarized, discharge goals discussed), whereas other elements were performed with less regularity.
Family Engagement During FCRs
Across services and pre- and postintervention periods, mean family engagement in relationship building during FCRs ranged from 36.0 to 43.7 utterances (Table 1). Overall, families made an average of 23.4 to 33.1 information-giving utterances and 3.0 to 3.3 information-gathering utterances per round. Families engaged in decision-making an average of 2.9 to 4.4 times during FCRs.
Perceptions of Safety
Across services and pre- and postintervention periods, families reported strongly positive views of the 4 hospital safety climate domains, with mean scores ranging from 3.9 to 4.5 (Table 1). In general, families rated their own ability to communicate openly most highly, whereas the other 3 measures of safety climate received less positive ratings.
Intervention Impact
Impact of the Intervention on Checklist Element Performance
The intervention significantly improved the total number of checklist elements performed, with intervention teams, on average, completing 1.2 more checklist elements per round than usual care (β = 1.2, 95% CI: 0.72–1.67). The intervention significantly increased the likelihood that families were asked for questions (OR = 2.43, P < .05), the health care team was asked for questions (OR = 4.28, P = .002), and the health care team read back orders during FCRs (OR = 12.43, P < .001). Performance of the other checklist elements was not impacted significantly (Table 2).
TABLE 2.
Adjusted ORs and 95% CIs for the Intervention’s Effect on FCR Checklist Element Performance (n = 668 Rounds)
| FCR Checklist Element | OR (95% CI) |
|---|---|
| Nurse present | 0.63 (0.23 to 1.74) |
| Introductions made | 1.62 (0.70 to 3.76) |
| Assessment provided | 1.92 (0.69 to 5.31) |
| Plan summarized | 0.22 (0.02 to 2.08) |
| Family was asked for questions | 2.43 (1.01 to 5.85)a |
| Health care team was asked for questions | 4.28 (1.73 to 10.60)a |
| Discharge goals discussed | 1.96 (0.79 to 4.87) |
| Orders were read back | 12.43 (4.62 to 33.47)a |
Indicates P < .05. Random effects logistic regression models compared pre- and postintervention checklist element performance for intervention services versus usual care services, accounting for repeated measures across the stay for a given patient and adjusting for child age, health status, length of stay, and parent education.
Impact of the Checklist Intervention on Family Engagement
Adjusted models demonstrated no significant intervention effect on family engagement. However, performance of 2 checklist elements significantly increased family engagement, whereas 2 other checklist elements decreased family engagement (Table 3). Specifically, when the health care team read back orders, families engaged in more information giving (8.20 more utterances; P = .002), information gathering (0.86 more utterances; P = .02), and decision-making (0.66 more decision-making activities; P = .04). In addition, when the health care team discussed goals for discharge, relationship building increased (5.30 more utterances; P = .03). With regard to checklist elements associated with reduced engagement, when health care teams provided assessments of children’s progress, families engaged in significantly less relationship building (4.22 fewer utterances; P = .04), information gathering (0.86 fewer utterances; P = .005), and decision-making (0.57 fewer instances; P = .04). Additionally, when families were asked for questions during FCRs, they engaged in significantly less information giving (12.15 fewer utterances; P < .001).
TABLE 3.
Adjusted Regression Coefficients (β) and 95% CIs for Association of FCR Checklist Element Performance With Family Engagement in Communication Tasks (n = 668 rounds)
| FCR Checklist Element | β (95% CI) | |||
|---|---|---|---|---|
| Relationship Building | Information Giving | Information Gathering | Decision-making | |
| Nurse present | −1.30 (−6.98 to 4.39) | 0.06 (−6.34 to 6.46) | −0.77 (−1.60 to 0.06) | 0.24 (−0.49 to 0.97) |
| Introductions made | 2.52 (−1.92 to 6.96) | −2.11 (−7.14 to 2.93) | −0.01 (−0.66 to 0.63) | 0.27 (−0.30 to 0.84) |
| Assessment provided | −4.22 (−8.33 to −0.11)a | −4.44 (−8.88 to 0.00) | −0.86 (−1.45 to −0.26)a | −0.57 (−1.10 to −0.04)a |
| Plan summarized | 4.36 (−6.45 to 15.18) | −11.09 (−23.52 to 1.34) | 0.95 (−0.63 to 2.54) | 0.38 (−1.03 to 1.78) |
| Family was asked for questions | −4.22 (−8.64 to 0.20) | −12.15 (−17.06 to −7.24)a | −0.22 (−0.87 to 0.42) | 0.01 (−0.56 to 0.58) |
| Health care team was asked for questions | −0.38 (−4.55 to 3.79) | −1.41 (−5.99 to 3.17) | 0.23 (−0.38 to 0.84) | 0.08 (−0.46 to 0.62) |
| Discharge goals discussed | 5.30 (0.63 to 9.96)a | −3.58 (−8.91 to 1.75) | 0.54 (−0.15 to 1.22) | 0.13 (−0.48 to 0.74) |
| Orders were read back | 4.08 (−0.76 to 8.93) | 8.20 (2.97 to 13.43)a | 0.86 (0.16 to 1.56)a | 0.66 (0.04 to 1.29)a |
Indicates P < .05. β describes the change in the number of utterances or decision-making events associated with a 1% increase in the percentage of FCR in which the checklist element was performed. Random effects models included all participants across intervention arms both pre- and postintervention, accounted for repeated measures across the stay for a given patient, and were adjusted for child age, health status, length of stay, and parent education.
Impact of Checklist Intervention on Parent Perceptions of Safety
Adjusted models demonstrated no significant intervention effect on parent perceptions of safety. However, the performance of particular FCR checklist elements improved parent perceptions of 2 safety climate domains (Table 4). Specifically, parent views of staff communication openness significantly increased with the proportion of FCRs in which the family was asked for questions. In addition, parents’ perceptions of the safety of handoffs and transitions significantly increased with the proportion of FCRs in which the health care team gave an assessment of their child’s progress or asked the family if they had any questions.
TABLE 4.
Adjusted Regression Coefficients (β) and 95% CIs for Association of FCR Checklist Element Performance With Parent Perceptions of Safety (n = 298 Admissions)
| FCR Checklist Element | β (95% CI) | |||
|---|---|---|---|---|
| Overall Safety | Staff Communication Openness | Family Communication Openness | Handoffs and Transitions | |
| Nurse present | −0.03 (−0.33 to 0.27) | −0.01 (−0.31 to 0.29) | 0.20 (−0.06 to 0.45) | 0.07 (−0.32 to 0.46) |
| Introductions made | −0.15 (−0.36 to 0.06) | −0.14 (−0.35 to 0.07) | −0.12 (−0.30 to 0.06) | −0.11 (−0.38 to 0.17) |
| Assessment provided | 0.17 (−0.03 to 0.36) | 0.18 (−0.02 to 0.38) | 0.06 (−0.11 to 0.23) | 0.27 (0.02 to 0.53)a |
| Plan summarized | 0.03 (−0.67 to 0.73) | 0.39 (−0.32 to 1.10) | −0.19 (−0.79 to 0.41) | 0.04 (−0.87 to 0.95) |
| Family was asked for questions | 0.07 (−0.17 to 0.31) | 0.38 (0.14 to 0.62)a | 0.09 (−0.11 to 0.29) | 0.32 (0.01 to 0.62)a |
| Health care team was asked for questions | 0.00 (−0.21 to 0.21) | 0.01 (−0.20 to 0.23) | −0.02 (−0.20 to 0.16) | 0.07 (−0.20 to 0.33) |
| Discharge goals discussed | 0.12 (−0.23 to 0.47) | −0.05 (−0.40 to 0.31) | 0.02 (−0.28 to 0.32) | 0.23 (−0.23 to 0.68) |
| Orders were read back | −0.04 (−0.27 to 0.19) | −0.01 (−0.25 to 0.22) | 0.08 (−0.11 to 0.28) | 0.03 (−0.27 to 0.33) |
Indicates P < .05. β describes the change in parent perceptions for each of the 4 safety domains associated with a 1% increase in the average percentage of FCRs in which the checklist element was performed during the child’s stay. Models included all participants across intervention arms both pre- and postintervention and were adjusted for child age, health status, length of stay, and parent education.
Discussion
Implementation of the FCR checklist intervention succeeded in increasing the likelihood that key FCR elements, as defined by patients, families, and staff, were performed. Although the intervention did not alter family engagement or perceptions of safety, performance of specific checklist elements significantly influenced both of these outcomes. Thus, implementation of the checklist has implications for the delivery of safe, high-quality pediatric inpatient care. The checklist also offers a way to structure the delivery of FCRs to meet the needs of families, learners, and the health care team while also supporting future research comparing the effects of FCRs on other health care and educational outcomes.
Teams that used the checklist were significantly more likely to ask families and health care team members for questions. The act of asking for questions allows health care teams to leverage the expertise of families as the primary caregivers for the child and also provides other team members, such as nurses, pharmacists, and case managers, an opportunity to share their expertise. Nurses in particular can present issues or questions that families may have raised to them, but which families may not feel comfortable speaking up about during FCRs.
Asking families if they have questions was associated with improved perceptions of safety, but also with less information giving by families during FCRs. It is possible that families who were specifically invited to ask questions may have been empowered to directly ask whatever questions they had, rather than repeating or providing additional information in hopes that the health care team might infer their question and address it. Alternatively, health care teams may have been more likely to ask families for questions when the family had been less engaged in providing information during rounds. Yet asking families for questions positively influenced parent perceptions of safety, improving both perceptions of staff communication openness and of the safety of handoffs and transitions, which is consistent with other studies of interventions to promote communication and teamwork.41–43 Thus, implementation of this checklist element may be an appropriate intervention to improve parent perceptions of safety in children’s hospitals.
The intervention also increased the likelihood that orders would be read back during FCRs, and performance of this checklist element increased family engagement. When orders were read back, families both asked for and gave more information and also engaged more in decision-making. Reading back orders may signal a willingness to have those orders questioned or modified. This read back also promotes a shared mental model of the orders, creating a foundation on which families and health care team members could formulate questions. In previous work, we found that many families use FCR as a venue to discuss medication topics.20 Because computerized physician order entry has not yet been able to eliminate medication errors and potential or actual adverse events,44,45 order read back may be particularly powerful in fostering safe medication use for hospitalized children.
Also, interestingly, providing an assessment of the child’s progress increased perceptions of the safety of handoffs and transitions, yet it reduced family engagement across all 4 communication areas. Because our coding of checklist element performance did not assess the family-centeredness of this performance, providing this assessment may have structured FCRs in a manner that was less family-centered, reducing family comfort with engaging. Alternatively, provision of this assessment may have created reassurance or clarity for families, who then felt less need to engage verbally during FCRs. This latter hypothesis is additionally supported by the fact that providing an assessment was associated with greater parent perception of safety during handoffs and transitions. Thus, although providing an assessment reduced family engagement as measured in this study, this checklist element should not necessarily be seen as a detriment to care. Future work could attempt to tease out these complex relationships, which may lead to improvements in the family-centeredness of this checklist item, for example, by engaging families in providing assessments of children’s progress.
As with all studies, certain limitations are notable. As a single institution study, findings may not be generalizable to children’s hospitals broadly. Our study population had relatively few minority families and was better educated than the general population. Thus, we may be underrepresenting the impact of the checklist for these families, who may be especially likely to benefit, given that they are often more concerned about the safety of health care.46 In addition, because some tools for assessing family engagement have been validated only for English-speaking interactions, we excluded non–English-speaking families, who may face unique challenges in participating in FCRs. The checklist, however, does incorporate many of the recommendations for successful FCRs with non–English-speaking Latino families.47 Although randomizing 4 services would not be expected to balance measured and unmeasured covariates, trial arms were not significantly different across numerous relevant characteristics. In addition, we employed a pre–post controlled design to mitigate the impact of differences between services and also adjusted our models for imbalances and clinically relevant potential confounders. Coders were blinded, but they may have been able to distinguish between arms after coding multiple videos.
Our intervention did not significantly affect performance of the remaining 5 checklist elements. For 2 of these, performance rates were high before the intervention. For other elements, performance improved in intervention and usual care services, perhaps because FCRs were a critically important hospital initiative or because the intervention diffused to usual care services through shared staff, such as nurses who worked on both intervention and usual care services daily and interns who cross-cover patients during nights and weekends. Although this diffusion limits our ability to detect significant intervention effects, we still found evidence of the intervention’s impact. To additionally enhance the family-centeredness of the performance of these elements, specific suggestions, such as inviting families to speak, ask questions, or share updates early in FCRs, might additionally improve the impact of the intervention.48–50 Future research could also examine whether the intervention improved the family-centeredness of the health care team’s communication with families or had differential effects across services.
Conclusions
The FCR checklist intervention succeeded in increasing the performance of specific FCR elements. The intervention itself did not alter family engagement or parent perceptions of safety; however, performance of specific checklist elements significantly influenced both of these outcomes. Thus, the FCR checklist intervention can help effectively promote consistent delivery of high-quality, family-centered pediatric inpatient care while also improving patient safety from the perspective of parents.
Supplementary Material
Glossary
- CI
confidence interval
- FCR
family-centered round
- OR
odds ratio
Footnotes
Dr Cox secured funding, conceived and designed the study, codeveloped the intervention and its implementation, created or adapted the video-coding methods, oversaw all data collection, coding, and analyses, and drafted and revised the manuscript; Dr Jacobsohn cocreated the coding scheme for the family-centered rounds checklist elements, oversaw the coding of videos for the family-centered rounds checklist elements, performed analyses, and revised the manuscript; Ms Rajamanickam performed analyses and revised the manuscript; Drs Carayon, Kelly, and Wetterneck codeveloped the intervention and its implementation and revised the manuscript; Drs Rathouz and Brown oversaw analyses and revised the manuscript; and all authors approved the final version for submission.
This trial has been registered at www.clinicaltrials.gov (identifier NCT02625142).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded through an Agency for Healthcare Research and Quality Health Services Research Dissemination and Demonstration grant (R18 HS018680) to Dr Cox. The project described was also supported by the Clinical and Translational Science Award program, previously through the National Center for Research Resources grant 1UL1RR025011 and now by the National Center for Advancing Translational Sciences grant 9U54TR000021. In addition, Dr Cox has received honoraria and contract funding from the Patient-Centered Outcomes Research Institute and serves on their Improving Healthcare Systems advisory panel. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funders and sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001 [PubMed] [Google Scholar]
- 2.Committee on Hospital Care and Institute for Patient- and Family-Centered Care Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404 [DOI] [PubMed] [Google Scholar]
- 3.Davidson JE, Powers K, Hedayat KM, et al. ; American College of Critical Care Medicine Task Force 2004-2005, Society of Critical Care Medicine . Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007;35(2):605–622 [DOI] [PubMed] [Google Scholar]
- 4.Sisterhen LL, Blaszak RT, Woods MB, Smith CE. Defining family-centered rounds. Teach Learn Med. 2007;19(3):319–322 [DOI] [PubMed] [Google Scholar]
- 5.Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126(1):37–43 [DOI] [PubMed] [Google Scholar]
- 6.Sharma A, Norton L, Gage S, et al. A quality improvement initiative to achieve high nursing presence during patient- and family-centered rounds. Hosp Pediatr. 2014;4(1):1–5 [DOI] [PubMed] [Google Scholar]
- 7.Cox E, Carayon P, Kelly M, DuBenske L, Wetterneck T, Brown R The family-centered rounds toolkit. Available at: www.hipxchange.org/familyrounds. Accessed June 12, 2016
- 8.Xie A, Carayon P, Cox ED, et al. Application of participatory ergonomics to the redesign of the family-centred rounds process. Ergonomics. 2015;58(10):1726–1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly MM, Xie A, Carayon P, DuBenske LL, Ehlenbach ML, Cox ED. Strategies for improving family engagement during family-centered rounds. J Hosp Med. 2013;8(4):201–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landry MA, Lafrenaye S, Roy MC, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275–280 [DOI] [PubMed] [Google Scholar]
- 11.Rosen P, Stenger E, Bochkoris M, Hannon MJ, Kwoh CK. Family-centered multidisciplinary rounds enhance the team approach in pediatrics. Pediatrics. 2009;123(4). Available at: www.pediatrics.org/cgi/content/full/123/4/e603 [DOI] [PubMed] [Google Scholar]
- 12.Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829–832 [DOI] [PubMed] [Google Scholar]
- 13.Lewis C, Knopf D, Chastain-Lorber K, et al. Patient, parent, and physician perspectives on pediatric oncology rounds. J Pediatr. 1988;112(3):378–384 [DOI] [PubMed] [Google Scholar]
- 14.Kuo DZ, Sisterhen LL, Sigrest TE, Biazo JM, Aitken ME, Smith CE. Family experiences and pediatric health services use associated with family-centered rounds. Pediatrics. 2012;130(2):299–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kendall EM. Improving patient care with collaborative rounds. Am J Health Syst Pharm. 2003;60(2):132–135 [DOI] [PubMed] [Google Scholar]
- 16.Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292–297 [DOI] [PubMed] [Google Scholar]
- 17.Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19(5):421–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cameron MA, Schleien CL, Morris MC. Parental presence on pediatric intensive care unit rounds. J Pediatr. 2009;155(4):522–528 [DOI] [PubMed] [Google Scholar]
- 19.Lehmann LS, Brancati FL, Chen MC, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155 [DOI] [PubMed] [Google Scholar]
- 20.Benjamin JM, Cox ED, Trapskin PJ, et al. Family-initiated dialogue about medications during family-centered rounds. Pediatrics. 2015;135(1):94–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mercer SL, DeVinney BJ, Fine LJ, Green LW, Dougherty D. Study designs for effectiveness and translation research: identifying trade-offs. Am J Prev Med. 2007;33(2):139–154 [DOI] [PubMed] [Google Scholar]
- 22.Cable G. Enhancing causal interpretations of quality improvement interventions. Qual Health Care. 2001;10(3):179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyle J. Stimulated recall: a report on its use in naturalistic research. Br Educ Res J. 2003;29(6):861–878 [Google Scholar]
- 24.Xie A, Carayon P, Cartmill R, et al. Multi-stakeholder collaboration in the redesign of family-centered rounds process. Appl Ergon. 2015;46(pt A):115–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233 [DOI] [PubMed] [Google Scholar]
- 26.Roter D. RIASWORKS. Available at: www.riasworks.com/. Accessed April 27, 2016
- 27.Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243–251 [DOI] [PubMed] [Google Scholar]
- 28.Cox ED, Raaum SE. Discussion of alternatives, risks and benefits in pediatric acute care. Patient Educ Couns. 2008;72(1):122–129 [DOI] [PubMed] [Google Scholar]
- 29.Cox ED, Smith MA, Brown RL. Evaluating deliberation in pediatric primary care. Pediatrics. 2007;120(1). Available at: www.pediatrics.org/cgi/content/full/120/1/e68 [DOI] [PubMed] [Google Scholar]
- 30.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174 [PubMed] [Google Scholar]
- 31.Fleiss JL, Shrout PE. Approximate interval estimation for a certain intraclass correlation coefficient. Psychometrika. 1978;43(2):259–262 [Google Scholar]
- 32.Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res. 2010;10(1):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singer S, Lin S, Falwell A, Gaba D, Baker L. Relationship of safety climate and safety performance in hospitals. Health Serv Res. 2009;44(2 pt 1):399–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosen AK, Singer S, Shibei Zhao, Shokeen P, Meterko M, Gaba D. Hospital safety climate and safety outcomes: is there a relationship in the VA? Med Care Res Rev. 2010;67(5):590–608 [DOI] [PubMed] [Google Scholar]
- 35.Hansen LO, Williams MV, Singer SJ. Perceptions of hospital safety climate and incidence of readmission. Health Serv Res. 2011;46(2):596–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6(4):226–232 [DOI] [PubMed] [Google Scholar]
- 37.Deilkås E, Hofoss D. Patient safety culture lives in departments and wards: multilevel partitioning of variance in patient safety culture. BMC Health Serv Res. 2010;10:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cox ED, Carayon P, Hansen KW, et al. Parent perceptions of children’s hospital safety climate. BMJ Qual Saf. 2013;22(8):664–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan A, Furtak SL, Melvin P, Rogers JE, Schuster MA, Landrigan CP. Parent-reported errors and adverse events in hospitalized children. JAMA Pediatr. 2016;170(4):e154608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Daniels JP, Hunc K, Cochrane DD, et al. Identification by families of pediatric adverse events and near misses overlooked by health care providers. CMAJ. 2012;184(1):29–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blegen MA, Sehgal NL, Alldredge BK, Gearhart S, Auerbach AA, Wachter RM. Improving safety culture on adult medical units through multidisciplinary teamwork and communication interventions: the TOPS Project. Qual Saf Health Care. 2010;19(4):346–350 [DOI] [PubMed] [Google Scholar]
- 42.Muething SE, Goudie A, Schoettker PJ, et al. Quality improvement initiative to reduce serious safety events and improve patient safety culture. Pediatrics. 2012;130(2). Available at: www.pediatrics.org/cgi/content/full/130/2/e423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weaver SJ, Rosen MA, DiazGranados D, et al. Does teamwork improve performance in the operating room? A multilevel evaluation. Jt Comm J Qual Patient Saf. 2010;36(3):133–142 [DOI] [PubMed] [Google Scholar]
- 44.Cho I, Park H, Choi YJ, Hwang MH, Bates DW. Understanding the nature of medication errors in an ICU with a computerized physician order entry system. PLoS One. 2014;9(12):e114243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wetterneck TB, Walker JM, Blosky MA, et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tarini BA, Lozano P, Christakis DA. Afraid in the hospital: parental concern for errors during a child’s hospitalization. J Hosp Med. 2009;4(9):521–527 [DOI] [PubMed] [Google Scholar]
- 47.Seltz LB, Zimmer L, Ochoa-Nunez L, Rustici M, Bryant L, Fox D. Latino families’ experiences with family-centered rounds at an academic children’s hospital. Acad Pediatr. 2011;11(5):432–438 [DOI] [PubMed] [Google Scholar]
- 48.Subramony A, Hametz PA, Balmer D. Family-centered rounds in theory and practice: an ethnographic case study. Acad Pediatr. 2014;14(2):200–206 [DOI] [PubMed] [Google Scholar]
- 49.Coyne I, Gallagher P. Participation in communication and decision-making: children and young people’s experiences in a hospital setting. J Clin Nurs. 2011;20(15-16):2334–2343 [DOI] [PubMed] [Google Scholar]
- 50.Stivers T. Physician-child interaction: when children answer physicians’ questions in routine medical encounters. Patient Educ Couns. 2012;87(1):3–9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.