Abstract
Objective
This study was designed to compare weight loss with a traditional behavioral treatment approach (BT), an approach that integrated skills for managing the obesogenic food environment (BT+E), and an approach that integrated environmental and acceptance-based skills (BT+EA). Moderators were examined as an exploratory aim.
Methods
Adults (n =283) were randomly assigned to treatment condition and provided with 26 group-based sessions over the course of 12 months. Weight was measured in the clinic at months 0, 6, and 12.
Results
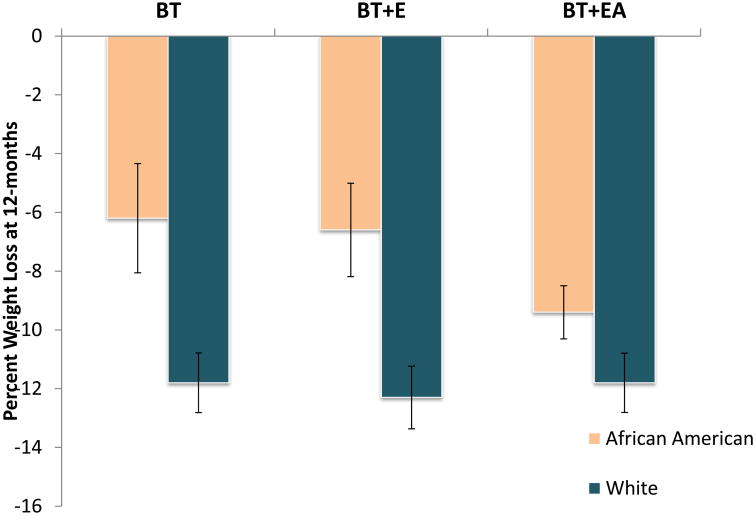
Change in weight over time did not significantly differ by condition. However, race significantly moderated the effect of condition on weight loss (p= .04), such that African-American participants lost less weight than non-Hispanic white participants in the BT (6.2% vs. 11.5%) and BT+E conditions (6.6% vs. 12.2%), but weight loss in these two groups was similar in the BT+EA condition (9.4% vs. 11.5%). Among African-Americans, rates of achieving a clinically significant weight loss (i.e., >5%) at 12 months were higher in BT+EA (80%) than BT (57%) or BT+E (48%) (p = .04).
Conclusions
This innovative behavioral approach shows promise for treatment of African-Americans, which is notable given the lack of progress to date addressing racial disparities in obesity intervention efficacy.
Keywords: weight loss, race, behavioral therapy, obesity
Introduction
Behavioral treatment (i.e., lifestyle modification) is one of the most powerful tools available for treating obesity.1 Continuing to refine and improve the efficacy of behavioral treatment is important because a sizable proportion of individuals do not experience clinically significant short-term benefits,2 and the majority of participants regain lost weight in the long-term.3 Adherence to the dietary intake and physical activity prescriptions necessary for weight control is exceptionally difficult due to the interaction of biological (e.g., appetitive drive and metabolic efficiency) and environmental factors (e.g., omnipresence of high-calorie food and energy-saving devices).4 Resisting powerful drives to consume more calories and expend less energy than necessary requires a great deal of self-regulation effort and skill.4
Treatment may attempt to facilitate adherence to a healthy lifestyle by engineering the environment such that the temptation for lapses in diet or physical activity is minimized, thus requiring fewer self-regulatory resources. An intervention that targets environmental challenges might position participants to engineer the modifiable aspects of their households and other settings such that limiting calorie intake (and, secondarily, engaging in physical activity) becomes easier and more automatic, ultimately reducing self-regulatory demands.5-7 Previous research has shown some evidence for the effectiveness of this approach,8 but is limited.
An alternate framework for addressing the challenges of self-regulation of weight in the modern environment may operate from the assumption that biological and environmental challenges can never be fully prevented or managed. As such, it may be especially valuable for participants to learn skills for engaging in value-driven behaviors despite the challenging internal experiences that will likely occur throughout the course of lifestyle modification (e.g., perceived loss of pleasure, behavioral fatigue, etc.).9 Acceptance-based behavioral treatment represents one such approach to teaching these skills.10, 11 This weight control approach has produced promising findings in a small body of literature, included one clinical trial that demonstrated superior efficacy compared to standard behavioral treatment.12-14 However, no previous work has tested the hypothesis that participants' ability to achieve and maintain weight loss may be improved if they are provided with a version of behavioral treatment that integrates 1) tools for engineering the home environment, which should reduce the need to rely on self-regulatory resources, and 2) an acceptance-based approach to uncomfortable internal experiences, which should strengthen the ability to engage in desirable weight control behaviors even when biological and environmental factors make doing so difficult.
The primary aim of this study was to compare the efficacy of three versions of behavioral treatment in a randomized clinical trial: traditional behavioral treatment (BT), behavioral treatment that integrated skills for managing the obesogenic environment (BT+E), and behavioral treatment that integrated both environmental and acceptance-based skills (BT+EA). Given previous research demonstrating heterogeneity in response to behavioral treatment, moderators also were of interest.2 As an exploratory aim, several demographic moderators of treatment efficacy were tested (i.e., race, sex, and education).
Methods
Participants
Participants were 283 adults recruited from the community through radio, newspaper, local websites, and postcards. Outlets that were expected to reach a racially diverse audience were targeted. (A priori power analyses indicated that 297 participants would provide > 80% power to detect a medium effect size.) Inclusion criteria were as follows: BMI of 27 to 45 kg/m2; age 18 to 70 years; ability to engage in physical activity; completion of a 7-day food diary and two pre-randomization screening/assessment visits. Exclusion criteria included medical or psychiatric condition that may have limited ability to comply with the behavioral recommendations of the program or posed a risk to the participant during weight loss; pregnancy; recently began a course of or changed the dosage of medication that could cause significant change in weight; current or planned participation in another weight loss program. Written informed consent was obtained from all participants upon enrollment. The study was approved by the Drexel University institutional review board.
Study Design
Participants were randomly assigned to one of three treatments: 1) standard BT, 2) BT with a primary focus on learning skills to modify the home environment in order to support weight loss efforts (BT+E), or 3) an acceptance-based version of behavioral treatment that also included skills for modifying the home environment (BT+EA). Across conditions, treatment sessions were held weekly in Months 1-4, biweekly in Months 5-6, and monthly in Months 7-12, for a total of 26 sessions. Participant assessments were completed at baseline, 6 months (mid-treatment), and 12 months (i.e., end of treatment). Percent weight loss was the primary outcome.
All treatment was delivered in 75-minute sessions in closed groups, with 10-14 participants per group. Groups were held in a research clinic on a university campus. Group composition was mixed in terms of sex and race. Clinicians held a master's or doctoral degree in psychology and had previous experience conducting behavioral weight loss interventions. Sessions were audio-recorded and 10% of recordings were rated for fidelity, such that each segment of the session was compared to the treatment manual and rated on a 10-point scale ranging from 1 to 10, in which 1 equaled “no adherence to treatment manual” and 10 equaled “perfect adherence to treatment manual.”
Treatment Conditions
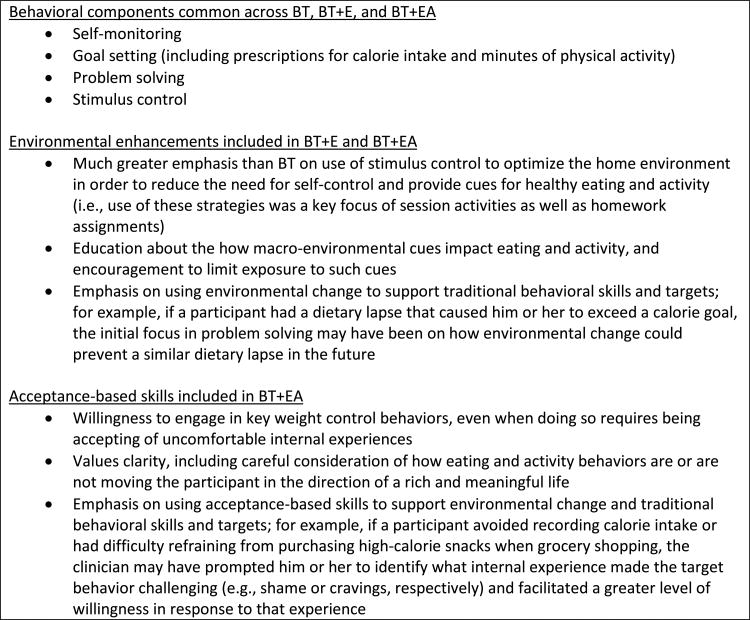
Standard behavioral treatment (BT)
The BT intervention was adapted from the Look AHEAD15 and the Diabetes Prevention Program protocols.16 Self-monitoring of calorie intake, physical activity, and weight was a core skill. Participants also learned to identify triggers for overeating; set specific goals for calorie intake, physical activity, and associated behaviors; use problem solving skills as a way of overcoming obstacles to behavior change; develop social support for behavior changes; and use relapse prevention techniques to prepare for lapses, anticipate challenges, and develop strategies for addressing them. Of note, reflecting standard practice, stimulus control techniques were taught in BT but were not a primary focus of session activities or participant assignments outside of session. In all conditions, participants were given calorie goals based on weight, in accordance with standard balanced deficit diet guidelines, and were instructed to gradually increase their physical activity until they reached an ultimate goal of at least 250 minutes per week of moderate activity.
Behavior therapy + environmental change (BT+E)
In the BT+E condition, participants learned all of the core BT skills, as shown in Figure 1. However, the session content associated with these standard activities and discussions in session was reduced to allow sufficient time for other treatment components. The primary focus of BT+E was learning how to modify the home environment (or other settings in which the participant could make changes, such as the workplace) in a way that would facilitate healthy eating. Treatment strategies emphasized reducing the availability of foods that promote overconsumption (e.g., through “Cabinet Cleanouts”) and increasing the availability of foods that were likely to facilitate weight control (e.g., pre-portioned foods, fruits and vegetables).8 Secondarily, participants learned how to modify the home environment in a way that would promote physical activity (e.g., increasing cues for exercise in the home). They also learned to navigate the macro-environment in a way that reduced the need for self-control (e.g., rather than buying coffee each morning from a store in which donuts were prominently displayed, make coffee at home or order from a drive-thru window).
Figure 1.
Summary of treatment components.
Acceptance-based behavior therapy + environmental change (BT+EA)
In the BT+EA condition, participants were taught core BT skills and learned to make key modifications to the home environment, but the time devoted to these activities was abbreviated so that there was ample opportunity to teach acceptance-based skills. Acceptance-based skills were designed to facilitate greater adherence to behavioral and environmental targets. Participants were encouraged to adopt a stance of acceptance towards uncomfortable internal experiences encountered as part of weight loss efforts (e.g., feeling an urge to buy a bag of potato chips in the grocery store or having the thought that watching television after dinner would be more enjoyable than going for a walk). Willingness was framed as a skill that positions individuals to choose behaviors that are consistent with their values and long-term goals (e.g., refrain from buying chips; go for the walk after dinner), regardless of how pleasurable or uncomfortable these behaviors may feel in the short-term. Discussions and exercises were used to develop greater clarity about what is most important in one's life. Ultimately, treatment was designed to enhance psychological flexibility, so that individuals could choose values-driven behavior, rather than allowing transient internal experiences to dictate eating and activity choices
Measurement
Weight and height
Anthropometric measurements included body weight using a Seca® scale accurate to 0.1 kg (measured in street clothes) and height using the built-in height rod. Height in meters and weight in kilograms were measured at each assessment point, and weight also was measured at each treatment session.
Weight-related covariates
At baseline, participants self-reported their highest weight since reaching adult height. Weight suppression was measured as the absolute difference between this weight and an individual's weight at baseline.17 Participants who were currently at their highest weight had weight suppression values of zero. Weight suppression significantly predicted 12-month weight loss in this sample (p = .04), such that those with more weight suppression lost less weight, consistent with previous research demonstrating that weight change over time can be predicted by previous highest weight or weight suppression.18-20 In addition, early weight loss was calculated as change in weight during the first four weeks of treatment, a time during which participants across conditions were learning the same core behavioral skills. Weight at the beginning of session 5 was imputed using the last available weight measurement for individuals who were not present at this session.
Weight control behaviors
Minutes of moderate-to-vigorous physical activity were measured with GT3X accelerometers worn for 7 days at each assessment point. Calorie intake was measured with 24-hour food recalls administered by registered dieticians at pre- and post-treatment (data were collected for three days at each time point).
Self-report measures
Participants completed a demographic questionnaire that included sex, race, and education level. Measures of self-efficacy (Weight Efficacy Lifestyle Questionnaire21), autonomous motivation (Treatment Self-Regulation Questionnaire22), and uncontrolled eating (Three-Factor Eating Questionnaire23) were administered. Participants also were asked to rate their satisfaction with the treatment approach on a Likert scale ranging from 1 (“not at all satisfied”) to 5 (“very satisfied”).
Statistical Analyses
Descriptive statistics of baseline characteristics for each treatment condition were computed. Baseline characteristics were compared using ANOVA (or non-parametric Kruskal-Wallis, as appropriate) for continuous variables and χ2 test for categorical variables. Percent weight loss was examined as the primary outcome. Multilevel modeling was performed to investigate weight change trajectories from 0, 6, and 12 month assessments for each participant and to examine how treatment effects influenced individual growth trajectories. Furthermore, percent weight loss at the end of treatment was compared among treatment conditions using ANCOVA. Weight suppression, early weight loss (during the first 4 weeks of treatment, when similar core behavioral skills were taught in all conditions), baseline BMI, and attendance were controlled for in outcome analyses because of the significant variability they account for in long-term weight loss. In addition, we examined whether race, sex, or education significantly moderated the effect of condition on weight loss using a two-way ANCOVA. Analyses were performed on an intent-to-treat basis. For missing data, we performed multiple imputation in SPSS using MCMC algorithms known as chained equations imputation.24 Rubin's rules were used to combine analysis results from multiply imputed data.25, 26 Analyses were conducted using R and SPSS. All reported P values are based on 2-sided hypotheses and statistical significance is taken at the 5% level.
Results
Preliminary Analyses
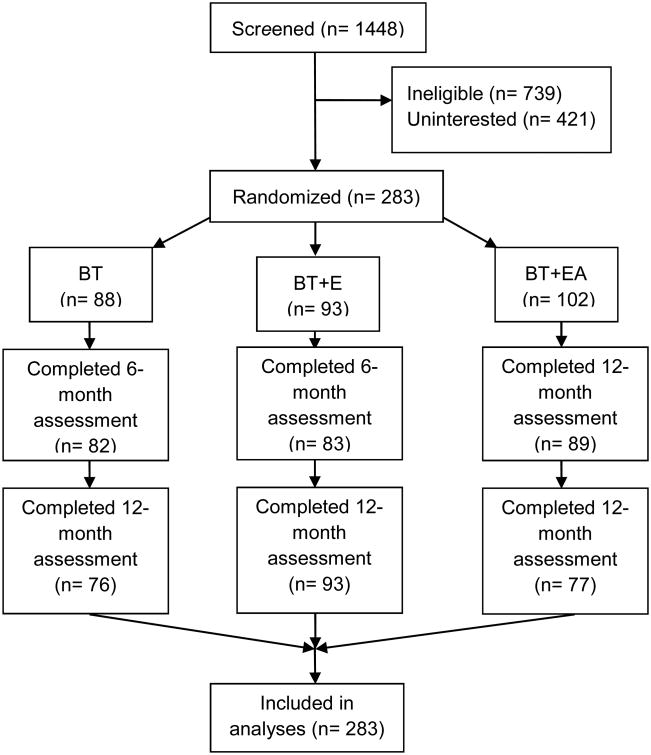
The sample was comprised primarily of non-Hispanic white or African-American participants (as shown in Table 1) and 78.8% were female. Treatment groups did not differ significantly at baseline on any demographic or outcome variables (see Table 1). On average, participants attended 74.6% of group treatment sessions (of the 26 scheduled sessions, M = 19.43, SD = 5.99; see Table 2). Across conditions, average number of sessions attended did not significantly differ (p = .53). Fidelity to treatment condition was high (means: BT = 9.13, BT+E = 9.20, BT+EA= 9.24, with a maximum value for fidelity of 10). As shown in Figure 2, assessments were completed by 91.2% of participants at 6 months and 85.5% of participants at 12 months.
Table 1. Comparison of baseline characteristics of study participants across treatment conditions.
| Condition | ||||
|---|---|---|---|---|
|
| ||||
| BT (n =88) | BT+E (n = 93) | BT+EA (n = 102) | p-value | |
| Race, n (%) | 0.695 | |||
| American Indian/Alaskan Native | 0 (0%) | 0 (0%) | 1 (1%) | |
| Asian | 0 (0%) | 1 (1%) | 0 (0%) | |
| Native Hawaiian or other Pacific Islander | 1 (1%) | 0 (0%) | 0 (0%) | |
| Black or African-American | 24 (27%) | 27 (29%) | 32 (31%) | |
| White | 59 (67%) | 63 (68%) | 64 (63%) | |
| More than one race | 4 (5%) | 2 (2%) | 4 (4%) | |
| Ethnicity, n (%) | 0.156 | |||
| Hispanic/Latino | 7 (8%) | 4 (4%) | 12 (12%) | |
| Non-Hispanic/Latino | 81 (92%) | 89 (96%) | 89 (88%) | |
| Age, M (SD) | 53.02(9.32) | 53.41(10.28) | 53.23(9.43) | 0.965 |
| Black or African-American | 51.46(9.29) | 51.52(10.57) | 52.56(8.53) | |
| White | 53.66(9.67) | 54.63(10.08) | 54.11(9.10) | |
| Body mass index, M (SD) | 34.96(5.19) | 35.38(5.17) | 35.23(4.64) | 0.849 |
| Black or African-American | 36.69(6.18) | 35.82(4.91) | 37.09(4.55) | |
| white | 34.16(4058) | 34083(5.13) | 34.27(4.58) | |
| Female, n (%) | 67 (76%) | 72 (77%) | 84 (82%) | 0.535 |
| Black or African-American | 19 (79%) | 19 (70%) | 28 (87%) | |
| White | 43 (73%) | 51 (81%) | 51 (80%) | |
| Education, n (%) | 0.07 | |||
| High school or lower | 5 (6%) | 6 (6%) | 7 (7%) | |
| Associate's degree | 14 (16%) | 19 (21%) | 12 (12%) | |
| Bachelor's degree | 32 (36%) | 21 (23%) | 47 (46%) | |
| Graduate or professional degree | 37 (42%) | 46 (50%) | 35 (35%) | |
| Black or African-American | ||||
| High school or lower | 2 (8%) | 5 (19%) | 6 (19%) | |
| Associate's degree | 4 (17%) | 7 (27%) | 5 (16%) | |
| Bachelor's degree | 6 (25%) | 6 (23%) | 13 (42%) | |
| Graduate or professional degree | 12 (50%) | 8 (31%) | 7 (23%) | |
| White | ||||
| High school or lower | 2 (3%) | 1 (2%) | 1 (2%) | |
| Associate's degree | 9 (15%) | 11 (17%) | 5 (8%) | |
| Bachelor's degree | 25 (42%) | 14 (22%) | 31 (48%) | |
| Graduate or professional degree | 23 (39%) | 37 (59%) | 27 (42%) | |
Note: BT = Standard behavior therapy, BT+E = behavior therapy with environmental change, BT+EA = Acceptance-based behavior therapy with environmental change. P-value = p-value of chi-square or f-test evaluating potential differences in demographic variables across conditions.
Table 2.
Attendance, retention, and treatment satisfaction by race and treatment condition.
| Condition | |||
|---|---|---|---|
|
| |||
| BT (n =88) | BT+E (n = 93) | BT+EA (n = 102) | |
| Attendance rate, M (SD) | 0.74 (0.26) | 0.73 (0.23) | 0.76 (0.21) |
| Black or African-American | 0.66 (0.31) | 0.68 (0.30) | 0.75 (0.20) |
| White | 0.78 (0.21) | 0.75 (0.19) | 0.79 (0.21) |
| Retention rate, n (%) | 75 (85%) | 76 (82%) | 88 (86%) |
| Black or African-American | 19 (79%) | 20 (74%) | 27 (84%) |
| White | 51 (86%) | 53 (84%) | 58 (90%) |
| Satisfaction, M (SD) | 4.26 (0.96) | 4.37 (0.99) | 4.53 (0.72) |
| Black or African-American | 4.21 (0.97) | 4.53 (0.79) | 4.64 (0.57) |
| White | 4.23 (0.99) | 4.33 (1.06) | 4.52 (0.71) |
Note: BT = Standard behavior therapy, BT+E = behavior therapy with environmental change, BT+EA = Acceptance-based behavior therapy with environmental change. Post-hoc analyses revealed that among African-American participants, attendance was significantly higher in BT+EA, compared to BT (p = .04), and a trend was observed for higher treatment satisfaction (p = .06).
Figure 2.
Participant randomization and retention.
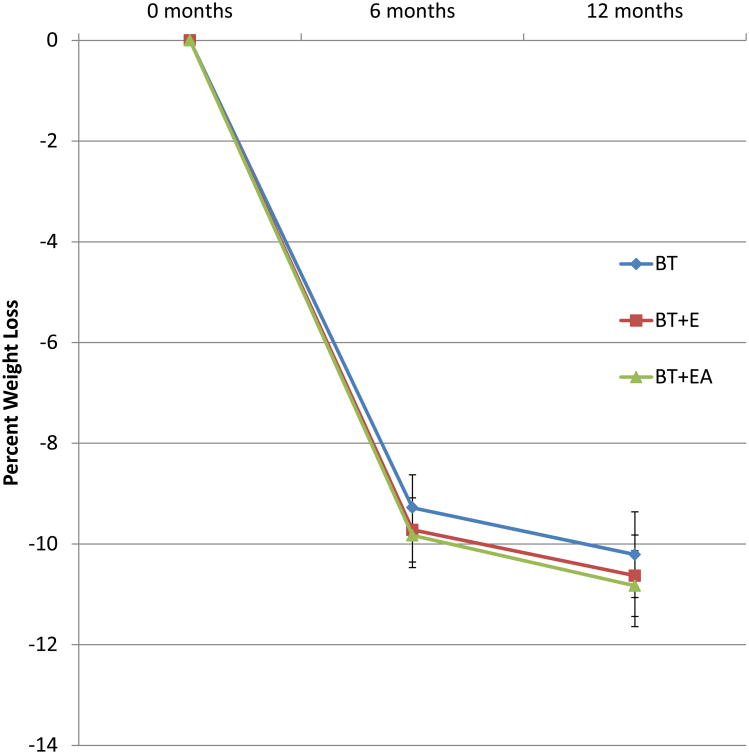
Efficacy
Multilevel modeling analysis revealed a significant linear increasing time effect (p<0.001), which indicated significantly increasing percent weight loss over time for all three conditions during treatment (Figure 3). At 6 months, weight loss means were 9.29% (SD = 6.14%), 9.73% (SD = 6.14%), and 9.83% (SD = 6.01%) in BT, BT+E, and BT+EA, respectively. At 12 months, weight loss means were 10.21% (SD=7.98%), 10.62% (SD=7.82%), and 10.84% (SD=7.04%) in BT, BT+E, and BT+EA, respectively. The interactions between time and treatment conditions were not statistically significant (p=0.94 for contrasting BT versus BT-EA, p=0.69 for contrasting BT versus BT-E, p=0.73 for contrasting BT-E versus BT-EA). In addition, results from ANCOVA revealed that percent weight loss at 12 months did not differ significantly among treatment conditions (p=0.65). There were no significant differences between conditions in change over time in calorie intake (p = .74) or minutes of moderate-to-vigorous physical activity (p = .45). Similarly, the interactions between condition and change in self-efficacy (p = .46), autonomous motivation (p = .41), and uncontrolled eating (p = .54) were not statistically significant.
Figure 3. Average percent weight loss over time by condition.
The pattern of weight loss during treatment did not significantly differ by condition (p=0.94 for contrasting BT versus BT+EA, p=0.69 for contrasting BT versus BT+E, p=0.73 for contrasting BT+E versus BT+EA).
Moderation
While there was no main effect of treatment condition, race significantly moderated the effect of condition on weight loss in a two-way ANCOVA (p= .04), such that African-American participants lost less weight than non-Hispanic white participants in the BT (6.2% vs. 11.5%) and BT+E conditions (6.6% vs. 12.2%), but weight loss in these two groups was similar in the BT+EA condition (9.4% vs. 11.5%) (Figure 4). Only African-American and non-Hispanic white participants were included in this analysis because the other race categories account for less than 5% of the data. The moderation effect was unchanged when education was added to the model as a covariate. To further examine treatment effects on weight loss among African-Americans, a chi-square test was conducted. A clinically significant weight loss (i.e., >5%) at treatment completion also was more likely in the BT+EA condition (80% of participants) than in the BT (57%) or BT+E (48%) conditions (p = .04). Among African-American participants in BT+EA vs. BT, program satisfaction was significantly higher (p = .03), and a statistical trend was observed for higher attendance (p = .06). Neither sex (p = 0.73) nor education (p = 0.72) was a significant moderator of treatment outcome.
Figure 4.
Percent weight loss at 12 months by Condition and Race.
Race significantly moderated the effect of condition on weight loss (p= .04).
Discussion
The current study examined the efficacy of behavioral treatment that included a focus on the home environment (BT+E) and an acceptance-based version of behavioral treatment that also included skills for modifying the home environment (BT+EA), relative to gold standard behavioral treatment (BT). These three interventions resulted in large weight losses at 6 months that were sustained at the 12-month mark. Primary hypotheses were not supported, as neither the addition of tools for home environment modification nor acceptance-based skills improved the overall efficacy of treatment.
The fact that the addition of home environment modification component failed to improve weight loss is at odds with Gorin's results.8 In that study, women, but not men, lost more weight if they were randomized to a version of BT+E versus a BT condition. One possible explanation for the discrepancy was that the BT+E condition in the Gorin study contained direct environmental modifications, while in the current study participants were responsible for initiating and maintaining environmental changes, in order to provide a more ecologically-valid test of this approach. For example, participants in the Gorin8 study were provided with home exercise equipment and were partially reimbursed for setting up an online supermarket shopping account in order to limit store-based impulse purchases. Moreover, that study required the participation of another overweight member of the household in order to support household changes. Perhaps these more robust and direct interventions are necessary in order to confer benefit, at least to women.
In contrast to the current study, another large trial (Mind Your Health II)13 recently reported substantially greater weight loss for participants who were assigned acceptance-based behavioral treatment compared to those who received gold standard BT. Several potentially important differences exist between the acceptance-based treatment protocol in that study and the current study that may explain the discrepancy. First, in the BT+EA treatment, the current study's acceptance-based content was substantially reduced to make room for a focus on modification of the environment. This change resulted in a reduced dosage and emphasis of acceptance-based skills and required participants to manage yet another category of information. Perhaps participants' cognitive “bandwidth” places constraints on the number of skills that can be mastered. In addition, the Mind Your Health II study set out to make a number of enhancements to the treatment protocol following a predecessor study which indicated that the experimental treatment was only more effective than BT under certain conditions. Changes included using a simplified treatment frame (“Control What You Can and Accept What You Can't”) and de-emphasizing skills related to eating in response to aversive experiences (e.g., anxiety, cravings) while instead emphasizing willingness to choose less pleasurable options. The current study's treatment protocol was not similarly modified which may also have contributed to the reduced difference between BT and BT+EA. Finally, there may have been a ceiling effect that limited the ability to observe superior performance of the BT+E or BT+EA conditions, because participants in the BT condition achieved large weight losses that were, on average, fully maintained during the month 6-12 period when weight regain would otherwise be expected to begin.
While no main effect of treatment condition was observed, the moderating effect of race was large and notable. Whereas, in the BT and BT+E conditions, African-American participants lost half the weight of non-Hispanic white participants, the disparity was greatly attenuated for African-Americans assigned to BT+EA. Similarly, African-Americans receiving BT+EA were 1.4 times to 1.7 times as likely to reach a clinically significant weight loss at 12 months compared to those receiving BT and BT+E, respectively. Previous research has revealed differences in behavioral weight loss treatment response by race; African-American participants typically lose approximately 50% less weight compared to white participants.27-29 Future research must be conducted to replicate this finding and identify mechanisms of action. One hypothesis is that the BT+EA emphasis on clarifying personal values and connecting them to weight control behaviors was especially important for African-American participants, given previously documented racial differences in motivators for weight loss.30-31 It also is possible that these participants found willingness skills to be especially helpful when faced with particular cultural, social, or environmental challenges to weight control, such as needing to put forth greater effort to acquire healthy foods or respond to social cues that encourage consumption of high-calorie foods.32-34
This study has several limitations. Weight and behavior likely changed in meaningful ways after treatment ended, as weight loss maintenance is notoriously difficult. Moderators were examined as an exploratory aim, and it is possible that results would have differed with larger sample sizes for particular demographic groups (e.g., men or African-American participants). Additional research (e.g., with qualitative interviews or careful measurement of mediators) is needed to understand why an interaction between race and treatment was observed. The generalizability and scalability of the interventions may be limited, given the intensive schedule of meetings and delivery in an academic weight loss clinic. These areas represent important directions for future research.
Study Importance Questions.
What Is Known
Environmentally-focused and acceptance-based behavioral treatments for weight loss both have promise, but their efficacy compared to traditional behavioral treatment has not been clearly established and a combined approach has not been tested.
Behavioral approaches to weight loss treatment are typically less effective for African-American participants compared to white participants; innovative interventions to improve outcome are specifically needed for this population.
What This Study Adds
This study found that there was no main effect of treatment condition on weight loss (i.e., in general, the efficacy of behavioral treatment did not depend on whether or not environmental or acceptance-based skills were integrated), but that efficacy was significantly moderated by race, such that the racial disparity in efficacy was smallest when African-American participants were taught an approach that integrated environmental and acceptance-based skills.
Acknowledgments
The authors wish to thank Stephanie Kerrigan, Madeline Kirch, Colleen Kase, and Alexandra Convertino for their contributions as research coordinators to this project.
Funding: NIH R01DK092374
Footnotes
Clinical Trial Registration: NCT01858714, ClinicalTrials.gov
Disclosure: The authors declared no conflict of interest.
References
- 1.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Christian JG, Tsai AG, Bessesen DH. Interpreting weight losses from lifestyle modification trials: using categorical data. International journal of obesity. 2010;34:207–209. doi: 10.1038/ijo.2009.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loveman E, Frampton GK, Shepherd J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health technology assessment. 2011;15:1–182. doi: 10.3310/hta15020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appelhans BM, French SA, Pagoto SL, Sherwood NE. Managing temptation in obesity treatment: a neurobehavioral model of intervention strategies. Appetite. 2016;96:268–279. doi: 10.1016/j.appet.2015.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poelman MP, de Vet E, Velema E, et al. PortionControl@HOME: results of a randomized controlled trial evaluating the effect of a multi-component portion size intervention on portion control behavior and body mass index. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2015;49:18–28. doi: 10.1007/s12160-014-9637-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorin AA, Phelan S, Raynor H, Wing RR. Home food and exercise environments of normal-weight and overweight adults. American journal of health behavior. 2011;35:618–626. doi: 10.5993/ajhb.35.5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: is it feasible? Obesity research. 2003;11(Suppl):44S–59S. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- 8.Gorin AA, Raynor HA, Fava J, et al. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2013;32:128–137. doi: 10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forman EM, Butryn ML. A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015;84:171–180. doi: 10.1016/j.appet.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forman EM, Butryn ML, Manasse SM, Bradley LE. Acceptance-based behavioral treatment for weight control: a review and future directions. Current opinion in psychology. 2015;2:87–90. doi: 10.1016/j.copsyc.2014.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forman EM, Butryn ML. Effective weight loss: an acceptance-based behavioral approach (Clinician Guide) New York: Oxford: 2016. [Google Scholar]
- 12.Forman EM, Butryn ML, Juarascio AS, et al. The Mind Your Health project: a randomized controlled trial of an innovative behavioral treatment for obesity. Obesity. 2013;21:1119–1126. doi: 10.1002/oby.20169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forman EM, Butryn ML, Manasse SM, et al. Acceptance-based versus standard behavioral treatment for obesity: results from the Mind Your Health randomized controlled trial. Obesity. 2016;24:2050–2056. doi: 10.1002/oby.21601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niemeier HM, Leahey T, Palm Reed K, Brown RA, Wing RR. An acceptance-based behavioral intervention for weight loss: a pilot study. Behavior therapy. 2012;43:427–435. doi: 10.1016/j.beth.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Look AHEAD Research Group. Wadden TA, West DS, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes care. 1999;22:623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychological bulletin. 1993;114:100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- 18.Byrne SM, Cooper Z, Fairburn CG. Psychological predictors of weight regain in obesity. Behaviour research and therapy. 2004;42:1341–1356. doi: 10.1016/j.brat.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 19.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? Journal of consulting and clinical psychology. 1999;67:177–185. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- 20.Stice E, Durant S, Burger KS, Schoeller DA. Weight suppression and risk of future increases in body mass: effects of suppressed resting metabolic rate and energy expenditure. Am J Clin Nutr. 2011;94:7–11. doi: 10.3945/ajcn.110.010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. Journal of consulting and clinical psychology. 1991;59:739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 22.Levesque CS, Williams GC, Elliot D, et al. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health education research. 2007;22:691–702. doi: 10.1093/her/cyl148. [DOI] [PubMed] [Google Scholar]
- 23.Pikramenou Z, Weinstein J, Pan Q, et al. Self-organization of photo-active nanostructures: general discussion. Faraday discussions. 2015;185:529–548. doi: 10.1039/c5fd90092a. [DOI] [PubMed] [Google Scholar]
- 24.Yuan YC. Multiple imputation for missing data: Concepts and new development. Rockville, MD: SAS Institute Inc.; 2005. [Google Scholar]
- 25.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- 26.Rubin DB. Multiple imputation after 18+ years. Journal of the American Statistical Association. 1996;91:473–489. [Google Scholar]
- 27.Cox TL, Krukowski R, Love SJ, et al. Stress management-augmented behavioral weight loss intervention for African American women: a pilot, randomized controlled trial. Health education & behavior : the official publication of the Society for Public Health Education. 2013;40:78–87. doi: 10.1177/1090198112439411. [DOI] [PubMed] [Google Scholar]
- 28.West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity. 2008;16:1413–1420. doi: 10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- 29.Lewis KH, Edwards-Hampton SA, Ard JD. Disparities in treatment uptake and outcomes of patients with obesity in the USA. Current obesity reports. 2016;5:282–290. doi: 10.1007/s13679-016-0211-1. [DOI] [PubMed] [Google Scholar]
- 30.Blixen CE, Singh A, Thacker H. Values and beliefs about obesity and weight reduction among African American and Caucasian women. J Transcult Nurs. 2006;17:290–297. doi: 10.1177/1043659606288375. [DOI] [PubMed] [Google Scholar]
- 31.Vaughan CA, Sacco WP, Beckstead JW. Racial/ethnic differences in Body Mass Index: the roles of beliefs about thinness and dietary restriction. Body Image. 2008;5:291–298. doi: 10.1016/j.bodyim.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnes AS, Goodrick GK, Pavlik V, et al. Weight loss maintenance in African-American women: focus group results and questionnaire development. Journal of general internal medicine. 2007;22:915–922. doi: 10.1007/s11606-007-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis EM, Clark JM, Carrese JA, Gary TL, Cooper LA. Racial and socioeconomic differences in the weight-loss experiences of obese women. American journal of public health. 2005;95:1539–1543. doi: 10.2105/AJPH.2004.047050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zenk SN, Schulz AJ, Israel BA, et al. Food shopping behaviours and exposure to discrimination. Public Health Nutr. 2014;17:1167–1176. doi: 10.1017/S136898001300075X. [DOI] [PMC free article] [PubMed] [Google Scholar]