Abstract
Extramammary Paget's disease (EMPD) is a rare malignant disorder of the skin, which was described in as early as the nineteenth century. EMPD usually occurs as a single lesion in the apocrine sweat gland-bearing skin with abundant hair follicles. Here, we present an elderly man who suffered from a non-resolving chronic genital pruritus for 8 months. Initially, he was managed for recurrent fungal infection and eczema. Later, a diagnosis of the rare condition multiple primary EMPD was made based on the histopathology findings and appropriate treatment was given.
Keywords: Axilla, extramammary, Paget's disease, scrotum, vulva
Case report
A 79-year-old Chinese man was first seen at a general outpatient clinic for itchiness of the skin over the genitalia for 8 months. Initially, he noticed a small red patch at the base of the penis, which gradually enlarged. The lesion was extremely itchy and occasionally became macerated and infected. He had consulted a number of doctors and was prescribed different treatments, without much improvement. His other medical problems included diabetes, dyslipidaemia and hypertension.
Clinically, a large, well-defined erythematous plaque was observed extending from the suprapubic area and involving the skin covering almost the whole of the scrotum and the shaft of the penis (Figure 1).
Figure 1.

Genital lesion: erythematous plaque with focal areas of erosions involving the skin of the scrotum, the penis and the adjacent suprapubic area
Incidental finding of a single well-demarcated brownish patch with central hyperpigmentation (4×5 cm) was noted on the left axilla (Figure 2). The axillary lesion appeared approximately at the same time but was less pruritic. Inguinal lymph and axillary nodes were not palpable bilaterally. Nipple, digital rectal, and other examination results were unremarkable. Symptoms of altered bowel movements, urinary symptoms or constitutional symptoms suggestive of any underlying visceral malignancy were also absent.
Figure 2.

Left axilla: well-demarcated brownish patch with darker central areas
The patient was initially managed as a case of cutaneous candidiasis by the general practitioner. When he did not show any improvement with topical antifungal treatment, the diagnosis was revised to eczema with secondary bacterial infection. He was subsequently treated with oral antihistamines, topical antifungals and topical steroids after different consultations without any improvement. The patient was eventually referred to a dermatology clinic for a second opinion and further management owing to poor response to therapy.
Differential diagnoses of EMPD, inverse psoriasis, candidiasis and Bowen's disease were considered. His full blood count was normal, but renal profile showed mild renal impairment. Serum calcium concentration was 2.45 mmol/L (2.09–2.42), whereas corrected calcium concentration was within normal values, that is, 2.31 mmol/L (2.14–2.58). Urine analysis results were normal. There was no evidence of primary or secondary lesions on chest radiographs. Computerized tomography (CT) of the neck, thorax, abdomen and pelvis did not reveal any abnormalities except for multifocal infarcts on brain CT. Histopathology of skin biopsy from the left axilla showed intra-epidermal proliferation of atypical, large (Paget) cells in nests and single distribution involving the follicular epithelium. These atypical cells had enlarged vesicular nuclei along with prominent nucleoli and pale cytoplasm containing mucin [periodic acid-Schiff (PAS)-positive, diastase resistant] extending throughout the full length of the epidermis. There was no invasion to the underlying dermis or subcutis. Histopathology of the lesion from the groin was similar to that of axilla. Immunohistochemically, the large cells were negative for S100 protein but positive for cytokeratin 7 (CK7) and carcinoembryonic antigen (CEA). Both lesions were also negative for p63 immunohistochemistry marker, which suggested that this was a primary EMPD.1 Fungal elements were absent on PAS and Grocott stains. Based on the investigations and histopathology findings, the diagnosis was confirmed as primary EMPD of the left axilla and the groin. Figures 3–5 display the histopathology and staining of the inguinal lesion.
Figure 3.
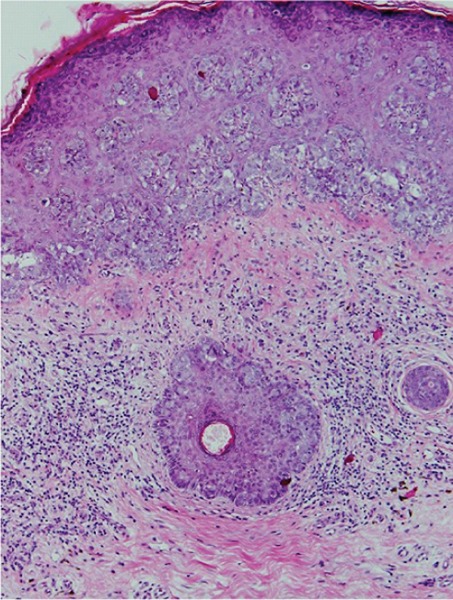
Intra-epidermal proliferation of Paget's cell in nests [10× magnification, haematoxylin and eosin (H&E)]
Figure 5.
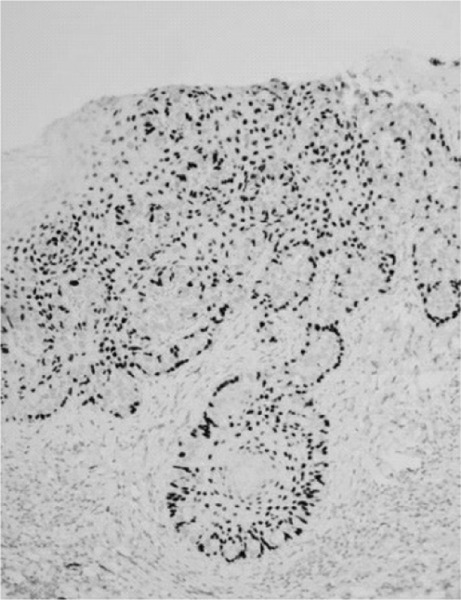
The Paget's cells stained negative for p63
Figure 4.

The Paget's cell stained positive for cytokeratin 7
A combination of surgery and radiotherapy was planned for the patient. The lesion on the left axilla was planned for excision because it was smaller, whereas radiotherapy was planned for the groin lesion owing to its extensive involvement.
Discussion
EMPD is a slow-growing adenocarcinoma developing in the apocrine gland-bearing skin, such as vulva, perianal, axilla and penoscrotal areas.2 Rarely, the sites devoid of this gland, such as the back and umbilicus, have also been involved.3,4 EMPD is similar to Paget's disease of the breast except that it occurs in sites away from the breast and is more common among the elderly. EMPD is a rare skin disorder usually occurring at a single site. Although multiple-site involvement of EMPD is uncommon, a number of cases have reported concurrent multiple EMPD, especially from Japan.2,3
The exact relationship between EMPD and an underlying malignancy is uncertain. It is believed that up to 42% of patients with EMPD may have an underlying primary or non-cutaneous malignancy.5 EMPD is generally classified as primary or secondary. Primary EMPD arises from the intra-epidermal cells and is generally not associated with any underlying carcinoma. In a recent finding, Toker cells were postulated as the precursor for primary EMPD.6 Secondary EMPD, in contrast, has a non-cutaneous origin and is associated with underlying adnexal or visceral carcinoma, commonly of rectal or urothelial origin.7 However, penoscrotal EMPD may have a lower incidence of internal malignancy (9%), mainly originating from the genitourinary system.8 Axillary lesions may be associated with breast malignancy. Hence, the diagnosis of EMPD warrants the search for possible underlying malignancy, particularly in younger patients and those with perianal or invasive disease.9,10
The initial diagnosis of EMPD is often delayed or missed such as in this case, as its symptoms and morphology mimics those of various types of dermatoses, for example, flexural psoriasis, seborrhoeic dermatitis, eczema, candidiasis, tinea cruris and erythrasma. Heavy pigmentation of the lesion may be misdiagnosed as malignant melanoma.11 In cases of multiple EMPD, two to four lesions may occur concurrently at different sites.2,4,9
The standard management strategy for primary EMPD is wide surgical excision; however, the recurrence rate is high (20%–50%).12 Other options include radiotherapy, chemotherapy, photodynamic therapy or laser therapy depending on the site and extent of the lesion. Radiotherapy is more suitable for extensive involvement, for lesions located at a site where excision would be difficult or when the patient is unfit for surgery.9
Recently, topical imiquimod, which is an immune response modifier, used as first line therapy, showed an 80% cure rate with minimal side effects. It may be considered in situations where the lesion is extensive or in cases where surgical excision is not a suitable option, for example, advanced age or due to concurrent multiple medical conditions. However, data pertaining to recurrence after treatment with imiquimod are still lacking.13
In general, the prognosis for primary EMPD is favourable provided that it is detected early and given adequate treatment.4 Ishihara et al. reported that some patients with both axillary and genital involvement did not develop invasive carcinoma even after many years of post-treatment follow-up.14
Conclusion
EMPD, although rare, must be considered as a differential diagnosis in elderly patients presenting with chronic dermatitis or candidiasis, especially when the condition does not respond to adequate therapy. Patients presenting with clinical suspicion of EMPD should be examined for the possibility of multiple site involvement, such as in this case. In suspected cases of secondary EMPD, investigation for primary malignancy in the gastrointestinal or genitourinary systems is necessary. Although primary EMPD is highly recurrent, the overall prognosis is promising, especially for smaller lesions and those detected early.
Acknowledgement
The authors would like to thank the patient for his consent to publish this case and the images. We also like to thank Dr. Suria Hayati and Dr. Fazarina from Department of Pathology of Universiti Kebangsaan Malaysia Medical Centre for the histopathology images and interpretation.
Footnotes
Leelavathi M, Norazirah MN, Nur Amirah AP. Multiple concurrent primary extramammary Paget's disease. Malays Fam Physician. 2016;11(1);18–21.
References
- 1.Yanai H, Takahashi N, Omori M. et al. Immunohistochemistry of P63 in primary and secondary valvular Paget's disease. Pathol Int. 2008;58:648–51. doi: 10.1111/j.1440-1827.2008.02284.x. [DOI] [PubMed] [Google Scholar]
- 2.Sawada Y, Bito T, Kabashima R. et al. Ectopic extramammary Paget's disease: Case report and literature review. Acta Derm Venereol. 2010;90(5):502–5. doi: 10.2340/00015555-0892. [DOI] [PubMed] [Google Scholar]
- 3.Kawatsu T, Miki Y. Triple extramammary Paget's disease. Arch Dermatol. 1971;104:316–9. [PubMed] [Google Scholar]
- 4.Abe S, Kabashima K, Nishio D. et al. Quadruple extra-mammary Paget's disease. Acta Derm Venereol. 2007;87(1):80–1. doi: 10.2340/00015555-0169. [DOI] [PubMed] [Google Scholar]
- 5.Lai YL, Yang WG, Tsay PK. et al. Penoscrotal extramammary Paget's disease: A review of 33 cases in a 20-year experience. Plast Reconstr Surg. 2003;112(4):1017–23. doi: 10.1097/01.PRS.0000076193.67701.6A. [DOI] [PubMed] [Google Scholar]
- 6.Hashemi P, Kao GF, Konia T. et al. Multicentric primary extramammary Paget disease: A Toker cell disorder? Cutis. 2014;94(1):35–8. [PubMed] [Google Scholar]
- 7.Chanda JJ. Extramammary Paget's disease: Prognosis and relationship to internal malignancy. J Am Acad Dermatol. 1985;13(6):1009–14. doi: 10.1016/s0190-9622(85)70254-x. [DOI] [PubMed] [Google Scholar]
- 8.Park S, Grossfeld GD, McAninch JW. et al. Extramammary Paget's disease of the penis and scrotum: excision, reconstruction and evaluation of occult malignancy. J Urol. 2001;166(6):2112–7. doi: 10.1016/s0022-5347(05)65516-4. [DOI] [PubMed] [Google Scholar]
- 9.Li B, Ding Q. Extramammary Paget's disease involving the penis, scrotum and the axilla. Australas J Dermatol. 2011;52(1):e18–20. doi: 10.1111/j.1440-0960.2009.00619.x. [DOI] [PubMed] [Google Scholar]
- 10.Chiu TW, Wong PS, Ahmed K. et al. Extramammary Paget's disease in Chinese males: A 21-year experience. World J Surg. 2007;31(10):1941–6. doi: 10.1007/s00268-007-9189-x. [DOI] [PubMed] [Google Scholar]
- 11.Hilliard NJ, Huang C, Andea A. Pigmented extramammary Paget's disease of the axilla mimicking melanoma: Case report and review of the literature. J Cutan Pathol. 2009;36(9):995–1000. doi: 10.1111/j.1600-0560.2009.01174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tonguc E, Gungor T, Var T. et al. Treatment of recurrent vulvar Paget disease with imiquimod cream: A case report and review of the literature. Arch Gynecol Obstet. 2011;283:97–101. doi: 10.1007/s00404-010-1653-4. [DOI] [PubMed] [Google Scholar]
- 13.Iavazzo C, Ntziora F, Karachalios C. et al. The clinical evidence and the role of imiquimod in the extramammary Paget disease. Acta Dermato Venerol Croat. 2014;22(2):103–9. [PubMed] [Google Scholar]
- 14.Ishihara K. Statistical study of extramammary Paget's disease in Japan. Skin Cancer. 1994;9:38. [Google Scholar]


