Abstract
Purpose:
The purpose of this study was to evaluate the clinical outcome and efficacy of transurethral resection of the prostate in patients of benign prostatic enlargement (BPE) with underactive bladder.
Materials and Methods:
Retrospective study of 174 patients, who underwent transurethral resection of prostate (TURP) between 2008 and 2015, for lower urinary tract symptoms with BPE with bladder underactivity. Clinical history, physical examination, renal function test, urinalysis, cystourethroscopy, transabdominal or transrectal ultrasonography, and urodynamic study were recorded. Patients having a history of neurologic conditions, spinal trauma or surgery, pelvic trauma or surgery, diabetes mellitus with end organ damage, urethral pathology or surgery, and prostatic cancer were excluded from the study.
Results:
The mean follow-up period was 22.4 ± 6.2 months. Mean prostate volume was 42.8 ± 6.4 ml and mean serum prostate-specific antigen was 2.3 ± 1.8 ng/ml. The International Prostate Symptom Score changed from 24.6 ± 4.2 preoperatively to 10.8 ± 5.8 postoperatively which was found statistically significant. Quality of life (QOL) score changed from 4.8 ± 1.2 to 2.6 ± 0.4. Twenty-two patients out of 174 remained on a per-urethral catheter or clean intermittent catheterization due to voiding failure after TURP beyond 1 month.
Conclusions:
TURP should be considered a viable treatment option in men with enlarged prostate with underactive detrusor who had poor response to medical treatment. Preoperative counseling and postoperative follow-up are crucial in the management of such patients.
Key Words: Benign prostatic enlargement, quality of life, transurethral resection of prostate, underactive bladder, urodynamic study
INTRODUCTION
Transurethral resection of prostate (TURP) is a time-tested gold standard surgical option for dealing with lower urinary tract symptoms (LUTS) in men having benign prostatic enlargement (BPE). About one-third of patients having LUTS have no evidence of BPE. Persistence of LUTS is reported in 5%–35% of patients undergoing TURP.[1] Detrusor underactivity is regarded as a common association for persistence of symptoms after TURP in such patients.[2,3] According to the International Continence Society, detrusor underactivity is defined as decreased strength or duration leading to prolongation of bladder emptying and/or inability of bladder to achieve complete emptying within normal micturition span.[4] Schäfer[5] derived bladder contractility index (BCI) from urodynamic variables and denoted bladder contractions as strong (BCI >150), normal strength (100≤ BCI <150), or weak detrusor contractility (BCI <100). However, no well-defined urodynamic parameters/criteria exist for detrusor underactivity. Conflicting results create dilemma about the efficacy and results of TURP in patients with LUTS with BPE and bladder underactivity of nonneurologic origin.[6] Detrusor underactivity is considered a poor predictor of outcome after TURP[7] though some authors have reported the beneficial results of TURP in patients with underactive detrusor.[8,9,10] Detrusor failure occurs secondary to long-standing outflow obstruction leading to damage of innervation or the ultrastructure morphology of detrusor muscle.[11]
In this study, we evaluated the clinical outcome and efficacy of TURP in patients of BPE with detrusor underactivity.
MATERIALS AND METHODS
This study was conducted in the Department of Urology, King George's Medical University, Lucknow, Uttar Pradesh. We retrospectively reviewed medical records of 1152 patients, who underwent TURP between July 2008 and June 2015, after failed medical therapy for LUTS with BPE. Out of 1152 men, 174 (mean age 64.4 ± 8.6 years) were included in the final analysis of our study showing detrusor underactivity (BCI <100) at urodynamic study.
Preoperative data including detailed clinical history, International Prostate Symptom Score (IPSS), and quality of life (QOL) score and physical examination including digital rectal examination, renal function test, urinalysis, postvoid residual urine (PVRU) measurement, serum prostate-specific antigen (PSA), cystourethroscopy, transabdominal or transrectal, and urodynamic study were recorded. Prostate size was measured by transabdominal ultrasonography in majority of patients and by transrectal ultrasonography in selected patients. As per our institutional protocol, all patients underwent cystoscopy preoperatively under local anesthesia. All patients had features of enlarged prostate on cystoscopy. Urodynamic study was routinely performed at our center preoperatively to prognosticate the outcome and in patients with LUTS disproportionate to prostate size.
Patients having a history of congenital or acquired neurologic conditions, neurogenic bladder, spinal trauma or surgery, pelvic trauma or surgery, diabetes mellitus with end organ damage, urethral pathology or surgery, and prostatic cancer were excluded from the study.
Urodynamic study was performed using the DUET® LOGIC G2 (Mediwatch UK Ltd.,) with a 7 F catheter at filling rate of 10–20 ml/min. Along with evaluation of bladder function with pressure flow studies, BCI (BCI = pdetQmax + 5 Qmax) and bladder outlet obstruction index (BOOI = pdetQmax – 2 Qmax) were calculated. BOOI was categorized as obstructed value >40 and unobstructed <40 and BCI denotes detrusor contractility as normal >100 or weak <100.[12,13] All patients were instructed to discontinue all medications having an impact on a detrusor function, such as anticholinergics, sedatives, and sympathomimetic, for 4–5 half-life of drugs before urodynamic study to assess bladder function appropriately.
As per our institutional protocol, all patients were counseled preoperatively regarding the outcome of TURP and possibility of clean intermittent catheterization (CIC) postoperatively. TURP was performed using standard technique with tungsten cutting wire loop using setting of 160 W of cutting current and 80 W of coagulating current. All procedures were performed by the urologists under spinal anesthesia used as per anesthetist's decision. Bladder irrigation was used in all cases until hematuria had cleared significantly.
Patients were evaluated at follow-up visit at 3 months. At follow-up visit, we recorded clinical history, IPSS and QOL score, PVRU, and urodynamic parameters.
Statistical analysis
Unpaired t-test was used to compare continuous data and Fisher's exact test was used to analyze categorical data. Statistical analysis was performed using SPSS®, version 16 (Chicago, IL, USA). The statistical significance level used up to P < 0.05. Data for risk factors were analyzed for univariate association with the study outcome.
RESULTS
The mean follow-up period was 22.4 ± 6.2 months (range, 7.2 43 months). Mean prostate volume was 42.8 ± 6.4 ml. Twenty-eight patients had a history of preoperative catheterization with mean duration of preoperative catheterization 27.6 ± 8.1 days (range, 11–46 days), and PVRU volume was 112.4 ± 30.2 ml. The mean serum creatinine was 0.9 ± 0.2 mg/dl (range, 0.7–2.3 mg/dl) and mean serum PSA was 2.3 ± 1.8 ng/ml.
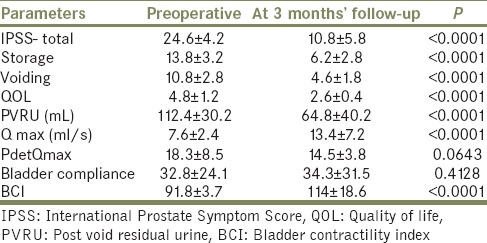
Twenty-two patients out of 174 (12.64%) remain on per-urethral catheter or CIC due to voiding failure after TURP beyond 1 month. Comparison of preoperative and post-TURP variables at 3 months is depicted in Table 1.
Table 1.
Comparison of preoperative and postoperative (at 3 month) follow up parameters
DISCUSSION
The surgical outcome of TURP in patients of BPE with detrusor underactivity remains debatable due to paucity of data. Geriatric patients are difficult to treat population having multiple comorbidities, long-lasting high postvoid residual (PVR), decompensated detrusor, and multiple drug intake having an impact on the urinary system. Clinical and urodynamic parameters remain in the armamentarium for predicting surgical outcome in patients with detrusor underactivity and prostatic enlargement.
Te and Kaplan[14] demonstrated detrusor underactivity in 17% men presenting with LUTS after urodynamic evaluation and Ameda et al.[15] found detrusor underactivity in 31% of symptomatic male without evidence of bladder outlet obstruction (BOO). At our center, among the patients who underwent TURP, 15% of patients demonstrated underlying detrusor underactivity on the preoperative urodynamic study.
Seki et al.[16] conducted a retrospective study of 190 patients having BPE with detrusor underactivity. They reported outcome of each variable (storage and voiding symptoms, QOL, maximum urinary flow rate) after TURP suboptimal when compared with normal detrusor function patients. Age of patients and the preoperative level of BOO independently affected post-TURP Qmax in their study.
In our study, at 3 months follow-up, a significant improvement in the IPSS, QOL, and PVRU was recorded in patients with detrusor underactivity. IPSS changed from 24.6 ± 4.2 preoperatively to 10.8 ± 5.8 after TURP which was found statistically as well as clinically significant. Impact on QOL after TURP in these patients became obvious by significant change in QOL score from 4.8 ± 1.2 to 2.6 ± 0.4. Both storage and voiding symptoms improved after TURP although voiding symptoms were relieved more than storage symptoms. Seki et al. reported in his study which had a population with a mean age of 71.3 ± 7.1 years while in our study mean age was 64.4 years (range, 50–91 years), which might be a possible reason for the suboptimal outcome of their study.
In literature, advanced age, preoperative detrusor underactivity, and high PVRU are described as risk factors and predictors of poor surgical outcome while no association of symptom score and prostate size is established.[17,18] Twenty-two patients of 174 were unable to void or having high PVRU leading to renal function damage, such patients were kept on permanent per-urethral catheter or CIC postoperatively.
We studied failure population with a keen interest in an effort to find out definite predictors of TURP outcome. Eighteen patients out of 22 preoperatively had decreased anal tone on digital rectal examination, which was documented subjectively; and all patients had a high PVRU volume (>150 ml) in our study. Twenty-two (12.6%) patients were unable to void after TURP. Intra- and post-operative complications of TURP were similar among these patients when compared with normal detrusor patients as described in the literature.[19,20,21] Overall, based on our study results, we advocate TURP in patients of detrusor underactivity with BPE with LUTS, because no major negative impact on QOL occurred. The majority of patients were benefited and few (12.6%) remained as such as they were preoperatively.
Alison et al. reported ultrastructural detrusor changes on biopsy as a predictive finding for voiding failure postoperatively, which included muscle cell shape, muscle cell size, disorganized fascicle, and collagenosis. Detrusor ultrastructural changes and its clinical implication always remain in research.[22] We had no documentation of detrusor tissue biopsy sampling.
Al-Hayek et al.[23] reported that surgical correction of outflow obstruction does not necessarily improve bladder contractility in men with normal or underactive detrusor. In patients with diagnosed underactive detrusor preoperatively, a higher value of detrusor pressure results in a better postoperative surgical outcome.[24] In our study, we found statistically significant improvement in calculating BCI at follow-up; however, pdetQmax was not significantly changed. Qmax changed from 7.6 ± 2.4 to 13.4 ± 7.2 after TURP; however, at this point, detrusor pressure changed only from 18.3 ± 8.5 to 14.5 ± 3.8, respectively. Improvement in BCI was a reflection of significant improvement in Qmax in our study, which ultimately led to decreased PVRU volume and better symptom score in our patients.
Patients of detrusor underactivity with enlarged prostate having large volume urinary retention had a vicious cycle leading further detrusor weakness and irreversible damage. Bladder compliance is a measure of the viscoelastic nature of the urinary bladder, which in turn is determined by viscoelastic properties of the various components of the bladder, such as collagen, elastin, and smooth muscle.[25] In our study, bladder compliance did not improve after TURP on follow-up study suggesting irreversible changes in detrusor. Patients reported improved urinary flow rate, which resulted from decreased outlet resistance after TURP in these patients of detrusor underactivity.
The strength of our study include: (1) We studied TURP outcome among a unique cohort of detrusor underactivity with BPO with LUTS, which always remains in the gray zone; (2) we performed an analysis of 174 patients, over 7 years, which is among one of the largest and longest study to author's knowledge.
Limitation of our study is that it is a retrospective study. Definite preoperative predictors of surgical outcome could not be identified. We had no data regarding detrusor muscle histological changes for further research on ultrastructural changes.
Patients having decreased anal tone and high PVR urine volume preoperatively had a poor surgical outcome. Clinical and urodynamic predictors of surgical outcome in patients of prostatic enlargement having LUTS with underactive bladder need further prospective studies with long follow-up to reach up to a definite consensus.
CONCLUSION
TURP should be considered a viable treatment option in men with enlarged prostate with underactive detrusor who had poor response to medical treatment. Preoperative counseling and postoperative follow-up are crucial in the management of such patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I acknowledge the cooperation of residents of the Urology Department of King George's Medical University who participated in data collection and evaluation of the patient. We also appreciate the commitment and compliance of the patients who reported the required data.
REFERENCES
- 1.Kanik EA, Erdem E, Abidinoglu D, Acar D, Akbay E, Ulusoy E. Can the outcome of transurethral resection of the prostate be predicted preoperatively? Urology. 2004;64:302–5. doi: 10.1016/j.urology.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 2.Schafer W. The value of free flow rate and pressure/flow-studies in the routine investigation of BPH patients. Neurourol Urodyn. 1988;7:219–21. [Google Scholar]
- 3.Rollema HJ, Van Mastrigt R. Improved indication and followup in transurethral resection of the prostate using the computer program CLIM: A prospective study. J Urol. 1992;148:111–5. doi: 10.1016/s0022-5347(17)36527-8. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the international continence society. Neurourol Urodyn. 2002;21:167–78. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 5.Schäfer W. Analysis of bladder-outlet function with the linearized passive urethral resistance relation, linPURR, and a disease-specific approach for grading obstruction: From complex to simple. World J Urol. 1995;13:47–58. doi: 10.1007/BF00182666. [DOI] [PubMed] [Google Scholar]
- 6.Han DH, Jeong YS, Choo MS, Lee KS. The efficacy of transurethral resection of the prostate in the patients with weak bladder contractility index. Urology. 2008;71:657–61. doi: 10.1016/j.urology.2007.11.109. [DOI] [PubMed] [Google Scholar]
- 7.Javlé P, Jenkins SA, Machin DG, Parsons KF. Grading of benign prostatic obstruction can predict the outcome of transurethral prostatectomy. J Urol. 1998;160:1713–7. [PubMed] [Google Scholar]
- 8.Ou R, Pan C, Chen H, Wu S, Wei X, Deng X, et al. Urodynamically diagnosed detrusor hypocontractility: Should transurethral resection of the prostate be contraindicated? Int Urol Nephrol. 2012;44:35–9. doi: 10.1007/s11255-011-0010-2. [DOI] [PubMed] [Google Scholar]
- 9.Masumori N, Furuya R, Tanaka Y, Furuya S, Ogura H, Tsukamoto T. The 12-year symptomatic outcome of transurethral resection of the prostate for patients with lower urinary tract symptoms suggestive of benign prostatic obstruction compared to the urodynamic findings before surgery. BJU Int. 2010;105:1429–33. doi: 10.1111/j.1464-410X.2009.08978.x. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka Y, Masumori N, Itoh N, Furuya S, Ogura H, Tsukamoto T. Is the short-term outcome of transurethral resection of the prostate affected by preoperative degree of bladder outlet obstruction, status of detrusor contractility or detrusor overactivity? Int J Urol. 2006;13:1398–404. doi: 10.1111/j.1442-2042.2006.01589.x. [DOI] [PubMed] [Google Scholar]
- 11.Neal DE, Styles RA, Powell PH, Ramsden PD. Relationship between detrusor function and residual urine in men undergoing prostatectomy. Br J Urol. 1987;60:560–6. doi: 10.1111/j.1464-410x.1987.tb05042.x. [DOI] [PubMed] [Google Scholar]
- 12.Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: Three simple indices to define bladder voiding function. BJU Int. 1999;84:14–5. doi: 10.1046/j.1464-410x.1999.00121.x. [DOI] [PubMed] [Google Scholar]
- 13.Griffith D, van Mastrigt R, Bosch R. Quantification of urethral resistance and bladder function during voiding, with special reference to the effects of prostate size reduction on urethral obstruction due to benign prostatic hyperplasia. Neurourol Urodyn. 1989;8:17–27. [Google Scholar]
- 14.Te AE, Kaplan SA. Urodynamics and benign prostatic hyperplasia. Textbook of Benign Prostatic Hyperplasia. 1996;1:187–98. [Google Scholar]
- 15.Ameda K, Sullivan MP, Bae RJ, Yalla SV. Urodynamic characterization of nonobstructive voiding dysfunction in symptomatic elderly men. J Urol. 1999;162:142–6. doi: 10.1097/00005392-199907000-00035. [DOI] [PubMed] [Google Scholar]
- 16.Seki N, Kai N, Seguchi H, Takei M, Yamaguchi A, Naito S. Predictives regarding outcome after transurethral resection for prostatic adenoma associated with detrusor underactivity. Urology. 2006;67:306–10. doi: 10.1016/j.urology.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: Immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients 1989. J Urol. 2002;167(2 Pt 2):999–1003. [PubMed] [Google Scholar]
- 18.Djavan B, Madersbacher S, Klingler C, Marberger M. Urodynamic assessment of patients with acute urinary retention: Is treatment failure after prostatectomy predictable? J Urol. 1997;158:1829–33. doi: 10.1016/s0022-5347(01)64139-9. [DOI] [PubMed] [Google Scholar]
- 19.Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: A randomized prospective trial in 200 patients. J Urol. 2004;172:1012–6. doi: 10.1097/01.ju.0000136218.11998.9e. [DOI] [PubMed] [Google Scholar]
- 20.Muzzonigro G, Milanese G, Minardi D, Yehia M, Galosi AB, Dellabella M. Safety and efficacy of transurethral resection of prostate glands up to 150 ml: A prospective comparative study with 1 year of followup. J Urol. 2004;172:611–5. doi: 10.1097/01.ju.0000131258.36966.d1. [DOI] [PubMed] [Google Scholar]
- 21.Berger AP, Wirtenberger W, Bektic J, Steiner H, Spranger R, Bartsch G, et al. Safer transurethral resection of the prostate: Coagulating intermittent cutting reduces hemostatic complications. J Urol. 2004;171:289–91. doi: 10.1097/01.ju.0000098925.76817.3a. [DOI] [PubMed] [Google Scholar]
- 22.Blatt AH, Brammah S, Tse V, Chan L. Transurethral prostate resection in patients with hypocontractile detrusor – What is the predictive value of ultrastructural detrusor changes? J Urol. 2012;188:2294–9. doi: 10.1016/j.juro.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Al-Hayek S, Thomas A, Abrams P. Natural history of detrusor contractility. Scand J Urol Nephrol. 2004;38:101–8. doi: 10.1080/03008880410015453. [DOI] [PubMed] [Google Scholar]
- 24.Ghalayini IF, Al-Ghazo MA, Pickard RS. A prospective randomized trial comparing transurethral prostatic resection and clean intermittent self-catheterization in men with chronic urinary retention. BJU Int. 2005;96:93–7. doi: 10.1111/j.1464-410X.2005.05574.x. [DOI] [PubMed] [Google Scholar]
- 25.Macarak EJ, Howard PS. The role of collagen in bladder filling. Adv Exp Med Biol. 1999;462:215–23. doi: 10.1007/978-1-4615-4737-2_17. [DOI] [PubMed] [Google Scholar]


