Abstract
Background
Ipilimumab (IPI) and BRAF inhibitors (BRAFi) improve survival in melanoma, but not all patients will benefit and toxicity can be significant. Pretreatment neutrophil to lymphocyte ratio (NLR) has been associated with outcome in IPI-treated patients, but has not been studied during treatment or in BRAFi-treated patients.
Methods
Using a prospectively maintained database, patients with unresectable stage III or IV melanoma treated with IPI or a BRAFi (vemurafenib or dabrafenib as monotherapy) from 2006 to 2011 were identified. NLR was calculated before treatment and at 3-week intervals after treatment initiation until 9 weeks. Baseline NLR was tested for association with overall survival (OS), progression free survival (PFS), and clinical response to treatment. On-treatment NLRs were tested for association with the same outcomes using landmark survival analyses and time-dependent Cox regression models. The association of relative change of NLR from baseline with outcomes was also examined. A multivariate model tested the association of NLR and OS/PFS with additional clinical factors.
Results
There were 197 IPI patients and 65 BRAFi patients. In multivariable analysis adjusting for M stage, and disease type (in OS)/gender (in PFS), an NLR value of 5 or above at every timepoint was associated with worse OS (HR 2.03–3.37, p < 0.001), PFS (HR 1.81–2.51, p < 0.001), and response to therapy (OR 3.92–9.18, p < 0.007), in the IPI cohort. In addition, a > 30% increase in NLR above baseline at any timepoint was associated with a worse OS and PFS (HR 1.81 and 1.66, p < 0.004). In BRAFi patients, NLR was not consistently associated with outcomes.
Conclusions
A high NLR, whether measured prior to or during treatment with IPI, is associated with worse OS, PFS, and clinical response in patients with advanced melanoma. An increasing NLR from baseline during treatment was correlated with worse OS and PFS in IPI-treated patients. In comparison, as NLR was not associated with outcomes in BRAFi patients, NLR may have a uniquely predictive value in patients treated with immunotherapy.
Keywords: Neutrophil to lymphocyte ratio, NLR, Melanoma, Immunotherapy, BRAF inhibitors
Highlights
-
•
Neutrophil to lymphocyte ratio is associated with important clinical outcomes in melanoma patients treated with ipilimumab.
-
•
Changes in neutrophil to lymphocyte ratio from baseline during treatment with ipilimumab correlate with clinical outcomes
-
•
Neutrophil to lymphocyte ratio is not associated with outcomes in those treated with BRAF inhibitors
Baseline neutrophil to lymphocyte ratio (NLR) and changes in NLR during treatment associate with important clinical outcomes, including overall survival, progression-free survival, and clinical response in advanced melanoma patients treated with immunotherapy, and therefore may have a valuable role in selecting patients most likely or least likely to benefit from treatment, or for monitoring response to treatment over time. This marker is not useful in patients treated with BRAF inhibitors, perhaps reflecting its unique value in immunotherapy.
1. Introduction
Although advanced melanoma still remains a challenging diagnosis, significant enthusiasm has been generated by new therapeutic agents that have demonstrated increases in survival. Ipilimumab (IPI) is a monoclonal antibody that inhibits cytotoxic T-lymphocyte associated antigen 4 (CTLA-4), thereby acting as a “checkpoint inhibitor” to enhance native immune function. In randomized trials, IPI produced objective responses in 11% of patients, but some degree of disease control in 29% (Hodi et al., 2010). Moreover, there is a pattern of delayed but often durable response, and long-term survival is possible in patients who respond to treatment (Prieto et al., 2012). In fact, some groups treated with IPI may have 4 year survival rates up to 49.5% (Wolchok et al., 2013a). Despite promising outcomes, immune-related adverse events have been described in a significant proportion of patients who receive the agent. These include diarrhea (30%), colitis (7%), hepatitis (3%), and hypophysitis (2%). In a randomized trial, 2.1% of enrolled patients died as a direct result of treatment (Hodi et al., 2010). The therapeutic effect of ipilimumab led to rapid investigation of other checkpoint blocking agents and antibodies blocking the PD-1 pathway have demonstrated 40–45% response rates with 35% > 3 year survival and reduced toxicity, compared with ipilimumab (Hamid et al., 2013, Robert et al., 2015a, Hodi et al., 2016). Further, combined checkpoint blockade with ipilimumab + nivolumab results in response rates up to 60% in melanoma, albeit with higher rates of toxicity (Wolchok et al., 2013b, Postow et al., 2015).
Targeted agents are also important in the treatment of advanced melanoma. BRAF inhibitors (BRAFi), including the agents vemurafenib and dabrafenib, are beneficial in the population of melanoma patients whose tumors harbor a BRAF mutation. In a prospective randomized trial, the response rate to vemurafenib approached 50% and improved overall and progression free survival when compared to dacarbazine, although median progression free survival was only 6 months even with vemurafenib (Chapman et al., 2011). Combined inhibition of BRAF and MEK improves the objective response rate to 64% and improves 12 month overall survival from 65% to 72% when compared with single-agent BRAFI (Robert et al., 2015b, McArthur et al., 2014). Combined BRAF and MEK inhibition is also associated with less dermatologic toxicity (Robert et al., 2015b, Larkin et al., 2014).
Therefore, immunotherapy and targeted agents provide important therapeutic options with distinct mechanisms in advanced melanoma, each capable of improving survival. However, not all patients derive benefit, and the personal and financial cost can be significant. In this setting, establishing biomarkers capable of predicting response to these agents would provide an opportunity to identify patients most likely or unlikely to benefit, while allowing a more refined calculation of the risk/benefit ratio.
There is a complex interaction between tumors and the innate and adaptive immune responses. The immune system may work to eradicate tumors, as is the theoretical basis of immunotherapy. Yet inflammation may also be associated with disease progression and adverse outcomes, thought to be due to the inflammatory production of bioactive molecules in the tumor microenvironment (Hanahan and Weinberg, 2011). Systemic inflammation leads to neutrophilia and lymphocytopenia, and can be quantified by the neutrophil to lymphocyte ratio (NLR). Elevated NLR is associated with inferior disease-specific survival in a number of malignancies including gastric cancer (Wang et al., 2016), pancreatic cancer (Stotz et al., 2013), hepatocellular carcinoma (Mano et al., 2013), colorectal cancer (Malietzis et al., 2014), renal cell carcinoma (de Martino et al., 2013), non-small cell lung cancer (Pinato et al., 2014), gastrointestinal stromal tumor (Perez et al., 2013), ovarian cancer (Williams et al., 2014), multiple myeloma (Kelkitli et al., 2014, Templeton et al., 2014).
There is evidence that pretreatment NLR may be associated with outcome in patients treated with IPI (Ferrucci et al., 2015, Zaragoza et al., 2016). In particular, prior studies have found that a baseline NLR < 5 is associated with improved survival in patients treated with IPI (Ferrucci et al., 2015). However, the predictive value of change in NLR over time during treatment has not yet been investigated. We sought to determine if change in NLR could be associated with treatment outcome. Additionally, the role of NLR has not been established in patients treated with BRAFi. Given the differences in mechanisms between immunotherapy and BRAFi, we sought to determine the value of NLR in these different therapeutic subgroups.
2. Methods
We performed a retrospective review of a prospectively maintained database to identify all patients with unresectable stage III and IV melanoma treated with IPI or a BRAFi as monotherapy between 2006 and 2011 at Memorial Sloan Kettering Cancer Center (MSKCC). Patients without pretreatment complete blood count (CBC) values were excluded. Clinicopathologic features, including age, gender, performance status, melanoma type, AJCC stage, lines of prior therapy, and follow-up status were documented. We recorded absolute neutrophil and lymphocyte values obtained before the initiation of treatment with either IPI or a BRAFi, and at three week intervals after treatment initiation until 9 weeks. Timepoints were the same for both cohorts. The MSKCC institutional review board approved this study.
IPI was administered intravenously at doses of either 3 mg/kg or 10 mg/kg every 3 weeks for up to 4 doses during the induction phase. Clinical assessments were conducted and patients with an objective response or stable disease were eligible to receive maintenance therapy at their assigned dose every 3 months. In the BRAFi group, patients received either vemurafenib (960 mg orally twice daily) or dabrafenib (150 mg orally twice daily).
Overall survival (OS) was calculated from date of treatment initiation to the date of death from any cause. Patients who were still alive were censored at the last follow-up. Progression-free survival (PFS) was calculated from the date of treatment initiation until progression, as documented by imaging, according to response evaluation criteria in solid tumors (RECIST) or clinical examination or death. Those alive and without progression were censored at last follow-up. Response to therapy was assessed at 12 weeks after treatment initiation by the treating physician and was classified as complete response (CR), partial response (PR), stable disease (SD), or no response (NR). For the purpose of this study, we considered clinical benefit to encompass CR, PR, and SD. NLR at each timepoint (pretreatment baseline, 3 weeks, 6 weeks, and 9 weeks after treatment initiation) was tested for association with OS, PFS, and clinical benefit. Landmark survival analyses with Cox regression models were fit for on-treatment timepoints. NLR values were stratified into ≥ 5 or < 5 for consistency with previously published reports (Stotz et al., 2013, Pinato et al., 2014, Ferrucci et al., 2015, Cananzi et al., 2014). Additionally, we tested for associations with the same outcomes using the median NLR value at each timepoint as the threshold. The association of relative change of NLR over time from baseline with OS and PFS was also determined. Over the treatment course, we marked the first increase of NLR from baseline with magnitudes between 10% and 100%, and assessed its associations with OS/PFS using time-dependent Cox regression. Multivariate models tested the association of NLR and OS/PFS in the context of other known clinically relevant prognostic factors including M stage, and disease type (in OS) or gender (in PFS). Multivariable models assessing associations between NLR change from baseline and OS/PFS controlled for the same sets of clinical factors plus baseline NLR ≥ 5. All analyses were carried out using SAS (version 9.2, SAS Institute Inc., Cary, NC) and R version 3.1 (The R Foundation for Statistical Computing).
3. Results
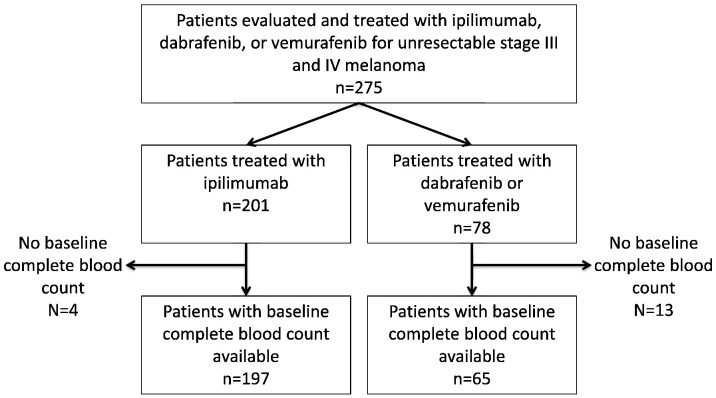
The study flow diagram is shown in Fig. 1. Baseline characteristics of patients included in the final analysis are shown in Table 1. There were 197 patients treated with IPI and 65 treated with a BRAFi who had pretreatment CBC available. Median time from baseline CBC to first dose of treatment was 0 days, with a range of 0–28 days. Median follow-up was 54.3 months in the IPI group (range 5–109) and 53 months in the BRAFi group (range 4–56).
Fig. 1.
Study flow diagram.
Table 1.
Patients characteristics and NLR.
| Ipilimumab group (n = 197) | BRAFi group (n = 65) | |
|---|---|---|
| Gender | ||
| F | 72 (37%) | 21 (32%) |
| M | 125 (63%) | 44 (68%) |
| Prior line | ||
| No | 47 (24%) | 24 (37%) |
| Yes | 150 (76%) | 41 (63%) |
| KPS | ||
| < 90 | 82 (42%) | 23 (42%) |
| 90/100 | 115 (58%) | 32 (58%) |
| Stage | ||
| III | 6 (3%) | 4 (6%) |
| IVA/B | 36 (18%) | 14 (21%) |
| IVC | 155 (79%) | 47(72%) |
| Melanoma type | ||
| Cutaneous | 171 (87%) | |
| Ocular | 13 (7%) | |
| Mucosal | 13 (7%) | |
| Dose (mg/kg) | ||
| 3 | 137 (70%) | |
| 10 | 60 (30%) | |
| Median (range), N | Median (range), N | |
| Age at 1st dose | 62.6 (9.8, 91), 197 | 59.8 (23.3, 87.8), 65 |
| Baseline NLR | 4.4 (0.9, 87.5), 197 | 4.9 (1.3, 31.9), 65 |
| Week 3 NLR | 3.4 (0.8, 57), 182 | 4.6 (0.5, 47.8), 59 |
| Week 6 NLR | 3.4 (0.6, 19.2), 153 | 3.9 (1.2, 228), 53 |
| Week 9 NLR | 3.2 (1, 26.8), 125 | 4.6 (1.1, 26.8), 54 |
| Median OS (95%CI), months | 10.1 (7.5, 12.6) | 12.1 (8.6, 23.0) |
| Median PFS (95%CI), months | 3.2 (2.6, 3.8) | 5.4 (3.7, 6.4) |
| Median OS followup in survivors (range), months | 54.3 (5.1, 108.7) | 52.8 (3.8, 55.9) |
In the IPI group, median baseline NLR was 4.4 (range 0.9–87.5) and decreased to 3.2 (range 1–26.8) by week 9 (Table 1). In contrast, NLR remained similar over the course of treatment in the BRAFi group, with a median at baseline and at week 9 of 4.9 (range 1.3–31.9) and 4.6 (range 1.1–26.8), respectively.
Univariate associations of NLR with OS and PFS in the IPI group are shown in Table 2. NLR ≥ 5 at all time points, in addition to stage IV M1C disease, mucosal melanoma and Karnofsky performance status score < 90 were associated with significantly worse OS and PFS. In multivariate analysis, NLR ≥ 5 at every timepoint was associated with poor OS (HR 2.03–3.37) and PFS (HR 1.81–2.51) (Table 2). Stage IV M1C disease and mucosal melanoma were also associated with worse outcomes. The associations of NLR with outcome remained significant if the median NLR at each timepoint was used as the cutoff to stratify patients.
Table 2.
Univariate and multivariable analyses of NLR associations with outcomes in IPI group.
| Univariate analysis |
Multivariable analysis |
|||||
|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | |||
| OS | ||||||
| Baseline | Baseline NLR ≥ 5 (ref: < 5) | 2.08 (1.52, 2.83) | < 0.001 | 2.03 (1.49, 2.77) | < 0.001 | |
| M stage C (ref = others) | 2.17 (1.45, 3.25) | < 0.001 | 2.07 (1.38, 3.13) | < 0.001 | ||
| Melanoma type (ref = mucosal): | Ocular | 0.49 (0.22, 1.06) | 0.024 | 0.53 (0.24, 1.17) | 0.085 | |
| Cutaneous/not specified | 0.45 (0.25, 0.8) | 0.52 (0.29, 0.93) | ||||
| Week 3 | Week 3 NLR ≥ 5 (ref: < 5) | 2.89 (2.05, 4.07) | < 0.001 | 2.82 (2.00, 4.00) | < 0.001 | |
| M stage C (ref = others) | 2.09 (1.38, 3.15) | < 0.001 | 1.97 (1.3, 3.01) | 0.002 | ||
| Melanoma type (ref = mucosal): | Ocular | 0.42 (0.19, 0.94) | 0.006 | 0.48 (0.22, 1.08) | 0.034 | |
| Cutaneous/not specified | 0.39 (0.22, 0.69) | 0.46 (0.25, 0.82) | ||||
| Week 6 | Week 6 NLR ≥ 5 (ref: < 5) | 3.50 (2.37, 5.17) | < 0.001 | 3.37 (2.26, 5.04) | < 0.001 | |
| M stage C (ref = others) | 1.97 (1.26, 3.08) | 0.003 | 1.85 (1.17, 2.92) | 0.008 | ||
| Melanoma type (ref = mucosal): | Ocular | 0.30 (0.13,0.74) | < 0.001 | 0.42 (0.17, 1.04) | 0.005 | |
| Cutaneous/not specified | 0.27 (0.15, 0.51) | 0.36 (0.19, 0.66) | ||||
| Week 9 | Week 9 NLR ≥ 5 (ref: < 5) | 2.26 (1.49,3.43) | < 0.001 | 2.06 (1.33, 3.19) | 0.001 | |
| M stage C (ref = others) | 2.14 (1.30, 3.50) | 0.003 | 2.01 (1.22, 3.33) | 0.006 | ||
| Melanoma type (ref = mucosal): | Ocular | 0.32 (0.12, 0.88) | 0.008 | 0.28 (0.10, 0.78) | 0.038 | |
| Cutaneous/not specified | 0.32 (0.16, 0.66) | 0.45 (0.22, 0.94) | ||||
| PFS | ||||||
| Baseline | Baseline NLR ≥ 5 (ref: < 5) | 1.81 (1.34, 2.45) | < 0.001 | 1.81 (1.33, 2.45) | < 0.001 | |
| M stage C (ref = others) | 2.28 (1.54, 3.38) | < 0.001 | 2.19 (1.48, 3.25) | < 0.001 | ||
| Gender male (ref = female) | 0.66 (0.49, 0.90) | 0.008 | 0.67 (0.50, 0.91) | 0.011 | ||
| Week 3 | Week 3 NLR ≥ 5 (ref: < 5) | 2.37 (1.69, 3.32) | < 0.001 | 2.26 (1.62, 3.17) | < 0.001 | |
| M stage C (ref = others) | 2.19 (1.46, 3.27) | < 0.001 | 2.10 (1.41, 3.14) | < 0.001 | ||
| Gender male (ref = female) | 0.64 (0.46, 0.88) | 0.007 | 0.68 (0.49, 0.94) | 0.018 | ||
| Week 6 | Week 6 NLR ≥ 5 (ref: < 5) | 2.68 (1.82, 3.96) | < 0.001 | 2.51 (1.70, 3.72) | < 0.001 | |
| M stage C (ref = others) | 2.06 (1.34, 3.18) | 0.001 | 1.98 (1.28, 3.06) | 0.002 | ||
| Gender male (ref = female) | 0.63 (0.44, 0.91) | 0.013 | 0.73 (0.50, 1.05) | 0.087 | ||
| Week 9 | Week 9 NLR ≥ 5 (ref: < 5) | 1.95 (1.27, 2.98) | 0.002 | 2.10 (1.40, 3.16) | < 0.001 | |
| M stage C (ref = others) | 2.10 (1.29, 3.42) | 0.003 | 2.02 (1.24, 3.29) | 0.005 | ||
| Gender male (ref = female) | 0.63 (0.42, 0.95) | 0.028 | 0.74 (0.49, 1.12) | 0.015 | ||
Clinical variables not listed in the table were not significant in multivariable analysis of any time point.
The NLR was then investigated in association with clinical benefit with IPI to see if it was an effective predictive biomarker. In univariate analysis, NLR ≥ 5 at any timepoint, either before or during treatment, was statistically correlated with lack of clinical benefit at 12 weeks (Table 3). The association remained in multivariable analysis.
Table 3.
Association between NLR and clinical benefit in IPI group.
| Clinical benefit at 12 weeks |
|||
|---|---|---|---|
| NLR timepoint | NLR < 5 | NLR ≥ 5 | p |
| Baseline (n = 192) | 44% | 19% | < 0.001 |
| Week 3 (n = 181) | 44% | 13% | < 0.001 |
| Week 6 (n = 153) | 50% | 9% | < 0.001 |
| Week 9 (n = 125) | 47% | 16% | 0.001 |
NLR was associated with some clinical endpoints in patients treated with BRAFi. While univariate analysis again demonstrated a baseline NLR ≥ 5 was associated with worse OS and PFS, NLR values at follow-up timepoints were not associated with outcome (Table 4). In multivariable analysis, baseline NLR lost statistical association with both OS and PFS. Additionally, the association of NLR with clinical benefit was not significant (Table 5).
Table 4.
Association of NLR with overall survival and progression free survival in BRAFi group.
| 12 month OS |
12 month PFS |
|||||
|---|---|---|---|---|---|---|
| NLR timepoint | NLR < 5 | NLR ≥ 5 | p | NLR < 5 | NLR ≥ 5 | p |
| Baseline (n = 65) | 66.4% | 35.5% | 0.016 | 29.4% | 9.7% | 0.006 |
| Week 3 (n = 59) | 44.2% | 48.1% | 0.422 | 25.8% | 11.1% | 0.503 |
| Week 6 (n = 53) | 53.5% | 39.4% | 0.253 | 22.6% | 13.6% | 0.198 |
| Week 9 (n = 54) | 59.9% | 30% | 0.078 | 25% | 11.8% | 0.129 |
Table 5.
Association between NLR and clinical benefit in BRAFi group.
| Clinical benefit at 12 weeks |
|||
|---|---|---|---|
| NLR timepoint | NLR < 5 | NLR ≥ 5 | p |
| Baseline (n = 65) | 76% | 65% | 0.413 |
| Week 3 (n = 59) | 69% | 70% | 0.999 |
| Week 6 (n = 53) | 74% | 55% | 0.155 |
| Week 9 (n = 54) | 76% | 60% | 0.230 |
To determine a clinically relevant threshold of change in NLR associated with adverse outcome, we characterized change in NLR over time in both cohorts by stratifying the percentage change from baseline value at any timepoint. While an increase in NLR was not associated with clinical benefit, an increase of 30% of the NLR at any time during therapy was strongly associated with worse OS (HR 1.81, 95%CI 1.27–2.57) and PFS (HR 1.66, 95%CI 1.18–2.31) in IPI-treated patients in multivariable models. In the BRAFi group, magnitude of change in NLR had no correlation with OS, PFS, or clinical response to therapy.
4. Discussion
NLR associates with prognosis in multiple tumor types, as demonstrated by prior reports (Wang et al., 2016, Stotz et al., 2013, Mano et al., 2013, Malietzis et al., 2014, de Martino et al., 2013, Pinato et al., 2014, Perez et al., 2013, Williams et al., 2014, Kelkitli et al., 2014). To our knowledge this is the largest series of patients treated for advanced melanoma with IPI to correlate NLR with both survival outcomes and objective response to therapy, and it is the only series to date that examines the relationship of NLR to outcome in melanoma patients treated with BRAFi. Furthermore, prior reports to date have based their analyses on pretreatment NLR only, while this is the only series to evaluate the meaning of changes in NLR during treatment. Interestingly, we have demonstrated that NLR is highly associated with OS, PFS, and objective response in multivariable analysis for IPI patients, but not for those treated with BRAFi. This suggests a novel interpretation of NLR as a prognostic and potentially predictive biomarker of oncologic outcomes reflecting the unique properties of immunotherapy, but not targeted therapy such as BRAFi.
Ferrucci et al. reported on the associations of NLR with OS and PFS in 187 patients with metastatic melanoma treated with IPI (Ferrucci et al., 2015). Consistent with our findings, pretreatment NLR < 5 was strongly and independently associated with improved OS and PFS. Objective clinical response to treatment was not reported, and only pretreatment NLR values were assessed. A similar study by Zaragoza et al. included 58 patients with metastatic melanoma treated with IPI (Zaragoza et al., 2016). These authors also chose the pretreatment value in the analysis, and correlated this with OS only. Using a cutoff NLR value of 4, high pretreatment NLR was independently associated with worse OS. Additional studies in small groups of patients consistently demonstrate an association of NLR with OS and PFS (Khoja et al., 2016), and taken together support our finding of a strong association of pretreatment NLR with OS and PFS. The current study adds an additional component to our understanding of NLR by demonstrating that changes in NLR during IPI treatment may also predict OS and PFS. This suggests an important dynamic biomarker, as an increase of the NLR during treatment may be a reason to consider changes in treatment earlier in certain clinical scenarios.
Other studies have examined the utility of absolute blood counts in predicting survival of advanced melanoma patients. In a cohort of patients with stage III–IV melanoma treated with surgical resection, absolute lymphocyte count (ALC), a component of NLR, was associated with PFS but not OS in stage IV patients only (Rochet et al., 2015). A larger study of patients treated with biochemotherapy (dacarbazine, cisplatin, or interferon alpha with or without interleukin 2), high absolute neutrophil count (ANC) was predictive of short OS (Schmidt et al., 2007).
In a general cohort of melanoma patients at any stage of disease, NLR was not associated with OS in patients with stage I–III disease (Gandini et al., 2016). However, NLR ≥ 5 was statistically significantly associated with OS in patients with stage IV disease, with a hazard ratio of 2.87. Details of therapy are not presented, but presumably these patients may have received immunotherapy in the course of their treatment. An increasing NLR was also correlated with progression from stage III to stage IV in this study. Therefore, NLR can be considered a marker of advanced disease in general, while also predicting survival in a subset of those with metastatic disease.
The intersection of cancer biology and inflammation has become an important and complex area of study. Inflammation is considered to be one of the hallmarks of cancer, as inflammatory cells may contribute bioactive factors to the tumor microenvironment that ultimately allow for proliferation, angiogenesis, invasion, and limitation of cell death (Hanahan and Weinberg, 2011). For surgical patients in particular, postoperative inflammatory conditions such as infectious complications have been correlated with worse oncologic outcomes, further underlying the complex interaction of systemic inflammation and cancer (Murthy et al., 2007, Tokunaga et al., 2013). The NLR represents a measure of the systemic inflammatory state, and this may account for its association with oncologic outcomes in melanoma and other diseases. Furthermore, there is evidence that NLR may be a strong predictor of survival even in non-cancer populations (Davis et al., 2016), suggesting an intimate association of systemic inflammation with mortality regardless of underlying disease.
The use of immunotherapy to treat advanced melanoma adds further complexity to the understanding of cancer and inflammation, as these agents aim to exploit pre-existing immunity to treat the disease (Hodi et al., 2010). In contrast, targeted agents such as BRAFi target a specific mutation present in some melanomas and therefore act by a different mechanism (Chapman et al., 2011). These differences may explain our observation of associations between NLR and outcomes in IPI patients, but not in BRAFi patients.
Due to the unique clinical properties of immunotherapy, NLR may be an especially useful in biomarker. Because treatment with IPI may show a pattern of delayed but durable clinical responses, clinical benefit is difficult to determine until many weeks after initiation (Wolchok et al., 2009). Furthermore, toxicities may be serious and can include dermatitis, diarrhea, colitis, hepatitis, and hypophysitis (Hodi et al., 2010). Our study demonstrates the association of NLR not only with OS and PFS but also with objective clinical response measured at 12 weeks. Patients with high NLR are less likely to derive clinical benefit (SD, PR, or CR), in addition to having higher risk for progression and death. Pretreatment NLR may aid in decisions about candidacy for therapy, by allowing clinicians to choose patients most likely to have a clinical benefit. NLR during treatment may serve as a simple monitoring test, since we have shown that increases of > 30% from baseline correlate with worse outcomes.
Several limitations of our study should be acknowledged. The population of BRAFi treated patients in this dataset is smaller than that in the IPI group, which may have limited the ability to demonstrate associations of NLR with outcomes in the BRAFi cohort. However, there were no perceivable trends in this group, and we believe the lack of association of NLR with outcome in this group, while being highly associated in IPI treated patients, reflects the unique properties of the their different mechanisms of action. Additionally, our study is a single-institution analysis at a highly specialized cancer referral center, and thus generalizability is a possible limitation. However, the data we present are largely drawn from patients treated in the context of clinical trials, and thus the quality of the prospectively collected data is high. Lastly, there is no standardized value that defines elevated NLR. The studies previously published regarding NLR use a variety of cutoffs, with 5 being a commonly used value. However, any selected value is arbitrarily chosen, and indeed an interpretation of NLR may be more nuanced than stratification into low and high groups based upon an arbitrary value.
As discussed, NLR has been associated with prognosis in a variety of cancers, and in patients undergoing a variety of treatments. It might be assumed that NLR is simply a general prognostic biomarker reflecting a patient's systemic inflammatory state and their anticipated survival irrespective of treatment. Yet our finding that NLR associates with survival outcomes, progression, and clinical benefit in IPI treated patients but not BRAFi treated patients lends support to the concept of NLR as a possible predictive biomarker that can identify a population of patients that are most likely to respond to IPI or potentially other immunotherapies. Future studies will integrate this information into new paradigms that include combination therapies with anti-PD1 agents.
Conflicts of Interest
Michael R Cassidy, MD: None.
Rachel E Wolchok: None.
Junting Zheng, MS: None.
Katherine S Panageas, DrPH: AstraZeneca (Travel).
Jedd D Wolchok, MD PhD: Bristol-Myers Squibb (Consulting or Advisory Role, Travel, Research Funding), Merck (Consulting or Advisory Role, Research Funding), MedImmune (Consulting or Advisory Role, Research Funding), ZIOPHARM Oncology (Consulting or Advisory Role), Polynoma (Consulting or Advisory Role), Polaris (Consulting or Advisory Role), Jounce Therapeutics (Consulting or Advisory Role), Genentech (Consulting or Advisory Role), GlaxoSmithKline (Research Funding), Potenza Therapeutics (Stock), Vesuvius Pharmaceuticals (Stock).
Daniel Coit, MD: None.
Michael A. Postow, MD: Bristol Myers Squibb (Consulting or Advisory Role, Travel, Research Funding), Amgen (Consulting or Advisory Role), Novartis (Consulting or Advisory Role).
Charlotte Ariyan, MD PhD: None.
Author Contributions
Study Design: Cassidy, R Wolchok, Ariyan.
Data Collection: Cassidy, R Wolchok, Ariyan.
Data Analysis: Cassidy, Zheng, Panageas, Ariyan.
Data Interpretation: Cassidy, Zheng, Panageas, J Wolchok, Coit, Postow, Ariyan.
Writing: Cassidy, J Wolchok, Coit, Postow, Ariyan.
Critical Revision: All authors.
Footnotes
This study was supported in part by NIH/NCI P30 CA008748 (Cancer Center Support Grant), with no role in the writing or publication of the manuscript.
References
- Cananzi F.C.M., Dalgleish A., Mudan S. Surgical management of intraabdominal metastases from melanoma: role of the neutrophil to lymphocyte ratio as a potential prognostic factor. World J. Surg. 2014;38:1542–1550. doi: 10.1007/s00268-013-2418-6. [DOI] [PubMed] [Google Scholar]
- Chapman P.B., Hauschild A., Robert C. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011;364:2507–2516. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis J.L., Moutinho V., Panageas K.S., Coit D.G. A peripheral blood biomarker estimates probability of survival: the neutrophil–lymphocyte ratio in noncancer patients. Biomark. Med. 2016;10:953–957. doi: 10.2217/bmm-2016-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrucci P.F., Gandini S., Battaglia A. Baseline neutrophil-to-lymphocyte ratio is associated with outcome of ipilimumab-treated metastatic melanoma patients. Br. J. Cancer. 2015;112:1904–1910. doi: 10.1038/bjc.2015.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandini S., Ferrucci P.F., Botteri E. Prognostic significance of hematological profiles in melanoma patients. Int. J. Cancer. 2016;139:1618–1625. doi: 10.1002/ijc.30215. [DOI] [PubMed] [Google Scholar]
- Hamid O., Robert C., Daud A. Safety and tumor responses with lambrolizumab (anti–PD-1) in melanoma. N. Engl. J. Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D., Weinberg R.A. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Hodi F.S., O'Day S.J., McDermott D.F. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodi F.S., Chesney J., Pavlick A.C. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016;17:1558–1568. doi: 10.1016/S1470-2045(16)30366-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelkitli E., Atay H., Cilingir F. Predicting survival for multiple myeloma patients using baseline neutrophil/lymphocyte ratio. Ann. Hematol. 2014;93:841–846. doi: 10.1007/s00277-013-1978-8. [DOI] [PubMed] [Google Scholar]
- Khoja L., Atenafu E.G., Templeton A. The full blood count as a biomarker of outcome and toxicity in ipilimumab-treated cutaneous metastatic melanoma. Cancer Med. 2016 doi: 10.1002/cam4.878. 10.1002/cam4.878 (published online Sept) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin J., Ascierto P.A., Dréno B. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N. Engl. J. Med. 2014;371:1867–1876. doi: 10.1056/NEJMoa1408868. [DOI] [PubMed] [Google Scholar]
- Malietzis G., Giacometti M., Askari A. A preoperative neutrophil to lymphocyte ratio of 3 predicts disease-free survival after curative elective colorectal cancer surgery. Ann. Surg. 2014;260:287–292. doi: 10.1097/SLA.0000000000000216. [DOI] [PubMed] [Google Scholar]
- Mano Y., Shirabe K., Yamashita Y.-I. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann. Surg. 2013;258:301–305. doi: 10.1097/SLA.0b013e318297ad6b. [DOI] [PubMed] [Google Scholar]
- de Martino M., Pantuck A.J., Hofbauer S. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio in localized nonclear cell renal cell carcinoma. J. Urol. 2013;190:1999–2004. doi: 10.1016/j.juro.2013.06.082. [DOI] [PubMed] [Google Scholar]
- McArthur G.A., Chapman P.B., Robert C. Safety and efficacy of vemurafenib in BRAFV600E and BRAFV600K mutation-positive melanoma (BRIM-3): extended follow-up of a phase 3, randomised, open-label study. Lancet Oncol. 2014 doi: 10.1016/S1470-2045(14)70012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy B.L., Thomson C.S., Dodwell D. Postoperative wound complications and systemic recurrence in breast cancer. Br. J. Cancer. 2007;97:1211–1217. doi: 10.1038/sj.bjc.6604004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez D.R., Baser R.E., Cavnar M.J. Blood neutrophil-to-lymphocyte ratio is prognostic in gastrointestinal stromal tumor. Ann. Surg. Oncol. 2013;20:593–599. doi: 10.1245/s10434-012-2682-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinato D.J., Shiner R.J., Seckl M.J., Stebbing J., Sharma R., Mauri F.A. Prognostic performance of inflammation-based prognostic indices in primary operable non-small cell lung cancer. Br. J. Cancer. 2014;110:1930–1935. doi: 10.1038/bjc.2014.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postow M.A., Chesney J., Pavlick A.C. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N. Engl. J. Med. 2015;372:2006–2017. doi: 10.1056/NEJMoa1414428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto P.A., Yang J.C., Sherry R.M. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin. Cancer Res. 2012;18:2039–2047. doi: 10.1158/1078-0432.CCR-11-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert C., Long G.V., Brady B. Nivolumab in previously untreated melanoma without BRAF mutation. N. Engl. J. Med. 2015;372:320–330. doi: 10.1056/NEJMoa1412082. [DOI] [PubMed] [Google Scholar]
- Robert C., Karaszewska B., Schachter J. Improved overall survival in melanoma with combined dabrafenib and trametinib. N. Engl. J. Med. 2015;372:30–39. doi: 10.1056/NEJMoa1412690. [DOI] [PubMed] [Google Scholar]
- Rochet N.M., Kottschade L.A., Grotz T.E., Porrata L.F., Markovic S.N. The prognostic role of the preoperative absolute lymphocyte count and absolute monocyte count in patients with resected advanced melanoma. Am. J. Clin. Oncol. 2015;38:252–258. doi: 10.1097/COC.0b013e31829b5605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt H., Suciu S., Punt C.J.A. Pretreatment levels of peripheral neutrophils and leukocytes as independent predictors of overall survival in patients with American Joint Committee on Cancer Stage IV Melanoma: results of the EORTC 18951 Biochemotherapy Trial. J. Clin. Oncol. 2007;25:1562–1569. doi: 10.1200/JCO.2006.09.0274. [DOI] [PubMed] [Google Scholar]
- Stotz M., Gerger A., Eisner F. Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br. J. Cancer. 2013;109:416–421. doi: 10.1038/bjc.2013.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Templeton A.J., McNamara M.G., Šeruga B. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl. Cancer Inst. 2014;106:dju124. doi: 10.1093/jnci/dju124. [DOI] [PubMed] [Google Scholar]
- Tokunaga M., Tanizawa Y., Bando E., Kawamura T., Terashima M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann. Surg. Oncol. 2013;20:1575–1583. doi: 10.1245/s10434-012-2720-9. [DOI] [PubMed] [Google Scholar]
- Wang S.C., Chou J.F., Strong V.E., Brennan M.F., Capanu M., Coit D.G. Pretreatment neutrophil to lymphocyte ratio independently predicts disease-specific survival in resectable gastroesophageal junction and gastric adenocarcinoma. Ann. Surg. 2016;263:292–297. doi: 10.1097/SLA.0000000000001189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K.A., Labidi-Galy S.I., Terry K.L. Prognostic significance and predictors of the neutrophil-to-lymphocyte ratio in ovarian cancer. Gynecol. Oncol. 2014;132:542–550. doi: 10.1016/j.ygyno.2014.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchok J.D., Hoos A., O'Day S. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin. Cancer Res. 2009;15:7412–7420. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- Wolchok J.D., Weber J.S., Maio M. Four-year survival rates for patients with metastatic melanoma who received ipilimumab in phase II clinical trials. Ann. Oncol. 2013;24:2174–2180. doi: 10.1093/annonc/mdt161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchok J.D., Kluger H., Callahan M.K. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 2013;369:122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaragoza J., Caille A., Beneton N. High neutrophil to lymphocyte ratio measured before starting ipilimumab treatment is associated with reduced overall survival in patients with melanoma. Br. J. Dermatol. 2016;174:146–151. doi: 10.1111/bjd.14155. [DOI] [PubMed] [Google Scholar]