Abstract
Background:
Restoring the vertical dimension is a critical procedure in prosthetic dentistry. Anterior facial height has a significant impact on the length of the ramus. Patients with deep bite will exhibit a shorter lower facial height; hence, restoring the vertical dimension esthetically without altering the facial form is highly challenging.
Aim:
To evaluate the relationship of gonial angle, ramus height, and dental height with different facial forms.
Subjects and Methods:
A total of 51 subjects in all facial form aged between 20 and 40 with deep bite were randomly selected. Lateral cephalograms and facial photographs were made for each patient. Ramus height was measured on lateral cephalogram by measuring the distance from articulare to gonion. The gonial angles were calculated and anterior and posterior dental height were measured from cephalogram. Facial forms were evaluated using patient's photographs.
Results:
The obtained measurements were evaluated, and compared statistically with one way analysis of variance and regression correlation test. Statistical analysis revealed that there was no correlation found between the gonial angle and ramus height.
Conclusion:
Correlation found between the ramus height and anterior and posterior dental height in patients with deep bite disorders. The ramus height can be calculated using the formulas 46.42 + (0.095 × AD height), 46.046+ (0.123 × PD height).
Keywords: Dental height, Facial form, Gonial angle, Ramus height
Introduction
Deep bite can be defined as “vertical overlap of upper teeth on the labial surface of lower teeth in centric occlusion which exceeds normal range of 1–2 mm.” Deep bite has been considered one of the most common malocclusions and the most difficult to treat successfully. Several factors are associated with development of deep bite. Among these are incisor supraocclusion, excessive overjet, canine position, molar infraocclusion, ramus height, and vertical face type.[1] Deep bite has been found to be associated with abnormal mandibular function and disorders.[2,3]
A skeletal type of overbite may be due to either malrelationship of alveolar bones or an overgrowth or undergrowth of any alveolar segments. The diminished anterior vertical height of the face is also an important criterion for diagnosis of skeletal deep overbites. Complex deep bite is frequently associated with Class II Division 2 and occasionally with Class III.
Deep bite due to dentition may be (a) loss or mesial tipping of posterior teeth (diminished posterior dental [PD] height), (b) early loss of teeth and lingual collapse of the anterior teeth (c) over eruption of the incisor teeth, infraocclusion of the buccal segment or combination of both (d) accentuated aberration in the tooth morphology (e) periodontal disease. Deep bite may worsen the existing condition if the posterior tooth drift mesially during the pathological migration.[4]
Vertical dimension is the distance between two selected anatomic or marked points, one on a fixed and one on a movable member (usually one on the tip of the nose and the other upon the chin).[1] Occlusal vertical dimension (OVD) is the distance measured between two points when the occluding members are in contact.[5]
Tooth surface loss may be purely physiological and occurs as a consequence of aging. However, certain non-carious factors may lead to tooth surface loss pathologically. The etiology of such non-carious tooth surface wear includes abrasion, attrition, erosion, and abfraction.[6] Attrition describes mechanical wear resulting from mastication or parafunction and is limited to the contacting surfaces of teeth during function or parafunction. Such direct contact occurs at the proximal areas, on supporting cusps, and on guiding surfaces.[7]
The phonetic method which measures vertical dimension by means of the closest speaking space.[8] This space can be measured before the loss of the remaining natural teeth to give us the patient's natural vertical dimension which can be recorded and used at later dates. When a patient has lost natural occlusal stops, this technique has provided consistently reliable results.[9,10] Cephalometrics can also be utilized in evaluating OVD. Hard tissue cephalometric analyses such as McNamara's analysis and Andrews' analysis, which determine the lower anterior facial height are used for this purpose.[11]
Rationale for altering OVD comprise esthetics, altering the occlusal relationship, and for prosthetic convenience to allow space for restorations. Clinical problems associated with altered OVD include joint or muscle pain, impaired muscle activity, and altered phonetics.[12,13,14] Altering VD does not produce pain for more than one to 2 weeks which might be a result of increased temporary muscle activity. Response after opening OVD may differ from patient to patient. Some can remain stable while others may relapse a lot. However, this is not being a problem usually as this may go unnoticed dentally. Patients usually get adapted otherwise need correction by creating space.[15]
Management of these patients using fixed or removable prostheses is complex and are the most difficult to restore. It is important to establish the cause of wear before intervention to improve the effectiveness of any prosthesis and maintain the vertical dimension in the rehabilitation of worn dentition.[16,17]
Many studies[18,19,20,21] are there in relating gonial angle and ramus height in identifying the sex, but there are no other studies relating ramus height and dental height in establishing vertical dimension of dentate cases. It is difficult to determine if there is a loss of OVD without knowing the initial position of the stable bony points of reference and the dental changes. Clinicians may decide to increase OVD based on the amount of interocclusal space required to restore the dentition to proper esthetics, form, and function. The decision whether to restore at increased or existing OVD is made by assessing the free way space and dentoalveolar compensation in distal extension edentulous and full mouth rehabilitation in completely worn cases. Hence, this study was conducted to evaluate the relationship of gonial angle, ramus height, and dental height with different facial forms of dentate cases.
Subjects and Methods
It was a cross-sectional, observational study carried from the cephalogram of patient with deep bite reported to the Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, India. The investigation was approved by the Institutional Ethical Committee of SRM Dental College, Ramapuram, and SRM University. A written informed consent was obtained from all subjects.
A total of 51 subjects in all facial form aged between 20 and 40 with deep bite were randomly selected based on the inclusion criteria of the presence of a fully erupted dentition, no structural deformity, and no developmental anomaly in dentition with different facial forms, in equal male and female ratio. Lateral cephalograms and facial photographs were made for each patient.
Ramus height was measured on lateral cephalogram by measuring the distance from the articulare to gonion. The gonial angles were calculated and anterior and PD heights were measured from cephalogram [Figure 1]. Upper anterior dental (AD) height which is the perpendicular distance from upper incisal edge projected right angle to the palatal plane and lower AD height, which is the perpendicular distance from lower incisal edge projected right angle to the mandibular plane (MP).[22] Upper PD height which is the perpendicular distance from the mesiobuccal cusps of the upper first molar to the palatal plane. Lower PD height which is the perpendicular distance from the mesiobuccal cusp of the lower first molar to the MP.[23] Gonial angle is the angle between the posterior border of the ramus (Ar–Go) and lower border of the mandible or MP (Go–Me).[24,25] The values were calculated and subjected to statistical analysis using one way analysis of variance (ANOVA).
Figure 1.
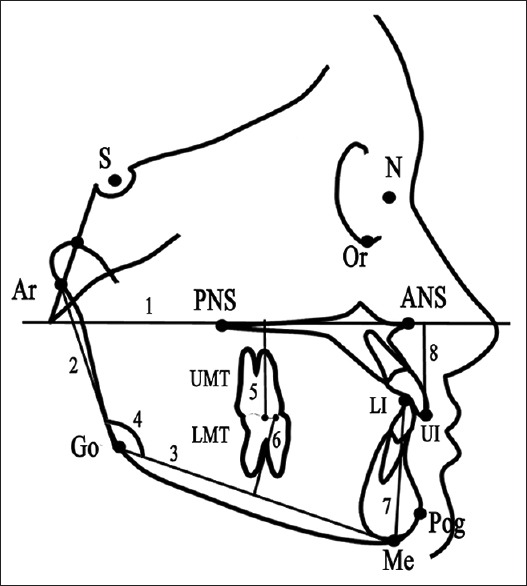
Cephalometric landmarks: (1) palatal plane (2) ramus height, (3) mandibular plane (4) gonial angle (5) upper posterior dental height, (6) lower posterior dental height,(7) lower anterior dental height, (8) upper anterior dental height
Facial forms were evaluated using the participant's photographs. For each photograph, standardized distance of 150 cm was maintained. A full face photograph with the closed lip was obtained with lens positioned parallel to the subject's face [Figure 2]. The facial form was determined from the measured three horizontal distances on the face: temporal width (Ft-Ft), zygomatic width (Zyg-Zyg), and gonial width (Go-Go).[26]
Figure 2.
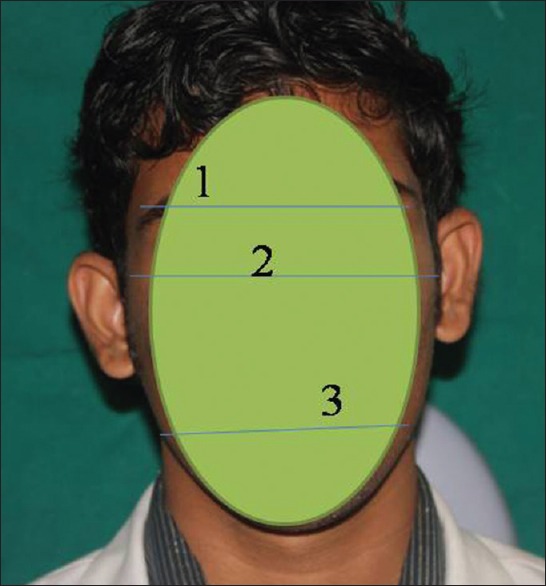
Facial form landmarks: (1) temporal width (Ft-Ft), (2) zygomatic width (Zyg-Zyg), (3) gonial width (Go-Go)
Statistical analysis
All the data were analyzed using SPSS for Windows version 22 (IBM Corp., Released 2013, Armonk, NY, USA). The values were statistically analyzed using one way ANOVA to compare the ramus height with facial form within the groups. Multiple comparison between groups was done using Tukey's honestly significant difference (HSD) post hoc test. All the P < 0.001 were considered statistically insignificant, and the level of significance was 95% confidence interval.
Results
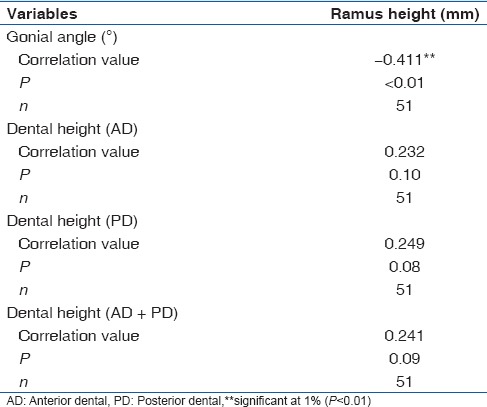
A total of 51 radiographs were analyzed for this study of which 26 males and 25 females between 20 and 40 years old. The Highest mean ramus height 55.5 mm (standard deviation [SD] 8.3) and 55.4 mm (SD 6.1) were found in square and square tapering form [Table 1]. Comparison between groups was done using Tukey's HSD post hoc test. Least difference was found between square and square tapering facial form [Table 2]. The correlation between the ramus height and other variables were done using Pearson correlation coefficient. The analysis showed that there was no correlation between ramus height and gonial angle. There was a correlation found between the ramus height and dental height because the P > 0.001 [Table 3]. Hence, linear regression analysis was used to calculate the ramus height using AD height. [Graph 1] Ramus height = 46.42 + 0.095 × dental height (AD) [Tables 4 and 5]. Similarly, the ramus height was calculated using PD height. [Graph 2] Ramus height = 46.046 + 0.123 × dental height (PD) [Tables 6 and 7]. Using both anterior and PD height, [Graph 3] the ramus height was calculated using the formula ramus height = 46.168 + 0.055 × dental height (AD + PD) [Tables 8 and 9].
Table 1.
One-way analysis of variance to compare mean ramus height between facial forms
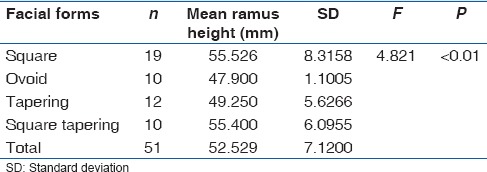
Table 2.
Tukey's highly significant difference post hoc tests for multiple comparisons
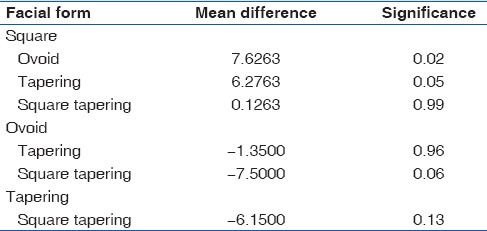
Table 3.
Pearson correlation coefficient between ramus height and other variables
Graph 1.
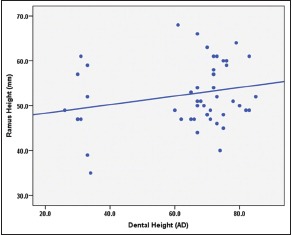
Regression plot showing the correlation between ramus height and anterior dental height
Table 4.
Linear regression analysis to find the ramus height based on dental height (AD)
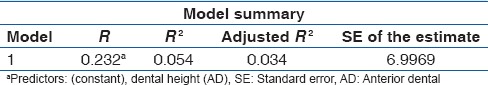
Table 5.
Regression coefficients
Graph 2.
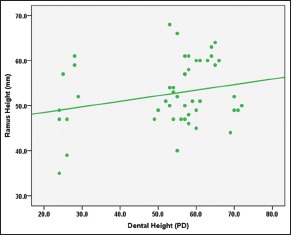
Regression plot showing the correlation between ramus height and posterior dental height
Table 6.
Linear regression analysis to find the ramus height based on dental height (PD)
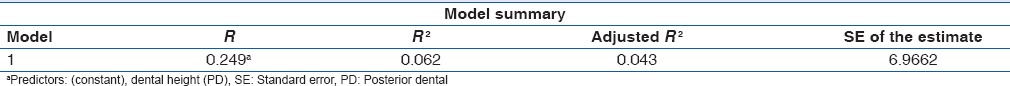
Table 7.
Regression coefficients
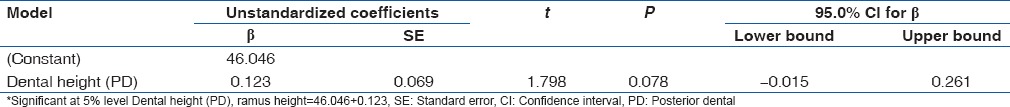
Graph 3.
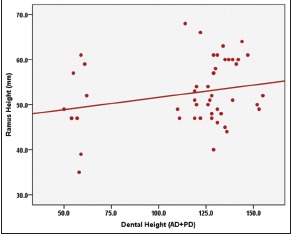
Regression plot showing the correlation between ramus height and (anterior dental + posterior dental) dental height
Table 8.
Linear regression analysis to find the ramus height based on dental height (AD+PD)
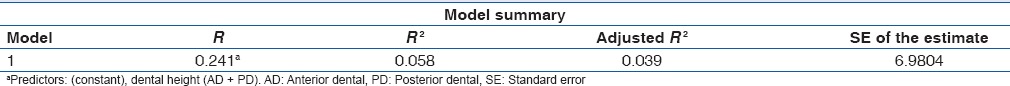
Table 9.
Regression coefficients

Discussion
Bite collapse can result in damage to the jaw joints and severe pain or dysfunction of the temperomandibular joint (TMJ). A critical aspect for successful treatment is to determine the OVD and the interocclusal rest space.[27] The articulated study casts and diagnostic wax-up can provide important information which is helpful for the evaluation of treatment options.[28] A systematic approach for managing tooth wear can lead to a predictable and favorable prognosis.[29]
The most popular method for correcting deep overbite is by anterior bite plane. The anterior bite plane is a modified Hawley's appliance with a built-in flat acrylic bite plate or inclined plane or platform lingual to the maxillary incisors. The mandibular incisors come into contact with the acrylic platform, which causes a disocclusion of the posterior teeth during the mandibular closing movement. The disocclusion of the bite accelerates the passive eruption of the posterior teeth, which stops when one or more opposing teeth come in contact. It is advisable not to disocclude the posterior teeth more than 2 mm. If bite opening in the anterior region is not sufficient, the acrylic platform can be augmented in small increments several times during the treatment. Small increments also apparently do not cause a sudden TMJ or myofunctional change. If a correct treatment plan is followed, the bite plate can also help in minor labiolingual and mesiodistal movements of teeth with the help of a labial bow or auxiliary springs. The patient wears this appliance almost 24 h a day. The use of bite plates, at the time of attaining the desired overbite, should not be suddenly stopped, the bite plate itself should be used as a retainer and its discontinual should be gradual.[4] The posterior bite plane is fabricated for the mandibular teeth and consists of areas of hard acrylic located over the posterior teeth and connected by a cast metal lingual bar. It is advocated for the cases of severe loss of vertical dimension or when there is a need of major changes in anterior positioning of the mandible.[30,31]
The patient's gonial angle has an impact on the patient's anterior vertical dimension. The patient's with an acute gonial angle has a tendency to mimic the facial features of long ramus, with square face and short lower face compared to their midface. These patients are commonly having a flat MP angle. Patients who have more obtuse gonial angles mimic the appearance of patients with short ramus heights, with a long narrow face, excessive tooth, and gingival display, and a long lower face when compared to their midface. Patients with more obtuse gonial angles often are having steep MP angles. There appears to be some evidence that the formation of the gonial angle, which may be influenced by the strength of the masseter muscle. If muscles are stronger and more developed, the gonial angle will be more acute. In addition to ramus length and gonial angles, tooth eruption plays a critical role in the development of a patient's vertical dimension. In normal growth and development, the maxillary and mandibular teeth erupt to maintain occlusal contact as the face grows. There can be variations, however, in tooth eruption that can result in alterations in facial vertical dimension. After the completion of, tooth eruption is necessary to maintain the vertical dimension if any wear occurs. If eruption occurs at the same rate as tooth wear, the vertical dimension of the patient will be unchanged. If, however, the eruption does not keep up with tooth wear, the vertical dimension may decrease with time.[32,33]
The mandibular basal bone morphology changes as consequences of tooth loss, which can be expressed as widening of the gonial angle and shortening of the ramus and condylar height. The findings highlight the importance of prosthetic rehabilitation of the masticatory system to maintain good functioning of the masticatory muscles.[34]
In this study, the ramus height was compared with gonial angle, anterior and PD height with facial forms using ANOVA and Tukey's HSD post hoc test and found out that there was no correlation between ramus height, gonial angle, and facial form. However, there was a correlation between ramus height and dental height. Hence, linear regression analysis was used to find out the relationship of the dental height and ramus height and derived a formula that the ramus height can be calculated with the formula Ramus height (mm) = 46.42 + (0.095 × AD), Ramus height = 46.046 + (0.123 × P D), and ramus height = 46.168 + (0.055× (AD + PD) and the deviation was ± 1 mm. Hence, if the anterior teeth are only present (collapsed bite or attritted dentition), the ramus height can be calculated using the above formula. This measurement can be used as a guide to maintain the vertical dimension of the patient and also useful to choose the type of bite plane. Square facial and square tapering facial form were found in Pearsons with more ramus height and less lower facial height with more obtuse gonial angle. There was no correlation between facial form and deep bite in this study.
The study is based on the radiograph, so there are more chances for magnification error which is the limitation of this study. Using the results of this study, the vertical dimension at occlusion can be established in completely worn out dentition.
Clinical significance
Vertical dimension can be increased with posterior bite plane in patients with long ramus and less PD height without deep bite. However, patient with deep bite and long ramus height with less PD height can be managed with anterior bite plane. Increasing vertical dimension in patient with short ramus and more PD height lead to TMJ problems. Such kind of cases can be managed with cap splint.
Conclusion
Ramus height is most closely correlated with PD height than AD height. If ramus height is more and lower facial height is less which will be leading to square facial form and vice versa. If gonial angle is more obtuse and the lower facial height more, thus leading to long tapering face and vice versa. The ramus height can be calculated using the formulas 46.42 + (0.095 × AD height), 46.046 + (0.123 × PD height). Using both anterior and PD height, the ramus height was calculated using the formula ramus height = 46.168 + (0.055 × AD + PD).
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
References
- 1.Parker CD, Nanda RS, Currier GF. Skeletal and dental changes associated with the treatment of deep bite malocclusion. Am J Orthod Dentofacial Orthop. 1995;107:382–93. doi: 10.1016/s0889-5406(95)70091-9. [DOI] [PubMed] [Google Scholar]
- 2.McDowell EH, Baker IM. The skeletodental adaptations in deep bite correction. Am J Orthod Dentofacial Orthop. 1991;100:370–5. doi: 10.1016/0889-5406(91)70076-9. [DOI] [PubMed] [Google Scholar]
- 3.Sonnesen L, Bakke M, Solow B. Malocclusion traits and symptoms and signs of temporomandibular disorders in children with severe malocclusion. Eur J Orthod. 1998;20:543–59. doi: 10.1093/ejo/20.5.543. [DOI] [PubMed] [Google Scholar]
- 4.Sreedhar CV, Baratam S. Deep overbite a review. Ann Essences Dent. 2009;1:9–25. [Google Scholar]
- 5.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:57. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135:1109–18. doi: 10.14219/jada.archive.2004.0369. [DOI] [PubMed] [Google Scholar]
- 7.The glossary of prosthodontic terms. J Prosthet Dent. 1999;81:48. [PubMed] [Google Scholar]
- 8.Silverman MM. Determination of vertical dimension by phonetics. J Prosthet Dent. 1956;6:465–71. [Google Scholar]
- 9.Dawson PE. Functional Occlusion, from TMJ to Smile Designs. St. Louis, Missouri: Mosby-Elsevier; 2007. pp. 121–32. [Google Scholar]
- 10.Dao TT, Feine JS, Lund JP. Can electrical stimulation be used to establish a physiologic occlusal position? J Prosthet Dent. 1988;60:509–14. doi: 10.1016/0022-3913(88)90259-4. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson A, Jacobson RL. Radiographic Cephalometry, From Basics to 3-D Imaging. 2nd ed. IL: Quintessence Publishing Co. Inc.; 2006. pp. 79–98.pp. 113–9. [Google Scholar]
- 12.Christensen J. Effect of occlusion-raising procedures on the chewing system. Dent Pract Dent Rec. 1970;20:233–8. [PubMed] [Google Scholar]
- 13.Ibbetson RJ, Setchell DJ. Treatment of the worn dentition: 2. Dent Update. 1989;16:300. [PubMed] [Google Scholar]
- 14.Dahl BL, Krogstad O. Long-term observations of an increased occlusal face height obtained by a combined orthodontic/prosthetic approach. J Oral Rehabil. 1985;12:173–6. doi: 10.1111/j.1365-2842.1985.tb00632.x. [DOI] [PubMed] [Google Scholar]
- 15.Bloom DR, Padayachy JN. Increasing occlusal vertical dimension – Why, when and how. Br Dent J. 2006;200:251–6. doi: 10.1038/sj.bdj.4813305. [DOI] [PubMed] [Google Scholar]
- 16.Smith BG. Toothwear: Aetiology and diagnosis. Dent Update. 1989;16:204–12. [PubMed] [Google Scholar]
- 17.Vinay Chila B, Meena Ajay A. Altering occlusal vertical dimension in functional and esthetic rehabilitation of severely worn dentition. J Oral Health Res. 2010;1:2–8. [Google Scholar]
- 18.Rupa KR, Chatra L, Shenai P, Veena KM, Rao PK, Prabhu RV, Kushraj T, Shetty P, Hameed S. Gonial angle and ramus height as sex determinants: A radiographic pilot study. J Cranio Max Dis. 2015;4:111–6. [Google Scholar]
- 19.Indira AP, Markande A, David MP. Mandibular ramus: An indicator for sex determination – A digital radiographic study. J Forensic Dent Sci. 2012;4:58–62. doi: 10.4103/0975-1475.109885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudhir N, Chittaranjan B, Kumar BA, Taruna M, Kumar MP, Reddy MR. Digital cephalometric tracings by PRO-CEPH V3 software for comparative analyses of vertical dimension in edentulous patients. J Clin Diagn Res. 2015;9:ZC01–5. doi: 10.7860/JCDR/2015/12034.5862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kedarisetty SG, Rao GV, Rayapudi N, Korlepara R. Evaluation of skeletal and dental age using third molar calcification, condylar height and length of the mandibular body. J Forensic Dent Sci. 2015;7:121–5. doi: 10.4103/0975-1475.155077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsai HH. Cephalometric characteristics of bimaxillary dentoalveolar protrusion in early mixed dentition. J Clin Pediatr Dent. 2002;26:363–70. doi: 10.17796/jcpd.26.4.lqn08w5827576j60. [DOI] [PubMed] [Google Scholar]
- 23.Haralabakis NB, Yiagtzis SC, Toutountzakis NM. Cephalometric characteristics of open bite in adults: A three-dimensional cephalometric evaluation. Int J Adult Orthodon Orthognath Surg. 1994;9:223–31. [PubMed] [Google Scholar]
- 24.Cangialosi TJ. Skeletal morphologic features of anterior open bite. Am J Orthod. 1984;85:28–36. doi: 10.1016/0002-9416(84)90120-9. [DOI] [PubMed] [Google Scholar]
- 25.Katsaros C, Berg R. Anterior open bite malocclusion: A follow-up study of orthodontic treatment effects. Eur J Orthod. 1993;15:273–80. doi: 10.1093/ejo/15.4.273. [DOI] [PubMed] [Google Scholar]
- 26.Bell RA. The geometric theory of selection of artificial teeth: Is it valid? J Am Dent Assoc. 1978;97:637–40. doi: 10.14219/jada.archive.1978.0349. [DOI] [PubMed] [Google Scholar]
- 27.Doan PD, Goldstein GR. The use of a diagnostic matrix in the management of the severely worn dentition. J Prosthodont. 2007;16:277–81. doi: 10.1111/j.1532-849X.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- 28.Song MY, Park JM, Park EJ. Full mouth rehabilitation of the patient with severely worn dentition: A case report. J Adv Prosthodont. 2010;2:106–10. doi: 10.4047/jap.2010.2.3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okeson JP. The effects of hard and soft occlusal splints on nocturnal bruxism. J Am Dent Assoc. 1987;114:788–91. doi: 10.14219/jada.archive.1987.0165. [DOI] [PubMed] [Google Scholar]
- 30.dos Santos JD, Jr, de Rijk WG. Vectorial analysis of the equilibrium of forces transmitted to TMJ and occlusal biteplane splints. J Oral Rehabil. 1995;22:301–10. doi: 10.1111/j.1365-2842.1995.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 31.Mahboub F, Fard EM, Geramipanah F, Hajimiragha H. Prosthodontic rehabilitation of a bruxer patient with severely worn dentition: A clinical case report. J Dent Res Dent Clin Dent Prospects. 2009;3:28–31. doi: 10.5681/joddd.2009.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brodie AG. On the growth pattern of the human head from the third month to the eighth year of life. Am J Anat. 1941;68:209–62. [Google Scholar]
- 33.Ingervall B, Thilander B. Relation between facial morphology and activity of the masticatory muscles: An electromyographic and radiographic cephalometric investigation. J Oral Rehabil. 1974;1:131–47. doi: 10.1111/j.1365-2842.1974.tb00771.x. [DOI] [PubMed] [Google Scholar]
- 34.Huumonen S, Sipilä K, Haikola B, Tapio M, Söderholm AL, Remes-Lyly T, et al. Influence of edentulousness on gonial angle, ramus and condylar height. J Oral Rehabil. 2010;37:34–8. doi: 10.1111/j.1365-2842.2009.02022.x. [DOI] [PubMed] [Google Scholar]


