Abstract
Objective
social inequalities in health are believed to arise in part because individuals make use of social and economic resources in order to improve survival. In recent years, health literacy has received increased attention as a factor that can help explain differences in health outcomes. However, examination of life course predictors of health literacy has been limited.
Methods
life course data from the Wisconsin Longitudinal Study 1957–2011 were used to examine predictors of health literacy in old age (N = 2,122), using the Newest Vital Sign. Generalised structural equation modelling was used to model pathways to health literacy.
Results
predictors of health literacy included educational attainment, and adolescent cognitive and non-cognitive skills, and, in men, rate of cognitive decline from middle to later life.
Discussion
numerous studies have documented health literacy issues among older adults, and recommendations have been made for ways to improve health literacy for this population. This study reports on risk factors across the life course that are associated with health literacy later in life, identifying possible intervention targets to reduce risk of poor health as people age. Our results suggest that a range of life course factors, beginning in early life, predict health literacy. Further research studying health literacy over the life course is warranted.
Keywords: health literacy, life course epidemiology, social inequalities in health, cognitive epidemiology, psychology, older people
Background
Health self-management is integral to healthy ageing and lowered disease burden. For example, the US government's Healthy People 2020 policy [1], American Heart Association's cardiovascular health guidelines [2] and American Cancer Society's cancer prevention guidelines [3] offer behavioural change as a main mechanism for improving health. Indeed, these policies are informed by health belief models [4] and theories of planned behaviours [5], which tend to focus on choices and promote ‘capability’ or self-efficacy as the mechanism of action [6].
Health literacy has been increasingly used as an explanation for why some are at risk of having difficulties navigating healthcare and treatment routines [7]. Defined as ‘the degree to which individuals have the capacity to obtain, process and understand basic information and services needed to make appropriate decisions regarding their health’ [8], health literacy tends to be lower in populations with lower incomes, lower education and older ages [9, 10].
Intervening to improve health in patients with low health literacy requires that we understand its influencing factors, and consider individual characteristics in the face of health system demands and a complex information environment [11]. One key factor that may impact health literacy is cognitive function, which declines with age [7]. In fact, recent research finds that health literacy is associated with indicators of lifetime cognitive function [12–14]. Research further suggests that providers should consider the potential for cognitive burden when making recommendations about the potential for patient self-management in older populations [15, 16].
While there are a number of studies about cognitive function and health literacy, less is known about how health literacy develops across the life course in general, and relatively little is known about how cognitive function interacts with other factors over the life course to impact health literacy. Childhood cognition was found to be a significant predictor of midlife literacy and numeracy in the British 1946 birth cohort [17], but little is known about the association between non-cognitive skills and health literacy. Non-cognitive skills, sometimes referred to as ‘grit’, were found to be a stronger adolescent predictor of later life cognition than adolescent cognition in the Wisconsin Longitudinal Study (WLS) [18]. However, to our knowledge, these factors have not been studied in relation to health literacy.
Objective
This study examined early and midlife correlates of late-life health literacy.
Hypotheses
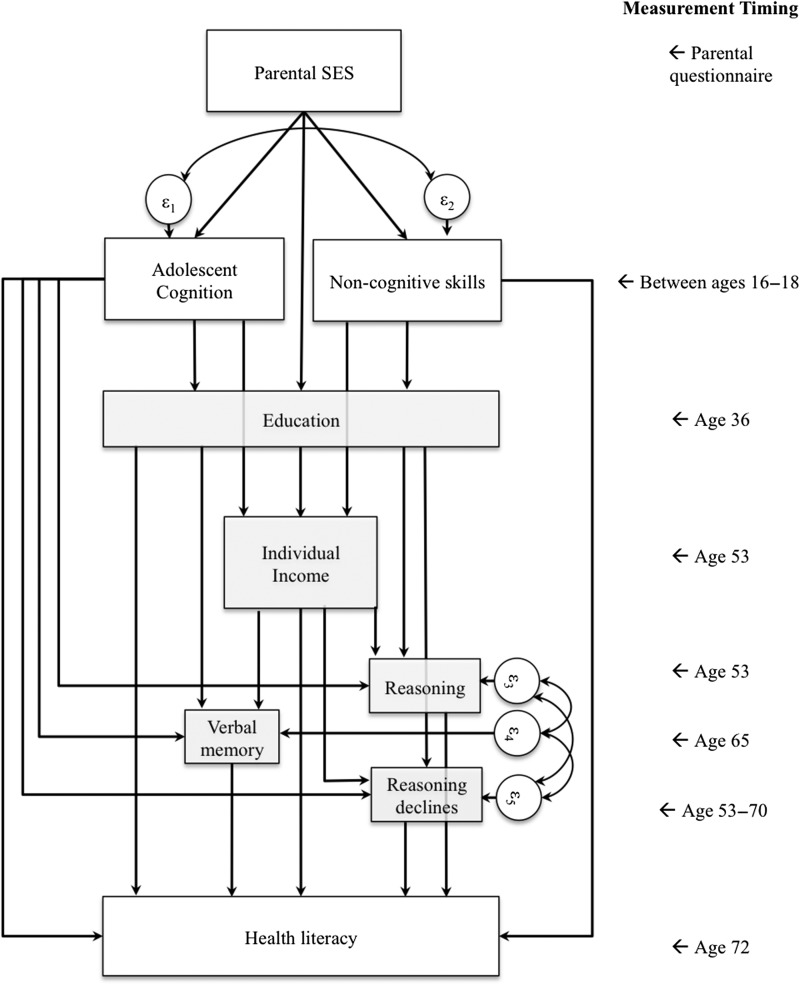
Lower education, poorer adolescent non-cognitive skills, poorer lifetime cognitive function and more rapid cognitive decline will directly predict poorer health literacy (Figure 1 for theoretical model). Parental socioeconomic status (SES) will have an indirect influence on health literacy through these pathways.
Figure 1.
Hypothesised linkages between socioeconomic inequalities, cognitive performance and late-life health literacy alongside legend showing timing of measurement in the WLS 1957–2011.
Methods
Data
Secondary data analyses were conducted using the WLS, which prospectively followed 10,317 individuals who graduated from high school in Wisconsin in 1957 (Figure 1) at ages 18, 25, 36, 53, 65 and 72 (in 2011; www.ssc.wisc.edu) [19]. At age 72, the WLS newly incorporated a measure of health literacy among a random subsample of respondents (n = 2,212) that year. Of the original sample, 2,049 had died, 1,080 had permanently refused, 940 refused the current wave and 96 were lost to follow-up leaving 6,152 individuals who participated in the 2011 wave.
Outcome
The Newest Vital Sign (NVS) is commonly used to quickly assess health literacy [20]. Respondents are shown a sample nutrition label and asked a series of six questions by an interviewer; the questions assess reading, comprehension and numeracy skills using a common nutritional label. The NVS scores the number of correct answers. While requiring only 3 min to administer, the NVS is reliable (Cronbach's α > 0.76), and has good accuracy (Area under the receiver-operating curve = 0.88) at a common cutoff (NVS <4) to detect poor health literacy [20]. Following standard practice, the NVS was dichotomised to identify low health literacy (NVS <4); sensitivity analyses using the full NVS range provide similar results.
Developmental indicators
Early-life indicators included adolescent cognition and non-cognitive skills. Adolescent cognition was measured at age 16 by the State of Wisconsin using the Henmon–Nelson test [19]. Results were linked to respondent surveys. On average, respondents did not differ from the rest of the State of Wisconsin at age 16, but the State performed better scores on this test than other US States. Non-cognitive skills are generally defined as motivation, perseverance and tenacity [21]. This study has no direct measure of non-cognitive skills; however, the economic literature examining non-cognitive skills has reliably used residual differences between cognitive scores and school grades [22]. To measure non-cognitive skills, we utilise high school rankings and adjust for cognitive performance. Both cognition and non-cognitive skills were standardised to facilitate comparison.
Adult cognition
Aging-related decline in cognitive ability may reduce health literacy; we used three indicators to examine such declines: abstract reasoning, verbal memory and individual declines in abstract reasoning. Abstract reasoning was the only measure of cognition at age 53, 65 and 72, and consistently included the similarities component of the Weschler Revised test [23]. To account for declining cognitive capability, longitudinal modelling was used to calculate individually specific random cognitive slopes across these ages [24] and reflects the estimated rate of change.
At age 65, the WLS incorporated a test of verbal working memory. Respondents were tasked with correctly recalling 10 words listed orally. Respondents were then distracted with other questions for ~12 min before again being asked to recall the list. In both cases, the number of words correctly recalled was recorded. The summation of these measures was used.
Socioeconomic indicators
Socioeconomic factors may be associated with both development and gender, and with health literacy. Parental socioeconomic status was measured directly from parents when respondents were 18 years old [25]. Education was measured at age 36 and indicates respondents’ highest level of education, grouped into high school, vocational or college-level qualifications. Individual income was measured in thousands of dollars at age 53.
Demographic indicators
Gender was included. Marital status and household size at age 53 were also examined under the hypothesis that dependents and partners may incentivize individuals to improve health literacy.
Analysis
Means, standard deviations and where appropriate percentages were provided to describe the sample. To examine sample selection, characteristics were separated into those who completed the NVS (n = 2,212), those who were not selected to complete the NVS (n = 3,940) and those who were lost to follow-up (n = 4,165). T-tests were used to compare between samples.
Structural equation modelling (SEM) is a tool commonly utilised to help elucidate pathways between covariates [26]. Generalised structural equation modelling (GSEM) is an application of generalised linear modelling that affords all of the capabilities of SEM, but further allows analysis of count data utilising non-linear assumptions necessary to model dichotomous data using a logistic link function or count data via Poisson regression [27]. To integrate individual rate of change in cognition into the GSEM model, we estimated individual slopes using longitudinal modelling. Longitudinal modelling applies multilevel modelling [24] to account for repeat-measurement biases and is commonly used to model trajectories of cognitive change [28]. Specifically, the following equation was used: , where Y is abstract reasoning, which differed between individuals (i) and was time variant (t), β0 indicated average capability, β1 indicated change over time, γ0i identified individual-level random intercepts and γ1it referenced individual-level random slopes. Marginal posterior expectations were estimated, divided by person-time and incorporated into GSEM models to indicate cognitive decline. Slopes were standardised to ease interpretation.
As is common in SEM analyses, results were reported graphically. Non-linear assumptions were highlighted on the graph using subtextual notation. Beta coefficients (B), standard errors (SE) and P-values (P) were provided. Because GSEM does not allow for many of the model comparisons normally used with SEM, model fit was assessed using adjusted pseudo-R2 [25]. Associated P-values were calculated using F-tests. To arrive at final models, significant associations among indicators with direct or indirect links to health literacy were displayed. To ensure no loss of generality, ΔPseudo-R2 was calculated comparing the full theoretical model to the model shown. Analyses were conducted using Stata 13.1/IC (StataCorp: www.stata.com).
Results
Descriptive analyses also revealed that 43.4% of respondents had low health literacy. The sample included mostly women. One in five respondents had a university degree (19.4%) and 41.9% had more than a high school degree.
Sample differences
Examining within-sample differences by type of follow-up (see Supplementary Table 1, available at Age and Ageing online) revealed that those who completed the NVS were similar to those who were not randomly selected to participate, but had marginally higher adolescent cognition (P = 0.048). On average, those who were surveyed in 2011 had significantly higher adolescent cognition, abstract reasoning, class rankings, education and income than those who were lost to follow-up.
Bivariate analyses
Bivariate analyses (Table 1) revealed that women and men differed in risk of low health literacy. There were baseline associations between health literacy and parental SES, adolescent cognition, non-cognitive skills, education and income.
Table 1.
Bivariate analyses linking main socioeconomic and adolescent differences with late-life health literacy, WLS 1957–2011
| High health literacy (56.6%) | Poor health literacy (43.4%) | P | |
|---|---|---|---|
| Education, N (%) | |||
| High school | 606 (47.2%) | 679 (52.8%) | <0.001 |
| Vocational schooling | 321 (64.6%) | 176 (35.4%) | |
| University degree | 325 (75.6%) | 105 (24.4%) | |
| Sex, N (%) | |||
| Male | 556 (52.6%) | 502 (47.5%) | <0.001 |
| Female | 696 (60.3%) | 458 (39.%) | |
| Adolescent cognition, mean (SD) | 0.48 (0.85) | −0.27 (0.94) | <0.001 |
| High school rank, mean (SD) | 0.42 (0.95) | −0.19 (0.93) | <0.001 |
| Parental socioeconomic status, mean (SD) | 0.18 (1.07) | −0.12 (0.97) | <0.001 |
| Individual income (/$1,000), mean (SD) | 37.51 (43.64) | 31.56 (36.60) | <0.001 |
| Verbal memory, mean (SD) | 10.82 (3.31) | 9.73 (3.75) | <0.001 |
| Abstract reasoning, mean (SD) | 6.92 (2.26) | 5.58 (2.35) | <0.001 |
| Reasoning slopes, mean (SD) | 0.007 (0.008) | 0.009 (0.008) | <0.001 |
| Total | 1,252 | 960 |
Multivariable analyses
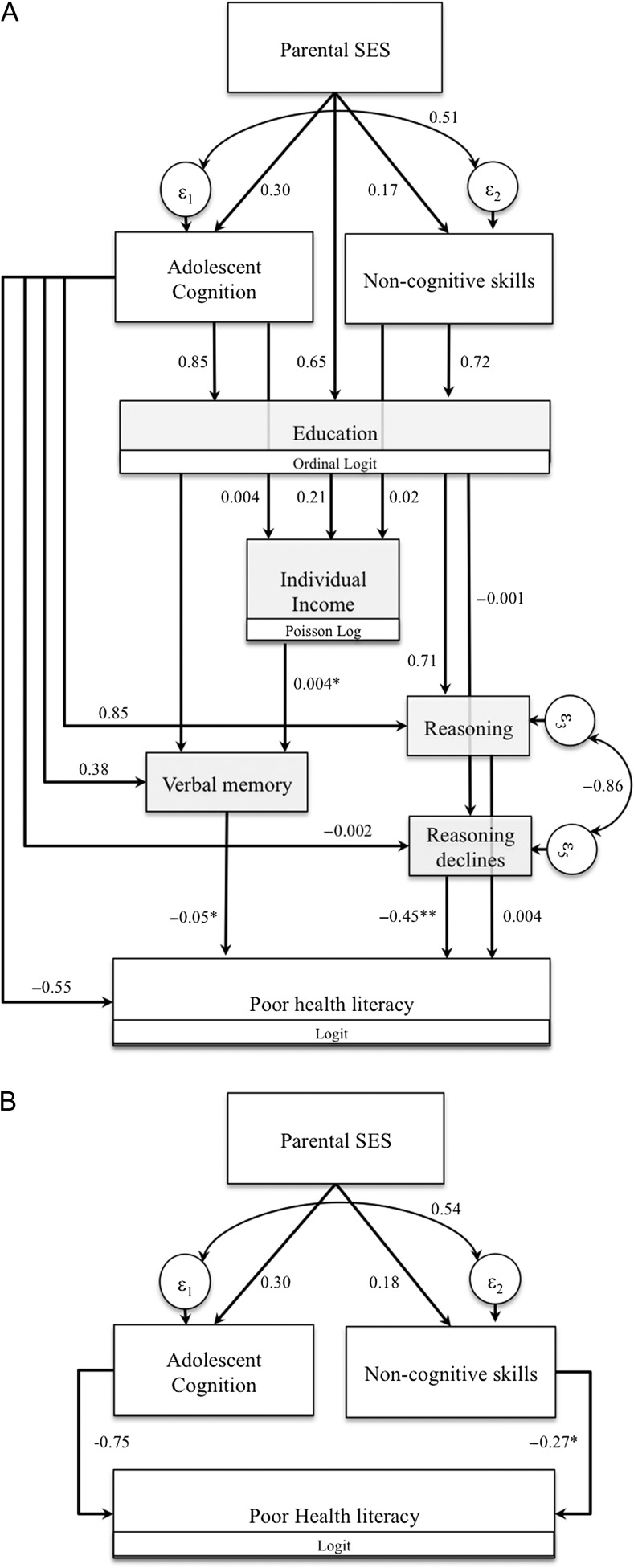
GSEM analyses revealed substantial gender differences in pathways to low health literacy, and thus only gender-stratified results were presented. Models fit well, with significant pseudo-R2 statistics exceeding 0.12. Models shown fit as well as the full theoretical model.
Results for men (Figure 2A) suggested that direct associations between parental SES, adolescent non-cognitive skills, higher education and individual income with poorer health literacy were completely explained by adolescent cognition and midlife cognitive factors including verbal memory, baseline abstract reasoning and declines in abstract reasoning. Direct associations between adolescent cognition and health literacy remained.
Figure 2.
Beta coefficients estimated using GSEM linking life course socioeconomic and cognitive predictors to health literacy. Only significant (α = 0.05) relationships with paths to health literacy are shown, WLS 1957–2011. (A) Males (Pseudo-R2 = 0.153, P < 0.001, ΔPseudo-R2 = 0.01, P = 0.135). (B) Females (Pseudo-R2 = 0.129, P < 0.001, ΔPseudo-R2 = 0.005, P = 0.608)
Note: Significance levels: *P < 0.05, **P < 0.01, all other associations shown have P < 0.001.
In contrast to men, women's poorer health literacy was predicted by adolescent traits (Figure 2B). Specifically, both adolescent cognition and non-cognitive skills retained both direct pathways while all other associations dissipated. As with men, associations between parental SES and poor health literacy were entirely mediated by adolescent characteristics.
Discussion
Using a cohort of Wisconsin graduates from the class of 1957 we examined life course factors associated with poor health literacy at age 72 years. Cognitive, non-cognitive, socioeconomic and demographic factors were measured from ages 18 to 72 years. The risk of low health literacy was high (43.4%) in this well-educated cohort. Women performed better than men on the health-literacy task: only two-fifths of women had poor health literacy, compared with half of men. Generalised structural equation models revealed that poor health literacy was associated predominantly with lower adolescent cognition and non-cognitive characteristics in both men and women. It was also associated with, among men, lower or declining midlife cognition, potentially indicative of impending cognitive impairment. To our knowledge, this is the first study to examine lifelong predictors of health literacy and to differentiate analysis by gender. Furthermore, it is the first to explicitly highlight the potentially high prevalence of low health literacy in a well-educated sample of older adults.
Gender effects
Supporting earlier research, this study found that women tended to have higher health literacy than men [29]. Notably, this study additionally found that risk factors for poor health literacy differed by sex. Reasons for such differences are unclear. The lack of association between income and health literacy may be because women were not main household earners, though analyses utilising household income were not supportive of this explanation. Educational attainment or educational returns may have been limited among women in this era. Prior work has noted that fewer women graduated from university, but suggests that educational returns to graduates were similar between men and women [30]. Additionally, the NVS asks respondents to read and interpret food labelling, a practice that may be more familiar to women due to traditional gender roles regarding healthcare and nutrition in this cohort [31]. Future research should consider men and women separately to ensure reliable results.
Health literacy is an important factor to consider in life course analysis. Healthy ageing begins early in life, and are influenced by experiences and exposures later in life [32]. In context, these findings regarding the role of adolescent cognitive and non-cognitive skills add to our understanding of how health literacy might change over time. Since many health decisions are made later in life, when disease management protocols may be complex and conflicting, understanding medical treatment programmes is integral to health self-management [7]. In this sense, the influence of cognitive decline on health literacy in men is particularly significant.
Measuring health literacy
The NVS is a standard measure of health literacy, assessing recognition and understanding of nutrition labelling and may be informed by prior experiences with dietary labelling while caring for the household. However, in an age of rapidly changing and easily accessible health information it is important to note that the particular NVS used here lacks domains of health literacy, for example understanding medication labelling or being able to understand and enact healthcare providers’ instructions. Future work should utilise different, or develop new, measures that are reliable among older respondents.
Limitations
The WLS is confined to information on high school graduates residing in Wisconsin in 1957, thereby limiting generalisability. Notably excluded from this study are individuals who did not graduate from high school and were thus most disadvantaged. Such exclusions may reduce the prevalence of poor health literacy and reduce the size of associations between socioeconomic factors that are strong determinants of prior mortality.
Insofar as gender roles may help explain some of these results, it is noteworthy that gender roles differ around the United States and have changed substantially since the 1950s. Additional research is needed to understand how gender roles are related to the development and application of health literacy skills.
Researchers using SEM often rely on the root mean square error of the approximation (RMSEA) to examine model fit, or modification indices to improve model structure. Using GSEM does not facilitate the calculation of these factors so they were not presented. Nevertheless, using linear assumptions to calculate RMSEA (=0.019) substantiated Psuedo-R2 statistics and revealed good model fit, while modification indices offered no substantive changes to models shown.
Clinical implications
Researchers increasingly critique use of instruments including the NVS in clinical practice [13, 33]. In the face of poor health literacy emerging from childhood, clinical integration of methods such as teach-back [34], accounting for differences in patient capabilities, may be an effective way of ensuring that patients understand and effectively manage their own health. However, despite being a relatively well-educated sample, nearly half of this late-life sample had poor health literacy that was associated with cognitive decline. Interventions noted above to improve health management might be more challenging among individuals with cognitive impairment or dementia. Given the high prevalence of cognitive impairment in samples over 70 years of age, older individuals identified as having low health literacy should also be screened for cognitive impairment.
Policy implications
Behavioural change is a mechanism at the head of a number of policies [1–3] that rely upon health belief models [4] and theories of planned behaviours [5]. Behaviourally focused interventions target processes of reflection, asking individuals to make better choices when providing them with better information, often with dissatisfying results [31]. In this study, men experiencing cognitive decline were experienced poorer health literacy, but men's and women's health literacy was also shaped by factors earlier in the life course. As such, improving health behaviours may require a holistic approach that engages children, adults, families and communities for improving health behaviours and chronic disease management over the life course.
Key points.
In this life course study, adolescent cognition, gender, adolescent non-cognitive skills, and rate of cognitive decline predicted late life health literacy.
Health literacy may be a result of cognitive decline, challenging its interpretation in old-age populations.
Low educated men were substantially worse off in health literacy later in life.
Future clinical and research efforts should differentiate health literacy from cognitive impairment.
Supplementary data
Conflicts of interest
None declared.
Funding
This manuscript was completed in part through funding provided by the National Institute on Aging (P01 AG043362) and by the UK Medical Research Council [MC_UU_12019/1, MC_UU_12019/4]. The funders played no role in the preparation of this manuscript, the analyses presented, the data collection or the decision to submit this manuscript for publication. A previous version of this manuscript was presented at the 2014 Health Literacy Annual Research Conference (HARC) in Washington, DC. Since 1991, the WLS has been principally supported by the US National Institute on Aging, with additional support from the Vilas Estate Trust, the National Science Foundation, the Spencer Foundation, and the Graduate School of the University of Wisconsin-Madison.
Supplementary Material
Acknowledgements
Data come from the Wisconsin Longitudinal Study (WLS). Detailed documentation and data are freely available: http://www.ssc.wisc.edu/wlsresearch/
References
- 1. US Department of Health and Human Services Healthy people 2020. In: US Department of Health and Human Services, editor. http://www.healthypeople.gov/2020/default.aspx: Washington, DC; 2011.
- 2. Pearson TA, Bazzarre TL, Daniels SR et al. American Heart Association guide for improving cardiovascular health at the community level a statement for public health practitioners, healthcare providers, and health policy makers from the American Heart Association Expert Panel on Population and Prevention Science Circulation. 2003;107:645–51. [DOI] [PubMed] [Google Scholar]
- 3. American Cancer Society Cancer Prevention & Early Detection Facts & Figures. Atlanta, GA: American Cancer Society, 2013. [Google Scholar]
- 4. Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun 2010; 25: 661–9. [DOI] [PubMed] [Google Scholar]
- 5. Ajzen I. Theory of planned behavior In: Van Lange PAM, Kruglanski AW, Higgins ET (eds.),. The Handbook of Theories of Social Psychology. Thousand Oaks, CA: SAGE Publications Inc., 2012: pp. 438–59. [Google Scholar]
- 6. Abel T, Frohlich KL. Capitals and capabilities: Linking structure and agency to reduce health inequalities. Soc Sci Med 2012; 74: 236–44. [DOI] [PubMed] [Google Scholar]
- 7. Richards M, Deary IJ. A life course approach to cognitive capability In: Kuh D, Cooper R, Hardy R, Richards M, Ben-Shlomo Y (eds.),. A Life Course Approach to Healthy Ageing. Oxford: Oxford University Press, 2014: pp. 32–45. [Google Scholar]
- 8. Kindig DA, Panzer AM, Nielsen-Bohlman L. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press, 2004. [PubMed] [Google Scholar]
- 9. Goodman MS, Gaskin DJ, Si X, Stafford JD, Lachance C, Kaphingst KA. Self-reported segregation experience throughout the life course and its association with adequate health literacy. Health Place 2012; 18: 1115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zamora H, Clingerman EM. Health literacy among older adults: a systematic literature review. J Gerontol Nurs 2011; 37: 41–51. [DOI] [PubMed] [Google Scholar]
- 11. Parker RM, Ratzan SC, Lurie N. Health literacy: a policy challenge for advancing high-quality health care. Health Aff 2003; 22: 147–53. [DOI] [PubMed] [Google Scholar]
- 12. Wister AV, Malloy-Weir LJ, Rootman I, Desjardins R. Lifelong educational practices and resources in enabling health literacy among older adults. J Aging Health 2010; 22: 827–54. [DOI] [PubMed] [Google Scholar]
- 13. Murray C, Johnson W, Wolf MS, Deary IJ. The association between cognitive ability across the lifespan and health literacy in old age: The Lothian Birth Cohort 1936. Intelligence 2011; 39: 178–87. [Google Scholar]
- 14. Serper M, Patzer RE, Curtis LM et al. Health literacy, cognitive ability, and functional health status among older adults Health Serv Res. 2014;49:1249–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kobayashi LC, Smith SG, O'Conor R et al.. The role of cognitive function in the relationship between age and health literacy: a cross-sectional analysis of older adults in Chicago, USA. BMJ Open. 2015;5:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kaphingst KA, Goodman MS, MacMillan WD, Carpenter CR, Griffey RT. Effect of cognitive dysfunction on the relationship between age and health literacy. Patient Educ Couns; 95: 218–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Richards M, Power C, Sacker A. Paths to literacy and numeracy problems: evidence from two British birth cohorts. J Epidemiol Commun Health 2009; 63: 239–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rhodes E, Devlin KN, Steinberg L, Giovannetti T. Grit in adolescence is protective of late-life cognition: non-cognitive factors and cognitive reserve. Aging Neuropsychol Cogn 2016: 1–12 (ePub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herd P, Carr D, Roan C. Cohort Profile: Wisconsin Longitudinal Study (WLS). Int J Epidemiol 2014; 43: 34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weiss BD, Mays MZ, Martz W et al. Quick assessment of literacy in primary care: the newest vital sign Ann Fam Med. 2005;3:514–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Heckman JJ, Stixrud J, Urzua S. The effects of cognitive and nooncognitive abilities on labor market outcomes and social behavior. J Labor Econ 2006; 24: 411–82. [Google Scholar]
- 22. Jacob BA. Where the boys aren't: non-cognitive skills, returns to school and the gender gap in higher education. Econ Educ Rev 2002; 21: 589–98. [Google Scholar]
- 23. Wechsler D. WAIS-R manual: Wechsler Adult Intelligence Scale-Revised. London, UK: Psychological Corporation, 1981. [Google Scholar]
- 24. Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. College Station, TX: STATA Press, 2008. [Google Scholar]
- 25. McFadden D. Conditional Logit Analysis of Qualitative Choice Behavior 1973. [Google Scholar]
- 26. Ullman JB, Bentler PM. Structural Equation Modeling. Hoboken, NJ: Wiley Online Library, 2003. [Google Scholar]
- 27. Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull 1995; 118: 392–404. [DOI] [PubMed] [Google Scholar]
- 28. Sliwinski MJ, Buschke H. Modeling intraindividual cognitive change in aging adults: Results from the Einstein aging studies. Aging Neuropsychol Cogn 2004; 11: 196–211. [Google Scholar]
- 29. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the ‘Newest Vital Sign’ ease of use and correlates. J Am Board Fam Med 2010; 23: 195–203. [DOI] [PubMed] [Google Scholar]
- 30. Clouston S, Kuh D, Herd P, Elliott J, Richards M, Hofer SM. Benefits of educational attainment on adult fluid cognition: International evidence from three birth cohorts. Int J Epidemiol 2012; 41: 1729–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: the importance of targeting automatic processes. Science 2012; 337: 1492–5. [DOI] [PubMed] [Google Scholar]
- 32. Kuh D, Cooper R, Hardy R, Richards M, Ben Shlomo Y. A Life Course Approach to Healthy Ageing. London: Oxford University Press, 2014. [Google Scholar]
- 33. Mottus R, Johnson W, Murray C, Wolf MS, Starr JM, Deary IJ. Towards understanding the links between health literacy and physical health. Health Psychol 2014; 33: 164–73. [DOI] [PubMed] [Google Scholar]
- 34. Kripalani S, Bengtzen R, Henderson LE, Jacobson TA. Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB: Ethics & Human Research 2008; 30: 13–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.