Abstract
We present 3 cases of duplicated or fenestrated internal jugular veins in patients undergoing neck dissection, including the first known case of concomitant bovine aortic arch. The prevalence of this anomaly is 1.0% (3 out of 295 patients). Internal jugular vein duplication and fenestration may risk iatrogenic injury to the vasculature and spinal accessory nerve during neck dissection. The existence of this anatomic abnormality should be considered when variation of the internal jugular vein is encountered. The objective of this report is to discuss the presentation, clinical implications, and literature pertaining to internal jugular vein duplication and fenestration.
Keywords: Internal jugular vein, anatomical variant, neck dissection, duplication, fenestration, spinal accessory nerve
INTRODUCTION
Cervical lymphadenectomy or neck dissection is a common procedure performed in the management of head and neck cancer. Complications associated with this surgery include hemorrhage, nerve damage, and chylous fistula. Successful surgical management of these patients is therefore predicated on recognizing patient-specific anatomic structures that may increase their risk of an adverse outcome.
The internal jugular vein (IJV) is the largest caliber blood vessel in the head and neck. It serves as a major surgical landmark for adjacent structures (e.g., spinal accessory nerve, carotid artery, cervical lymph nodes). Anomalies of the IJV, including duplications and fenestrations, have been reported.1,2 IJV duplication refers to a bifurcation of the vein with each branch having an separate connection to the subclavian vein, while IJV fenestration refers to a bifurcation that reunites proximal to the subclavian vein,1 although these terms are commonly interchanged in the literature. Understanding anomalies of the IJV is important to avoid iatrogenic damage during neck surgery or central venous catheterization.
There have been limited attempts to characterize the prevalence of IJV duplication and fenestration.2,3 We report 3 cases of IJV anomalies in patients undergoing neck dissection from 2008 to 2015 and discuss the clinical implications, management, and literature pertaining to IJV duplication and fenestration.
CASE REPORT
Patient 1
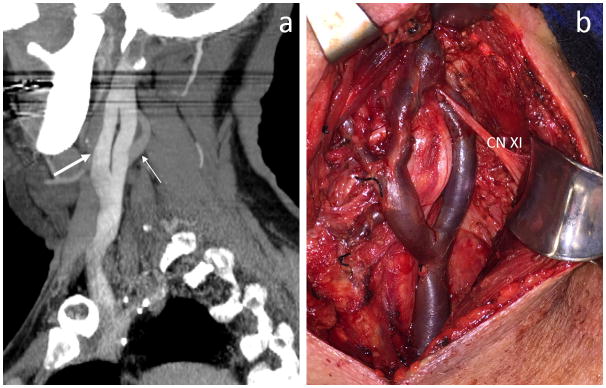
A 65-year old Caucasian man presented with a several week history of a left tonsillar mass. The patient was diagnosed with human papilloma virus associated T3N2bM0 squamous cell carcinoma of the left tonsil. His work-up included a PET/CT, although no mention was made of an IJV abnormality in the report. He underwent transoral robotic left radical tonsillectomy and right tonsillectomy, followed by a left selective neck dissection of levels II–IV. A fenestrated left IJV was observed bifurcating at the level of the hyoid and then reuniting 3.5 cm inferior within the carotid sheath (Fig. 1). The spinal accessory nerve traversed the fenestration from superficial to deep as it traveled towards the skull base. His post-operative course showed no evidence of recurrence or spinal accessory nerve dysfunction.
Fig. 1.
Left internal jugular vein fenestration. (a) Sagittal thick slab reconstruction image of a contrast-enhanced CT shows the internal jugular vein bifurcating into anterior and posterior channels (thick arrow) which reunite prior to the subclavian vein. Note the proximal internal carotid artery (thin arrow) deep to the internal jugular vein. (b) Intraoperative image shows spinal accessory nerve coursing from superficial to deep through the fenestration towards the skull base. CN XI = spinal accessory nerve.
Patient 2
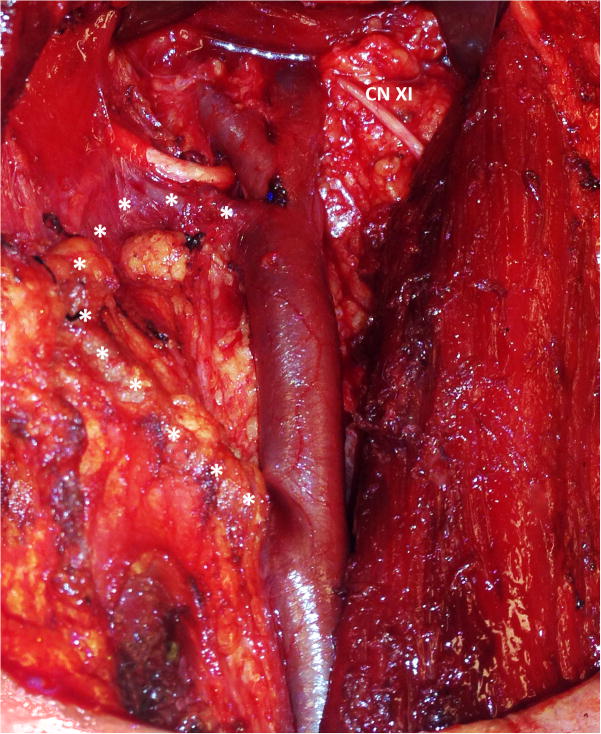
A 49-year old Caucasian man presented with a 3-month history of a tongue lesion, initially attributed to an abrasion by a chipped tooth. Biopsy of the tongue lesion showed squamous cell carcinoma of the left lateral tongue and he was clinically staged as T1N0M0 after PET/CT. The radiology report did not mention an IJV abnormality. He underwent a left partial glossectomy with primary closure and left selective neck dissection of levels I–IV. A fenestrated IJV was seen during surgery bifurcating just distally to the inflow of the common facial vein (Fig. 2). The spinal accessory nerve did not pass through the fenestration. The patient recovered well from the procedure with minimal regional pain and no evidence of cancer recurrence or spinal accessory nerve dysfunction.
Fig. 2.
Intraoperative image of left fenestrated internal jugular vein beginning immediately distal to the common facial vein. Anterior branch, demarcated by asterisks, is partially obstructed by lymphatic tissue. CN XI = spinal accessory nerve.
Patient 3
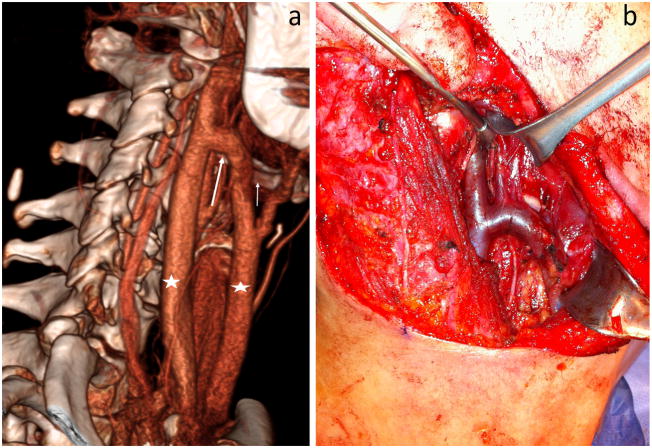
A 51-year old Caucasian woman with a 15 pack year smoking history presented with a mildly tender mass in the tail of the parotid that had been gradually increasing in size for approximately one year. Workup included fine needle aspiration of the parotid which showed histological features suspicious for high grade adenoid cystic carcinoma and a neck CT with intravenous contrast demonstrated no evidence of neck metastasis. She was clinically staged as T2N0M0. The radiology report mentioned a right IJV duplication, branching at the level of the hyoid bone and independently draining into the right subclavian vein (Fig. 3). She was also found to have a bovine aortic arch with a common origin for the brachiocephalic and left common carotid artery. The patient underwent subtotal parotidectomy, neck dissection, and sternocleidomastoid flap reconstruction. She had no evidence of recurrence or spinal accessory nerve damage.
Fig. 3.
Left duplicated internal jugular vein. (a) 3D reconstruction showing two separate internal jugular veins (stars) that drain separately into the subclavian vein and are joined together superiorly by a transversely oriented branch (long arrow) at the level of the hyoid bone (short arrow). (b) Intraoperative image of bifurcation.
DISCUSSION
IJV duplications and fenestrations are rare. We report a prevalence of 1.0%, based on 3 cases out of 295 neck dissections performed by a single surgeon at our institution from 2008 to 2015. Two prior studies that have assessed prevalence of these anatomical variations of the IJV. Hashimoto et al. reported a prevalence of 3.3% based on 4 cases out of 123 neck dissections in a Japanese population.2 A second report estimated a prevalence of 0.4% based on 3 cases out of roughly 750 neck dissections in France.3
The IJV fenestration in Patients 1 and 2 in this study were identified by direct visualization during surgery, the most common diagnostic method reported in the literature. The IJV duplication of Patient 3 was identified pre-operatively by a contrast-enhanced CT. A single case report notes identification of IJV duplication by ultrasound.4 Despite the ability to identify these anomalies with contrast-enhanced CT pre-operatively, it was only mentioned in 1 out of 3 radiology reports in our patients—likely reflecting the lack of attention paid to the venous system in the face of pathologic adenopathy.
The 3 patients described above had an absence of symptoms related to their IJV anomalies. This is consistent with past reports, although there have been cases of patients presenting with neck swelling, dyspnea and dysphagia.5 Previous cases of IJV duplication and fenestration have been associated with venous ectasia,3 with one study reporting concern for IJV anomalies being mistaken as laryngoceles or branchial cleft cysts.5
To our knowledge, there have been no reported cases of IJV duplication with concomitant bovine aortic arch. However, secondary vascular abnormalities have been reported to occur with IJV bifurcation.6 There are 2 reported cases of bilateral IJV bifurcation.1,7 Patients with IJV bifurcation may have a higher prevalence of additional vascular abnormalities, prompting additional precautions. Consideration of a contrast-enhanced CT is warranted if a patient with known IJV anomaly is undergoing future procedures involving major vascular structures. Regardless of anticipated medical care, clear documentation of an IJV bifurcation or fenestration is strongly recommended.
Knowledge of the various types IJV anomalies may be critical to avoid iatrogenic injury. If a duplication or fenestration is not appreciated and only part of the IJV is controlled during a neck procedure, copious bleeding can ensue. Furthermore, this bleeding may prove challenging to control as there may be multiple feeders from above and below, including the duplication. Securing control of a hemorrhaging IJV places the hypoglossal and spinal accessory nerves at risk for injury.
Preservation of the spinal accessory nerve is important to reduce functional complications following neck dissection. The spinal accessory nerve often passes through the IJV fenestration, however empty fenestrations not bisected by a nerve have also been reported.8 We found both types of spinal accessory variants in relation to the IJV anomalies.
The etiology of IJV duplications and fenestrations is unknown. Currently, 4 possible theories have been proposed, occupying 4 general categories: neural, vascular, bony, and muscular.9 A neural etiology suggests branching of the IJV is the result of obstructed growth by the spinal accessory nerve during development. Although this is consistent with cases of the spinal accessory nerve bisecting the IJV (Patient 1), it does not explain IJV duplications or fenestrations without the spinal accessory nerve coursing through it (Patients 2 and 3). Alternatively, vascular weakness associated with turbulent flow could result in endothelial reorganization into separate vessels during development. However, we did not find any persistent evidence of weakness of the IJV vascular wall in our patients during surgery. A bony etiology proposes that bifurcation occurs due to developmental impingement of the IJV at the jugular foramen. Lastly, one case report has suggested a muscular etiology, based on an observed IJV duplication around the posterior belly of the omohyoid.10
CONCLUSION
We report a prevalence of IJV fenestration or duplication of 1.0% and the first case of IJV duplication with concomitant bovine aortic arch. Identification of these cases is most likely to occur intraoperatively and incidentally. Patients with IJV duplication and fenestration are at risk of injury to the vasculature and spinal accessory nerve. Head and neck surgeons should be aware of the occurrence and presentation of IJV duplication and fenestration to avoid iatrogenic injury.
Footnotes
Disclosures: None
Funding: None
BIBLIOGRAPHY
- 1.Downie SA, Schalop L, Mazurek JN, Savitch G, Lelonek GJ, Olson TR. Bilateral duplicated internal jugular veins: case study and literature review. Clin Anat. 2007;20(3):260–266. doi: 10.1002/ca.20366. [DOI] [PubMed] [Google Scholar]
- 2.Hashimoto Y, Otsuki N, Morimoto K, Saito M, Nibu K. Four cases of spinal accessory nerve passing through the fenestrated internal jugular vein. Surg Radiol Anat. 2012;34(4):373–375. doi: 10.1007/s00276-011-0875-x. [DOI] [PubMed] [Google Scholar]
- 3.Prades JM, Timoshenko A, Dumollard JM, Durand M, Merzougui N, Martin C. High duplication of the internal jugular vein: clinical incidence in the adult and surgical consequences, a report of three clinical cases. Surg Radiol Anat. 2002;24(2):129–132. doi: 10.1007/s00276-002-0020-y. [DOI] [PubMed] [Google Scholar]
- 4.Radak D, Tanaskovic S, Marinkovic S, Antonic Z, Kolar J. Internal jugular vein duplication: a further truncular malformation in a patient with multiple sclerosis. Phlebology. 2012;27(4):194–196. doi: 10.1258/phleb.2011.011027. [DOI] [PubMed] [Google Scholar]
- 5.Wong BY, Strachan DR, Loney EL. Duplication of internal jugular veins: case report. J Laryngol Otol. 2010;124(3):341–344. doi: 10.1017/S0022215109990855. [DOI] [PubMed] [Google Scholar]
- 6.Ayoub O, Benton J, Jackson S. A persistent left superior vena cava, with the accessory nerve passing through a duplicate segment of the left internal jugular vein: a unique presentation. Ear Nose Throat J. 2014;93(10–11):E6–8. doi: 10.1177/014556131409310-1101. [DOI] [PubMed] [Google Scholar]
- 7.Coca Pelaz A, Rodrigo Tapia JP. Bilateral duplication of the internal jugular vein. Acta Otorrinolaringol Esp. 2008;59(6):314. [PubMed] [Google Scholar]
- 8.Ozturk NC, Talas DU. Fenestration of internal jugular vein and relation to spinal accessory nerve: Case report and review of the literature. Clin Anat. 2010;23(8):883–884. doi: 10.1002/ca.20897. [DOI] [PubMed] [Google Scholar]
- 9.Nayak BS. Surgically important variations of the jugular veins. Clin Anat. 2006;19(6):544–546. doi: 10.1002/ca.20268. [DOI] [PubMed] [Google Scholar]
- 10.Bachoo I, Evans B. Duplication of the lower third of the internal jugular vein - case report and surgical implications. Br J Oral Maxillofac Surg. 2014;52(8):772–773. doi: 10.1016/j.bjoms.2014.05.016. [DOI] [PubMed] [Google Scholar]