Abstract
Background: Cyclicity is the essential feature of Bipolar disorder, but the effect of different cycle patterns on the clinical features is poorly understood. Moreover, no studies investigated the relationship between mania and depression inside the manic-depressive cycle.
Objective: The aim of this study is to verify the presence of a relationship between the manic and the depressive phase during the course of bipolar disorder.
Method: 160 consecutive patients with BD type I were recruited and followed for a mean period of 10 years. During the follow-up period, four types of euthymic phases were collected: free intervals present between a depressive and a manic/hypomanic episode (D-M); free intervals present between a manic/hypomanic and a depressive episode (M-D); free intervals present between two depressive episodes (D-D); free intervals present between two manic/hypomanic episodes (M-M). One-way ANOVA using the groups as independent variable and the duration of the free intervals as dependent variables was used. Furthermore, ANOVA was followed by Fisher's Protected Least Significant Difference post-hoc test to measure between-group differences.
Results: M-D-free interval phases were shorter than D-M-free intervals. M-D intervals were the shortest ones, the D-D and D-M did not differ, and the M-M were the longest.
Conclusion: The strict temporal link between manic and depressive phases supports the idea that the manic-depressive cycle usually begins with a manic episode, and that the subsequent depression is often the consequence of subsiding mania.
Keywords: Bipolar Disorder, Cycle, Depression, Episode, Interval, Mania, Phase
1. INTRODUCTION
The essential feature of bipolar disorder (BD) is its cyclicity [1, 2]. This should not be considered a simple recurrence of the different affective phases (mania/ hypomania, depression, free interval (or euthymia) that, in a sort of casual way, appear during the course of the illness. Cyclicity is the core of the disorder, at least from a clinical point of view, and its understanding may help unveil the pathogenesis of BD, guide clinicians to choose adequate therapeutic strategies, and improve BD patients’ long-term outcome.
Since Hippocrates (V Century b.C.) [3], the concepts of periodicity appeared in the description of the different types of fever. During the following Centuries, many physicians observed that mania and depression appeared and disappeared in a regular way during the course of psychic disorders. Aretaeus [4] noted during the I Century that mania occurs at intervals. Alexander of Tralles [5], a Byzantine physician active during the VI century, stated that people with mania “present intervals and attacks that occur in fever that recur periodically”. The term periodic associated with different forms of melancholia was also used by Georg Ernst Stahl (1659-1734) in De affectibus periodicis [6], Friedrich Hoffmann (1660-1742) in his Melancholia cum mania periodica alternans [7] and by Friedrich Casimir Medicus (1736-1808) in “History of period-setting diseases” [8]. At the beginning of the 19th Century, Jean-Étienne Dominique Esquirol (1772-1840) [9] described the folie continue, rémittente ou intermittente. Since that time, the term was used very often in psychiatry. In 1845, Wilhelm Griesinger (1817-1868) [10] introduced the word “cycle” in psychiatry in his Mental Pathology and Therapeutics: “Not rarely the whole disease consists of a cycle of both forms (mania and melancholia), which often regularly alternate with each other.” Since that time, the term periodic was gradually replaced by the term “cyclic” [11, 12].
During the XX Century, the idea that cyclicity was the core of mood disorders declined. It reemerged only in the last thirty years, mostly thanks to the work of Koukopoulos and his group. They first observed that if mania was completely suppressed by lithium the next depression did not occur; conversely, if lithium failed to suppress the manic phase, they observed that depression took place as though lithium had not been given. They hypothesized that lithium prevents depression by supressing mania [13].
In the mid-seventies, Koukopoulos et al. [14] first compared the cycle-sequence of depression-mania/hypomania-free interval (DMI cycle pattern), and its opposite (mania/hypomania-depression-free interval, MDI) in patients with BD. The MDI cycle pattern was more frequent in patients with BD type I. The DMI cycle pattern was more prevalent among patients with BD type II, and typically involved severe agitated depression. Smaller proportions of cases had a continuous circular sequence, with <4 episodes/ year without euthymic intervals (continuous circularity, CC) or with ≥4 episodes/year rapid-cycling (continuous circularity with rapid cycling course, CC-RC), or an irregular course (IRR).
In the following years, Koukopoulos and colleagues found that patients whose cycle started with mania responded better to prophylactic lithium than those whose cycle started with depression, which is followed by mania/hypomania [15]. Subsequently, this observation was confirmed by Grof et al. [16], Haag et al. [17], Maj et al. [18], Faedda et al. [19] and again by the same group [20, 21].
Despite these interesting findings, few studies have focused on the effect of cycle pattern on the clinical features of BD. Furthermore, the relationship between mania and depression inside the manic-depressive cycle has not been investigated.
We aimed to investigate the relationship between the manic and the depressive phases during the course of BD. We believe that the depressive phase can be more often driven by the preceding manic phase, while the manic phase is less often driven by the preceding depression. We thus hypothesized that the free intervals between manic and depressive episodes would be dramatically shorter than those between depressive and manic episodes and that standard deviations would be considerably smaller for the former pattern.
2. MATERIAL AND METHODS
2.1. Participants
In a prospective cohort study design, we recruited 160 consecutive patients with BD type I according to the DSM-IV-TR™ [22] criteria seen at the Centro Lucio Bini in Rome. DSM-IV criteria (21) were applied to all patients by the treating clinicians (GS, DR, AEK, PG) who have worked together in the same outpatient setting for more than fifteen years, reaching a high level of agreement.
We used the semi-structured diagnostic interview in use at Centro Lucio Bini since 1980, purposely constructed to assess patients with mood disorders. Briefly, the interview is based on DSM criteria and on clinical evaluation (not on simple yes/no answers to structured questions). The wording of the questions can be changed to improve/check understanding, and the final evaluation also takes into account all information from family members/close friends (present during at least one visit for all cases) and from any other medical documentation. All data collected about past social and family history, past psychiatric history and current psychiatric history were entered in preprinted medical records.
According to the cycle pattern, we divided patients in five groups:
Mania/hypomania-Depression-Free interval (MDI);
Depression-Mania/hypomania-Free interval (DMI);
Continuous circularity (CC);
Irregular cycle pattern (IRR);
Unipolar mania course (UPM) (Fig. 1).
Fig. (1).
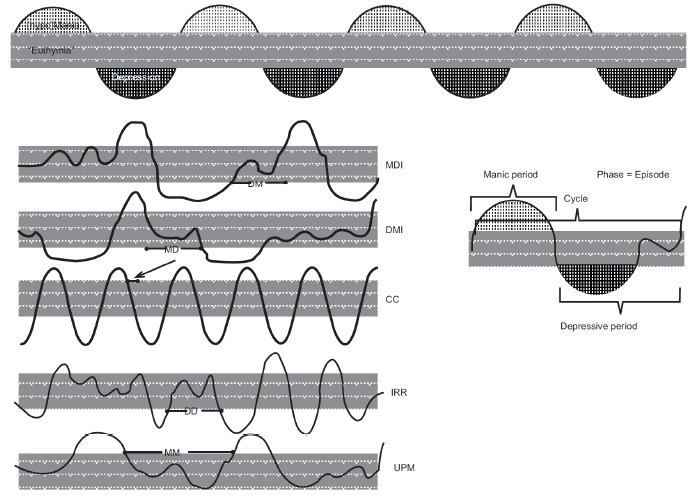
Cycle patterns, types of intervals (euthymic phases), and phases in the manic-depressive cycle.
Using both patient and family member interviews, and all other reliable sources (i.e., social workers, physicians, and other relevant informants), demographic and clinical data were obtained at baseline and during the follow-up period. The affective temperament of patients was assessed using Akiskal and Mallya’s method [23]. Mood symptom severity was assessed through the 21-item Hamilton Rating Scale for Depression (HDRS-21) [24], and the Young Mania Rating Scale (YMRS) [25]. During follow-up, every patient’s illness course was accurately assessed and depicted in a specific life chart where all the mood episodes and free intervals, with their characteristics and durations, were annotated. For our purposes, we distinguished four types of euthymic phases according to the type of consecutive mood episodes that preceded and followed them:
free interval between a depressive and a manic/ hypomanic episode (D-M);
free interval between a manic/hypomanic and a depressive episode (M-D);
free interval between two depressive episodes (D-D);
free interval between two manic/hypomanic episodes (M-M) (Fig. 1).
This subdivision is not valid for mixed states, since it is not easy to describe what type of episode one is getting-off; furthermore, cases in which exiting from mania and plunging directly into depression or vice versa, could apparently go unaccounted for. However, if we admit that mood has ups and downs and we define what is a threshold for (hypo)mania and depression, we get an interval that can be defined as euthymia or symptom-free interval. Then it is clear, that if one is to get off from an episode of whatever polarity to switch to another of the opposite polarity, he/she has to cross the euthymic space, even if it is too shortly (Fig. 1).
Exclusion criteria were diagnosis of mental retardation or documented IQ<70, presence of an unstable general medical condition and presence of clinically significant pre-study physical examination, electrocardiogram, laboratory or urinalysis abnormalities indicating serious medical disease that could impair evaluation. All patients gave free, informed consent.
2.2. Statistical Analyses
We compared the five groups of patients (i.e. MDI, DMI, IRR, CC and UPM) on sociodemographic and clinical characteristics using chi-square tests for nominal variables and one-way analysis of variance (ANOVA) for continuous variables. We set significance at p<0.05.
For the aim of this study, we focused on the duration of the four types of free intervals (i.e., D-M, M-D, D-D, M-M). To detect differences among the groups, we conducted a one-way analysis of variance (ANOVA-1way) using the groups as the independent variables and the duration of the free intervals as dependent variables. Furthermore, ANOVA-1way was followed by the Fisher's Protected Least Significant Difference (PLSD) post hoc test to measure between-group differences. A p<0.05 level of significance cut-off was used for comparative measurements.
3. RESULTS
3.1. Sociodemographic and Clinical Characteristics
One hundred sixty patients with BD type I were divided into five different groups according to the different cycle pattern; 100 had an MDI cycle pattern, 26 had an IRR cycle pattern, 14 a DMI cycle pattern, 14 a CC and 6 a UPM. Among the groups, patients showed significant difference in age at evaluation, education, temperament, type of first episode, and duration of illness.
The patients were prospectively followed for a mean period of 10±9.8 years; however the groups differed significantly at this respect, with the MDI, DMI and continuously circling groups having shorter follow-up periods than the irregular pattern, and the unipolar mania group more so. Among clinical characteristics, duration of mood episodes was smaller in the MDI group and longer in the DMI, irregular and unipolar mania groups (Table 1).
Table 1. Socio-demographic and past clinical characteristics of 160 patients with bipolar disorder type I.
| Characteristics |
Total sample
(n= 160) |
MDI
(n=100) |
DMI
(n=14) |
IRR (n=26) | CC (n=14) |
UPM
(n=6) |
F or χ2 | df | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male gender, n (%) | 73 (45.6) | 47 (47) | 6 (43) | 10(38.5) | 8 (57) | 2 (33.3) | 1.77 | 4 | 0.7 | ||||||||||
|
Age mean ± SD (range) |
36.9 ±13.6 (13-83) |
34.6 ±12.6 (13-78) |
48.6 ±17.9 (29-83) |
40 ±15.6 (16-67) |
35.9 ±13.7 (13-83) |
36.9 ±7.8 (24-43) |
3.8 | 4 | 0.0054 | ||||||||||
|
Education mean ± SD (range) |
14.07 ±3.8 (5-22) |
14.07 ±3.5 (5-22) |
15.7 ±3.8 (8-18) |
11.8 ±4.1 (8-18) |
13 ±3.7 (8-18 |
11.3 ±4 (8-18) |
4.33 | 4 | 0.0025 | ||||||||||
| Temperament | |||||||||||||||||||
| Hyperthymic n (%) | 92 (57.5) | 58 (58) | 9 (64.2) | 12 (46.1) | 10 (71.4) | 3 (50) | 29.7 | 12 | 0.003 | ||||||||||
| Cyclothymic n (%) | 32 (20) | 26 (26) | 3 (21.4) | 1 (3.9) | 2 (14.4) | 0 | |||||||||||||
| Dysthymic n (%) | 16 (10) | 8 (8) | 2 (14.4) | 3 (11.5) | 1 (7.1) | 2 (16) | |||||||||||||
| Other n (%) | 20 (12.5) | 8 (8) | 0 | 10 (38.5) | 1 (7.1) | 1 (34) | |||||||||||||
|
Age at onset mean ± SD (range) |
28.4 ±11.5 (12-83) |
27.6 ±10.8 (12-61) |
33.5 ±19.4 (15-83) |
29.2±10.4 (15-45) |
27.3 ±7.9 (17-45) |
29.9 ±9.0 (19-43) |
0.89 | 4 | 0.47 | ||||||||||
| Subtype of first episode | |||||||||||||||||||
| Mania n (%) | 77 (51) | 56 (57.7) | 1 (7.1) | 10 (47.6) | 4 (30.8) | 6 (100) | 21.03 | 9 | 0.01 | ||||||||||
| Depression n (%) | 52 (34.5) | 25 (25.7) | 11 (78.6) | 9 (42.9) | 7 (53.9) | - | |||||||||||||
| Hypomania n (%) | 17 (11.2) | 12 (12.3) | 2 (14.3) | 1 (4.7) | 2 (15.3) | - | |||||||||||||
| Mixed n (%) | 5 (3.3) | 4 (4.1) | 0 | 1 (4.7) | 0 | - | |||||||||||||
| Suicide attempts | n (%) | 39 (30.6) | 25(25) | 4 (28) | 9 (34.6) | 9 (64.2) | 2 (33.3) | 9.2 | 4 | 0.05 | |||||||||
|
Hospitalizations mean ± SD (range) |
2.4 ±2.7 (1-20) |
2.6 ±3.1 (1-20) |
1.6 ±1.1 (1-3) |
2.6 ±1.8 (1-7) |
1.5 ±0.8 (1-3) |
2 ±1.4 (1-3) |
0.30 | 4 | 0.8 | ||||||||||
|
Number of past episodes mean ± SD (range) |
5.1±5.1 (0-28) |
5.3±5.4 (0-28) |
6.3±2.4 (4-10) |
4.7±5.1 (0-20) |
5.9±5 (1-18) |
2.2±2.8 (0-5) |
0.5 | 4 | 0.68 | ||||||||||
|
Years of illness duration mean ± SD (range) |
18.3±13.5 (0.1-62) |
15.7±12.1 (0.1-51) |
23.7±21.1 (1.5-62.6) |
23.5±13 (2.2-45) |
18.6±10 (2-38) |
27.1±16.6 (5.6-49.5) |
2.96 | 4 | 0.02 | ||||||||||
|
Follow-up duration in years, mean ± SD (range) |
10 ±9.8 (0-42) |
9±9.1 (0-42) |
8.1 ±11.1 (0-38.7) |
12.8 ±10.7 (1-31) |
9.9±8.9 (0.1-29.8) |
20.1±11.8 (0.9-29.5) |
2.4 | 4 | 0.04 | ||||||||||
|
Number of episodes, mean ± SD (range) |
6.1 ±5.2 (1-24) |
5.7 ±5 (1-20) |
7.2 ±7.4 (1-24) |
7.9±5.4 (1-21) |
5.1 ±4.3 (1-17) |
5 ±2.3 (2-9) |
1.2 | 4 | 0.3 | ||||||||||
| Episode subtype | |||||||||||||||||||
|
Mania, mean ± SD (range) |
2.9 ±2.8 (0-17) |
2.9 ±3.1 (0-17) |
1.7 ±1.9 (0-7) |
3.5 ±2.7 (0-10) |
2.2 ±2.2 (0-8) |
4.6 ±1.7 (2-7) |
1.6 | 4 | 0.1 | ||||||||||
|
Depression, mean ± SD (range) |
2.4 ±2.4 (0-14) |
2.3 ±2.1 (0-10) |
3.5±4.2 (0-14) |
3 ±2.7 (0-12) |
2.3 ±1.9 (0-7) |
- | 1.3 | 3 | 0.2 | ||||||||||
|
Hypomania, mean ± SD (range) |
0.5 ±1.3 (0-7) |
0.5±1.2 (0-7) |
1.1 ±2.1 (0-6) |
0.6 ±1.7 (0-7) |
0.3 ±0.6 (0-2) |
- | 0.8 | 3 | 0.5 | ||||||||||
| Characteristics |
Total sample (n= 160) |
MDI (n=100) |
DMI (n=14) |
IRR (n=26) | CC (n=14) |
UPM (n=6) |
F or χ2 | df | p | ||||||||||
| Episode subtype | |||||||||||||||||||
|
Duration of episodes, weeks mean ± SD (range) |
15.8 ±18.6 (1-188) |
13.6 ±10.5 (1-84) |
18.4 ±15.3 (5-61) |
16.3 ±14.1 (1-71) |
30.6 ±50 (1-188) |
11 ±5.9 (4-20) |
2.8 | 4 | 0.02 | ||||||||||
|
Number of psychotic episodes, mean ± SD (range) |
2.2 ±1.9 (1-11) |
2.2 ±2.1 (1-11) |
1.4±0.5 (1-2) |
2.1 ±1.2 (1-5) |
2 ±1.4 (1-3) |
3.5 ±1.7 (1-5) |
0.7 | 4 | 0.6 | ||||||||||
|
HDRS total score, mean ± SD (range) |
19.7 ±2.8 (12-28) |
19.1 ±3.3 (12-26) |
20.1 ±1.9 (17-24) |
19.8 ±0.4 (19-20) |
20.6 ±3.9 (17-28) |
- | 0.5 | 3 | 0.6 | ||||||||||
|
YMRS total score, mean ± SD (range) |
22.6 ±3.9 (12-41) |
22.7 ±4.5 (12-34) |
22.2 ±2.6 (20-26) |
22.6 ±4.5 (12-34) |
21.7 ±1.8 (20-26) |
23.8 ±5.2 (21-34) |
0.2 | 4 | 0.9 | ||||||||||
Legend MDI: Mania/hypomania-Depression-Free interval Cycle; DMI: Depression-Mania/hypomania-Free interval Cycle; CC: Circular Continuous Circularity; IRR: Irregular Cycle; UPM: Unipolar Mania Cycle. Significant p values are indicated in bold.
3.2. Duration of Free Intervals
During the follow-up period, 838 euthymic phases (symptom-free intervals) were observed. According to different type of episode polarity succession, we found 307 M-D free interval periods, 266 D-M free interval periods, 219 M-M free interval periods and 46 D-D free interval periods. Among the groups, the mean duration of the euthymic phase was statistically different: D-M lasted
4. DISCUSSION
The aim of our study was to verify the existence of a relationship between the manic and the depressive phases of the illness. Our findings confirmed our a priori hypothesis, i.e., M-D free interval phases were dramatically shorter than D-M free intervals. Specifically, we found the M-D-free interval to be the shortest intervals, the D-D and D-M were intermediate and did not differ from eachother, and M-M were found to be the longest.
These findings may be better interpreted in the light of the manic-depressive cycle concept. The cycle consists of a manic phase (or episode), a depressive phase (or episode) and a free interval phase. The cycle starts from the beginning of one phase to the beginning of the next one of the same polarity including a phase of opposite polarity and an interval whenever they occur. The period, instead, starts from the beginning of one phase to the beginning of the next one including the interval whenever it occurs between them (see Fig. 1). According to the hypothesis of the primacy of Mania [1, 26], in the classic MDI cycle, the second part of the cycle, i.e. the depressive phase, should be considered as the consequence of mania itself. In other words, depressions following a manic episode should be viewed as the clinical manifestations of the underling neurobiological exhaustion provoked by the manic process. Our data support this view. The strict temporal link between these two phases may unveil a common pathogenetic mechanism.
On the contrary, manic episodes usually arose without any apparent relationship with the preceding episode. We have already suggested that most of them are triggered by external factors that act on predisposed individuals (mainly those with a hyperthymic temperament) and that the cyclic pattern is not correlated to inherent biological mechanisms [1]. In support of this view, our findings show that the intervals that separate manic recurrences are very long. Our data are in line with those found by Kraepelin [27], i.e., 3.3 years for the first manic-manic interval, 4.5 for the second and 2 years for the third and subsequent intervals. In this light, it is hard to consider the existence of an internal neurobiological mechanism that link two phases at much distance. It is acceptable on the contrary, that external factors can occur in the course of the life of BD patients, and trigger now and again a manic episode. Once the manic episode takes place, a new cycle starts ending in a new depression, ensuing after the exhaustion of mania and as the end result of the inability of the organism to sustain the unsustainable manic state.
The duration of D-D and M-M intervals is the longest. This finding is also in line with our hypothesis. According to the definition of cycle, two episodes of the same polarity belong to two different cycles. Thus, it is not surprising that they are separated by a long symptom-free interval, thus exhibiting greater variability than the M-D free interval.
Taken together, our data support the idea that the manic-depressive cycle begins with a manic episode, often provoked by external stimuli that may be readily identified or not (or “internal” stimuli, such as interoceptive stimuli or brain reverberating circuits that ensue in somehow general neural excitation; however, the interplay of these internal stimuli with external stimuli cannot be ruled out), and that the subsequent depression is a consequence. If we consider that the manic-depressive cycle is the essential clinical core of BD, inevitably the manic process plays an essential role in the pathogenesis of the disorder.
This view has immediate clinical consequences. Firstly, lithium, antiepileptic, and antipsychotic drugs, which are often used in combination, thus resulting in polypharmacy [28], are basic for stabilizing mood in patients with BD. All these agents have a prominent antimanic effect. To consider mania as the driving force of the illness may help understanding their clinical effect. Lithium is certainly the most studied mood stabilizer. As stated earlier, lithium owns an important prophylactic effect in patients with the MDI course. The most likely hypothesis is that lithium easily suppresses a manic process that develops gradually, thus preventing the subsequent depression that otherwise would have followed the mania [15]. The onset of mania after a free interval is usually slow. It seems conceivable that lithium, taken during the prodromal period, acts to suppress the otherwise growing excitatory process. Thus, it stops the cycle and stabilizes mood. Furthermore, it is possible to suggest a strategy to treat depression that follows mania. It is known that bipolar depression is difficult to treat, because of the risk of switching into the opposite phase [29], the risk of mixed states [30], and the risk for developing rapid cycling course [31]. Different strategies have been suggested, such as the use of antidepressants with concomitant mood stabilizers [32], electroconvulsive therapy [33, 34], deep transcranial magnetic stimulation [35], and therapeutic drug monitoring [36, 37]. Considering the secondary nature of the depressive episode that follows the manic one, it is possible to see why lowering prophylactic drug doses potentiates recovery from the depressive episode; we may suppose that as our prophylactic drugs are mainly antimanic, they may prolong the duration of depression.
A major objection could be that not always what follows is caused by what precedes it. If it is true that the post hoc, propter hoc rule is a logical fallacy, in this case, the very strong temporal relationship between maniac and depressive episodes and the very long time between same-polarity episodes and between those belonging to different cycles support our hypothesis. The temporal relationship is in fact considered to be the fundamental criterion in any definition of causality proposed by scientists and philosophers. Although it does not constitute scientific and conclusive evidence, time sequence strengthens the idea of a powerful interconnection between mania and subsequent depression, while wakening the evidence for a direct causal relationship between depressive episodes being followed by manic ones (and between episodes belonging to different manic-depressive cycles, i.e., successive same-polarity episodes).
Some limitations should be mentioned at this point. We enrolled only patients with BD I. Given the speculative nature of our study, we wanted to strengthen the consistency of the sample and the reliability of our findings, even at the expense of their generalizability. In fact, patients with BD I are a more homogeneous group compared to BD II. Generally, the course of BD II is strongly influenced by a preexisting mood oscillations of the cyclothymic pattern. External events often trigger mood episodes in patients with intense nervous reactivity, but the underlying mood instability may eventually kindle unprovoked episodes, thus resulting in destabilized mood, according to Robert Post’s kindling model of BD [38]. The model for this type of BD lies on cyclothymic temperament and disorder. In these patients, a causal relationship between (hypo)mania and depression is not always clear, even though it cannot be ruled out. Along this line, Koukopoulos and Ghaemi [26] in an attempt to explain the post-excitement depression in the absence of a clear (hypo)mania, proposed to view those symptom clusters that are triggered by stressful life events and often precede depression as hypomanic equivalents; these are characterized by subjective distress, sleep disturbances, emotional turmoil, and hyperactivity. Summarizing then, we showed a stronger interdependence between manic and ensuing depressive episodes in BD patients than between depressive and subsequent manic episodes.
CONCLUSION
We found that M-D intervals are significantly shorter than D-M intervals. Among all intervals, M-D are the shortest, while those which separate phases of the same polarity (i.e., those belonging to different cycles) are the longest. Our data support Koukopoulos’ hypothesis of a causality relationship between the manic phase and the subsequent depression (primacy of mania hypothesis), which is more direct than the relationship of subsiding depression with the subsequent onset of mania. Our results should prompt further longitudinal investigations with the aim to identify psychopathological mechanisms underpinning the manic-depressive cycle.
Table 2. Duration of different free interval types between mood episodes.
| Type of interval | |||||||
|---|---|---|---|---|---|---|---|
|
D-M
(n=266) |
M-D
(n=307) |
D-D
(n=46) |
M-M
(n=219) |
F | df | p | |
| Interval duration in weeks, mean ± SD (range) | 107.41±175.32 (0-672) |
2.25±5.58 (0-36) |
93.67±92.93 (28-53) |
136.91±247.10 (8-936) |
33.1 | 3 | <0.0001 |
| Fisher’s LSD | |||||||
| Post hoc test | D-D vs. M-D | D-D vs. M-D | D-D vs. M-M | D-M vs. M-D | D-M vs. M-M | M-D vs. M-M | |
| p values | 0.12 | <0.0001 | 0.9 | <0.0001 | 0.0002 | <0.0001 | |
Legend: D-M: Depression-Mania/Hypomania free interval; M-D: Mania/Hypomania-Depression free interval; D-D: Depression-Depression free interval; df: degrees of freedom; F: F-value for F-tests (ANOVA); Fisher’s LSD: Fisher’s least square differences; M-M: Mania-Mania free interval. Significant p values are indicated in bold.
107.4±175.32 weeks, M-D 2.25±5.58 weeks, D-D 58.93±92.93 and M-M 136.91±247.10 weeks (p<0.0001) (Table 2). As evidenced by Fisher’s PLSD post hoc test, differences were present between D-D and M-D intervals (p<0.0001), the D-M and M-D intervals (p<0.0001), the D-M and M-M (p=0.0002), and the M-D and M-M intervals (p<0.0001) (Table 2). Furthermore, standard deviations were narrower for the M-D pattern, as predicted (Table 2).
ACKNOWLEDGEMENTS
We express our gratitude to the patients who dedicated their time and efforts in participating in this study.
LIST OF ABBREVIATIONS
- ANOVA
One-Way Analysis of Variance
- BD
Bipolar Disorder
- CC
Continuous Circularity Pattern
- D-D
Free Intervals Present Between two Depressive Episodes
- D-M
Free Intervals Present Between a Depressive and a Manic/Hypomanic Episode
- DMI
Depression-Mania/Hypomania-Free Interval
- HDRS-21
21-Item Hamilton Rating Scale for Depression
- IRR
Irregular Cycle Pattern
- M-D
Free Intervals Present Between A Manic/ Hypomanic and A Depressive Episode
- MDI
Mania/Hypomania-Depression-Free Interval Pattern
- M-M
Free Interval Present between two Manic/ Hypomanic Episodes
- RC
Rapid Cycling pattern
- UPM
Unipolar Mania Course
- YMRS
Young Mania Rating Scale
FUNDING
This study has been partially supported by an Educational Grant of the Ministry of Research of Italy (RBFR12LD0W_002).
CONFLICT OF INTEREST
Paolo Girardi has received unrestricted educational grants support from Eli Lilly Italia S.p.A., Janssen-Cilag S.p.A., and Springer Healthcare, and has participated in Advisory Boards for Eli Lilly Italia S.p.A., Otsuka, Pfizer, Schering, and Springer Healthcare and received honoraria from Eli Lilly Italia S.p.A. and Springer Healthcare. All authors of this paper have no relevant affiliations or financial involvement with any organization or entity with a financial interest in, or financial conflict with the subject matter or materials discussed in the manuscript. This work has not been supported by any funding.
REFERENCES
- 1.Koukopoulos A. The primacy of mania. In: Akiskal H.S., Tohen M., editors. Bipolar Psycho- pharmacotherapy: Caring for the Patient. Hoboken, New Jersey: John Wiley and Sons; 2006. pp. 169–191. [http://dx.doi.org/10.1002/0470017953.ch10] [Google Scholar]
- 2.Koukopoulos A., Sani G., Koukopoulos A.E., Albert M.J., Girardi P., Tatarelli R. Endogenous and exogenous cyclicity and temperament in bipolar disorder: review, new data and hypotheses. J. Affect. Disord. 2006;96(3):165–175. doi: 10.1016/j.jad.2006.08.031. [http://dx.doi.org/10.1016/ j.jad.2006.08.031]. [PMID: 16997381]. [DOI] [PubMed] [Google Scholar]
- 3.Hippocrates . In: (460 b.C.–377 b.C.). Nature of Man. The Loeb Classical Library, Hippocrates IV. Jones W.H., editor. Cambridge, MA: Harvard University Press; 1967. pp. 1–42. [Google Scholar]
- 4.Aretaeus de Cappadoccia (I Century) De causis et signis acutorum et diuturnorum morborum, Libri quatuor. De curatione acutorum et diuturnorum morborum, libri quatuor. Cum mss. duobus, Harleyano, & Vaticano, contulit: novamque versionem dedit, Johannes Wigan. E Typographeo Clarendoniano: Oxoniæ. Oxford: Clarendon Press; 1723. [Google Scholar]
- 5.Alexander trallianus. De melancholia. In Alexander von Tralles. Puschmann, T., Eds.; Wien: Wilhelm Braumüller; 1878. [Google Scholar]
- 6.Stahl G.E. Dissertatio Inauguralis Medica de Affectibus Periodicis. Halle an der Saale: Typis Orphanotrophii Glaucha-Halensis; 1702. [Google Scholar]
- 7.Hoffmann F. Opera omnia physico-medica, in sex tomos distributa. Genève: Fratres De Tournes; 1740. [Google Scholar]
- 8.Medicus F.C. Geschichte Periode haltender Krankheiten. Frankfurt am Main, Leipzig: Georg Ludwig Macklot; 1794. [Google Scholar]
- 9.Esquirol J-É. Des maladies mentales considérées sous les rapports médical, hygiénique et médico-légal. 1838. [PMC free article] [PubMed]
- 10.Griesinger W. Pathologie und Therapie der psychischen Krankheiten. Für Ärzte und Studirende dargestellt. Stuttgart: Verlag von Adolph Krabbe; 1845. [Google Scholar]
- 11.Kirn L. Die periodischen Psychosen. Stuttgart: Verlag von Ferdinand Enke; 1878. [Google Scholar]
- 12.Pilcz A. Die periodischen Geistestörungen. Eine klinische Studie. Jena: Gustav Fischer Verlag; 1901. [Google Scholar]
- 13.Kukopulos A., Reginaldi D. Does lithium prevent depressions by suppressing manias? Int. Pharmacopsychiatry. 1973;8(3):152–158. doi: 10.1159/000467986. [PMID: 4803866]. [DOI] [PubMed] [Google Scholar]
- 14.Kukopulos A., Reginaldi D., Girardi P., Tondo L. Course of manic-depressive recurrence. Compr. Psychiatry. 1975;16(6):517–524. doi: 10.1016/s0010-440x(75)80014-9. [http://dx.doi.org/10.1016/S0010-440X(75)80014-9]. [PMID: 1192716]. [DOI] [PubMed] [Google Scholar]
- 15.Kukopulos A., Reginaldi D., Laddomada P., Floris G., Serra G., Tondo L. Course of the manic-depressive cycle and changes caused by treatment. Pharmakopsychiatr. Neuropsychopharmakol. 1980;13(4):156–167. doi: 10.1055/s-2007-1019628. [PMID: 6108577]. [DOI] [PubMed] [Google Scholar]
- 16.Grof E., Haag M., Grof P., Haag H. Lithium response and the sequence of episode polarities: preliminary report on a Hamilton sample. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1987;11(2-3):199–203. doi: 10.1016/0278-5846(87)90060-1. [http://dx.doi.org/10.1016/0278-5846(87)90060-1]. [PMID: 3114828]. [DOI] [PubMed] [Google Scholar]
- 17.Haag H., Heidorn A., Haag M., Greil W. Sequence of affective polarity and lithium response: preliminary report on Munich sample. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1987;11(2-3):205–208. doi: 10.1016/0278-5846(87)90061-3. [http://dx.doi.org/10.1016/0278-5846(87)90061-3]. [PMID: 3628828]. [DOI] [PubMed] [Google Scholar]
- 18.Maj M., Pirozzi R., Starace F. Previous pattern of course of the illness as a predictor of response to lithium prophylaxis in bipolar patients. J. Affect. Disord. 1989;17(3):237–241. doi: 10.1016/0165-0327(89)90005-0. [http://dx.doi.org/ 10.1016/0165-0327(89)90005-0]. [PMID: 2529291]. [DOI] [PubMed] [Google Scholar]
- 19.Faedda G.L., Baldessarini R.J., Tohen M., Strakowski S.M., Waternaux C. Episode sequence in bipolar disorder and response to lithium treatment. Am. J. Psychiatry. 1991;148(9):1237–1239. doi: 10.1176/ajp.148.9.1237. [http://dx.doi.org/10.1176/ajp.148.9.1237]. [PMID: 1883005]. [DOI] [PubMed] [Google Scholar]
- 20.Koukopoulos A., Reginaldi D., Minnai G. The long term prophylaxis of affective disorders. In: Gessa G.L., Fratta W., Pani L., Serra G., editors. Depression and Mania. From Neurology to Treatment. New York: Raven Press; 1995. pp. 127–147. [PubMed] [Google Scholar]
- 21.Koukopoulos A., Reginaldi D., Tondo L., Visioli C., Baldessarini R.J. Course sequences in bipolar disorder: depressions preceding or following manias or hypomanias. J. Affect. Disord. 2013;151(1):105–110. doi: 10.1016/j.jad.2013.05.059. [http://dx.doi.org/10.1016/j.jad.2013.05.059]. [PMID: 23827534]. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders Fourth Ed. Washington, D.C: American Psychiatric Publishing, Inc; 2000. [Google Scholar]
- 23.Akiskal H.S., Mallya G. Criteria for the soft bipolar spectrum: treatment implications. Psychopharmacol. Bull. 1987;23(1):68–73. [PMID: 3602332]. [PubMed] [Google Scholar]
- 24.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [http://dx.doi.org/10.1136/jnnp.23.1. 56]. [PMID: 14399272]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young R.C., Biggs J.T., Ziegler V.E., Meyer D.A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry. 1978;133(11):429–435. doi: 10.1192/bjp.133.5.429. [http://dx.doi.org/10.1192/bjp.133.5.429]. [PMID: 728692]. [DOI] [PubMed] [Google Scholar]
- 26.Koukopoulos A., Ghaemi S.N. The primacy of mania: a reconsideration of mood disorders. Eur. Psychiatry. 2009;24(2):125–134. doi: 10.1016/j.eurpsy.2008.07.006. [http://dx.doi.org/10.1016/j.eurpsy.2008.07.006]. [PMID: 18789854]. [DOI] [PubMed] [Google Scholar]
- 27.Kraepelin E. Psychiatrie. Ein Lehrbuch für Studierende und Ärzte, 8. Auflage, III; Teil. Vol. II. Leipzig: Johann Ambrosius Barth; 1913. [Google Scholar]
- 28.Centorrino F., Fogarty K.V., Sani G., Salvatore P., Cimbolli P., Baldessarini R.J. Antipsychotic drug use: McLean Hospital, 2002. Hum. Psychopharmacol. 2005;20(5):355–358. doi: 10.1002/hup.700. [http://dx.doi.org/ 10.1002/hup.700]. [PMID: 15957153]. [DOI] [PubMed] [Google Scholar]
- 29.Bond D.J., Noronha M.M., Kauer-SantAnna M., Lam R.W., Yatham L.N. Antidepressant-associated mood elevations in bipolar II disorder compared with bipolar I disorder and major depressive disorder: a systematic review and meta-analysis. J. Clin. Psychiatry. 2008;69(10):1589–1601. doi: 10.4088/jcp.v69n1009. [http://dx.doi.org/10.4088/JCP.v69n1009]. [PMID: 19192442]. [DOI] [PubMed] [Google Scholar]
- 30.Sani G., Napoletano F., Vöhringer P.A., Sullivan M., Simonetti A., Koukopoulos A., Danese E., Girardi P., Ghaemi N. Mixed depression: clinical features and predictors of its onset associated with antidepressant use. Psychother. Psychosom. 2014;83(4):213–221. doi: 10.1159/000358808. [http://dx.doi.org/10.1159/000358808]. [PMID: 24970376]. [DOI] [PubMed] [Google Scholar]
- 31.Koukopoulos A., Sani G., Koukopoulos A.E., Minnai G.P., Girardi P., Pani L., Albert M.J., Reginaldi D. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J. Affect. Disord. 2003;73(1-2):75–85. doi: 10.1016/s0165-0327(02)00321-x. [http:// dx.doi.org/10.1016/S0165-0327(02)00321-X]. [PMID: 12507740]. [DOI] [PubMed] [Google Scholar]
- 32.Viktorin A., Lichtenstein P., Thase M.E., Larsson H., Lundholm C., Magnusson P.K., Landén M. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am. J. Psychiatry. 2014;171(10):1067–1073. doi: 10.1176/appi.ajp.2014.13111501. [http://dx.doi.org/10.1176/appi.ajp. 2014.13111501]. [PMID: 24935197]. [DOI] [PubMed] [Google Scholar]
- 33.Dierckx B., Heijnen W.T., van den Broek W.W., Birkenhäger T.K. Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: a meta-analysis. Bipolar Disord. 2012;14(2):146–150. doi: 10.1111/j.1399-5618.2012.00997.x. [http://dx.doi.org/10.1111/j.1399-5618.2012. 00997.x]. [PMID: 22420590]. [DOI] [PubMed] [Google Scholar]
- 34.Bailine S., Fink M., Knapp R., Petrides G., Husain M.M., Rasmussen K., Sampson S., Mueller M., McClintock S.M., Tobias K.G., Kellner C.H. Electroconvulsive therapy is equally effective in unipolar and bipolar depression. Acta Psychiatr. Scand. 2010;121(6):431–436. doi: 10.1111/j.1600-0447.2009.01493.x. [http://dx.doi.org/10.1111/j.1600-0447.2009.01493.x]. [PMID: 19895623]. [DOI] [PubMed] [Google Scholar]
- 35.Bersani F.S., Girardi N., Sanna L., Mazzarini L., Santucci C., Kotzalidis G.D., Sani G., De Rossi P., Raccah R.N., Caltagirone S.S., Battipaglia M., Capezzuto S., Bersani G., Girardi P. Deep transcranial magnetic stimulation for treatment-resistant bipolar depression: a case report of acute and maintenance efficacy. Neurocase. 2013;19(5):451–457. doi: 10.1080/13554794.2012.690429. [http://dx.doi.org/10.1080/ 13554794.2012.690429]. [PMID: 22827578]. [DOI] [PubMed] [Google Scholar]
- 36.Lostia A.M., Mazzarini L., Pacchiarotti I., Lionetto L., De Rossi P., Sanna L., Sani G., Kotzalidis G.D., Girardi P., Simmaco M., Tatarelli R. Serum levels of risperidone and its metabolite, 9-hydroxyrisperidone: correlation between drug concentration and clinical response. Ther. Drug Monit. 2009;31(4):475–481. doi: 10.1097/FTD.0b013e3181aa4780. [http:// dx.doi.org/10.1097/FTD.0b013e3181aa4780]. [PMID: 19531984]. [DOI] [PubMed] [Google Scholar]
- 37.Musenga A., Saracino M.A., Sani G., Raggi M.A. Antipsychotic and antiepileptic drugs in bipolar disorder: the importance of therapeutic drug monitoring. Curr. Med. Chem. 2009;16(12):1463–1481. doi: 10.2174/092986709787909604. [http://dx.doi.org/10.2174/092986709787909604]. [PMID: 19355900]. [DOI] [PubMed] [Google Scholar]
- 38.Post R.M., Uhde T.W., Putnam F.W., Ballenger J.C., Berrettini W.H. Kindling and carbamazepine in affective illness. J. Nerv. Ment. Dis. 1982;170(12):717–731. doi: 10.1097/00005053-198212000-00002. [http://dx.doi.org/10.1097/00005053-198212000-00002]. [PMID: 6754868]. [DOI] [PubMed] [Google Scholar]


