Abstract
Abstract: Objectives: Early psychopathology in children diagnosed with Bipolar Disorder (BD) remains poorly characterized. Parental retrospective reports provide helpful details on the earliest manifestations and their evolution over time. These symptoms occur early in the course of BD, often before a formal diagnosis is made and/or treatment is implemented, and are of great importance to early recognition and prevention.
Methods: Parents of pre-pubertal children and adolescents with DSM-IV diagnoses of BD attending an outpatient mood disorders clinic provided retrospective ratings of 37 symptoms of child psychopathology. Stability and comorbidity of diagnoses were evaluated, and severity of symptoms for each subject was assessed by identifying the earliest occurrence of the reported symptoms causing impairment.
Results: Severe mood instability, temper tantrums, anxiety symptoms, sleep disturbances and aggression were among the most common signs of psychopathology reported in children diagnosed with BD before puberty. Symptoms were already apparent in the first three years in 28%, and formal diagnoses were made before the age of 8 y in the majority of cases.
Conclusions: Retrospective parental reports of early symptoms of psychopathology in pre-pubertal children with BD revealed a very early occurrence of affective precursors (irritability and mood dysregulation) and clinical risk factors like impulsive aggression and anxiety that can precede the syndromal onset of mania by several years. These findings support previous reports suggesting a progression of symptoms from abnormal, non-specific presentations to sub-threshold and finally syndromal BD. The importance of early identification and intervention is discussed.
Keywords: Adolescent, bipolar disorder, children, onset, parents, prodromes, psychopathology
INTRODUCTION
Bipolar Disorder (BD) is a debilitating psychiatric disorder characterized by discrete periods of mood instability, circadian disruption, and abnormal shifts in energy, activity levels, and cognitive processes. BD (type-1, -2 and NOS) has an estimated lifetime prevalence of 4.5% in adults in the United States [1] and 1.8% in children globally [2]. Among adults with BD, 50% reported syndromal onset before the age of 18, a greater number of acute episodes, higher rates of comorbidities, rapid cycling, and long delays to treatment [3, 4]. Early presentations of childhood and adolescent onset of BD often include fewer symptoms, shorter episodes, or sub-threshold symptoms, falling into the BD-NoS (bipolar disorder not otherwise specified) diagnostic category [5, 6].
BD youths often present with comorbid psychiatric disorders, with high rates reported for anxiety disorders (54%), and externalizing disorders such as attention deficit-hyperactivity disorder (ADHD) (48%), disruptive behavior disorder (31%), and substance use disorder (31%) [7]. Comorbid ADHD and anxiety symptoms in pediatric BD was associated with increased symptoms and impairment in several domains of functioning [7]. The controversies characterizing the diagnosis of pediatric BD stem from: 1) the vague characterization and lack of specificity of its prodromal features; 2) the use of adult criteria to diagnose children and adolescents; 3) the high rates of symptomatic overlap and comorbidity with other childhood-onset disorders. Although all forms of BD have been described in pre-pubertal children, a majority of cases onset with atypical features (BD- NOS). These cases do not meet diagnostic criteria for hypomania due to short duration or an insufficient number of symptoms, but often progress towards BD type I or type II [5, 6].
The revisions in the DSM-V did not account for the developmental differences in BD symptom presentations between pediatric and adult populations [8]. Before crossing the diagnostic threshold, BD presents with a variety of symptoms and behaviors, as well documented in retrospective, prospective and high-risk studies [9-11]. Fergus (2003) identified four components explaining 50% of the variance in the symptomatology of patients with or without BD (depression, irritability – dyscontrol, mania and psychosis – suicidality), using a parent-rated survey of 37 common symptoms of DSM-IV childhood-onset disorders. Children with community diagnoses of BD experienced symptoms of the irritability - dyscontrol component earlier (age three) and more frequently than the other groups; the depression, mania and psychosis – suicidality components were able to discriminate BD case only at later ages (seven, eight and nine, respectively). The same group [10] analyzed retrospective parental ratings of yearly symptom presentations in pediatric outpatients with K- SADS diagnoses of BD and ADHD in order to determine whether early symptoms (or symptom clusters) can discriminate between the two disorders. Symptoms of brief and extended mood elevations distinguished BD from ADHD as early as age three. Other early discriminating symptoms included severe irritability and a decreased need for sleep whereas common symptoms of depression (sadness, changes in appetite, and suicidal ideation) were only able to differentiate BD and ADHD at about age seven. Children with BD diagnoses were also more likely to have symptoms of night terrors, night time enuresis, and physical complaints compared to those with ADHD. Not surprisingly, symptoms common to mania and ADHD (hyperactivity, inattention, and impulsivity) were unlikely to differentiate between ADHD and BD diagnostic groups. However, symptoms of anxiety, obsessions, compulsions, and poor frustration tolerance also did not differ significantly between groups.
Prospective longitudinal studies offer the most accurate and unbiased data [11, 12], but much about the early presentation and evolution of BD can be evinced from retrospective observations in children with BD, especially if diagnosed early in the course of their illness. Since recurrent episodes and treatments probably modify the clinical features of BD, studying BD early in its course can minimize any confounder due to its course or treatment. Similarly, studies of children at genetic risk for BD have documented the heterogeneity of psychopathological manifestations [13-17]. Studies of children with BD have evidenced the uncertain diagnostic value of some ADHD-like symptoms such as hyperactivity, impulsivity, irritability and distractibility [9, 10, 18, 19]. In an attempt to further clarify the symptoms’ onset, co-occurrence and evolution in pediatric BD, we used the same parental survey of psychopathology in an independent cohort of children with BD.
METHODS
Outpatients were recruited for participation from the Lucio Bini Mood Disorders Center (LBMDC), an outpatient specialty clinic in New York, NY, between 1998 and 2008. The study was approved by a private IRB (Liberty IRB, DeLand, FL).
Participants were recruited from existing outpatients whose families consented to complete a battery of questionnaires and a structured diagnostic interview. All parents and patients provided oral and written informed consent and assent for participation in the clinical evaluation, diagnostic interviews, and rating scale completion. Children were assessed by direct observation and diagnostic interview with their parent/s, as part of their clinical evaluation. The diagnostic status was assessed by parental K-SADS-PL interview, providing DSM-IV current and lifetime diagnoses. We used COBY criteria for the diagnosis of BD-NOS [6]. Parental ratings of symptoms for each year of the child’s life were obtained with a survey of early psychopathology derived from the DSM-IV previously used in the assessment of longitudinal course of childhood psychopathology in other cohorts with community [9] or K-SADS [10] diagnoses of BD. We obtained ratings on 35 symptoms, removing from the scale two symptoms (mute and tics) rarely endorsed in previous studies using the same instrument. Symptoms were rated for each year of the child’s life on a severity of impairment scale (0=not present; 1=mild; 2=moderate; 3=severe). Only symptoms that were impairing (score 2 or 3) were analyzed in this study.
RESULTS
The sample consisted of 83 patients, 60% males, ranging in age from 5 to 17 (mean age=9.4, SD 3.8 years). There were 24 BD type I, 8 BD type II and 51 BD-NOS. Demographic, socio-economic characteristics, comorbidity and clinical variables are presented in Table 1.
Table 1. Demographics and comorbidities by Bipolar subtype.
| Bipolar NOS (n=51) | Bipolar I (n=24) | Bipolar II (n=8) | All (n=83) | |
|---|---|---|---|---|
| Age at time of study, mean ± SD | 9.0 ± 3.93 | 9.9 ± 3.59 | 10.5 ± 4.34 | 9.4 ± 3.86 |
| Socioeconomic status, n (%) | ||||
| 0-29 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| 30-39 | 8 (0%) | 3 (3%) | 2 (2%) | 13 (16%) |
| 40-54 | 24 (29%) | 7 (8%) | 4 (5%) | 35 (42%) |
| 55-66 | 19 (23%) | 14 (17%) | 2 (2%) | 35 (42%) |
| Gender, n (%) | ||||
| Male | 31 (37%) | 14 (16%) | 5 (6%) | 50 (60%) |
| Female | 20 (24%) | 10 (12%) | 3 (3%) | 33 (40%) |
| Adoption Status, n (%) | ||||
| Adopted | 10 (12%) | 4 (5%) | 1 (1%) | 15 (18%) |
| Not Adopted | 41 (49%) | 20 (24%) | 7 (8%) | 68 (82%) |
| Family psychiatric disorder, n (%) | 46 (55%) | 22 (26%) | 6 (7%) | 74 (89%) |
| Comorbidity, n (%) | ||||
| ADHD | 33 (40%) | 15 (18%) | 3 (4%) | 51 (61%) |
| Oppositional Defiant Disorder | 26 (31%) | 13 (16%) | 2 (2%) | 41 (50%) |
| Simple/Social Phobia | 16 (19%) | 5 (6%) | 5 (6%) | 26 (31%) |
| Separation Anxiety Disorder | 11 (13%) | 8 (10%) | 2 (2%) | 21 (25%) |
| Generalized Anxiety Disorder | 9 (11%) | 8 (10%) | 3 (4%) | 20 (24%) |
| Panic Disorder/Agoraphobia | 7 (8%) | 6 (7%) | 3 (4%) | 16 (19%) |
| OCD | 11 (13%) | 3 (4%) | 0 (0%) | 14 (17%) |
| Psychotic Features | 7 (8%) | 6 (7%) | 0 (0%) | 13 (16%) |
| Conduct Disorder | 7 (8%) | 2 (2%) | 1 (1%) | 10 (12%) |
| Motor/Vocal Tic Disorders | 7 (8%) | 1 (1%) | 0 (0%) | 8 (10%) |
| Enuresis | 3 (4%) | 0 (0%) | 1 (1%) | 4 (5%) |
Note: All percentages are rounded to the nearest whole number; ADHD = Attention Deficit/Hyperactivity Disorder; OCD= Obsessive-Compulsive Disorder; NOS = Not otherwise specified.
The total number of symptoms reported in each age–epoch increased from 79 in the first year, to 145 before age 3, 436 and 454 before age 7 and 12, decreasing by age 12-18 to 175. Almost all the psychopathology reported in the first year of life was found in BD-NOS (73%) and BD type I (21%). Before age 3, 28% of the sample manifested severe, impairing psychopathology (see Fig. 1).
Fig. (1).
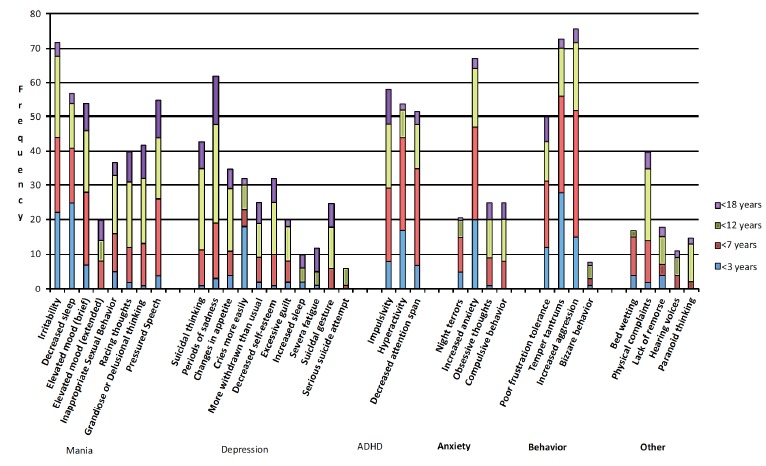
Frequencies of psychiatric symptoms by age in Bipolar patients (n=83).
The most frequently reported symptoms (>20%) were: decreased sleep, irritability, temper tantrums and increased anxiety. Additionally, affective symptoms such as frequent crying, poor frustration tolerance, hyperactivity and aggression were reported in more than 10% of patients before the age of 3 years, supporting published reports of early psycho- pathology observed in pediatric BD.
By the age of 7, the most frequent parent reported symptoms included: temper tantrums (56%), aggression (52%), anxiety (47%), decreased attention span (45%), hyperactivity (43%), irritability (42%), and decreased sleep (41%). While less frequent but perhaps more unique to BD were reported symptoms of poor frustration tolerance (31%), brief elevated mood (28%), pressured speech (25%), hypersexual behavior (16%), grandiosity and racing thoughts (12%). Bedwetting (17%), and somatic complaints (16%), symptoms usually associated with depression and/or anxiety, also occurred often. The mean age of onset of psychiatric symptoms was significantly lower in children with BD-NOS and those with comorbid ADHD compared to children without comorbid ADHD (F=5.04, p<0.05). There were no significant differences between groups when most severe manic or depressive episodes were compared (F=1.67, p>0.05).
We were not able to replicate in our sample the four factors identified in a previous study [10] as contributing to 50% of the variance (Data not shown).
DISCUSSION
In our study, parental reports of disabling psycho- pathology in children with a K-SADS diagnosis of BD were consistent with previous reports of prodromal features of BD in youths [6, 9, 10, 15, 20, 21] and adults with an early onset of illness [3, 4, 22, 23]. Symptoms severe enough to be considered disabling were found in the first year of life in children later diagnosed with BD-NOS, BD-I but not in BD-II, pointing to a possible later age of onset in this subtype. Also, in the first three years of life the symptoms of emotional dysregulation, disturbances of sleep and arousal, impulsivity and aggression were prominent. These symptoms were persistent, and their chronicity is confirmed by their clinical course.
Both affective psychopathology (clinical precursors) and non-affective psychopathology (risk factors) were reported several years before the diagnosis of BD was made, and often before any treatment [11, 12]. This is consistent with the retrospective reports of Fergus and Luckenbaugh [9,10] but also with findings from prospective longitudinal studies of community and clinical samples [6] and from studies of youth at familial risk [13-17].
In prospective studies, the findings are suggestive of precursors such as mood swings, sleep disturbances and fluctuating level of activity (from hyperactivity to hypoactivity and psychomotor retardation) [11]. However, as most of the cases had a positive family history for mood or substance use disorder, these results might not apply to all cases of BD. Nevertheless, there are similarities between our findings and studies of early psychopathology in adults diagnosed with BD [3, 4].
Similar to the study by Luckenbaugh [10], we found elevated rates of severe irritability, sleep disturbances, impulsivity and hyperactivity before age 3. Fergus [9] reported that only irritability, decreased sleep or hypersexual behavior distinguished BD from ADHD. Since we did not have a control population, we can only report on the consistency of these findings with other cohorts with juvenile BD. However, in our sample, subjects with BD-NOS or with comorbid ADHD were more symptomatic, and from an earlier age. The relative contribution of manic, depressive, anxiety related and psychotic symptoms to impairment in children prior to the diagnosis of a psychiatric disorder remains poorly characterized. Our data adds to the evidence of both mood (tearfulness, irritability) and non-mood related symptoms (anxiety, enuresis) may precede the onset of bipolar disorders, and suggests the value of tracking symptoms regardless of their clear connection with the final outcome.
We found no evidence that excitatory symptoms consistently preceded the onset of depression, as postulated by Koukopoulos and Ghaemi [24]. Rather, symptoms of emotional lability, including elevated symptoms of anxiety were associated with hyperactivity and sleep disturbances with circadian dysregulation. However, these preliminary findings are insufficient to address questions about onset polarity and predominant manic vs. depressive vs. mixed symptomatology.
The study has several strengths: 1) the study relied solely on parents' reports rather than subjective accounts. Patients’ subjective experience may be biased by poor recall, lack of insight and potential negative effects of manic and depressive symptoms on memory; 2) the parents were not aware of the research question other than the description of early psychiatric symptoms, and therefore it is unlikely that parents were biased towards over- or under-reporting of any symptom or symptoms’ cluster or the age of occurrence; 3) we used an established instrument for eliciting and reporting childhood psychopathology; 4) BD diagnoses were confirmed by structured clinical interviews; 5) since the ratings were obtained early in the course of the patients life, the time delay between symptoms’ onset and data collection was short, compared to other retrospective studies (especially in adults), limiting recall bias; 6) we included all subtypes of BD, especially cyclothymia, often not diagnosed or assessed in most studies of childhood-onset BD. We avoided selecting cases based on the presence of mania or psychotic symptoms, thus focusing on psychopathology preceding the first episode, allowing for a broader assessment of early psychopathology.
Limitations of this study include: 1) the design of the study is observational; 2) no control group available for comparison; 3) parents were specifically asked about some symptoms rather than rely on spontaneous reporting; 4) while we did not formally assess the psychiatric health of the parent reporting on their child, parents were considered to be good historian and reliable reporters; 5) school reports were consistently reviewed, but no formal assessment of teachers’ reports was used; and 6) the retrospective nature of the study. Given the higher prevalence of psychopathology at home, rather than in school or social settings, this might lead to an under- estimation of psychopathology; 6) as this was a convenience sample, we cannot generalize these findings to all pediatric patients with bipolar disorder. There is growing evidence from the literature and in the data presented here for both, homotypic and heterotypic development of BD: BD develops from attenuated mood symptoms, affective temperaments and sleep disturbances, but sometimes cognitive, anxiety or attention deficit disorders precede the onset of bipolar disorder. Further evaluation of possible developmental trajectories and their specificity for different bipolar subtypes can help identify and intervene early in the course of the illness, possibly reducing morbidity and mortality, and improving treatment response and outcome.
ACKNOWLEDGEMENT
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Merikangas K.R., Akiskal H.S., Angst J., Greenberg P.E., Hirschfeld R.M., Petukhova M., Kessler R.C. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch. Gen. Psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543. [http://dx.doi.org/10.1001/archpsyc.64.5.543]. [PMID: 17485606]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Meter A.R., Moreira A.L., Youngstrom E.A. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J. Clin. Psychiatry. 2011;72(9):1250–1256. doi: 10.4088/JCP.10m06290. [http://dx.doi.org/10.4088/ JCP.10m06290]. [PMID: 21672501]. [DOI] [PubMed] [Google Scholar]
- 3.Leverich G.S., Post R.M., Keck P.E., Jr, Altshuler L.L., Frye M.A., Kupka R.W., Nolen W.A., Suppes T., McElroy S.L., Grunze H., Denicoff K., Moravec M.K., Luckenbaugh D. The poor prognosis of childhood-onset bipolar disorder. J. Pediatr. 2007;150(5):485–490. doi: 10.1016/j.jpeds.2006.10.070. [http://dx.doi.org/10.1016/j.jpeds.2006.10. 070]. [PMID: 17452221]. [DOI] [PubMed] [Google Scholar]
- 4.Perlis R.H., Dennehy E.B., Miklowitz D.J., Delbello M.P., Ostacher M., Calabrese J.R., Ametrano R.M., Wisniewski S.R., Bowden C.L., Thase M.E., Nierenberg A.A., Sachs G. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: results from the STEP-BD study. Bipolar Disord. 2009;11(4):391–400. doi: 10.1111/j.1399-5618.2009.00686.x. [http://dx.doi.org/10.1111/j.1399-5618.2009.00686.x]. [PMID: 19500092]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birmaher B., Axelson D., Goldstein B., Strober M., Gill M.K., Hunt J., Houck P., Ha W., Iyengar S., Kim E., Yen S., Hower H., Esposito-Smythers C., Goldstein T., Ryan N., Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am. J. Psychiatry. 2009;166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569. [http:// dx.doi.org/10.1176/appi.ajp.2009.08101569]. [PMID: 19448190]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Axelson D.A., Birmaher B., Strober M.A., Goldstein B.I., Ha W., Gill M.K., Goldstein T.R., Yen S., Hower H., Hunt J.I., Liao F., Iyengar S., Dickstein D., Kim E., Ryan N.D., Frankel E., Keller M.B. Course of subthreshold bipolar disorder in youth: diagnostic progression from bipolar disorder not otherwise specified. J. Am. Acad. Child Adolesc. Psychiatry. 2011;50(10):1001–16.e3. doi: 10.1016/j.jaac.2011.07.005. [http://dx.doi.org/10.1016/j.jaac.2011.07.005]. [PMID: 21961775]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frías Á., Palma C., Farriols N. Comorbidity in pediatric bipolar disorder: prevalence, clinical impact, etiology and treatment. J. Affect. Disord. 2015;174:378–389. doi: 10.1016/j.jad.2014.12.008. [http://dx.doi.org/10.1016/ j.jad.2014.12.008]. [PMID: 25545605]. [DOI] [PubMed] [Google Scholar]
- 8.Safer D.J., Rajakannan T., Burcu M., Zito J.M. Trends in subthreshold psychiatric diagnoses for youth in community treatment. JAMA Psychiatry. 2015;72(1):75–83. doi: 10.1001/jamapsychiatry.2014.1746. [http://dx.doi.org/ 10.1001/jamapsychiatry.2014.1746]. [PMID: 25426673]. [DOI] [PubMed] [Google Scholar]
- 9.Fergus E.L., Miller R.B., Luckenbaugh D.A., Leverich G.S., Findling R.L., Speer A.M., Post R.M. Is there progression from irritability/dyscontrol to major depressive and manic symptoms? A retrospective community survey of parents of bipolar children. J. Affect. Disord. 2003;77(1):71–78. doi: 10.1016/s0165-0327(02)00176-3. [http://dx.doi.org/10.1016/ S0165-0327(02)00176-3]. [PMID: 14550937]. [DOI] [PubMed] [Google Scholar]
- 10.Luckenbaugh D.A., Findling R.L., Leverich G.S., Pizzarello S.M., Post R.M. Earliest symptoms discriminating juvenile- onset bipolar illness from ADHD. Bipolar Disord. 2009;11(4):441–451. doi: 10.1111/j.1399-5618.2009.00684.x. [http://dx.doi.org/10.1111/j.1399-5618.2009.00684.x]. [PMID: 19500097]. [DOI] [PubMed] [Google Scholar]
- 11.Faedda G.L., Marangoni C., Serra G., Salvatore P., Sani G., Vázquez G.H., Tondo L., Girardi P., Baldessarini R.J., Koukopoulos A. Precursors of bipolar disorders: a systematic literature review of prospective studies. J. Clin. Psychiatry. 2015;76(5):614–624. doi: 10.4088/JCP.13r08900. [http://dx.doi.org/10.4088/JCP.13r08900]. [PMID: 26035191]. [DOI] [PubMed] [Google Scholar]
- 12.Faedda G.L., Serra G., Marangoni C., Salvatore P., Sani G., Vázquez G.H., Tondo L., Girardi P., Baldessarini R.J., Koukopoulos A. Clinical risk factors for bipolar disorders: a systematic review of prospective studies. J. Affect. Disord. 2014;168:314–321. doi: 10.1016/j.jad.2014.07.013. [http://dx.doi.org/10.1016/j.jad.2014.07.013]. [PMID: 25086290]. [DOI] [PubMed] [Google Scholar]
- 13.Nurnberger J.I., Jr, McInnis M., Reich W., Kastelic E., Wilcox H.C., Glowinski A., Mitchell P., Fisher C., Erpe M., Gershon E.S., Berrettini W., Laite G., Schweitzer R., Rhoadarmer K., Coleman V.V., Cai X., Azzouz F., Liu H., Kamali M., Brucksch C., Monahan P.O. A high-risk study of bipolar disorder. Childhood clinical phenotypes as precursors of major mood disorders. Arch. Gen. Psychiatry. 2011;68(10):1012–1020. doi: 10.1001/archgenpsychiatry.2011.126. [http:// dx.doi.org/10.1001/archgenpsychiatry.2011.126]. [PMID: 21969459]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Egeland J.A., Endicott J., Hostetter A.M., Allen C.R., Pauls D.L., Shaw J.A. A 16-year prospective study of prodromal features prior to BPI onset in well Amish children. J. Affect. Disord. 2012;142(1-3):186–192. doi: 10.1016/j.jad.2012.04.023. [http://dx.doi.org/10.1016/j.jad.2012.04.023]. [PMID: 22771141]. [DOI] [PubMed] [Google Scholar]
- 15.Duffy A., Alda M., Hajek T., Sherry S.B., Grof P. Early stages in the development of bipolar disorder. J. Affect. Disord. 2010;121(1-2):127–135. doi: 10.1016/j.jad.2009.05.022. [http://dx.doi.org/10.1016/j.jad.2009.05.022]. [PMID: 19541368]. [DOI] [PubMed] [Google Scholar]
- 16.Reichart C.G., van der Ende J., Wals M., Hillegers M.H., Nolen W.A., Ormel J., Verhulst F.C. The use of the GBI as predictor of bipolar disorder in a population of adolescent offspring of parents with a bipolar disorder. J. Affect. Disord. 2005;89(1-3):147–155. doi: 10.1016/j.jad.2005.09.007. [http://dx.doi.org/10.1016/j.jad.2005.09.007]. [PMID: 16260043]. [DOI] [PubMed] [Google Scholar]
- 17.Mesman E., Nolen W.A., Reichart C.G., Wals M., Hillegers M.H. The Dutch bipolar offspring study: 12-year follow-up. Am. J. Psychiatry. 2013;170(5):542–549. doi: 10.1176/appi.ajp.2012.12030401. [http://dx.doi.org/10.1176/appi. ajp.2012.12030401]. [PMID: 23429906]. [DOI] [PubMed] [Google Scholar]
- 18.Biederman J., Mick E., Faraone S.V., Spencer T., Wilens T.E. Wozniak, J. Pediatric mania: a developmental subtype of bipolar disorder? Biol. Psychiatry. 2000;48(6):458–466. doi: 10.1016/s0006-3223(00)00911-2. [http://dx.doi. org/10.1016/S0006-3223(00)00911-2]. [PMID: 11018219]. [DOI] [PubMed] [Google Scholar]
- 19.Findling R.L., Gracious B.L., McNamara N.K., Youngstrom E.A., Demeter C.A., Branicky L.A., Calabrese J.R. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord. 2001;3(4):202–210. [http://dx. doi.org/10.1034/j.1399-5618.2001.30405.x]. [PMID: 11552959]. [PubMed] [Google Scholar]
- 20.Dilsaver S.C., Akiskal H.S. Mixed hypomania in children and adolescents: is it a pediatric bipolar phenotype with extreme diurnal variation between depression and hypomania? J. Affect. Disord. 2009;116(1-2):12–17. doi: 10.1016/j.jad.2008.10.016. [http://dx.doi.org/10.1016/j.jad.2008.10. 016]. [PMID: 19007995]. [DOI] [PubMed] [Google Scholar]
- 21.Hillegers M.H., Reichart C.G., Wals M., Verhulst F.C., Ormel J., Nolen W.A. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disord. 2005;7(4):344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [http://dx.doi.org/10.1111/j.1399-5618.2005. 00215.x]. [PMID: 16026487]. [DOI] [PubMed] [Google Scholar]
- 22.Post R.M., Leverich G.S., Kupka R.W., Keck P.E., Jr, McElroy S.L., Altshuler L.L., Frye M.A., Luckenbaugh D.A., Rowe M., Grunze H., Suppes T., Nolen W.A. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J. Clin. Psychiatry. 2010;71(7):864–872. doi: 10.4088/JCP.08m04994yel. [http://dx.doi.org/ 10.4088/JCP.08m04994yel]. [PMID: 20667291]. [DOI] [PubMed] [Google Scholar]
- 23.Berk M., Dodd S., Callaly P., Berk L., Fitzgerald P., de Castella A.R., Filia S., Filia K., Tahtalian S., Biffin F., Kelin K., Smith M., Montgomery W., Kulkarni J. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J. Affect. Disord. 2007;103(1-3):181–186. doi: 10.1016/j.jad.2007.01.027. [http://dx.doi.org/10. 1016/j.jad.2007.01.027]. [PMID: 17324469]. [DOI] [PubMed] [Google Scholar]
- 24.Koukopoulos A., Ghaemi S.N. The primacy of mania: a reconsideration of mood disorders. Eur. Psychiatry. 2009;24(2):125–134. doi: 10.1016/j.eurpsy.2008.07.006. [http://dx.doi.org/10.1016/j.eurpsy.2008.07.006]. [PMID: 18789854]. [DOI] [PubMed] [Google Scholar]


