Abstract
Background:
Polycystic ovary syndrome (PCOS) is known to be associated with insulin resistance and anti-Mullerian hormone (AMH), leading to the use of insulin-sensitizing agents (ISAs) to manage PCOS. Metformin is the most widely used ISA to treat irregular menstruation; however, the gastrointestinal side effects are quite debilitating. The development of herbal medicines such as bioactive fraction DLBS3233 offers a possibly effective treatment with minimal side effects.
Aim:
To determine the effect of metformin and DLBS3233 on serum AMH level.
Materials and Methods:
This study was a double-blind, randomized, controlled trial conducted between March 2013 and June 2015 at Yasmin Clinic, RSCM Kencana, Jakarta and Hasan Sadikin Hospital, Bandung. The patients with PCOS were diagnosed using the Rotterdam criteria. All participants received daily treatment consisting of 1500 mg metformin divided into two doses or 100 mg DLBS3233 for 6 months. An evaluation of serum AMH level was conducted before and after the completion of therapy.
Results:
Twenty patients received metformin, whereas 18 patients received DLBS3233. The levels of AMH prior to the intervention were 9.30 ± 5.06 ng/mL and 11.27 ± 6.47 ng/mL. After 6 months of therapy, we found that the decrease in AMH level was higher in the metformin group compared to the DLBS3233 group (ΔAMH = 1.83 ng/mL, P = 0.003 and ΔAMH = 1.15 ng/mL, P = 0.077, respectively). However, more side effects were observed in the metformin group compared to the DLBS3233 group (P = 0.01). A total of seven patients (18.42%) were confirmed as pregnant during the study.
Conclusion:
There was a significant decrease in the serum AMH level after administration of either metformin or DLBS3233.
KEYWORDS: Anti-mullerian hormone, DLBS3233, metformin, PCOS, RCT
INTRODUCTION
Worldwide, polycystic ovary syndrome (PCOS) is a common disorder affecting 15–20% of the women in reproductive age.[1] To date, the diagnosis of PCOS remains a challenge because of the wide variety of clinical manifestations. However, the Rotterdam criteria have simplified the diagnosis of PCOS. A patient has to fulfill two out of the following three criteria: (1) oligo- and/or anovulation (OA), (2) hyperandrogenism (either clinical or biochemical) (HA), and (3) polycystic ovaries (PCO) on ultrasound examination, after other etiologies have been excluded.[2] Four different phenotypes in PCOS have been acknowledged based on the following criteria: phenotype A (OA + HA + PCO), phenotype B (HA + OA), phenotype C (HA + PCO), and phenotype D (OA + PCO).[2]
Several factors have been found to be correlated with the development of PCOS, including insulin resistance (found in 50–70% of the patients with PCOS).[3] More recently, anti-Mullerian hormone (AMH), a transforming growth factor-β, was found to be a contributing factor. Because a follicular arrest is present in the patients with PCOS, a study found that serum AMH level may increase up to threefold higher in the patients with PCOS than in controls without PCOS.[4] A recent Indonesian study also found that serum AMH level may increase to 2.5 times that of healthy women.[5] In the Indonesian population, the cutoff value of AMH level in the patients with PCOS is determined as 4.45 ng/mL (sensitivity 76.1% and specificity 74.6%).[5]
Because of the involvement of AMH in the pathogenesis and insulin resistance in the pathophysiology of PCOS, the condition can be managed by administering insulin-sensitizing agents (ISAs), with metformin being the most widely used ISA. However, to date, the effect of ISAs on AMH level remains controversial.[6,7,8,9] Studies reveal that the administration of metformin may reduce the serum level of AMH,[7,9] with several side effects including vomiting.[10] New medications with insulin-sensitizing properties such as bioactive fraction DLBS3233 may become a promising and effective ISA with minimal side effects for the patients with PCOS.[11]
DLBS3233 is a herbal medicine produced in Indonesia containing herbal extracts combination containing Lagerstroemia spesiosa and Cinnamomum burmanii. This medicine has been known to increase glucose uptake by cells as well as adiponectin secretion. DLBS3233 can also stimulate the increase of glucose transporter type 4 (GLUT-4) translocation from the cytoplasm into the membrane and can increase the genetic expression of peroxisome proliferator-activated receptor on messenger ribonucleic acid (mRNA) level, resulting in the synthesis of new GLUT-4. DLBS3233 has also been investigated as an antidiabetic for type 2 diabetes mellitus.[11,12,13]
DLBS3233 has a promising effect on insulin resistance and, therefore, PCOS; however, to our knowledge, no studies have been published on the use of DLBS3233 in the management of PCOS, especially on its effect on serum AMH. This research aims to investigate the effect of ISAs, namely metformin and DLBS3233, on serum AMH.
MATERIALS AND METHODS
This study was a double-blind, randomized, controlled trial conducted between March 2013 and June 2015 at Yasmin Clinic, RSCM Kencana, Jakarta and Hasan Sadikin Hospital, Bandung. The participants were recruited using consecutive sampling and were randomly allocated by a third party to prevent bias and to produce high internal validity.
Inclusion criteria were women of reproductive age between 18 and 40 years, who came to Yasmin clinic, RSCM Kencana or Hasan Sadikin Hospital; diagnosed with PCOS based on the Rotterdam criteria;[2] having homeostatic model assessment-insulin resistance (HOMA-IR) level ≥2.0; and who consented to be included in this study. Pregnant women, lactating mothers, patients who consumed ISAs or oral contraceptive pills, and the patients with Cushing syndrome, late onset congenital adrenal hyperplasia, androgen-secreting tumor, uncontrolled thyroid disease, hyperprolactinemia, or other chronic diseases considered detrimental to thepatient’s health or might influence the results of the study were excluded.
The participants were then divided into the following two groups: (1) 2 × 750 mg metformin and one placebo tablet daily and (2) 1 × 100 mg DLBS3233 and two placebo tablets daily. Monthly follow-up was conducted by interviewing and performing physical examinations on the participants. After follow-up, the participants were given medications for 1 month according to their groups. The participants who did not come back for follow-up or did not consume the medications for two consecutive weeks were considered as dropouts. Serum AMH, urea, creatinine, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) levels were examined at baseline and after 6 months of treatment, or immediately after a participant is confirmed pregnant. At the end of the study, the side effects, menstrual diary, lifestyle, and physical conditions of the participants were also assessed. Serum AMH examination was performed in the integrated laboratory of Faculty of Medicine, Universitas Indonesia using Beckman-Coulter gen II AMH assay (Beckman Coulter, Inc., Brea, CA, USA).
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 software (SPSS Inc., Chicago, IL, USA; IBM Copr. © Copyright IBM Corporation). Serum AMH level was assessed using paired t-test, whereas the side effects of the medications were assessed using one-way analysis of variance. Each study question was analyzed using SPSS version 20.0 software.
This study has been approved by the Ethical Committee of the Faculty of Medicine, Universitas Indonesia.
RESULTS
There were 51 patients who fulfilled the inclusion criteria. All were then randomly divided into the metformin group or the DLBS3233 group. A total of 13 patients dropped out from the study [Figure 1]. Nine patients were lost to follow-up, one patient moved to another city, and three patients felt the duration of treatment was too long. Twenty patients in the metformin group and 18 in the DLBS3233 group were included in the final analysis.
Figure 1.
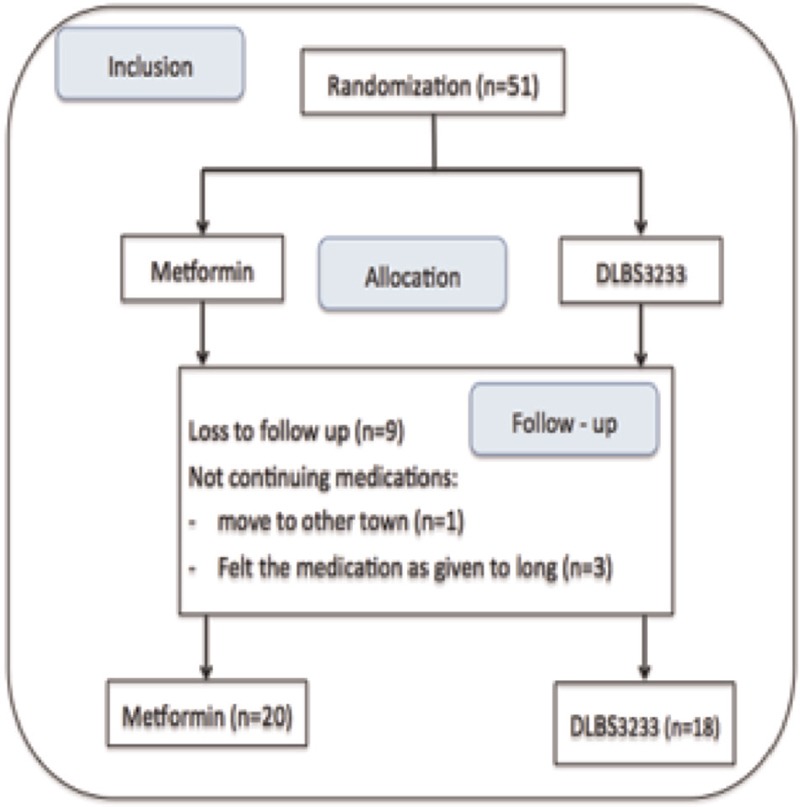
Flow of study
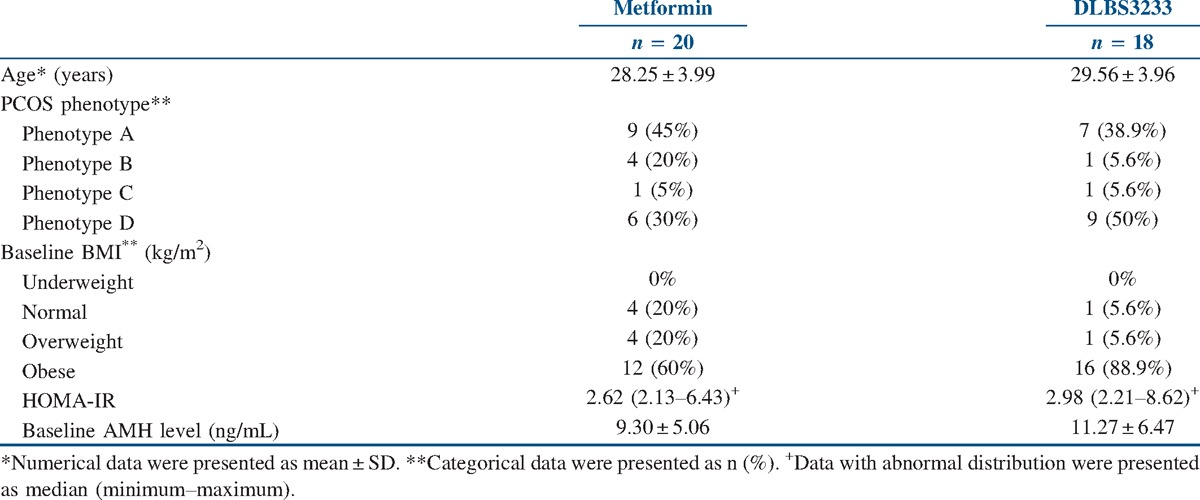
The mean ages were 28.25 ± 3.99 years in the metformin group and 29.56 ± 3.96 years in the DLBS3233 group, with phenotype A as the most common type of PCOS in both the metformin and DLBS3233 groups (45 and 38.9%, respectively). More than 60% of the patients were obese. The mean baseline serum levels of AMH in both groups were 9.30 and 11.27 ng/mL, respectively. There were no significant differences in the characteristics between both the groups [Table 1].
Table 1.
Patients' characteristics
As presented in Table 2, after 6 months of therapy, we found that the decrease in AMH level was higher in the metformin group compared to the DLBS3233 group (ΔAMH = 1.83 ng/mL, P = 0.003 and ΔAMH = 1.15 ng/mL, P = 0.077, respectively).
Table 2.
Baseline and post-treatment serum AMH level
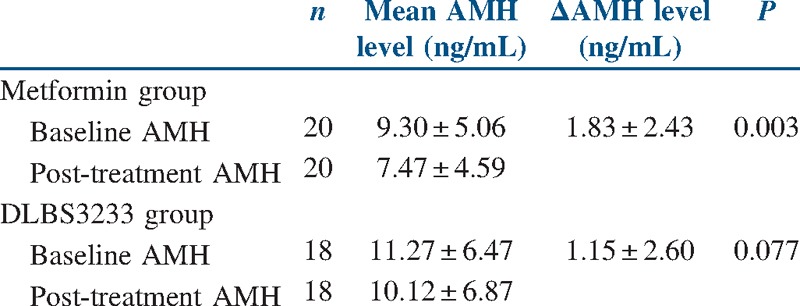
The cutoff point of AMH level, which produced the most significant reduction, was 9.27 ng/mL. Changes in AMH level after metformin or DLBS3233 treatment are presented in Figures 2 and 3.
Figure 2.
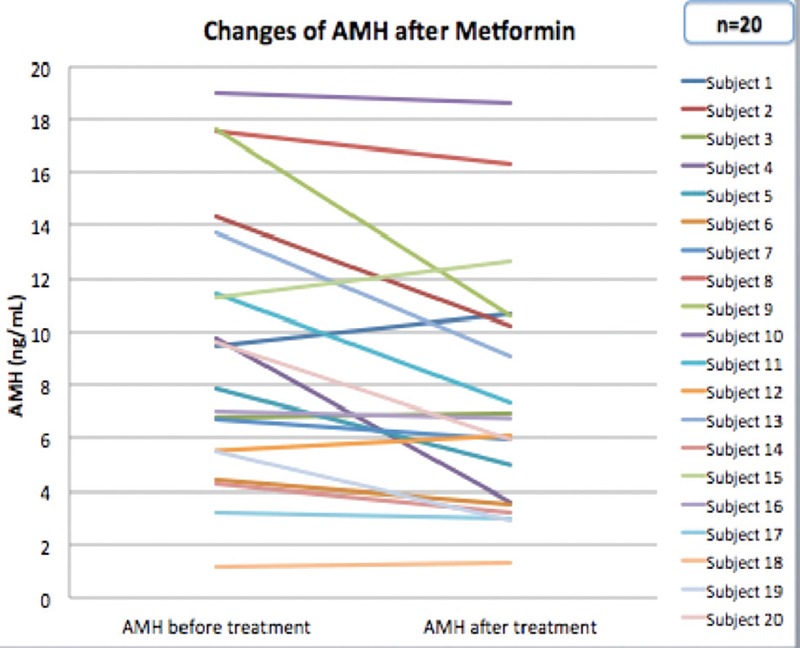
Changes in AMH level after treatment with metformin
Figure 3.
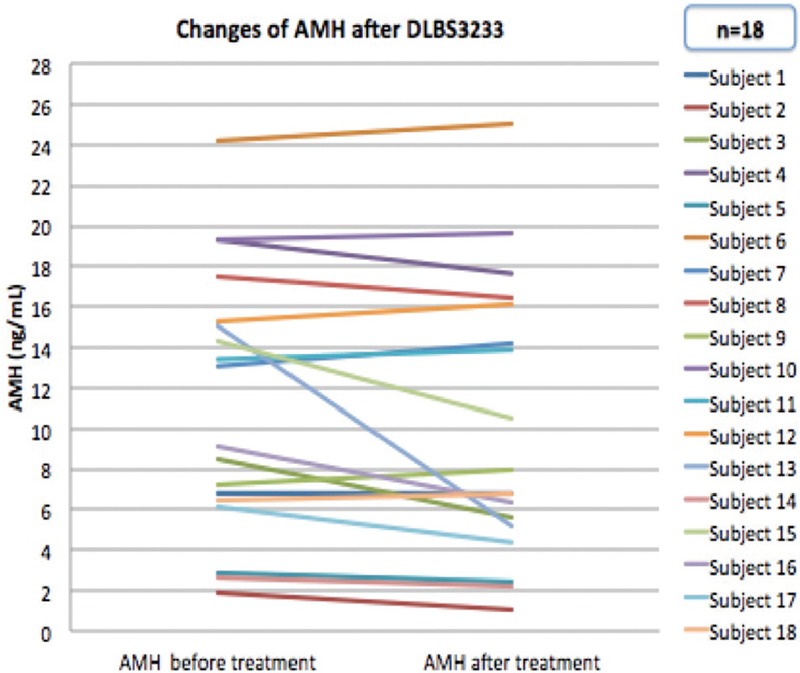
Changes in AMH level after treatment with DLBS3233
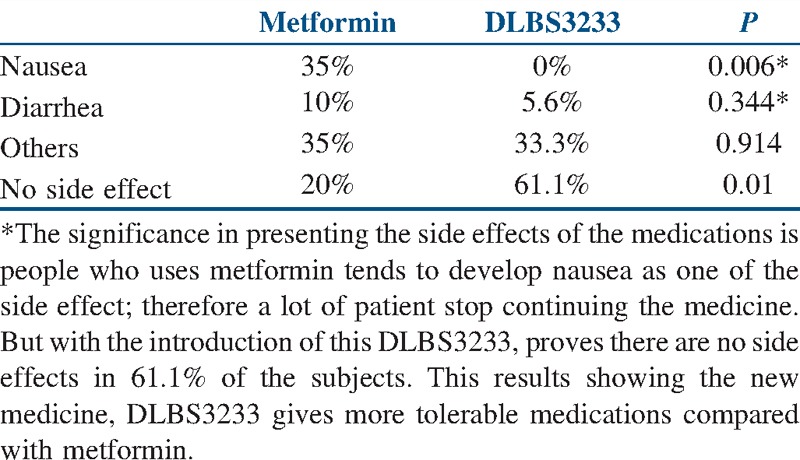
The most common side effect was nausea (P = 0.006) in the metformin group, followed by diarrhea, vomiting, headache, and flu-like syndrome. On the other hand, DLBS3233 induced minimal side effects (P = 0.01) [Table 3].
Table 3.
Side effects of medications
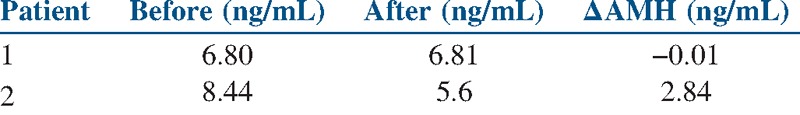
From a total of 38 patients, in the entire study, seven patients (18.42%) conceived naturally, with five (13.16%) in the metformin group [Table 4] and two (5.26%) in the DLBS3233 group [Table 5]. Serum AMH was examined once the patients were confirmed to be pregnant, and treatment was immediately discontinued.
Table 4.
Baseline and post-metformin treatment AMH level in pregnant patients
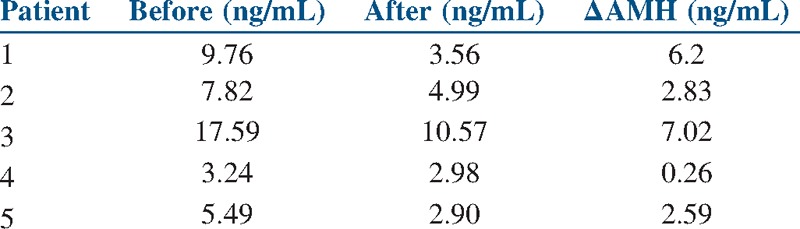
Table 5.
Baseline and post-DLBS3233 treatment AMH level in pregnant patients
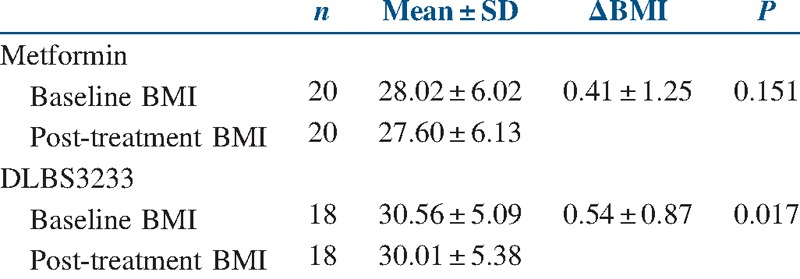
A significant decrease of body mass index (BMI) was observed in the DLBS3233 group. The same effect was not observed in the metformin group [Table 6].
Table 6.
Baseline and post-treatment BMI
DISCUSSION
This study is the first to examine the effect of both metformin and DLBS3233 on serum AMH level. Serum AMH level in both metformin and DLBS3233 groups was initially very high (9.3 ± 5.06 ng/mL and 11.27 ± 6.47 ng/mL, respectively). This finding was consistent with that of previous studies on the patients with PCOS showing increased serum AMH level up to 2.5–3 times than that of women without PCOS (9.5 ± 5.11 vs. 3.53 ± 1.95, P < 0.001).[4,5] AMH is known to decrease follicle sensitivity to follicle-stimulating hormone (FSH); thus, with a high AMH level, folliculogenesis arrest may occur.[14] On the contrary, with low AMH level, the inhibitory effect of AMH can be suppressed and follicle sensitivity to FSH can return to normal. Studies have shown that ISAs can reduce insulin resistance[15] and can also decrease AMH level.[7,9] A study by Fleming et al. examined a patient with PCOS after treatment with 3 × 500 mg metformin daily. The study showed a decreasing level of AMH up to 1.5 ng/mL in the fourth month and 2.3 ng/mL in the eighth month.[7] In this study, both metformin and DLBS3233 decreased AMH level up to 1.83 ng/mL and 1.15 ng/mL, respectively.
To date, the exact mechanism of how ISAs can decrease AMH level remains unclear. The effect of DLBS3233 in the patients with PCOS has not been thoroughly studied, although some studies have shown that DLBS3233 may increase insulin sensitivity.[16,17] It is believed that metformin is capable of improving ovarian morphology by increasing peripheral resistance to insulin and increasing sex-hormone binding globulin level in the liver. These mechanisms are believed to be capable of normalizing luteinizing hormone (LH) level, thus increasing FSH level.[18,19,20]
Recently, the use of metformin in the management of PCOS is proven to be superior to pioglitazone. After treatment with metformin, the rate of ovulation induction is higher than placebo [odds ratio (OR) 3.88; 95% confidence interval (CI) 2.25–6.69; number needed to treat (NNT) 4.4].[15] Another study by Kandarakis[16] also showed less insulin resistance and a decreasing level of androgen in the obese-type patients with PCOS who received 2 × 850 mg metformin daily for 6 months. In this study, as many as 13.15% of the patients conceived spontaneously after the administration of metformin.
However, a 2012 systematic review by Tang et al.[17] found that there were some side effects with metformin, especially nausea (OR 4.27; 95% CI 2.4–7.59). This gives rise for the need of a new ISA with less side effects. DLBS3233 has been shown to have a positive outcome without serious side effects. Tjandrawinata et al.[13] found that the administration of DLBS3233 did not cause gastrointestinal disturbances and had a lower risk of hypoglycemic episodes. In this study, no patient experienced nausea after treatment with DLBS3233 (P = 0.006). Other side effects such as diarrhea and headaches were also considerably less compared to the metformin group. Overall side effects in the DLBS3233 group were significantly lower than in the metformin group (P = 0.01). After the administration of ISAs, seven patients (18.26%) conceived naturally, with five in the metformin group and two in the DLBS3233 group. Most patients conceived 3 months after the start of treatment. A meta-analysis by Palomba et al.[21] in 2014 demonstrated that the use of metformin would increase the pregnancy rate (OR 2.25; 95% CI 1.10–3.44; P = 0.02).
Our study has several limitations. First, the number of patients was relatively small. Second, there was a high level of dropout (25%) from this study because of its long duration. Third, this study did not investigate the DLBS3233 mechanism of action in reducing serum AMH level.
In conclusion, both metformin and DLBS3233 could decrease the serum level of AMH. However, DLBS3233 showed fewer side effects compared to metformin. Further studies are needed to investigate the exact mechanism of ISAs in reducing AMH level.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors take full responsibility for the content of this article and wish to thank to all the members of Indonesian Reproductive Medicine Research and Training Center (INA-REPROMED), Division of Reproductive Endocrinology and Infertility Department of Obstetric and Gynecology, Faculty of Medicine, Universitas Indonesia; Dr. Cipto Mangunkusumo, General Hospital, Jakarta, Indonesia; and Yasmin, IVF Clinic.
REFERENCES
- 1.Sirman S, Pate KA. Epidemiology, diagnosis and management of polycystic ovary syndrome. J Clin Epidemiol. 2014;6:1–13. doi: 10.2147/CLEP.S37559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Rotterdam ESHRE/ASRM-sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS) Hum Reprod. 2004;19:41–7. doi: 10.1093/humrep/deh098. [DOI] [PubMed] [Google Scholar]
- 3.Bako AU, Morad S, Atiomo W. Polycystic ovary syndrome: An overview. Rev Gynaecol Pract. 2005;5:115–22. [Google Scholar]
- 4.Pigny P, Jonard S, Robert Y, Dewailly D. Serum anti-Müllerian hormone as a surrogate for antral follicle count for definition of the polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91:941–5. doi: 10.1210/jc.2005-2076. doi: 10.1210/jc. 2005-2076. [DOI] [PubMed] [Google Scholar]
- 5.Wiweko B, Maidarti M, Priangga MD, Shafira N, Fernando D, Sumapraja K, et al. Anti-Mullerian hormone as a diagnostic and prognostic tool for PCOS patients. J Assist Reprod Genet. 2014;31:1311–16. doi: 10.1007/s10815-014-0300-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saleh BO, Ibraheem WF, Ameen NS. The role of anti-Mullerian hormone and inhibin B in the assessment of metformin therapy in women with polycystic ovarian syndrome. Saudi Med J. 2015;36:562–7. doi: 10.15537/smj.2015.5.11112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleming R, Harborne L, MacLaughlin DT, Ling D, Norman J, Sattar N, et al. Metformin reduces serum Mullerian-inhibiting substance levels in women with polycystic ovary syndrome after protracted treatment. Fertil Steril. 2005;83:130–6. doi: 10.1016/j.fertnstert.2004.05.098. [DOI] [PubMed] [Google Scholar]
- 8.Nascimento AD, Silva Lara LA, Japur de Sa Rosa-e-Silva AC, Ferriani RA, Reis RM. Effects of metformin on serum insulin and anti-Mullerian hormone levels and on hyperandrogenism in patients with polycystic ovary syndrome. Gynecol Endocrinol. 2013;29:246–9. doi: 10.3109/09513590.2012.736563. [DOI] [PubMed] [Google Scholar]
- 9.Neagu M, Cristescu C. Anti-Mullerian hormone − A prognostic marker for metformin therapy efficiency in the treatment of women with infertility and polycystic ovary syndrome. J Med Life. 2012;5:462–4. [PMC free article] [PubMed] [Google Scholar]
- 10.Hundal R, Inzucchi S. Metformin: New understandings, new uses. Drugs. 2003;18:1879–94. doi: 10.2165/00003495-200363180-00001. [DOI] [PubMed] [Google Scholar]
- 11.Tjandrawinata RR, Suastika K, Nofiamy D. DLBS3233 extract, a novel insulin sensitizer with negligible risk of hypoglycemia: A phase-I study. Int J Diabetes Metabol. 2012;21:13–20. [Google Scholar]
- 12.Tandrasasmita OM, Wulan DD, Nailufar F, Sinambela J, Tjandrawinata RR. Glucose-lowering effect of DLBS3233 is mediated through phosphorylation of tyrosine and upregulation of PPARgamma and GLUT4 expression. Int J Gen Med. 2011;4:345–57. doi: 10.2147/IJGM.S16517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tjokroprawiro A, Murtiwi S, Tjandrawinata RR. DLBS3233, a combined bioactive fraction of Cinnamomum burmanii and Lagerstroemia speciosa, in type-2 diabetes mellitus patients inadequately controlled by metformin and other oral antidiabetic agents. J Complement Integr Med. 2016;13:413–20. doi: 10.1515/jcim-2016-0031. [DOI] [PubMed] [Google Scholar]
- 14.Gruijters M, Visser JA, Durlinger AL, Themmen AP. Anti-Mullerian hormone and its role in ovarian function. Mol Cell Endocrinol. 2003;211:85–90. doi: 10.1016/j.mce.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Lord JM, Flight IH, Norman RJ. Insulin-sensitising drugs (metformin, troglitazone, rosiglitazone, pioglitazone, D-chiro-inositol) for polycystic ovary syndrome. Cochrane Database Syst Rev. 2003:CD003053. doi: 10.1002/14651858.CD003053. [DOI] [PubMed] [Google Scholar]
- 16.Kandarakis E, Kouli C, Trianateli T, Bergiele A. Therapeutic effects of metformin on insulin resistance and hyperandrogenism in polycystic ovary syndrome. Eur J Endocrinol. 1998;138:269–74. doi: 10.1530/eje.0.1380269. [DOI] [PubMed] [Google Scholar]
- 17.Tang T, Lord JM, Norman RJ, Yasmin E, Balen AH. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev. 2012;5:CD003053. doi: 10.1002/14651858.CD003053.pub5. [DOI] [PubMed] [Google Scholar]
- 18.Bayrak A, Terbell H, Urwitz-Lane R, Mor E, Stanczyk FZ, Paulson RJ. Acute effects of metformin therapy include improvement of insulin resistance and ovarian morphology. Fertil Steril. 2007;87:870–5. doi: 10.1016/j.fertnstert.2006.08.096. [DOI] [PubMed] [Google Scholar]
- 19.Piltonen T, Morin-Papunen L, Koivunen R, Perheentupa A, Ruokonen A, Tapanainen JS. Serum anti-Mullerian hormone levels remain high until late reproductive age and decrease during metformin therapy in women with polycystic ovary syndrome. Hum Reprod. 2005;20:1820–6. doi: 10.1093/humrep/deh850. [DOI] [PubMed] [Google Scholar]
- 20.Falbo A, Rocca M, Russo T, D’Ettore A, Tolino A, Zullo F. Serum and follicular anti-Mullerian hormone levels in women with polycystic ovary syndrome (PCOS) under metformin. J Ovarian Res. 2010;3:16. doi: 10.1186/1757-2215-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palomba S, Falbo A, La Sala G. Metformin and gonadotropins for ovulation induction in patients with polycystic ovary syndrome: A systematic review with meta-analysis of randomized controlled trials. Reprod Biol Endocrinol. 2014;12:3. doi: 10.1186/1477-7827-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


