Stroke remains a leading cause of serious long-term disability,1 with most stroke survivors returning home under the care of family members who are often unprepared for the caregiving role, and lack training from healthcare providers.2,3 As a result, many stroke family caregivers experience burden, depressive symptoms, and reduced health-related quality of life.2,3 Aside from these individual issues, caregivers commonly experience interpersonal and organizational issues.2,3 Interpersonal issues reflect changes in relationships with the survivor and others, impacting roles and social activities.2 Organizational issues involve difficulty in finding resources and services.2
The American Heart Association/American Stroke Association published a scientific statement with evidence-based recommendations for stroke family caregiver and dyad interventions that are summarized in five main areas (Supplementary Table I).4 Dyad interventions were defined as those that targeted both the stroke survivor and the family caregiver, with both being active participants in the intervention.4 Intervention studies that involved family caregivers in the intervention, but did not target the health or well-being of the caregiver, were not considered to be dyad interventions.4 The recommendations were based upon a critical analysis of 17 caregiver and 15 dyad intervention studies found in the literature between January 1990 and October 2012.4 Because of the rapidly growing literature in this area, the purpose of this paper is to provide an update on the state of the evidence for stroke family caregiver and dyad interventions published between November 2012 and December 2016.
Methods
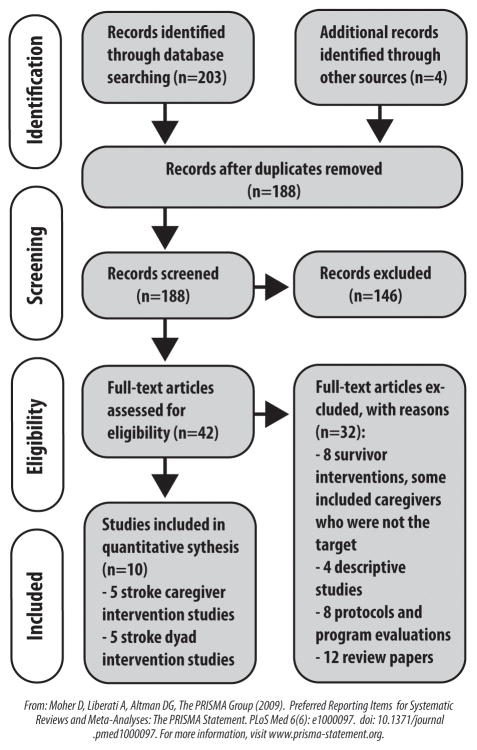
A critical analysis of published stroke family caregiver and dyad intervention studies was conducted using the following inclusion criteria: (a) written in the English language; (b) published from November 2012 through December 2016; (c) used a quasi-experimental or experimental research design; (d) involved a stroke caregiver or dyad intervention; (e) included stroke survivor or family caregiver outcomes; and (f) was implemented during any part of the stroke care continuum. Dissertations, books, and conference proceedings were excluded. As in the original statement,4 we searched MEDLINE, PubMed, CINAHL, and PsycINFO using the keywords stroke, family, caregiver, interventions, experimental studies, and quasi-experimental studies. Additional sources were located from reference lists of relevant articles. We tracked the search process using a PRISMA flow diagram (Figure 1).5 Articles meeting our inclusion criteria were abstracted into Supplementary Tables II and III. Consensus was reached on article inclusion by all authors. The studies were critiqued using criteria from the CONSORT and TREND statements,6,7 and assessed for threats to validity.8 Findings were compared with recommendations made in the original scientific statement.4
Figure 1.
PRISMA Flow Diagram.
Results
Based on our PRISMA flow diagram in Figure 1,5 we identified 10 studies9–18 that met our inclusion criteria (5 caregiver intervention studies;9–13 5 dyad intervention studies14–18).
Critique of the 10 articles
Designs
Six of the 10 studies were experimental designs that involved randomization of caregivers or dyads to intervention or control/usual care groups. 9,10,13,14,17,18 One large study used cluster randomization by unit.11 The remaining three studies were quasi-experimental (e.g., non-random assignment to condition12,16 or single group15).
Samples
Total sample sizes ranged from N=1915 to N=928.11 Five studies had sample sizes of less than 50.10,12,14,15,17 These studies should be interpreted with caution, particularly since small pilot studies do not provide meaningful effect size estimates for larger studies, let alone enough power for hypothesis testing.19 Some smaller studies reported statistically significant results, which could have resulted from Type I error.19 Likewise, non-significant findings could have resulted from Type II error.19 Small pilot studies are useful in testing feasibility of recruitment, retention, and implementation of the intervention, among other procedures; however, intervention effectiveness cannot be adequately determined in these studies.19 Four studies9,13,16,18 had moderate sample sizes ranging N=11916 to N=254,9 and one study was quite large (N=928).11
Interventions
Most studies provided detailed descriptions regarding the intervention, although one was unclear as to the actual number of sessions provided.11 Treatment fidelity (i.e., design, training of interveners, delivery, receipt, enactment)20 was described in only two studies,9,14 yet is an important factor in testing and reporting interventions.6,20
Outcomes
Outcomes were assessed with measures that had evidence of reliability and validity, although some studies used modified scales or single items.14,15,17,18 Outcomes are further detailed in Supplementary Table IV.
Generalizability
One study limited enrollment to spousal dyads.18 The rest included all types of informal caregivers, such as family and or friends. Recruitment setting and stage of recovery ranged from inpatient/acute/early discharge9–12,16 to those who had used “adult daycare services” for at least 12 months.15 One study included caregivers of survivors who were between six months and 5 years post stroke.13 Two studies included caregivers of survivors who were 60 years of age or older,13,15 resulting in limited generalizability for survivors who are in early to mid-life and experiencing the unique stressors that accompany those life stages.21 Six countries were represented (USA,9,14,18 Canada,10 UK,11 Germany,12,13 Netherlands,16 Korea15,17), many with drastically different healthcare systems and cultural norms around illness recovery and caregiving, raising further questions about generalizability; however, these studies provide a more global perspective.
What types of family caregiver and dyad interventions are best?
Target of interventions
The recommendation that caregiver interventions are preferred for caregiver outcomes and that dyad interventions are preferred for survivor outcomes is supported by the studies reviewed. For example, three of the caregiver studies did not measure survivor outcomes,9,10,13 and the two that did,11,12 did not find significant results. All of the dyad intervention studies reported at least one significant caregiver outcome; however, most were primarily targeted toward the survivor with positive survivor outcomes.14–18
Types of interventions
Six of the intervention studies employed a combination of skill building and psycho-educational strategies,9,11–14,18 whereas four studies used psycho-educational strategies alone.10,15–17 Recommendations from the original scientific statement emphasized the importance of using a combination of skill-building and psycho-educational interventions.4 Skill-building strategies focus on processes such as problem solving, stress management, goal setting, or hands on training.4 Psycho-educational interventions involve the provision of information about stroke.4 Support interventions facilitate interactions with peers for support and advice (e.g., support groups, online discussion forums).4 None of the 10 studies used support interventions as defined here; however, evidence is lacking regarding the effectiveness of these types of interventions.4
Intervention delivery design
Nine of the 10 studies used tailored approaches based on individual assessment of participant needs.9–11,13–18 This is important because evidence indicates that “one-size-fits all” type interventions are not as effective.4 Interventions that are tailored or individualized based on stroke caregiver needs should be chosen, and individual interventions are probably recommended over group sessions.4
Mode of delivery
Most interventions used face to face delivery,11,12,15,16,18 or a combination of face to face and telephone,10,13 with two studies being delivered completely by telephone.9,14 These studies adhere to recommendations from the original scientific statement for face to face and/or telephone interventions. One study was delivered via the web.17 The current lack of web-based interventions is noteworthy, considering the increase in technology use among a wide variety of family caregivers.22
Frequency of sessions
The total number of sessions ranged from one self-directed session10 to an unlimited number of sessions,12 with the number of sessions being unclear in one study.11 Current recommendations are for 5 to 9 sessions.4 Studies that fell within 5 to 9 sessions9,10,16,17 reported positive caregiver or survivor outcomes; however, so did those that reported having 12 to 20 sessions.13–15,18 The two studies that had an unlimited number of sessions,12 or where the number of sessions were unclear,11 were not as successful.
Discussion and Conclusions
Best designed studies
Out of the 10 studies reviewed, three were deemed the best designed studies based on their randomized controlled design and adequate sample size.9,13,18 While two of these studies used mailed information control groups,13,18 Bakas and colleagues9 employed an attention control group that received the same number of contacts from nurses as the intervention group, addressing an important threat to validity.8,9 This study also reported details regarding treatment fidelity,9,20 and incorporated more than one type of skill-building as part of the intervention.9
Studies with small sample sizes 10,12,14,15,17 teach us a great deal about feasibility of recruitment, implementation of the intervention, and preliminary data trends. It was fascinating that the largest study (N=928)11 reported no significant findings, although they only had two outcomes: survivor ADLs and caregiver burden. The authors admitted challenges in implementing a large multi-site study.11 Furthermore, the number of sessions provided to caregivers was uncertain, and attention to treatment fidelity was likely compromised. Cluster randomization by site could have also influenced the results.
Comparison of findings with recommendations
Overall, the recommendations in the original scientific statement4 (Supplementary Table I) were supported by the findings in these 10 studies published between November 2012 and December 2016. Studies should include measures of survivor outcomes when testing caregiver interventions to demonstrate the benefits of these interventions on the survivor. Dyad interventions could be better designed in the future to provide more emphasis on the health and well-being of the family caregiver. Most of the dyad interventions reviewed placed a majority of emphasis on how to care for the stroke survivor, rather than how to take care of oneself as a family caregiver. Consistent with current recommendations,4 most interventions are incorporating skill-building strategies in addition to providing psycho-education, while providing more tailored or individualized approaches to meet assessed needs of survivors and caregivers. While most interventions continue to be delivered face to face or by telephone, it is likely that more web-based or technologically enhanced approaches will emerge over the coming years.22
Supplementary Material
Supplementary Table I. Summary of recommendations for stroke caregiver and dyad interventions.4
Supplementary Table II. Summary of 5 articles testing family caregiver interventions.
Supplementary Table III. Summary of 5 articles testing dyad interventions.
Supplementary Table IV. Summary of survivor and caregiver outcomes.
Take Home Points.
Several recommendations exist for designing and testing stroke caregiver and dyad interventions4 that continue to be supported by this updated review.
A careful critique of existing intervention studies is needed to best evaluate the evidence in this area.
Future studies with more rigorous designs and larger sample sizes are needed, along with interventions that focus more on the health and well-being of the family caregiver.
Web-based and other technology-enhanced modes of delivery should be offered to meet the changing needs of technologically diverse caregivers.22
Footnotes
Disclosures
Dr. Bakas has received prior stroke family caregiver research funding from the National Institutes of Health, National Institute of Nursing Research, R01NR010388.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Grant JS, Hunt CW, Steadman L. Common caregiver issues and nursing interventions after a stroke: State-of-the-science nursing review. Stroke. 2014;45:e151–e153. doi: 10.1161/STROKEAHA.114.005094. [DOI] [PubMed] [Google Scholar]
- 3.Miller EL, Murray L, Richards L, Zorowitz RD, Bakas T, Clark P, et al. Comprehensive Overview of Nursing and Interdisciplinary Rehabilitation Care of the Stroke Patient: A Scientific Statement From the American Heart Association. Stroke. 2010;41:2402–2448. doi: 10.1161/STR.0b013e3181e7512b. [DOI] [PubMed] [Google Scholar]
- 4.Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller EL American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. Evidence for stroke family caregiver and dyad interventions: a statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke. 2014;45:2836–2852. doi: 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT Statement to Randomized Trials of Nonpharmacologic Treatment: Explanation and Elaboration. Ann Intern Med. 2008;148:295–W259. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]
- 7.Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94:361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston: Houghton Mifflin Company; 2002. [Google Scholar]
- 9.Bakas T, Austin JK, Habermann B, Jessup NM, McLennon SM, Mitchell PH, et al. Telephone Assessment and Skill-Building Kit for Stroke Caregivers: A randomized controlled clinical trial. Stroke. 2015;46:3478–3487. doi: 10.1161/STROKEAHA.115.011099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cameron JI, Maglie G, Green TL, Gignac MAM, Bayley M, Huijbregts M, et al. A feasibility and pilot randomized controlled trial of the “Timing it Right Stroke Family Support Program”. Clinical Rehabilitation. 2015;29:1129–1140. doi: 10.1177/0269215514564897. [DOI] [PubMed] [Google Scholar]
- 11.Forster A, Dickerson J, Young J, Patel A, Kalra L, Nixon J, et al. A structured training programme for caregivers of inpatients after stroke (TRACS): a cluster randomised controlled trial and cost-effectiveness analysis. Lancet. 2013;382:2069–2076. doi: 10.1016/S0140-6736(13)61603-7. [DOI] [PubMed] [Google Scholar]
- 12.Hirsch O, Leyh J, Karch C, Ferlings R, Schafer D. Impact of a training program for caregivers of neurological patients on depression, prostration, and subjective burden. Journal of Neuroscience Nursing. 2014;46:97–105. doi: 10.1097/JNN.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 13.Pfeiffer K, Beische D, Hautzinger M, Berry JW, Wengert J, Hoffrichter R, et al. Telephone-based problem-solving intervention for family caregivers of stroke survivors: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82:628–643. doi: 10.1037/a0036987. [DOI] [PubMed] [Google Scholar]
- 14.Bishop D, Miller I, Weiner D, Guilmette T, Mukand J, Feldmann E, et al. Family intervention: Telephone tracking (FITT): A pilot stroke outcome study. Top Stroke Rehabil. 2014;21(Suppl I):S63–S74. doi: 10.1310/tsr21S1-S63. [DOI] [PubMed] [Google Scholar]
- 15.Chang AK, Park Y, Fritschi C, Kim MJ. A family involvement and patient-tailored health management program in elderly Korean stroke patients’ day care centers. Rehabilitation Nursing. 2015;40:179–187. doi: 10.1002/rnj.95. [DOI] [PubMed] [Google Scholar]
- 16.Fens M, van Heugten CM, Beusmans G, Metsemakers J, Kester A, Limburg M. Effect of a stroke-specific follow-up care model on the quality of life of stroke patients and caregivers: A controlled trial. J Rehabil Med. 2014;46:7–15. doi: 10.2340/16501977-1239. [DOI] [PubMed] [Google Scholar]
- 17.Kim J, Lee S, Kim J. Effects of a web-based stroke education program on recurrence prevention behaviors among stroke patients: A pilot study. Health Education Research. 2013;28:488–501. doi: 10.1093/her/cyt044. [DOI] [PubMed] [Google Scholar]
- 18.Ostwald SK, Godwin KM, Cron SG, Kelley CP, Hersch G, Davis S. Home-based psychoeducational and mailed information programs for stroke-caregiving dyads post-discharge: a randomized trial. Disabil Rehabil. 2014;36:55–62. doi: 10.3109/09638288.2013.777806. [DOI] [PubMed] [Google Scholar]
- 19.Leon AC, Davis LL, Kraemer HC. The role and implementation of pilot studies in clinical research. J Psychiatr Res. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Czajkowski S, Breger R, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psych. 2005;73:852–860. doi: 10.1037/0022-006X.73.5.852. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy MJ, Sucharew HJ, Alwell K, Moomaw CJ, Woo D, Flaherty ML, et al. Age, subjective stress, and depression after ischemic stroke. J Behav Med. 2016;39:55–64. doi: 10.1007/s10865-015-9663-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chi NC, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015;21:37–44. doi: 10.1177/1357633X14562734. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I. Summary of recommendations for stroke caregiver and dyad interventions.4
Supplementary Table II. Summary of 5 articles testing family caregiver interventions.
Supplementary Table III. Summary of 5 articles testing dyad interventions.
Supplementary Table IV. Summary of survivor and caregiver outcomes.