Abstract
Background
Neutrophil-to-lymphocyte ratio (NLR) has been investigated as a prognostic marker in patients with diffuse large B-cell lymphoma (DLBCL); however, the results remain controversial. This study aimed to explore the association between NLR and survival outcomes and clinicopathological factors in DLBCL.
Methods
Relevant studies were retrieved by searching PubMed, Embase, Web of Science, and China National Knowledge Infrastructure (CNKI) databases. The last search was updated on February 17, 2017. Hazard ratios (HRs) and odds ratios (ORs) and their 95% confidence intervals (CIs) were used as effective measures in the meta-analysis. Random-effects models and fixed-effects models were used for analyses. Meta-regression was performed. Publication bias was assessed using Begg’s test. Stata version 12.0 was used for all analyses.
Results
A total of 9 studies with 2297 patients were included in the meta-analysis. The pooled results showed that NLR was a significant indicator for poor overall survival (OS) (HR = 1.84, 95% CI = 1.52–2.22, p<0.001) and poor progression-free survival (PFS) (HR = 1.64, 95% CI = 1.36–1.98, p<0.001). NLR remained a significant biomarker for OS and PFS regardless of location, sample size or cut-off value. In addition, high NLR was also associated with Ann Arbor stage (OR = 2.09, 95% CI = 1.14–3.81, p = 0.017), lactate dehydrogenase level (OR = 2.74, 95% CI = 1.16–6.46, p = 0.021), extranodal disease (OR = 1.63, 95% CI = 1.06–2.52, p = 0.027), and International Prognostic Index score (OR = 2.44, 95% CI = 1.03–5.08, p = 0.043). However, NLR was found to have no significant association with sex (OR = 0.89, 95% CI = 0.71–1.11, p = 0.29), age (OR = 1.18, 95% CI = 0.94–1.48, p = 0.152), European Cooperative Oncology Group performance status score (OR = 1.78, 95% CI = 0.71–4.46, p = 0.217), or presence of B symptoms (OR = 1.56, 95% CI = 0.7–3.48, p = 0.278).
Conclusion
In conclusion, our meta-analysis demonstrated that NLR has a strong association with worse OS and PFS in patients with DLBCL. NLR could be recommended as an inexpensive prognostic biomarker in DLBCL.
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common lymphoid malignancy in adults, accounting for approximately 20% of newly diagnosed lymphoid neoplasms [1]. DLBCL accounts for 31% of all non-Hodgkin’s lymphomas (NHL) in Western countries[2]. DLBCL is biologically and clinically heterogeneous and is typically treated with an R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) strategy [3]. Approximately 60–70% of DLBCL patients are curable using various regimens whereas other patients fail to respond to chemotherapy or have poor long-term survival outcomes [4]. Some indexes such as the International Prognostic Index (IPI) and gene expression profiling (GEP) can be used to identify risk patients [5, 6]. However, these parameters either lack the accuracy for prognosis or are hard to obtain in everyday clinical practice. Therefore, simple, inexpensive, and easily available prognostic biomarkers are urgently needed.
Inflammation often already exists in the tumor microenvironment before tumor occurrence and continues to facilitate tumor progression [7, 8]. Systemic inflammatory responses caused by and accompanied by tumorigenesis could provide information for prognostication. A series of prognostic indexes based on laboratory test results have emerged as objective and inexpensive indicators [9]. Such parameters include C-reactive protein (CRP), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), lymphocyte-to-monocyte ratio (LMR), and modified Glasgow Prognostic Score (mGPS)[10–15], of which, NLR was found to be related with worse survival outcomes in a variety of tumors [16], including DLBCL [12, 13, 17, 18]. However, previous studies have reported controversial results concerning the prognostic value of NLR in DLBCL [12, 17–20]. The conflicting results may be due to small sample sizes and heterogeneous patients in individual studies. To comprehensively evaluate NLR in DLBCL, a meta-analysis was performed by aggregating data from relevant studies. In this meta-analysis, we investigated the relationship between NLR and overall survival (OS) and progression-free survival (PFS); in addition, we also explored the association between NLR and different clinicopathological factors in DLBCL.
Materials and methods
This meta-analysis was carried out in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [21].
Literature search
A systematic literature search was performed by using the databases of PubMed, Embase, Web of Science, and China National Knowledge Infrastructure (CNKI) for all relevant studies. There was no language restriction. The last literature search was updated on February 17, 2017. The following terms were used in the search: “NLR,” “neutrophil-lymphocyte ratio,” “neutrophil to lymphocyte ratio,” “diffuse large B-cell lymphoma,” “lymphoma, large B-cell, diffuse” [MeSH Terms], and DLBCL. The references in the relevant studies were also screened for possible inclusions.
Selection criteria
The inclusion criteria were as follows: (a) NLR was obtained from a hematological test before treatment; (b) the diagnosis of DLBCL was pathologically confirmed; (c) the relationships between NLR and survival including OS or PFS were investigated or sufficient data were provided; (d) studies were published as full-text articles in English or Chinese. Literature falling under the following category was excluded: (a) reviews, meeting abstracts, letters, and duplicate studies; (b) irrelevant studies; (c) animal studies; and (d) studies without sufficient data.
Data extraction and qualitative assessment
Data were extracted by two independent investigators from eligible studies; discrepancies were resolved by joint discussion. The following information was extracted: first author, year of publication, study location, number of patients, tumor stage, treatment regimens, research period, cut-off value, survival outcomes, and hazard ratios (HRs) and 95% confidence intervals (CIs) for OS and/or PFS. The quality of each study was evaluated by using the 9-star Newcastle-Ottawa Scale (NOS) for cohort studies[22]. Studies with scores ≥7 were considered high-quality studies.
Statistical analysis
HRs with corresponding 95% CIs were used to evaluate the relationships between NLR and OS and/or PFS in DLBCL. Odds ratios (ORs) with 95% CIs were used to assess the strength of association between NLR and clinicopathological parameters. The heterogeneity among studies was calculated using Cochran’s Q test and Higgins I-squared statistic. P for heterogeneity <0.1 or I2 >50% was considered a significant level of heterogeneity. Both fixed effects (Mantel—Haenszel method) and random effects (DerSimonian and Laird method) models were performed to generate the pooled HRs. The random-effects model is more conservative and provides better estimates with wider confidence intervals[23, 24]. Meta-regression was also performed. Sensitivity analysis was conducted by sequential omission of each included studies. Publication bias was tested using Begg’s funnel plots. P<0.05 was considered statistically significant. All statistical analyses were performed with Stata version 12.0 (Stata Corp, College Station, TX).
Results
Literature selection and study characteristics
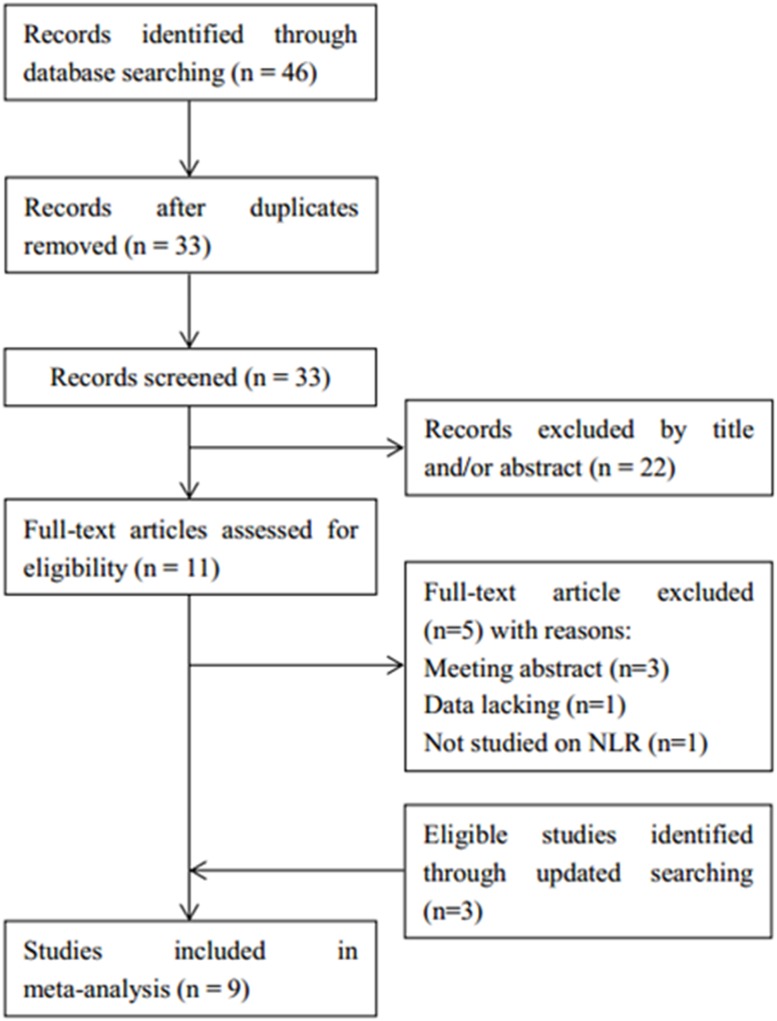
The flowchart of the literature selection process is shown in Fig 1. A total of 46 studies were identified through database searching, 33 records were screened after duplicates were excluded. Then, 22 records were excluded after title and/or abstract reading. Subsequently, 11 full-text articles were evaluated for eligibility. Five studies were further excluded because they were meeting abstracts and studies with insufficient or those that did not focus on NLR. Three studies[25–27] were found to be eligible through updated searching. In total, 9 studies [12, 13, 17, 18, 25–29] with 2297 patients were included for the meta-analysis. The main characteristics of included studies are demonstrated in Table 1. The studies were published between 2010 and 2017. Sample sizes ranged from 51 to 515. Seven studies[12, 13, 17, 18, 25–27] were published in English and 2 studies [28, 29] were published in Chinese. Eight studies [12, 13, 17, 18, 26–29] investigated the association between NLR and OS and 7 studies [12, 17, 18, 25–27, 29] reported a connection between NLR and PFS. All studies obtained a NOS score of ≥7. The detailed information of quality assessment is shown in Table 2.
Fig 1. Flowchart of article selection.
Table 1. Characteristics of included studies.
| Study | Year | Region | NOS score | Sample size | Age (years) median(range) | Stage | Treatment regimen | Study period | Cut-off | Outcomes analyzed |
|---|---|---|---|---|---|---|---|---|---|---|
| Porrata | 2010 | USA | 8 | 255 | 64(20–92) | I-IV | R-CHOP | 2000–2007 | 3.5 | OS, PFS |
| Ho | 2015 | Taiwan | 9 | 148 | 61(16–88) | I-IV | R-CHOP | 2001–2010 | 4.35 | OS, PFS |
| Keam | 2015 | Korea | 8 | 447 | 61(16–87) | I-IV | R-CHOP | 2003–2010 | 3 | OS, PFS |
| Melchardt | 2015 | Austria | 8 | 515 | 65(20–92) | I-IV | R-CHOP | 2004–2014 | 5.54 | OS |
| Ming | 2015 | China | 7 | 51 | 55(20–85) | I-IV | R-CHOP | 2009–2013 | 2.32 | OS |
| Hong | 2016 | Korea | 8 | 313 | 56(16–86) | I-IV | R-CHOP | 2008–2011 | 2.42 | PFS |
| Ni | 2016 | China | 7 | 57 | 54(14–75) | I-IV | R-CHOP | 2009–2015 | 2.915 | OS, PFS |
| Wang | 2016 | China | 8 | 156 | NR | I-IV | R-CHOP | 2006–2015 | 3 | OS, PFS |
| Wang | 2017 | China | 9 | 355 | 54(18–86) | I-IV | R-CHOP | 2005–2011 | 2.81 | OS, PFS |
OS = overall survival; PFS = progression-free survival; R-CHOP = rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; NOS = Newcastle-Ottawa Scale, NR = not reported.
Table 2. Newcastle-Ottawa Scale for quality assessment of studies included in the meta-analysis.
| Study | Selection | Comparability | Outcome | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the nonexposed cohort | Assessment of exposure | Outcome not present at start | Assessment of outcome | Follow-up long enough for outcomes | Adequacy of follow-up | |||
| Porrata (2010) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Ho (2015) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Keam (2015) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Melchardt (2015) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Ming (2015) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | 7 | ||
| Hong (2016) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Ni (2016) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | 7 | ||
| Wang (2016) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Wang (2017) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
NLR and OS, PFS
Eight studies [12, 13, 17, 18, 26–29] with 1984 patients showed the relationship between NLR and OS in DLBCL. The heterogeneity tests suggested non-significant heterogeneity (I2 = 7.3%, PH = 0.374; Table 3). The pooled data showed that a high NLR significantly correlated with a worse OS (HR = 1.84, 95% CI = 1.52–2.22, p<0.001, Table 3, Fig 2). For further investigation, we conducted subgroup analysis. As shown in Table 3, the results demonstrated that NLR remained a significant prognostic marker regardless of ethnicity (Asian or Non-Asian), sample size (<200 or ≥200), and cut-off value (NLR ≤3 or NLR >3). In terms of NLR and PFS, the combined results from 7 studies[12, 17, 18, 25–27, 29] with 1731 patients showed that NLR was also a factor predicting worse PFS in DLBCL (HR = 1.64, 95% CI = 1.36–1.98, p<0.001; I2 = 36.9%, PH = 0.147, Table 3, Fig 2). Subgroup analysis demonstrated that NLR was still a prognostic biomarker regardless of study location, sample size, and cut-off. The results of meta-regression are shown in Table 3.
Table 3. Main results of meta-analysis.
| Outcome | Variables | No. of studies | Heterogeneity | Fixed-effects model | Random-effects model | Meta-regression | |||
|---|---|---|---|---|---|---|---|---|---|
| I2(%) | PH | HR (95%CI) | p | HR (95%CI) | p | p | |||
| OS | All | 8 | 7.3 | 0.374 | 1.84(1.52–2.22) | <0.001 | 1.85(1.52–2.26) | <0.001 | |
| Ethnicity | 0.424 | ||||||||
| Asian | 6 | 0 | 0.479 | 1.98(1.55–2.54) | <0.001 | 1.98(1.55–2.54) | <0.001 | ||
| Non-Asian | 2 | 54.9 | 0.136 | 1.66(1.24–2.22) | 0.001 | 1.72(1.1–2.69) | 0.017 | ||
| Sample size | 0.264 | ||||||||
| <200 | 4 | 12.5 | 0.33 | 2.37(1.52–3.72) | <0.001 | 2.45(1.49–4.02) | <0.001 | ||
| ≥200 | 4 | 0 | 0.458 | 1.74(1.41–2.14) | <0.001 | 1.74(1.41–2.14) | <0.001 | ||
| Cut-off | 0.326 | ||||||||
| ≤3 | 5 | 2.9 | 0.39 | 2.04(1.57–2.67) | <0.001 | 2.05(1.56–2.7) | <0.001 | ||
| >3 | 3 | 10 | 0.329 | 1.65(1.27–2.16) | <0.001 | 1.67(1.25–2.21) | <0.001 | ||
| PFS | All | 7 | 36.9 | 0.147 | 1.64(1.36–1.98) | <0.001 | 1.69(1.32–2.15) | <0.001 | |
| Ethnicity | 0.059 | ||||||||
| Asian | 6 | 0 | 0.612 | 1.5(1.23–1.84) | <0.001 | 1.5(1.23–1.84) | <0.001 | ||
| Non-Asian | 1 | - | - | 2.98(1.78–4.98) | <0.001 | 2.98(1.78–4.98) | <0.001 | ||
| Sample size | 0.564 | ||||||||
| <200 | 3 | 0 | 0.756 | 1.88(1.3–2.71) | 0.001 | 1.88(1.3–2.71) | 0.001 | ||
| ≥200 | 4 | 63.6 | 0.041 | 1.57(1.26–1.95) | <0.001 | 1.61(1.11–2.33) | 0.011 | ||
| Cut-off | 0.083 | ||||||||
| ≤3 | 5 | 0 | 0.526 | 1.47(1.18–1.82) | <0.001 | 1.47(1.18–1.82) | <0.001 | ||
| >3 | 2 | 39.5 | 0.199 | 2.39(1.62–3.51) | <0.001 | 2.35(1.43–3.88) | 0.001 | ||
Fig 2. Forest plots for the estimate of NLR associated with (A) OS and (B) PFS in the meta-analysis.
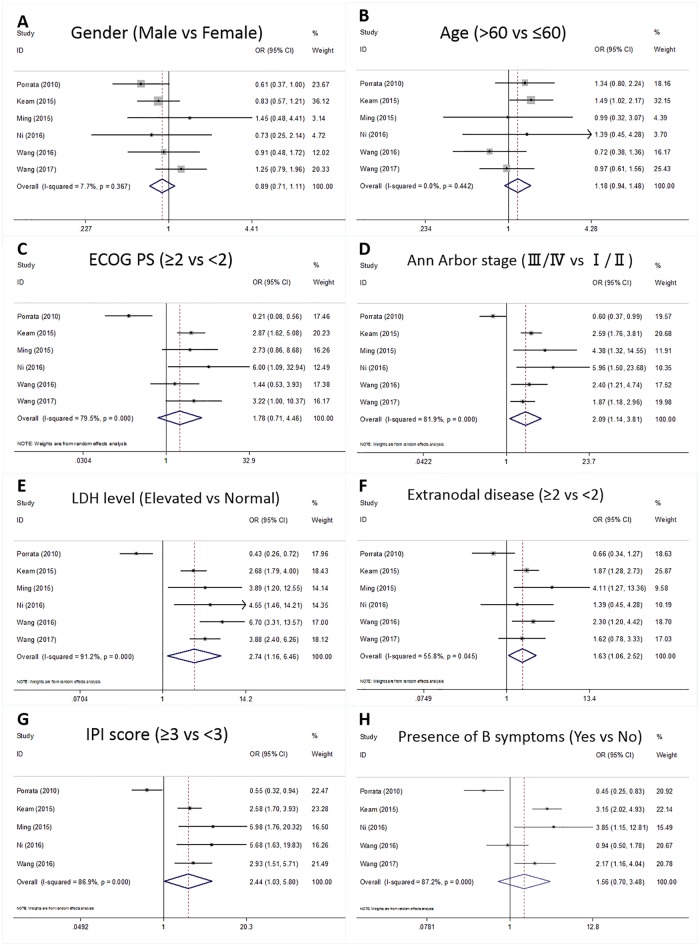
NLR and clinicalpathological features
We also comprehensively investigated the association between NLR and clinicopathological features. A total of 8 clinicopathological features were investigated, as follows: sex (male vs. female), age (>60 vs. ≤60 years), European Cooperative Oncology Group performance status score (ECOG PS; ≥2 vs. <2), Ann Arbor stage (III/IV vs. I/II), lactate dehydrogenase (LDH) level (elevated vs. normal), extranodal disease (≥2 vs. <2), IPI score (≥3 vs. <3), and presence of B symptoms (yes vs. no). The results are summarized in Fig 3. As shown in Fig 3, NLR was associated with Ann Arbor stage (OR = 2.09, 95% CI = 1.14–3.81, p = 0.017), LDH level (OR = 2.74, 95% CI = 1.16–6.46, p = 0.021), extranodal disease (OR = 1.63, 95% CI = 1.06–2.52, p = 0.027), and IPI score (OR = 2.44, 95% CI = 1.03–5.08, p = 0.043). However, NLR was found to have no significant association with sex (OR = 0.89, 95% CI = 0.71–1.11, p = 0.29), age (OR = 1.18, 95% CI = 0.94–1.48, p = 0.152), ECOG PS (OR = 1.78, 95% CI = 0.71–4.46, p = 0.217), or presence of B symptoms (OR = 1.56, 95% CI = 0.7–3.48, p = 0.278).
Fig 3. Forest plots for the association of NLR and (A) sex, (B) age, (C) ECOG PS, (D) Ann Arbor stage, (E) LDH level, (F) extranodal disease, (G) IPI score, and (H) presence of B symptoms in meta-analysis.
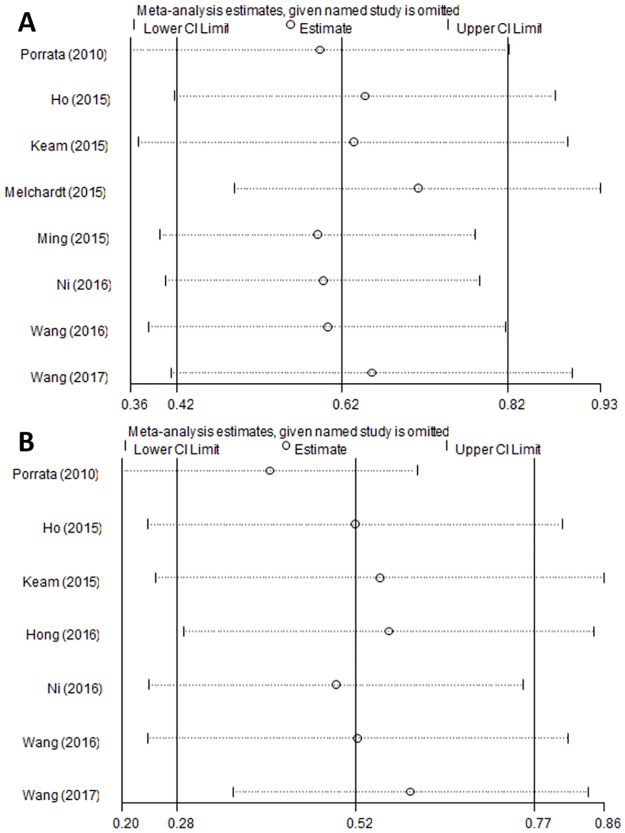
Sensitivity analysis
Sensitivity analysis was conducted by omitting one study at a time and analyzing the remaining studies. The results are shown in Fig 4, the results were not substantially changed, showing the reliability and stability of our results.
Fig 4. Sensitivity analysis for (A) OS and (B) PFS.
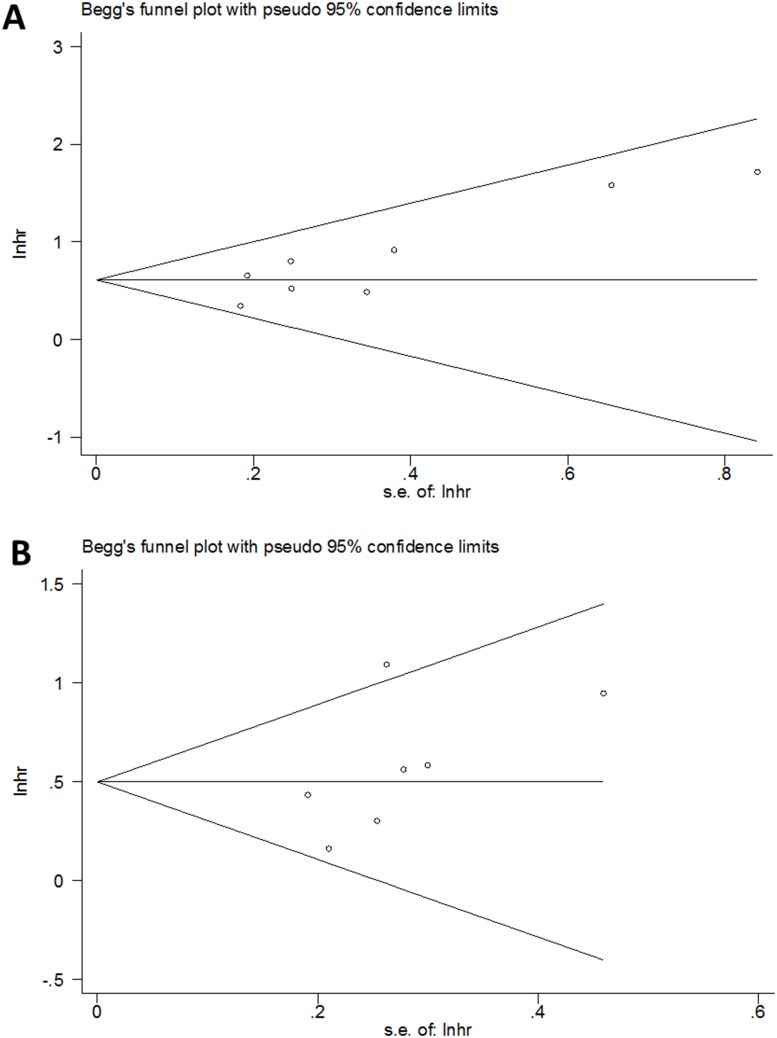
Publication bias
In this meta-analysis, we introduced Begg’s funnel plot to test publication bias. As shown in Fig 5, the results suggested no significant publication bias for OS (p = 0.063) and PFS (p = 0.133).
Fig 5. Begg’s test for (A) OS and (B) PFS.
Discussion
Prior studies have suggested that NLR is associated with worse survival outcomes in various cancers [30–35]. As for DLBCL, the prognostic role of NLR remains controversial, which may be due to the clinically heterogeneous features of this disease. In the current meta-analysis, we aggregated data from 9 studies including 2297 patients. The results showed that NLR was correlated with poor OS (HR = 1.84, 95% CI = 1.52–2.22, p<0.001) as well as worse PFS (HR = 1.64, 95% CI = 1.36–1.98, p<0.001). In addition, in the subgroup analysis stratified by location, sample size, and cut-off value, the prognostic value of NLR remained significant. Furthermore, NLR was also associated with Ann Arbor stage, LDH level, extranodal disease, and IPI score. The findings of this study suggest that NLR is a significant prognostic marker in DLBCL; additionally, because measurement of NLR is easy and inexpensive, NLR has potential to be validated in clinical practice for DLBCL patients.
A number of studies have shown that persistent chronic inflammation could trigger tumorigenesis [7, 36, 37]. Inflammatory responses could promote angiogenesis and protect cancer cells from immune attacks [36]. In the tumor microenvironment, neutrophils secrete a variety of cytokines including interleukin-2, interleukin-10, and tumor necrosis factor α, which further promote cancer development[38]. In contrast, lymphocytes are well known to exert dominant roles in immune defense against cancer cells [39]. Lymphocytes can induce cytotoxic cell death [40]. NLR has a biological rationale because it reflects the strength of immune responses in cancer patients. A variety of meta-analyses have shown the significant prognostic value of NLR in solid tumors including lung cancer[41], gastric cancer [42, 43], hepatocellular carcinoma [44], breast cancer [32], and renal cell carcinoma [30]. The results demonstrated that NLR was associated with poor survival in various tumors, which was in accordance with results in this meta-analysis. We also noted that a meta-analysis investigating the correlation between NLR and various solid tumors[16]; however, in this meta-analysis, only 1 study regarding Hodgkin’s lymphoma [45] was included for analysis, and DLBCL was not investigated. To the best of our knowledge, this is the first meta-analysis exploring the prognostic value of NLR in patients with DLBCL. We also noted that previous meta-analyses also showed that absolute lymphocyte count and lymphocyte/monocyte ratio were prognostic markers for DLBCL[46, 47]. Feng et al. revealed that low absolute lymphocytic count has an adverse effect on outcome in DLBCL [46]. This finding is in accordance with our results because low absolute lymphocytic count leads to high NLR when the neutrophil count is fixed.
Several limitations need to be pointed out in this study. First, the sample size was relatively small. Only 9 studies were included for analysis, especially for the association between NLR and clinical parameters. The small sample size may introduce bias. Second, cut-off values of NLR were inconsistent in primary studies, which suggests a need for a uniform cut-off value in further studies. Third, publication bias examination was suboptimal in detecting publications when the included studies were fewer than 10[48]. Only 9 studies were included in this meta-analysis, although Begg’s test suggested no significant publication bias. This could not rule out the possibility of publication bias because insufficient studies were included. Fourth, meta-regression was performed although meta-regression is most suitable for analyses that include >10 cohorts[49]. Eight studies were included for OS and 7 studies were for PFS; therefore, the results of meta-regression need to be treated with caution. Fifth, the confidence intervals for I2 were not reported, which could be useful for heterogeneity estimates[50].
In conclusion, this meta-analysis indicated that elevated NLR correlated with poor OS and poor PFS in patients with DLBCL. In addition, NLR was also strongly associated with Ann Arbor stage, LDH level, extranodal disease, and IPI score. The results suggested that NLR could be recommended as an inexpensive prognostic biomarker in clinical practice for DLBCL. However, due to the limitations mentioned above, further large-scale studies are needed to confirm our results.
Supporting information
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992–2001. Blood. 2006;107(1):265–76. Epub 2005/09/10. 10.1182/blood-2005-06-2508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher SG, Fisher RI. The epidemiology of non-Hodgkin's lymphoma. Oncogene. 2004;23(38):6524–34. 10.1038/sj.onc.1207843 [DOI] [PubMed] [Google Scholar]
- 3.Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. The New England journal of medicine. 2002;346(4):235–42. Epub 2002/01/25. 10.1056/NEJMoa011795 [DOI] [PubMed] [Google Scholar]
- 4.Sehn LH. Early detection of patients with poor risk diffuse large B-cell lymphoma. Leuk Lymphoma. 2009;50(11):1744–7. Epub 2009/10/29. 10.3109/10428190903308064 [DOI] [PubMed] [Google Scholar]
- 5.Ziepert M, Hasenclever D, Kuhnt E, Glass B, Schmitz N, Pfreundschuh M, et al. Standard International prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(14):2373–80. Epub 2010/04/14. [DOI] [PubMed] [Google Scholar]
- 6.Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403(6769):503–11. 10.1038/35000501 [DOI] [PubMed] [Google Scholar]
- 7.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. 10.1038/nature01322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schreiber RD, Old LJ, Smyth MJ. Cancer Immunoediting: Integrating Immunity's Roles in Cancer Suppression and Promotion. Science. 2011;331(6024):1565–70. 10.1126/science.1203486 [DOI] [PubMed] [Google Scholar]
- 9.Pinato DJ, Shiner RJ, Seckl MJ, Stebbing J, Sharma R, Mauri FA. Prognostic performance of inflammation-based prognostic indices in primary operable non-small cell lung cancer. Br J Cancer. 2014;110(8):1930–5. Epub 2014/03/29. 10.1038/bjc.2014.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: A decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–40. 10.1016/j.ctrv.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 11.Sun HL, Pan YQ, He BS, Nie ZL, Lin K, Peng HX, et al. Prognostic performance of lymphocyte-to-monocyte ratio in diffuse large B-cell lymphoma: an updated meta-analysis of eleven reports. OncoTargets and therapy. 2016;9:3017–23. 10.2147/OTT.S96910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Porrata LF, Ristow K, Habermann T, Inwards DJ, Micallef IN, Markovic SN. Predicting survival for diffuse large B-cell lymphoma patients using baseline neutrophil/lymphocyte ratio. Am J Hematol. 2010;85(11):896–9. Epub 2010/09/16. 10.1002/ajh.21849 [DOI] [PubMed] [Google Scholar]
- 13.Melchardt T, Troppan K, Weiss L, Hufnagl C, Neureiter D, Tränkenschuh W, et al. Independent prognostic value of serum markers in diffuse large B-cell lymphoma in the era of the NCCN-IPI. JNCCN Journal of the National Comprehensive Cancer Network. 2015;13(12):1501–8. [DOI] [PubMed] [Google Scholar]
- 14.Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014;110(10):2524–30. 10.1038/bjc.2014.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asano Y, Kashiwagi S, Onoda N, Noda S, Kawajiri H, Takashima T, et al. Platelet-Lymphocyte Ratio as a Useful Predictor of the Therapeutic Effect of Neoadjuvant Chemotherapy in Breast Cancer. PloS one. 2016;11(7):e0153459 Epub 2016/07/30. 10.1371/journal.pone.0153459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Journal of the National Cancer Institute. 2014;106(6):dju124 Epub 2014/05/31. 10.1093/jnci/dju124 [DOI] [PubMed] [Google Scholar]
- 17.Ho CL, Lu CS, Chen JH, Chen YG, Huang TC, Wu YY. Neutrophil/Lymphocyte Ratio, Lymphocyte/Monocyte Ratio, and Absolute Lymphocyte Count/Absolute Monocyte Count Prognostic Score in Diffuse Large B-Cell Lymphoma: Useful Prognostic Tools in the Rituximab Era. Medicine. 2015;94(24):e993 Epub 2015/06/20. 10.1097/MD.0000000000000993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keam B, Ha H, Kim TM, Jeon YK, Lee SH, Kim DW, et al. Neutrophil to lymphocyte ratio improves prognostic prediction of International Prognostic Index for patients with diffuse large B-cell lymphoma treated with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone. Leuk Lymphoma. 2015;56(7):2032–8. Epub 2014/11/11. 10.3109/10428194.2014.982642 [DOI] [PubMed] [Google Scholar]
- 19.Kong SY, Lee H, Sohn JY, Eom HS. Adverse prognostic impact of neutrophIL-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with diffuse large B cell lymphoma. Blood. 2014;124(21). [Google Scholar]
- 20.Spassov B, Balatzenko G, Vassileva D, Mihaylov G, Toshkov S, Guenova M. High neutrophil lymphocyte ratio at diagnosis identifies diffuse large B-cell lymphoma patients with poor clinical outcome. Haematologica. 2015;100:664. [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097 Epub 2009/07/22. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European journal of epidemiology. 2010;25(9):603–5. Epub 2010/07/24. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 23.Brockwell SE, Gordon IR. A comparison of statistical methods for meta-analysis. Stat Med. 2001;20(6):825–40. Epub 2001/03/17. 10.1002/sim.650 [DOI] [PubMed] [Google Scholar]
- 24.Kontopantelis E, Reeves D. Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: A simulation study. Statistical methods in medical research. 2012;21(4):409–26. Epub 2010/12/15. 10.1177/0962280210392008 [DOI] [PubMed] [Google Scholar]
- 25.Hong JY, Ryu KJ, Lee JY, Park C, Ko YH, Kim WS, et al. Serum level of CXCL10 is associated with inflammatory prognostic biomarkers in patients with diffuse large B-cell lymphoma. Hematological oncology. 2016. Epub 2016/12/13. [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Zhou M, Xu JY, Yang YG, Zhang QG, Zhou RF, et al. Prognostic role of pretreatment neutrophil-lymphocyte ratio in patients with diffuse large B-cell lymphoma treated with RCHOP. Medicine. 2016;95(38):e4893 Epub 2016/09/24. 10.1097/MD.0000000000004893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang J, Gao K, Lei W, Dong L, Xuan Q, Feng M, et al. Lymphocyte-to-monocyte ratio is associated with prognosis of diffuse large B-cell lymphoma: correlation with CD163 positive M2 type tumor-associated macrophages, not PD-1 positive tumor-infiltrating lymphocytes. Oncotarget. 2017;8(3):5414–25. Epub 2016/12/31. 10.18632/oncotarget.14289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ming Z, Yanli L, Zhitaa W, Qianshan T, Zhimin Z. Neutrophil to lymphocyte ratio and its relationship with the chemotherapy effect and the prognosis in patients with diffuse large B-cell lymphoma. Journal of Leukemia and Lymphoma. 2015;24(8):460–3. [Google Scholar]
- 29.Ni J, Wang YQ, Zhang YP, Wu W, Zeng QS, Yang MZ, et al. Value of Neutrophil/Lymphocyte Ratio and Platelet/Lymphocyte Ratio for Prognostic Evaluation of Diffuse Large B-cell Lymphoma. Journal of Experimental Hematology. 2016;24(2):427–32. Epub 2016/05/07. [DOI] [PubMed] [Google Scholar]
- 30.Hu K, Lou L, Ye J, Zhang S. Prognostic role of the neutrophil-lymphocyte ratio in renal cell carcinoma: a meta-analysis. BMJ open. 2015;5(4):e006404 Epub 2015/04/10. 10.1136/bmjopen-2014-006404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yin Y, Wang J, Wang X, Gu L, Pei H, Kuai S, et al. Prognostic value of the neutrophil to lymphocyte ratio in lung cancer: A meta-analysis. Clinics (Sao Paulo, Brazil). 2015;70(7):524–30. Epub 2015/07/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J, Deng Q, Pan Y, He B, Ying H, Sun H, et al. Prognostic value of neutrophil-to-lymphocyte ratio in breast cancer. FEBS open bio. 2015;5:502–7. Epub 2015/07/03. 10.1016/j.fob.2015.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun XD, Shi XJ, Chen YG, Wang CL, Ma Q, Lv GY. Elevated Preoperative Neutrophil-Lymphocyte Ratio Is Associated with Poor Prognosis in Hepatocellular Carcinoma Patients Treated with Liver Transplantation: A Meta-Analysis. Gastroenterology research and practice. 2016;2016:4743808 Epub 2016/02/26. 10.1155/2016/4743808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo Y, She DL, Xiong H, Fu SJ, Yang L. Pretreatment Neutrophil to Lymphocyte Ratio as a Prognostic Predictor of Urologic Tumors: A Systematic Review and Meta-Analysis. Medicine. 2015;94(40):e1670 Epub 2015/10/09. 10.1097/MD.0000000000001670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dong YW, Shi YQ, He LW, Su PZ. Prognostic significance of neutrophil-to-lymphocyte ratio in rectal cancer: a meta-analysis. OncoTargets and therapy. 2016;9:3127–34. Epub 2016/06/17. 10.2147/OTT.S103031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grivennikov SI, Greten FR, Karin M. Immunity, Inflammation, and Cancer. Cell. 2010;140(6):883–99. 10.1016/j.cell.2010.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. Epub 2011/03/08. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 38.Salazar-Onfray F, Lopez MN, Mendoza-Naranjo A. Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev. 2007;18(1–2):171–82. Epub 2007/03/03. 10.1016/j.cytogfr.2007.01.015 [DOI] [PubMed] [Google Scholar]
- 39.Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–48. Epub 2004/08/17. 10.1016/j.immuni.2004.07.017 [DOI] [PubMed] [Google Scholar]
- 40.Shi F, Shi M, Zeng Z, Qi RZ, Liu ZW, Zhang JY, et al. PD-1 and PD-L1 upregulation promotes CD8(+) T-cell apoptosis and postoperative recurrence in hepatocellular carcinoma patients. International journal of cancer Journal international du cancer. 2011;128(4):887–96. Epub 2010/05/18. 10.1002/ijc.25397 [DOI] [PubMed] [Google Scholar]
- 41.Gu XB, Tian T, Tian XJ, Zhang XJ. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysis. Scientific reports. 2015;5:12493 Epub 2015/07/25. 10.1038/srep12493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sun J, Chen X, Gao P, Song Y, Huang X, Yang Y, et al. Can the Neutrophil to Lymphocyte Ratio Be Used to Determine Gastric Cancer Treatment Outcomes? A Systematic Review and Meta-Analysis. PloS one. 2016;2016:7862469. Epub 2016/04/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang X, Zhang W, Feng LJ. Prognostic significance of neutrophil lymphocyte ratio in patients with gastric cancer: a meta-analysis. PloS one. 2014;9(11):e111906 Epub 2014/11/18. 10.1371/journal.pone.0111906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiao WK, Chen D, Li SQ, Fu SJ, Peng BG, Liang LJ. Prognostic significance of neutrophil-lymphocyte ratio in hepatocellular carcinoma: a meta-analysis. BMC Cancer. 2014;14:117 Epub 2014/02/25. 10.1186/1471-2407-14-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koh YW, Kang HJ, Park C, Yoon DH, Kim S, Suh C, et al. Prognostic significance of the ratio of absolute neutrophil count to absolute lymphocyte count in classic Hodgkin lymphoma. American journal of clinical pathology. 2012;138(6):846–54. Epub 2012/11/20. 10.1309/AJCPO46GFKGNXCBR [DOI] [PubMed] [Google Scholar]
- 46.Feng JH, Wang ZJ, Guo XP, Chen YY, Cheng YP, Tang YM. Prognostic significance of absolute lymphocyte count at diagnosis of diffuse large B-cell lymphoma: a meta-analysis. International journal of hematology. 2012;95(2):143–8. 10.1007/s12185-011-0993-6 [DOI] [PubMed] [Google Scholar]
- 47.Lin BC, Chen C, Qian Y, Feng JH. Prognostic role of peripheral blood lymphocyte/monocyte ratio at diagnosis in diffuse large B-cell lymphoma: a meta-analysis. Leukemia & Lymphoma. 2015;56(9):2563–8. [DOI] [PubMed] [Google Scholar]
- 48.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–29. Epub 2000/12/07. [DOI] [PubMed] [Google Scholar]
- 49.Li MX, Liu XM, Zhang XF, Zhang JF, Wang WL, Zhu Y, et al. Prognostic role of neutrophil- to- lymphocyte ratio in colorectal cancer: A systematic review and meta- analysis. International Journal of Cancer. 2014;134(10):2403–13. 10.1002/ijc.28536 [DOI] [PubMed] [Google Scholar]
- 50.Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ (Clinical research ed). 2007;335(7626):914–6. Epub 2007/11/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.