Abstract
Individuals with posttraumatic stress disorder (PTSD) have elevated rates of morbidity, and a sedentary lifestyle can cause and aggravate the physical health needs of adults with PTSD. The primary aim of this paper was to explore the impact of physical activity (PA) counseling (vs. usual care) on physical and psychological outcomes among individuals with PTSD. A secondary aim was to compare these arm effects between those with and without PTSD.
Methods
Older (>60 years) overweight veterans with impaired glucose tolerance were randomly assigned to an intervention or a usual care control arm. Of the 302 participants who underwent randomization, 67 (22%) had PTSD. Participants in the intervention arm received one in-person activity counseling session followed by regular PA telephone counseling over 12 months. Physical and psychological outcomes were assessed at baseline, 3, and 12 months.
Results
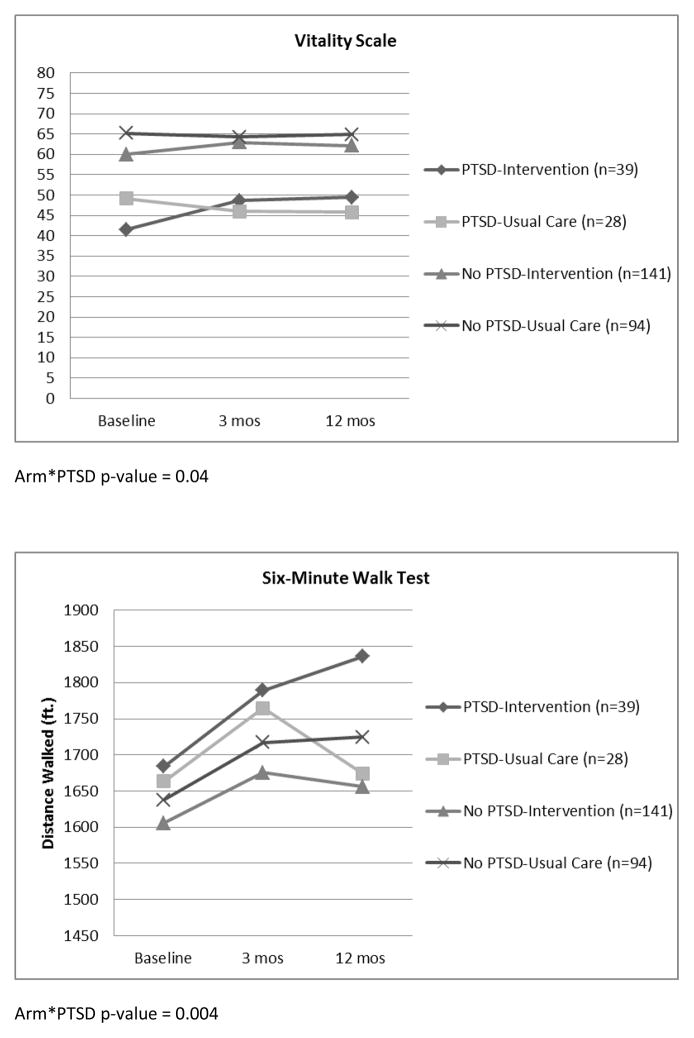
Primary Aim (intervention vs. usual care among those with PTSD): PA increased on average from 80 minutes/week to 161 minutes/week among participants in the intervention arm (p=0.01). Large, clinically meaningful improvements in six-minute walk test and psychological health were observed over the course of the intervention (p<0.01). Secondary Aim (PTSD/No PTSD, intervention/usual care): participants with PTSD responded equally well to the intervention compared to participants without PTSD, though we observed significantly greater improvements in vitality and six-minute walk compared to participants without PTSD (p<0.05).
Conclusions
Given the epidemic of comorbid psychological illness and lifestyle-related disease among persons with PTSD, our findings support development and implementation of targeted PA interventions in this high-risk population.
Keywords: Clinical, PTSD, RCT, Quality of Life, SF-36, Physical Function
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a mental health condition that is associated with dramatic societal and economic burden and is particularly common among U.S. military veterans. Compared to other veteran cohorts, older veterans (Vietnam War era) have among the highest rates of PTSD, with over 20% reporting PTSD symptoms (Marmar et al., 2015). The high and climbing prevalence of PTSD in this age group represents a significant public health concern as older veterans are the largest cohort served by the U.S. Department of Veterans Affairs (VA; National Center for Veterans Analysis and Statistics, 2016). This is also a public health consideration for non-VA healthcare systems, as approximately two-thirds of men over the age of 65 in the U.S. were military veterans in 2010 (Federal Interagency Forum on Aging-Related Statistics, 2012).
PTSD is often accompanied by comorbid anxiety, depressive, and substance use disorders (Galatzer-Levy, Nickerson, Litz, & Marmar, 2013). In addition to emotional pain, PTSD is also associated with a plethora of physical health conditions (e.g., respiratory, metabolic, cardiovascular disorders; (Levine, Levine, & Levine, 2014; Pacella, Hruska, & Delahanty, 2013) and neurocognitive conditions (e.g., dementia; (Yaffe et al., 2010), as well as functional impairment and pain (Hall et al., 2014; Pietrzak, Goldstein, Southwick, & Grant, 2012). In light of the significant comorbid mental health and physical health conditions associated with the disorder, PTSD can truly wreak havoc on the normal aging process. Indeed, these associations between PTSD and comorbid conditions are particularly strong in older age groups of veterans (Schnurr, Spiro, & Paris, 2000; Smith, Tyzik, Neylan, & Cohen, 2015), likely due, in part, to the cumulative effects of chronic PTSD and oftentimes decades of poor self-care.
In the last decade, the VHA has prioritized the dissemination of evidence-based psychotherapy for PTSD. While the development and dissemination of these empirically-supported psychotherapies represents an important positive step in the treatment of PTSD in later life, older veterans remain significantly less likely to engage in traditional psychotherapies (Elhai, Grubaugh, Richardson, Egede, & Creamer, 2008; Lu, Carlson, Duckart, & Dobscha, 2012). There is a substantial literature suggesting a strong link between PTSD and negative health behaviors, including high prevalence of tobacco use, substance use/dependence, medication non-adherence, sleep dysregulation, poor diet, and a lack of exercise (Gavrieli, Farr, Davis, Crowell, & Mantzoros, 2015; Hall, Hoerster, & Yancy, 2015; Zen, Whooley, Zhao, & Cohen, 2012), all of which contribute to poor chronic disease management and a higher likelihood of overweight and obesity. However, there is a dearth of research examining the treatment of obesity and/or metabolic syndrome in individuals with PTSD. Furthermore, individuals with psychological conditions have historically been excluded from health promotion interventions (Daumit et al., 2013).
There is growing appreciation of the need to address somatic PTSD comorbidities in addition to the psychiatric symptoms. This need to consider somatic comorbidities highlights a potential role for physical activity (PA). PA has demonstrated beneficial effects on both physical and psychological health (Penedo & Dahn, 2005). Despite these known benefits, rates of PA are extremely low among veterans with PTSD, with 67.5% not engaging in any regular PA (Chwastiak, Rosenheck, & Kazis, 2011), which is higher than veterans with other psychiatric diagnoses and the general population (Chwastiak et al., 2011; Hootman, Macera, Ham, Helmick, & Sniezek, 2003). As is the case with many other psychological conditions, many of the disease factors associated with PTSD (e.g., diabetes, hypertension) are linked to overweight/obesity, smoking, and unhealthy lifestyle, and interventions that target PA may represent promising approaches for reducing physical comorbidity and functional impairment among older adults with PTSD.
PA intervention studies in individuals with PTSD are sparse (Hall et al., 2015; Rosenbaum, Vancampfort, et al., 2015). In two pilot studies (Fetzner & Asmundson, 2015; Manger & Motta, 2005), positive effects of exercise on PTSD symptoms were reported; however, the impact on measures of physical health were not examined. The only randomized controlled exercise trial in adults with PTSD examined the efficacy of a 12-week program (a combination of supervised and non-supervised sessions) on psychological health and cardiometabolic risk factors among civilian patients hospitalized for treatment of PTSD (Rosenbaum, Sherrington, & Tiedemann, 2015). The authors reported that, in addition to mental health improvements, patients in the exercise intervention condition demonstrated significant improvements in physical health outcomes (i.e., body fat percentage, waist circumference, self-reported time spent sitting) within groups. However, each of these studies had significant methodological limitations such as very small sample sizes, limited to the inpatient setting, lack of control groups, or limited to younger adults.
The present study examined the impact of a randomized controlled 12-month telephone-based PA counseling trial (vs. usual care) in a sample of veterans from the Enhanced Fitness Study (Hall et al., 2011; Morey et al., 2012), a study of the effects of PA counseling in older overweight veterans. The primary aim of this paper was to explore the impact of PA counseling (vs. usual care) on physical and psychological outcomes among veterans with PTSD. A secondary aim was to compare these arm effects between those with and without PTSD (4 groups: PTSD/No PTSD, intervention/usual care).
METHODS
Participants and Procedure
The Enhanced Fitness study details are described in full detail elsewhere (Hall et al., 2011; Morey et al., 2012). Briefly, electronic medical records of all age-eligible individuals (≥60 years of age) from two large Department of Veterans Affairs (VA) clinics were prescreened for the following eligibility requirements: impaired fasting glucose (100–125 mg/dL), no diagnosis of diabetes mellitus, glycosylated hemoglobin of less than 7 percent, and body mass index (BMI) between 25 and 45 kg/m2. Individuals who exceeded current PA recommendations were excluded (n=54). Recruitment packets were mailed to 1,763 patients. Enrollment appointments were made for 561 (31.8%) potentially eligible individuals, of whom 302 (53.8%) were ultimately enrolled and randomized in the study. Sixty-seven of these participants had PTSD as determined by the electronic medical record. All participants provided written informed consent and the Durham Veterans Affairs Medical Center Institutional Review Board approved the research protocol.
Intervention Arm
The intervention was designed to help individuals reach a long-term goal of engaging in 30 or more minutes of aerobic exercise, preferably walking, ≥5 days/week, and 15 minutes of lower body strengthening exercises on 3 nonconsecutive days each week. The intervention has been described previously (Hall et al., 2011; Morey et al., 2012). Briefly, individuals assigned to the PA counseling arm received an in-person counseling consultation with a trained health counselor during which a progressive 2-week PA prescription was established. Individuals were given a packet of materials containing handouts on the health benefits of exercise, tips for exercising safely, a poster with specific exercises, elastic exercise bands of varying resistances, and a pedometer. The baseline counseling was supplemented with regular telephone counseling every 2 weeks for 6 weeks followed by monthly calls over the entire 1-year intervention period.
Usual Care Arm
Participants randomized to the usual care group received the standard of care as provided in their usual VA clinic. PA counseling by primary care providers as part of usual care varies considerably as there is no systematic assessment or mandate for PA counseling.
The VA has a national weight management program for veterans called “MOVE!,” a program that offers guidance on nutrition and PA. To ensure equal exposure to the MOVE! program across study participants, every randomized participant (regardless of arm) also received a referral to the MOVE! program, though it was ultimately up to the patients whether they participated in the MOVE! activities offered at the VA. Participation in MOVE! was queried at the 12-month in-person visit, and 16% of PA participants and 13% of UC participants reported initiating MOVE!.
Measures
Research staff blinded to intervention status assessed all study outcomes at baseline, 3 months, and 12 months. Assessment completion rates were similar across groups. Of the participants with PTSD, 91.0% (n=61) completed the assessments at 3 months and 89.5% (n=60) completed the assessments at 12 months, compared to 89.0% (n=209) and 86.5% (n=203) among those without PTSD, respectively.
PTSD
The electronic medical record (EMR) of each study participant was retrospectively reviewed for any documentation of PTSD (ICD-9 code 309.81). We also reviewed the “Active Problems” section of the EMR for inclusion of PTSD. Only those patients who had a PTSD diagnosis as indicated by the corresponding ICD-9 code and had this condition listed under “active problems” were categorized as such for this study.
Mental and Physical Health
Self-rated mental health and physical health were assessed using the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36; (Ware & Sherbourne, 1992). Mental health was assessed with the Mental Health Component Summary (MCS) score and four mental health-related subscales: Role-Emotional, Mental Health, Vitality, and Social Functioning. Self-rated physical health was assessed with the Physical Component Summary (PCS) score and the Physical Function subscale of the SF-36. Scale scores for all measures were standardized on a scale ranging from 0 to 100, with higher scores representing better health and functioning.
Cardiorespiratory Fitness
Aerobic endurance, a measure of cardiorespiratory fitness, was assessed using the six-minute walk test (6MWT; (Balke, 1963). This is a self-paced assessment in which individuals choose their own intensity of exercise, with the goal of walking as far as possible in 6 minutes. Greater distances walked reflect better aerobic endurance. This test has demonstrated excellent reliability and validity when compared with maximal oxygen uptake assessments in healthy older adults (Perera, Mody, Woodman, & Studenski, 2006).
Physical Activity
Minutes of moderate-intensity endurance PA was assessed with the Community Healthy Activities Model Program for Seniors (CHAMPS; (Stewart et al., 2001; Stewart et al., 1997). The CHAMPS questionnaire assesses the duration of a range of physical activities from which moderate activities can be separated. Minutes of moderate-intensity endurance PA were calculated as the sum of brisk walking, running/jogging, cycling/stationary cycle, and aerobic machine items from the CHAMPS.
Statistical Analysis
Primary Aim: Explore the Impact of PA counseling (vs. usual care) on physical and psychological outcomes among veterans with PTSD (N=67)
Mixed-models longitudinal trajectory analysis was used to explore change across three data points (baseline, 3-month, 12-month) among the 67 participants with PTSD randomized to PA counseling (n=39) vs. usual care (n=28). The baseline value of the particular outcome was entered as a covariate to adjust residual baseline differences between the groups at baseline. The statistical significance of the Time*Arm interactions were assessed. We initially specified an adjusted model including age, race, and depression. However, the effect of depression was not significant in any of the models as a main effect and inclusion of depression in the model did not substantially change the Arm parameter estimate. As a result we opted for a more parsimonious model that did not include depression.
For purposes of sufficiently powering future studies we also calculated 2 types of effect-size comparisons. First, intervention versus usual care post-intervention effect sizes were calculated as the intervention posttest mean minus the usual care posttest mean, divided by the pooled posttest standard deviation. Intervention pre-post effect sizes are within-group effect sizes for the arm effect over time. Second, a standardized mean difference (d) effect size was calculated for each outcome variable. A positive d reflects more favorable scores for the intervention arm at posttest. We interpreted the importance of the d using the benchmarks for “small effect size” (d=0.2), “medium effect size” (d=0.5), and “large effect size” (d=0.8) (Cohen, 1988).
Secondary Aim: Compare arm effects over time between those with and without PTSD in the entire study sample (N=302)
We examined longitudinal changes across all 4 study groups (PTSD/No PTSD, intervention/usual care) in the entire sample. Adjusted mixed-models longitudinal trajectory analysis was used to test a main effect for PTSD and a PTSD*Arm effect over time. Summary variables (propensity scores) were created using all measured baseline covariates to reflect the probability of each participant having a PTSD diagnosis. Propensity scores were dichotomized (yes/no) before being entered into the models and were used to account for the effect of covariates on the outcomes of interest. Propensity scores are a common data reduction method and we chose to use them here to save degrees of freedom in the model by adjusting for a single propensity score rather than multiple covariates. The baseline value of the particular outcome was entered as a covariate to adjust residual baseline differences between the groups at baseline. These models also adjusted for age, race and baseline propensity to have PTSD. Again, the effect of depression accounted for little of the variance, and was not included in the final model.
All analyses were conducted using IBM SPSS Statistics software version 21.0 and SAS version 9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
Characteristics of the entire Enhanced Fitness Study sample (N=302) are presented elsewhere (Morey et al., 2012). Briefly, this sample was predominantly Caucasian (70%), with an average age of 67 years (range 60–89). The BMI in this sample was in the obese range (31.2±3.6 kg/m2).
Characteristics of the 67 study participants with PTSD are presented in Tables 1 and 2. The average age of the sample was 63 years (range 60–79) and 40% of the sample had a high school degree or less. Physical health (mean score 40.5) and mental health (mean score 40.2) composite scores, obtained from the SF-36, were below average compared to the general population (Ware, 2001). Participants were at the 25th percentile in norms for 6-minute walk distance, indicating poor aerobic capacity for their age (Rikli & Jones, 1999). Comorbid depression was observed in over 50% of the PTSD sample. No significant differences were observed between the two study arms for any baseline characteristics.
Table 1.
Baseline Characteristics of Veterans with PTSD who Participated in the Enhanced Fitness Study by Study Arm (N=67)
| Characteristics | Intervention (n = 39) | Usual Care (n = 28) |
|---|---|---|
| Age, mean ± SD (range)b | 62.2 ± 2.8 (60–75) | 63.9 ± 4.9 (60–79) |
| White, n (%) | 21 (53.8) | 12 (42.9) |
| Male, n (%) | 37 (94.9) | 28 (100.0) |
| Some college education or trade school, n (%) | 23 (59.0) | 17 (60.7) |
| Number of comorbidities, mean ± SD | 4.2 ± 2.1 | 4.9 ± 2.4 |
| Body mass index (kg/m2), mean ± SD | 31.2 ± 3.9 | 31.4 ± 3.5 |
| Depression, n (%)a,b | 21 (53.8) | 18 (64.3) |
Note: No significant differences were observed between the two study arms for any variables. SD = standard deviation.
Diagnosis in the electronic medical record.
Significant differences PTSD vs. No PTSD, previously reported by Hall et al. (2014).
Table 2.
Group Means and Arm Effects over Time for All Outcomes among Participants with PTSD (N=67)
| Intervention
|
Usual Care
|
Difference within groups (follow-up minus baseline; SD)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Baseline (n = 39) | 3 Mos (n=33) | 12 mos (n=35) | Baseline (n=28) | 3 Mos (n=28) | 12 Mos (n=25) | Intervention | Usual care | Difference between groupsb |
| Physical activity, min/wk | 79.7(99.6) | 142.2(106.1) | 161.0(147.1) | 103.8(159.5) | 73.08(110.4) | 121.5(167.7) | +56.9(163.7)a
d=0.82 |
+18.5(177.4) | 59.3, P=0.012 d=0.35 |
|
| |||||||||
| Six-minute walk, ft | 1684.1(362.0) | 1789.1(382.6) | 1836.4(386.6) | 1663.2(349.7) | 1764.65(308.6) | 1674.0(371.7) | +142.7(212.4)a
d=0.42 |
−40.9(216.5) | 120.8, P=0.004 d=0.56 |
|
| |||||||||
| Self-rated mental health (SF-36) | |||||||||
|
| |||||||||
| MCS | 38.9(12.0) | 45.1(11.7) | 41.2(12.9) | 42.1(14.3) | 43.2(14.3) | 42.7(15.8) | +2.3(9.4)a
d=0.19 |
+0.6(8.5) | 2.80, P=0.15 d=0.31 |
|
| |||||||||
| Role- emotional | 35.0(41.8) | 55.5(43.8) | 47.6(40.6) | 47.6(48.4) | 53.8(43.3) | 49.3(47.2) | +8.9(35.2)a
d=0.30 |
+4.0(30.9) | 5.77, P=0.41 d=0.17 |
|
| |||||||||
| Mental health | 56.3(22.6) | 65.9(20.7) | 59.1(23.8) | 63.7(24.0) | 61.5(23.2) | 61.3(27.8) | +0.6(14.6) d=0.12 |
−0.8(13.7) | 4.76, P=0.10 d=0.34 |
|
| |||||||||
| Vitality | 41.5(19.5) | 48.6(19.1) | 49.4(21.9) | 49.1(21.8) | 46.0(25.0) | 45.8(23.6) | +4.1(15.3)a
d=0.40 |
−2.0(13.3) | 9.62, P=0.002 d=0.67 |
|
| |||||||||
| Social functioning | 59.0(25.1) | 67.8(24.6) | 62.5(27.1) | 55.8(30.1) | 58.6(25.4) | 55.0(33.6) | +2.3(22.1) d=0.14 |
+0.5(22.4) | 7.15, P=0.067 d=0.32 |
|
| |||||||||
| Self-rated physical health (SF-36) | |||||||||
|
| |||||||||
| PCS | 40.6(9.1) | 39.6(9.8) | 42.6(8.9) | 39.0(9.7) | 38.5(13.1) | 37.8(11.8) | +2.0(8.4) d=0.22 |
−1.2(7.4) | 1.55, P=0.31 d=0.19 |
|
| |||||||||
| Physical function | 63.2(25.3) | 63.9(25.4) | 68.6(24.6) | 63.0(26.4) | 58.4(28.6) | 57.6(27.6) | +2.4(21.7)a
d=0.21 |
−3.6(20.4) | 6.10, P=0.10 d=0.29 |
Values represent Mean(SD);
Significant time effect (p 0.10);
Adjusted for baseline value, age, and race;
d = effect size; MCS= Mental Health Component Score of the SF-36; PCS=Physical Health Component Score of the SF-36
A comparison of participants with and without PTSD on sociodemographic factors and other study variables at baseline was conducted previously (Hall et al., 2014). Those factors which differed significantly by PTSD status are indicated in Table 1. In summary, veterans with PTSD were significantly younger, were less likely to be White, and had significantly higher rates of depression compared to study participants without PTSD.
Primary Aim: Arm Effects over Time in Physical Performance and PA Outcomes among Participants with PTSD
The arm parameter estimates showed significant positive effects for minutes of PA (p = 0.012). PA increased significantly over time for the PTSD + intervention arm, from an average 80 minutes per week at baseline to an average 161 minutes per week at 12 months (+51%; d=0.82), in comparison with the PTSD + usual care arm, whose PA remained constant, from 104 minutes per week at baseline to 121 minutes per week at 12 months (p<0.05 for between-group difference) (Table 2). The observed increase in PA after the intervention compared with usual care had a small effect size (d=0.35).
The arm parameter estimates showed significant positive effects for six-minute walk distance (p = 0.004). Six-minute walk distance increased significantly over time for the PTSD + intervention arm, from an average 1,684 feet at baseline to an average 1,836 feet at 12 months (d=0.42), in comparison with the PTSD + usual care arm, whose walking distance remained constant, from 1,663 feet at baseline to 1,674 feet at 12 months (p<0.01 for between-group difference) (Table 2). Previous work has demonstrated that a cut-off of 1,950 feet during the six-minute walk test is the level of fitness needed by older adults to remain physically independent in later life (Rikli & Jones, 2013). The prevalence of individuals meeting this recognized fitness standard increased among those in the intervention arm from 28% at baseline to 42% at 12 months, compared to the usual care arm which went from 18% at baseline to 23% at 12 months. The observed improvement in six-minute walk distance after the intervention compared with usual care had a medium effect size (d=0.56).
Primary Aim: Arm Effects over Time in Health-Related Quality of Life among Participants with PTSD
Self-reports of health-related quality of life improved significantly over time on 3 of the SF-36 mental health scales for the PTSD + intervention arm: role-emotional health improved by an average 9 points from baseline to 12 months; vitality improved by an average of 4 points; and scores on the mental health component score improved by an average of 2 points among (ds=0.19–0.40). However, only vitality demonstrated significant between-group effects (p < 0.05), with the PTSD + intervention arm demonstrating greater improvement relative to PTSD + usual care (Table 2). We observed small declines over time in vitality among those in the usual care group, contributing to the between-group differences. The observed improvements in mental health, vitality, and social functioning after the intervention compared with usual care had small/medium effect sizes (ds=0.32–0.67).
Self-reports of physical function also significantly improved over time for the PTSD + intervention arm, by an average of 2 points (d=0.21), compared to PTSD + usual care, which declined an average of 4 points. The observed improvement in physical function after the intervention compared with usual care had a medium effect size (d=0.29). Self-rated physical health status was stable throughout the intervention period, demonstrating no significant changes over time or between groups.
Secondary Aim: Arm Effects between Participants with and without PTSD (PTSD/no PTSD, intervention/usual care)
We initially specified an adjusted model including age, race, depression, and baseline PTSD propensity score. A significant PTSD X Arm interaction was observed for the six-minute walk test (p < 0.01) and the Vitality scale of the SF-36 (p < 0.05). Figure 1 shows the six-minute walk and Vitality mean values by arm and PTSD status across Baseline, 3 months, and 12 months. We observed large improvements over time in the PTSD + intervention group for the six-minute walk test (d = 0.42), with little/no change observed amongst the other 3 groups (PTSD + usual care: d=0.15; No PTSD + intervention: d=0.12; No PTSD + usual care: d=0.23). For Vitality, we saw improvements among those in the intervention arms (PTSD + intervention: d=0.40; No PTSD + intervention: d=0.11) relative to usual care arms (PTSD + usual care: d=0.09; No PTSD + usual care: d=0.02). No significant interaction effects were observed for any of the other outcomes.
Figure 1.
DISCUSSION
This study shows that a relatively low-dose PA intervention was effective at improving leisure time PA, health-related quality of life, and functional performance in individuals with PTSD. This is in contrast to individuals with PTSD randomized to the usual care arm, whose scores remained stable or declined over the course of 12 months in the absence of a behavioral intervention. Veterans with PTSD in the intervention group reported gradual and significant gains in PA over the 12-month intervention period—on average 56 minutes per week—up to an average 160 minutes of total exercise per week. This increase also resulted in a greater prevalence of meeting the weekly goal of 150 minutes of moderate-intensity PA from 17% to 46% among those with PTSD (p < 0.01). This threshold is important as it reflects the amount of PA per week necessary to affect clinical health outcomes. Individuals with PTSD in this sample were largely sedentary at baseline and those in the intervention arm made steady progress in increasing PA throughout the activity counseling intervention. This is important, as reducing sedentary behaviors, independent of PA, has known cardiovascular, metabolic, and functional benefits in older adults (Wilmot et al., 2012).
The increase in PA observed among those with PTSD in the intervention arm was accompanied by significant improvements in the six-minute walk test. On average, this change over time roughly equates to moving from the 10th to the 25th percentile of age- and gender-based norms. The improvements we observed in the six-minute walk test reflect improvements in functional capacity, a clinically-meaningful indicator of physical reserve and resilience. The six-minute walk test is an objective measure and provides further validation of self-reported physical activity. We also observed significant positive effects of this low-dose PA intervention on health-related quality of life among individuals with PTSD. Despite improvements, mean scores of patients with PTSD were still below the age and sex matched norms in the general population on mental and social subscales. The benefit of PA interventions on physical and psychological health of older veterans with PTSD has not been fully explored; indeed, to our knowledge this is the first study to do so.
The older veterans with PTSD in this study benefitted across multiple domains. Although the parent study was not specifically designed to target individuals with PTSD, our results demonstrate that PTSD does not diminish the effect of PA counseling in this sample. That is, when we compared the longitudinal trajectories of the 4 study groups (PTSD/no PTSD, intervention/usual care), participants with PTSD responded the same as participants without PTSD. There was however, a significant moderating effect of PTSD on the six-minute walk test and vitality, driven largely by the positive gains observed in the PTSD + intervention group. These results are encouraging, for they suggest that individuals with PTSD are just as likely to benefit from PA counseling as individuals without PTSD, challenging the commonly held notion that this complex population with high physical and psychological comorbidity is intransigent.
Several issues require further investigation. Considered along the continuum of behavioral interventions, this study was relatively low-dose, requiring only 1 in-person counseling session, and using mail and telephone to deliver the intervention materials. Despite these efforts to reduce the burden of travel for study participants, the acceptability of this intervention appears to be low, ultimately enrolling only 17% of eligible patients contacted. Adherence to the home-based activity prescription cannot be verified, and is also noted as a study limitation. As discussed previously, the main study was not designed to target individuals with PTSD. Even so, we observed significant improvements in this sub-group. Future PA interventions that are tailored to individuals with PTSD and/or include a more intense exercise stimulus and design (i.e., supervised exercise) would likely report even more robust results and achieve a greater percentage of individuals meeting public health recommendations for PA for health promotion (Hoerster, Jakupcak, McFall, Unutzer, & Nelson, 2012). Finally, we recognize that this is an exploratory study with a small sample of individuals with PTSD. As such, future studies in larger populations are needed to fully assess these outcomes.
These data suggest a role for PA behavioral interventions as a vehicle for improving physical and psychological health outcomes among individuals with PTSD. It bears considering that PA interventions may be more palatable/approachable for older persons than traditional mental health therapies. We report that ten percent of veterans with PTSD in the intervention group withdrew from the study, while drop-out rates for evidence-based psychotherapy for PTSD are reportedly much higher ranging anywhere from 20–80% (Imel, Laska, Jakupcak, & Simpson, 2013; Najavits, 2015). PA programs for veterans with PTSD may also be of interest to clinicians and mental health providers alike, as both a primary and secondary prevention strategy. Exercise has demonstrated positive effects on physical and mental health outcomes including conditions that are highly comorbid with PTSD such as pain, functional impairment, sleep, and depression (Penedo & Dahn, 2005; Yang, Ho, Chen, & Chien, 2012). These comorbid conditions contribute to the substantial healthcare utilization observed in patients with PTSD. While the evidence-based cognitive behavioral treatments for PTSD have demonstrated efficacy for PTSD symptoms, these therapies are independent of lifestyle interventions which are needed to address the constellation of cardiometabolic disease risk factors that exist. Identifying evidence-based strategies to promote physical and psychological resilience in persons with chronic PTSD and integrating these services in both mental health and primary care clinics are public health priorities that warrant further consideration.
Acknowledgments
This study was funded by a VA Health Services Research and Development grant (IIR-06-252-3; Morey, PI) and National Institute on Aging grant AG028716. Drs. Hall and Hoerster are supported by Department of Veterans Affairs Career Development Awards (RR&D CDA 2RX001316 and HSR&D CDA 12-263, respectively). Dr. Bosworth is supported by a Department of Veterans Affairs Career Scientist Award (VA HSR&D 08-027). Drs. Hall and Morey and Mr. Sloane are supported by a National Institute on Aging Grant (AG028716). The funding sources had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the articles; and in the decision to submit it for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Balke B. A simple field test for the assessment of physical fitness. Report Cival Aeromedical Research Institute US. 1963;63:1–8. [PubMed] [Google Scholar]
- Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230–236. doi: 10.1016/j.psym.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DR. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, … Appel LJ. A behavioral weight-loss intervention in persons with serious mental illness. New England Jouranl of Medicine. 2013;368(17):1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Grubaugh AL, Richardson JD, Egede LE, Creamer M. Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans. Journal of Psychiatric Research. 2008;42(10):858–867. doi: 10.1016/j.jpsychires.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Federal Interagency Forum on Aging-Related Statistics. Washington, D.C: U.S. Government Printing Office; 2012. Older Americans 2012: Key Indicators of Well-Being. Retrieved from http://www.agingstats.gov/Main_Site/Data/2012_Documents/docs/EntireChartbook.pdf. [Google Scholar]
- Fetzner MG, Asmundson GJ. Aerobic Exercise Reduces Symptoms of Posttraumatic Stress Disorder: A Randomized Controlled Trial. Cognitive Behaviour Therapy. 2015;44(4):301–313. doi: 10.1080/16506073.2014.916745. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Nickerson A, Litz BT, Marmar CR. Patterns of lifetime PTSD comorbidity: a latent class analysis. Depression and Anxiety. 2013;30(5):489–496. doi: 10.1002/da.22048. [DOI] [PubMed] [Google Scholar]
- Gavrieli A, Farr OM, Davis CR, Crowell JA, Mantzoros CS. Early life adversity and/or posttraumatic stress disorder severity are associated with poor diet quality, including consumption of trans fatty acids, and fewer hours of resting or sleeping in a US middle-aged population: A cross-sectional and prospective study. Metabolism. 2015;64(11):1597–1610. doi: 10.1016/j.metabol.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Beckham JC, Bosworth HB, Sloane R, Pieper CF, Morey MC. PTSD is negatively associated with physical performance and physical function in older overweight military Veterans. Journal of Rehabilitation Research and Development. 2014;51(2):285–295. doi: 10.1682/JRRD.2013.04.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Hoerster KD, Yancy WS., Jr Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiologic Reviews. 2015;37:103–115. doi: 10.1093/epirev/mxu011. [DOI] [PubMed] [Google Scholar]
- Hall KS, Pieper CF, Edelman DE, Yancy WS, Jr, Lum H, Peterson MJ, … Morey MC. Lessons learned when innovations go awry: A baseline description of the Enhancing Fitness in Older Overweight Veterans with Impaired Glucose study. Translational Behavioral Medicine. 2011;1:573–587. doi: 10.1007/s13142-011-0075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerster KD, Jakupcak M, McFall M, Unutzer J, Nelson KM. Mental health and somatic symptom severity are associated with reduced physical activity among US Iraq and Afghanistan veterans. Preventive Medicine. 2012;55(5):450–452. doi: 10.1016/j.ypmed.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis & Rheumatology. 2003;49(1):129–135. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, Simpson TL. Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):394–404. doi: 10.1037/a0031474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine AB, Levine LM, Levine TB. Posttraumatic stress disorder and cardiometabolic disease. Cardiology. 2014;127(1):1–19. doi: 10.1159/000354910. [DOI] [PubMed] [Google Scholar]
- Lu MW, Carlson KF, Duckart JP, Dobscha SK. The effects of age on initiation of mental health treatment after positive PTSD screens among Veterans Affairs primary care patients. General Hospital Psychiatry. 2012;34(6):654–659. doi: 10.1016/j.genhosppsych.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Manger TA, Motta RW. The impact of an exercise program on posttraumatic stress disorder, anxiety, and depression. International Journal of Emergency Mental Health. 2005;7(1):49–57. [PubMed] [Google Scholar]
- Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, … Kulka RA. Course of Posttraumatic Stress Disorder 40 Years After the Vietnam War: Findings From the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry. 2015;72(9):875–881. doi: 10.1001/jamapsychiatry.2015.0803. [DOI] [PubMed] [Google Scholar]
- Morey MC, Pieper CF, Edelman DE, Yancy WS, Jr, Green JB, Lum H, … Taylor GA. Enhanced fitness: a randomized controlled trial of the effects of home-based physical activity counseling on glycemic control in older adults with prediabetes mellitus. Journal of the American Geriatrics Society. 2012;60(9):1655–1662. doi: 10.1111/j.1532-5415.2012.04119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM. The problem of dropout from "gold standard" PTSD therapies. F1000Prime Report. 2015;7:43. doi: 10.12703/P7-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics. Profile of Veterans: 2014. Data from the American Community Survey. United States Department of Veterans Affairs; 2016. Retrieved from http://www.va.gov/vetdata/report.asp. [Google Scholar]
- Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. Journal of Anxiety Disorders. 2013;27(1):33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Perera S, Mody S, Woodman R, Studenski SA. Meaningful change and responsiveness in common physical performanc measures in older adults. Journal of the American Geriatrics Society. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical health conditions associated with posttraumatic stress disorder in U.S. older adults: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American Geriatrics Society. 2012;60(2):296–303. doi: 10.1111/j.1532-5415.2011.03788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rikli RE, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60–94. Journal of Aging and Physical Activity. 1999;7(2):162–181. [Google Scholar]
- Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53(2):255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatrica Scandinavica. 2015;131(5):350–359. doi: 10.1111/acps.12371. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S, Vancampfort D, Steel Z, Newby J, Ward PB, Stubbs B. Physical activity in the treatment of Post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Research. 2015;230(2):130–136. doi: 10.1016/j.psychres.2015.10.017. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro A, 3rd, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychology. 2000;19(1):91–97. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- Smith BN, Tyzik AL, Neylan TC, Cohen BE. PTSD and obesity in younger and older veterans: Results from the mind your heart study. Psychiatry Research. 2015;229(3):895–900. doi: 10.1016/j.psychres.2015.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Medicine and Science in Sports and Exercise. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, Sepsis PG, King AC, McLellan BY, Roitz K, Ritter PL. Evaluation of CHAMPS, a physical activity promotion program for older adults. Annals of Behavioral Medicine. 1997;19(4):353–361. doi: 10.1007/BF02895154. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The Medical Outcomes Survey 36-item Short-Form Health Survey (SF-36): I. conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, … Biddle SJ. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, … Marmar C. Posttraumatic stress disorder and risk of dementia among US veterans. Archives of General Psychiatry. 2010;67(6):608–613. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang PY, Ho KH, Chen HC, Chien MY. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. Journal of Physiotherapy. 2012;58(3):157–163. doi: 10.1016/S1836-9553(12)70106-6. [DOI] [PubMed] [Google Scholar]
- Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: Findings from the Heart and Soul Study. Health Psychology. 2012;31(2):194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]