Abstract
Objective:
Explore and describe experiences and perceptions of falls, risk of falling, and fall-related consequences in individuals with incomplete spinal cord injury (SCI) who are still walking.
Design:
A qualitative interview study applying interpretive content analysis with an inductive approach.
Setting:
Specialized rehabilitation hospital.
Subjects:
A purposeful sample of 15 individuals (10 men), 23 to 78 years old, 2-34 years post injury with chronic incomplete traumatic SCI, and walking ⩾75% of time for mobility needs.
Methods:
Individual, semi-structured face-to-face interviews were recorded, condensed, and coded to find themes and subthemes.
Results:
One overarching theme was revealed: “Falling challenges identity and self-image as normal” which comprised two main themes “Walking with incomplete SCI involves minimizing fall risk and fall-related concerns without compromising identity as normal” and “Walking with incomplete SCI implies willingness to increase fall risk in order to maintain identity as normal”. Informants were aware of their increased fall risk and took precautions, but willingly exposed themselves to risky situations when important to self-identity. All informants expressed some conditional fall-related concerns, and a few experienced concerns limiting activity and participation.
Conclusion:
Ambulatory individuals with incomplete SCI considered falls to be a part of life. However, falls interfered with the informants’ identities and self-images as normal, healthy, and well-functioning. A few expressed dysfunctional concerns about falling, and interventions should target these.
Keywords: Self-identity, content analysis, accidental falls, incomplete spinal cord injury, fall risk awareness
Introduction
The proportion of individuals with spinal cord injury (SCI) who remain ambulatory, has risen significantly in the last decades as has the mean age.1 Limited walking performance implies increased risk of falling and subsequent injuries, and fall rates as well as injury rates are high in this group.2–4 From a safety perspective, this is a concern because of the vulnerability and the potential for further disability in this population.
Environmental hazards such as slippery walking conditions are known to accelerate fall-related psychological issues like fear of falling and fear avoidance beliefs in older adults.5 This may also apply to individuals with affected walking ability due to SCI, especially those with a fall-induced SCI, and may affect rehabilitation and participation in society. Research on falls in this group has further been actualized by the recent development of the Spinal Cord Injury Falls Concern Scale,6 which is the first scale to assess fall-related psychological issues in individuals with SCI.
Individual perceptions of falls, risk of falling, and fall-related consequences have been studied in older adults and in persons with multiple sclerosis,7,8 but there are currently no studies on this phenomenon in ambulatory individuals with chronic traumatic SCI. The group distinguishes itself significantly from the demography of other populations in that 80 percent are men, mean age is around 45 years1,9, and that it is characterized by intact cognitive functioning and to some extent by risk-taking behavior. Therefore, compared to older adults, they may have very unique and wide-ranging experiences and perceptions of falls that are important to fall-prevention programs. To gain a deeper understanding of the relationship between physical disabilities, walking, falls and fall risk in this group, a qualitative non-theory driven research approach seems appropriate.10–12 Therefore, the aim of this study was to explore and describe experiences and perceptions of falls, risk of falling and fall-related consequences among ambulatory individuals with traumatic SCI.
Methods
A qualitative interview study applying interpretive content analysis with an inductive approach10,13 was chosen to obtain a detailed description and understanding of how individuals with traumatic SCI experienced and perceived falls, risk of falling and fall-related consequences. A fall was defined as an unexpected event in which the participant comes to rest on the ground, floor, or lower level.14
Recruitment was performed face-to-face in connection with informants’ participation in regular SCI follow-up program at Sunnaas Rehabilitation Hospital. Inclusion criteria were ⩾ 18 years of age, chronic traumatic SCI (⩾ 1 year post-injury), walking ⩾ 75% of the time for mobility needs, fall experience during the previous year, and a good understanding of the Norwegian language. The sample was strategically selected to obtain wide variability in gender, age, number of years post-injury, level and extent of injury, rural/urban residence, and individual experiences of falling and risk of falling. Sample size was based on similar studies.
Participants gave their written informed consent to participate. The study was approved by the The Regional Ethics Committee for Medical Research Ethics in South East Norway (Dnr: 2012/531).
Data collection
Individual semi-structured interviews were chosen to generate rich data, and an interview guide with open-ended questions was developed by the authors in cooperation with the research group for the SCI Prevention of Falls (SCIP FALLS) Study. The main themes represented the aim of the study: experiences with falling, impact of falls, circumstances, contributing factors and consequences of falls as well as attitudes towards falls, fall prevention and risk of falling. Two pilot interviews were carried out to train the interview technique and test and adjust the interview guide. They were not included in the study.
The interviews were performed face-to-face by the first author, a physiotherapist with 25 years of experience in neurological rehabilitation working full-time as a researcher and without clinical connection to the informants at the time of the interviews. The long experience of working with individuals with SCI allowed the interviewer to meet with and respond to questions and concerns. This ensured the protection of the informants. All interviews were conducted between December 2013 and April 2014 with only the informant and the interviewer present. Eight interviews were performed at Sunnaas Rehabilitation Hospital, one was in another rehabilitation institution, and six were in the informants’ homes. The interviews lasted between 45 and 95 minutes. They were audio recorded and transcribed verbatim by the first author or an assistant.
Prior to the interviews, informants answered a background information questionnaire designed for the SCIP Falls Study17 containing fall history previous year (falls and fall-related injuries), a single-item question on fear of falling, risk taking behavior, ability to get up from the ground unaided and level of exercise and fitness training in the previous year.
Data analysis
The analysis was inspired by Baxter’s description of thematic interpretive content analysis where themes are threads of meaning emerging from the data. 10 The first author conducted the analysis in collaboration with the second author, an experienced researcher in qualitative research methods. The complementary clinical and research experience of the two authors was considered valuable for the data analysis. 18
The rigorous and systematic analysis process had the following steps: The interviews were read several times to obtain an impression of what was being reported, and two interviews were thoroughly read also by the second author. Guided by the study aim, the units of meaning were identified, condensed, and labeled with codes by the first author.13,19 Both authors coded four interviews individually and compared the results before deciding on the final coding frame. Data were displayed visually to identify connections and relationships within the data and to assist in data reduction by integrating categories into a smaller number of subthemes and mutually exclusive and exhaustive main themes (see Table 1). This was followed by an abstraction to seek out the overarching content of the text representing the thread of meaning recurring throughout the themes10. Findings and interpretations, including the authors’ own pre-understanding, were discussed repeatedly until consensus was achieved.
Table 1.
Two examples of the analytic process; at first meaning units were condensed; then coded and thereafter codes were sorted into subthemes.
| Meaning unit | Condensed meaning unit | Code | Subtheme |
|---|---|---|---|
| Clearly I’m concerned about falling … Very, because if you’re really unlucky and break a leg or break an arm or something like that, then obviously you are swept back half a year straight away. (man, 78) | Very concerned about breaking an arm or a leg when falling, physical function will be set back half a year | Afraid of consequences | Fall-related psychological issues |
| I could of course in my own house or something like that, but that’s because I try to be, live normally … Not that I seek out risk situations, I don’t feel I’m doing that … Yeah, trying to live normally at least (man, 23) | Could have sat down in a wheelchair or, isolated myself at home, but will try to live normally within safe limits | Live a normal life/self-identity as a normal and healthy person | Calculated risk taking |
Trustworthiness was assessed in terms of credibility, dependability, and transferability.19 The subthemes and themes are further validated by quotes throughout the results section12 and cited in terms of age and gender. They were translated by a professional interpreter with good knowledge of everyday Norwegian. Three independent researchers experienced in qualitative researched methods read the manuscript and provided valuable comments on the results of the analysis in relation to the aim of the study. This confirmed the results.
Results
A total of 16 individuals were invited to participate. One elderly individual declined due to poor health. Informant characteristics are shown in Table 2.
Table 2.
Informant characteristics.
| Gender | Age | Injury cause | Years post injury | Level and extent of injury (ISNCSCI)* | Walking-aid use in-/out-doors | Available orthopedic/technical walking aids | Falls previous year | Able to get up from ground unsupported | Exercise and fitness training level*** | “I like to take chances?” 15 | “Afraid of falling?” 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 23 | traffic | 7 | L2/AIS C | Yes/yes | AFO**/Crutches | 10 | Yes | Regular | No | Not at all |
| M | 25 | sport | 8 | T11/AIS C | No/yes | AFO**/Crutches | 7 | Yes | Moderate | Yes | Not at all |
| F | 26 | fall | 2 | L2/AIS C | Yes/yes | AFO**/Crutches, walker | 3 | No | Regular | No | Quite a bit |
| M | 29 | work-related | 7 | T12/AIS D | No/no | None | 100 | Yes | Regular | No | A little |
| F | 32 | traffic | 16 | C4/AIS D | No/no | None | 3 | Yes | Light | No | Quite a bit |
| M | 39 | traffic | 3 | C3/AIS D | No/no | Trekking poles | 6 | Yes | Moderate | No | Quite a bit |
| F | 43 | traffic | 18 | C6/AIS D | No/no | AFO** (Dictus)/ Crutches | 10 | No | Light | Yes | A little |
| M | 45 | traffic | 3 | L2/AIS D | Yes/yes | Crutches | 12 | No | Regular | Yes | A little |
| F | 49 | traffic | 30 | T10/AIS D | No/no | AFO** (Dictus)/ Trekking poles | 15 | Yes | Light | No | Quite a bit |
| M | 57 | sport | 5 | C5/AIS D | Yes/yes | AFO**/Crutches, walker | 24 | Yes | Regular | No | Not at all |
| F | 64 | fall | 6 | C6/AIS D | No/yes | Cane, trekking poles | 2 | Yes | Regular | No | A little |
| M | 64 | traffic | 2 | L2/AIS D | No/yes | Cane | 2 | Yes | Regular | No | A little |
| M | 68 | fall | 5 | C6/AIS D | No/yes | Crutches, walker | 1 | No | Moderate | Yes | A little |
| M | 69 | traffic | 34 | C5/AIS D | No/no | Trekking poles | 3 | Yes | Regular | Yes | Not at all |
| M | 78 | sport | 8 | C3/AIS D | No/no | None | 3 | No | Regular | No | Very much |
ISNCSCI = International Standard Neurological Classification of Spinal Cord Injury. ** AFO= ankle-foot orthosis. *** Regular= exercise and fitness training ⩾30 minutes 3 or more times/week; moderate=regular exercise and fitness training ⩾30 minutes 1-2 times/week; light=exercise ⩾ 2 hours/week, sitting still = exercise < 2hours/ week.
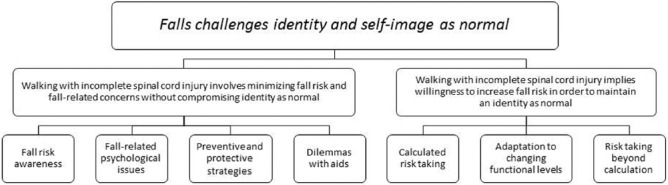
The analysis revealed one overarching theme comprising two main themes interpreting the informants’ experience of how falls, risk of falling, and fall-related consequences were influenced by their incomplete SCI. Seven subthemes constituted the two main themes (Figure 1).
Figure 1.
Overview of results showing that perceptions of falls and fall risk in ambulatory individuals with incomplete spinal cord injury could be expressed in one overarching theme, two main themes, and seven subthemes.
Overarching theme: Falling challenges identity and self-image as normal
The ability to walk was of prime importance to the informants despite the fact that it implied an increased risk of falling, fall-related concerns, embarrassment, and injuries. Falling was often perceived as a symbol of losing control of one’s self, and seemed to challenge the informants’ endeavor to maintain an identity as normal, healthy, and well-functioning in every respect. Despite this threat, they often described a willingness to operate at the limits of their functional ability and risked falling in activities that were important to maintaining their self-image as normal. The informants’ viewpoints appeared to be the same as the mountaineer’s: One should try to minimize risks but accept that there will always be a risk, which is justified by the goal. In this case, being a normal person with a somewhat impaired walking ability.
Main theme 1: Walking with incomplete SCI involves minimizing fall risk and fall-related concerns without compromising identity as normal
The first main theme comprised four subthemes:
Fall risk awareness
All informants described a plurality of fall risk situations. Risk factors included impaired body functions such as muscle weakness, spasticity, fatigue, and reduced sensitivity and environmental hazards such as door swills, carpets, stairs, hills, uneven ground, darkness, and moving in crowds. The winter climate, with its slippery walking conditions, was a particular worry.
Actually it dawned on me… that I’m not so fond of it (winter)… it’s slippery like hell, and that again means that you have to either walk very carefully or risk falling on your face all the time. (man, 26)
Some falls were perceived as “coming out of the blue”, but the informants reflecting on the fact that these often happened when they were not paying attention, i.e. in home environments, multi-task situations, or when in a hurry.
It’s precisely when feeling confident that now it’s safe and being a bit careless, and then it goes wrong. So it’s in those a bit sort of ridiculous situations that I fall then, and not the most risky ones. (man, 57)
Fall-related psychological issues
Fall-related psychological issues such as worries, fears, and feelings of shortcoming and embarrassment were experienced and discussed by the informants. A certain level of fall-related concern was perceived and used as a protective factor against harm. The informants were especially careful in dark places and when walking on slippery, uneven, or sloping surfaces.
… in those situations where you feel that here there’s a hazard of falling, then you’re likely to be so careful that it doesn’t happen… (man, 57)
One shared feeling was the embarrassment and dislike of attention caused by a fall. Adults simply do not fall in normal situations as one woman expressed. A few participants experienced an unpleasant loss of control and feelings of stigma, often linked to the belief that people perceived them as drunk due to their unsteady walking and subsequent fall.
… it’s (falling) embarrassing… They all stand there watching, and you look like an idiot, and a whole lot of them think I’m drunk, you know. (woman, 43)
A deterioration of physical function as a consequence of a fall was a major concern and closely linked to worries about losing independence and being a burden to others. As expressed by one man (78), “If you’re really unlucky and break a leg or break an arm or something like that, then obviously you are swept back half a year straight away.”
Not being able to protect vital body parts during a fall also seemed to increase concerns. One participant reported bodily reactions to the “taste of blood in my mouth” whenever she lost her balance. She attached this to a previous bad experience of falling on her face. Three informants had experienced huge difficulties getting up after a fall in harsh winter conditions. These events were frightening and, in fact, potentially life-threatening. Being unable to get up by oneself increased the informant’s concern and resulted in activity limitations and participation restrictions for some as expressed by one woman (26): “… I don’t go to places where there are no people.” Three women who had experienced falling when carrying or taking care of their child perceived these as frightening experiences and as threatening their role as a good and responsible parent.
Some informants expressed a severe fear of falling, and three related their fear directly to the fall causing their spinal cord injury, whether this was an actual fall or a fall related to a traffic accident.
… so it’s turned into a fear of losing control, because it was the fact that I lost control of the moped that made me fall over the steering wheel….. That’s the kind of things I’m left with, that deep fear. (woman, 32)
One informant even believed that “a fall will be the death of me” (woman, 64), arguing that if a fall when fit and sound could cause such a devastating injury, a fatal fall could certainly occur when the fall risk was even higher.
Preventive and protective strategies
Informants used numerous strategies to increase safety and prevent falls and injuries. Cognitive awareness seemed to be important. A great deal of thinking about how to resolve risky situations was necessary to compensate for impaired body functions.
…the head becomes a sort of control freak in relation to the body. Yeah, so there’s a lot of head traffic, just like to go out for a walk (in the winter). (woman, 32)
The typical immediate strategies were being careful in or avoiding risky situations, constantly screening the walking surface, using technical and/or orthopedic aids, avoiding alcohol, and slowing down.
Strategies were often a result of trial and error. After experiencing stumbling or falling, environmental hazards such as carpets were removed, handlebars were mounted, and walking aids that resulted in falls were abandoned. Some subjects received ideas from peers about how to deal with certain risk situations such as fall traps when using public transportation.
In the long term, strength and balance training was used as a preventive strategy. This applied in particular to informants who felt they had not reached their maximum level of functioning and activity, but also to informants attempting to prevent a decline as the years passed.
Yes, I’m more focused on improving my balance. I’m going to be strengthened when it comes to not falling. Well, that’s a goal in itself. (woman, 64)
Situations that were difficult to control, such as crowds or unpredictable movements of small children, were totally avoided by some informants while others discovered the safest way of acting, i.e., by waiting until everyone had left, holding onto someone, or sitting down when small children were around.
When falling, one important strategy was to protect vulnerable body parts, such as the head and arms, against injury. Several informants had developed falling techniques like bending the knees and hips to cushion the fall, landing on the shoulder, avoiding hand support, and rolling over.
… I try… to actually not put my hands in front of me, I try to protect my body, use my hands to protect my head, protect my belly, protect myself instead… (man, 29)
Dilemmas with aids
There seemed to be ambiguous feelings regarding the use of orthotics or walking aids. The informants had a range of feelings about aids in terms of their practicality and perceived safety in preventing falls as well as the symbolic value of aids in regard to stigma. A woman in need of walking aids showed ambiguous feelings:
… if I use crutches, then I know there’s a higher risk. And a walker, then I obviously know… if I fall, then at least I can lean (on) a walker and get up again… (woman, 26)
Some aids, although perceived as beneficial in preventing falls, were regarded difficult or impractical to use and thus neglected.
Main theme 2: Walking with incomplete SCI implies willingness to increase fall risk in order to maintain identity as normal
The second main theme comprised three subthemes.
Calculated risk taking
The risk of falling was, to some extent, dependent on what chance the informants were willing to take. In order to live their lives on their own terms, the majority took calculated risks within safe limits in the sense of balancing benefits versus risks. Thus, they were willing to pay the price of falling for a healthy self-image. Moving around without fall risk was perceived as impossible because the alternative was some degree of inactivity and dependence.
I could of course have sat down in a wheelchair or, isolated myself in my own house or something like that, but that’s because I try to be, live normally… Not that I seek out risk situations, I don’t feel I’m doing that… (man, 23)
Falls were therefore mostly considered a part of life, even within safe contexts.
Adaptation to changing functional levels
After an incomplete SCI, function increases over a period of a few years due to natural recovery and training. Many informants put a great deal of effort into training and strived to retain normal function. It seemed important for them to fight the image of being disabled as expressed by one informant, “…you feel simply a bit handicapped, and you don’t want to admit that”. (man, 39)
Several informants were predominately wheelchair users when they ended their hospitalized rehabilitation periods. Therefore, the process of improving gait, getting up after a fall, and steadily adapting to new functional levels was, to a large extent, achieved through their own trial and error in home environments.
Well, in the beginning I’d fall a lot, but over time I’ve created kind of a technique that makes me feel really safe. (man, 23)
The very nature of this striving was to push limits beyond safety limits when walking, which increased the risk of falling. One of the informants (man, 45) expressed this in the following way, “I have to go through falling to move on quite simply.” Likewise, informants who experienced a decline in physical functioning due to longstanding injury, increasing age, or overload problems were reluctant to give up activities exceeding their present capabilities. As a consequence, they experienced more fall risk situations because of reluctance to change to safer modes of walking.
Risk taking beyond calculation
One particular feature apparent through the interviews was that many informants had attempted walking in the countryside and skiing despite the high balance demands and increased risk of falling.
yeah, tried to go skiing. That was too much of a challenge,… I managed to go a little, but that didn’t go very well… I would like to try again…, but I don’t dare to go skiing alone. (man, 64)
Some informants were willing to take risks beyond the normal calculated ones. To achieve higher functional levels they exceeded both their own, peers’, and family members’ comfort zones.
“… I kind of have to challenge myself a little and… You don’t become a good skier without wiping out a few times. A lot of people would probably say that I’m a risk-taker… (man, 57)
Discussion
The main finding and overarching theme is, “Falls challenge identity and self-image as normal”. This comprised two main themes which interprets the informants’ contradictory view of falls. On one hand, enhanced risk of falling and falls were considered part of life, and the informants developed preventive strategies and justified concerns to protect their vulnerable bodies against falls and fall-related consequences. On the other hand, they were also willing to take risks to emphasize a normal identity.
In accordance with Watson,20 we found that the informants disliked or avoided looking upon themselves as disabled and fought to maintain established, normal identity and pre-injury activities and habits. A fall appeared to remind them of their motor-sensory shortcomings, which challenged several aspects of their individual and social identities (i.e., as a mother) and threatening some of their self-images (i.e., being physical fit). Negative attitudes towards people with physical disabilities, is still a prominent challenge. Watson argues that the image of a disabled individual as “weak and disempowered” is potent for disabled people who typically attempt to distance themselves from such a self-identity. For the informants, a fall - especially in everyday situations - seemed to aggravate and underpin the stigma of being disabled.
Fighting for a normal identity may suggest a high degree of self-efficacy and also resilience, which can protect against the negative impact of living with physical impairments and the uncertainty of outcome of an incomplete injury. This is supported by population-wide studies. 21, 22 The fight for a normal identity could also indicate a denial of disability or a fight against oneself as described by Angel et al. 23 For a few informants, self-image was exclusively linked to physical function, and thus, the acceptance of decreased functioning seemed impossible. This behavioral pattern is similar to persons with multiple sclerosis. 7
The ability to walk has a great symbolic value of being normal, 24 and a major goal of our informants was to regain or maintain walking despite the increased fall risk. This is similar to Angel et al. 25 The fact that a wheelchair has obvious advantages as an efficient and safe way of ambulating, and walking has the disadvantage of adverse outcomes in the long run for some, was given less significance. All informants were willing to take calculated fall risks to walk, and continue certain activities to maintain their self-image as normal. Walking in the countryside and cross-country skiing were common activities despite increased risk. Falling in the snow when skiing was regarded as safer than falling on hard surfaces and was also perceived as normal for able-bodied, thus posing less of a threat to self-image.
Risk is relative to individual interpretations. According to Slovic, 26 people base their judgments about how risky an activity is not only on what they think but also on how they feel about it. If the feeling is favorable, then the risk is judged as low and the benefits as high. Typically, informants dependent on walking aids often chose the aid with the least impact on their self-image, thus increasing fall-risk, i.e., using crutches instead of a walker, which was considered a device to be used solely by the elderly. Similar findings have been reported in individuals with multiple sclerosis and in the elderly. 7, 8
The informants developed numerous individual fall-prevention strategies. The most prominent strategy was the increased use of cognitive control through carefully planning activities that challenged their physical capabilities. Many falls were described as occurring when focus on walking was low or insufficient to control both the body and the environment at the same time or when unexpected situations emerged. This is in line with research showing dual task costs are related to falls in individuals with multiple sclerosis. 7, 27 Several informants mentioned strength and balance training as a fall-prevention strategy. This approach is supported by studies showing that muscle strength and balance are associated with falls in young adults with neurological conditions and correlate with walking level and performance. 28 Also, task-specific balance training can improve balance. 29
In accordance with studies in the elderly 30 and in individuals with neurological diseases, 31 many informants reported activity limitations and avoidance of activities especially related to walking on slippery surfaces in winter or activities with high demands on balance. Further research will show if avoidance behavior in this group impacts activities and participation as seen in the elderly. 5
In this study young men typically responded that they were not afraid of falling, while women and older informants mostly reported a somewhat higher fear of falling in line with research on the elderly. 5 As pointed out by Zijlstra et al., 32 some level of concern is a protective response to a realistic threat. This prevents people from undertaking activities with a high risk of falling and potential injury. Men have been shown to judge risks as being lower than women, and researchers have suggested that men underreport their fear due to perceived stigma. 26 This may be one explanation for the lower level of concern about falling as well as the higher risk willingness that is expressed by men versus women in this sample.
Having experienced injurious falls or not being able to get up after a fall, seemed to be mediators of developing fall-related concerns as reported in the elderly. 16 Good falling technique as a strategy to avoid injurious falls and reduce fear of falling could probably be taught—at least to younger individuals. Fall induced SCI may subsequently be reflected in concerns about falling as seen in this study. Several informants expressed excessive fear and catastrophic thoughts about falling related to the fall causing their SCI or other daunting falling experiences limiting activity and participation. According to Delbaere et al.,33 such excessive fear should be taken seriously and managed with cognitive behavioral interventions.
This study has some limitations. The questionnaire answered before the interview could have added to the informants pre-understanding of the subject matter. They may also have been influenced by the fact that the interviewer was a physiotherapist, whose role is to train and challenge gait and balance performance with the aim of enhancing physical function and decreasing fall risk.
Some factors may affect transferability. The informants covered a large age span with the majority being under the age of 65. Most fall research is in adults above this age, and little has been done in younger adult populations. We also lack knowledge about how able-bodied younger adults perceive falls and the consequences of falls. Moreover, 33% were women, which is a somewhat higher ratio than in the Norwegian traumatic spinal cord injured population (approximately 20%). 34 This may have led to an over-emphasis on certain aspects only mentioned by women. It is a limitation to the present study that all informants had experienced falling. Also, near fall events can influence perceptions of falls and risk of falling. A fairly high percentage compared to a study on a similar Norwegian population, 35 reported regular fitness training at least three times/week. This could have implications for the perception and the experiences of falls and the risk of falling.
One strength of the study is that the sample represents a wide variety in relation to age, injury, functional levels, and socio-demographic variables. In addition some of the findings in our study match the findings in a qualitative study of individuals with multiple sclerosis 7 and other quantitative studies, 2–4, 28 which support transferability. However, due to the diversity of this population and the somewhat limited study sample, there may be experiences and perceptions on falls and risk of falling not captured in this study.
In summary, perceptions of falls, fall risk and fall-related injuries in the context of ambulating individuals with SCI seems to be based on 1) minimizing fall risk and concerns, and 2) willingness to increase fall risks in order to maintain an identity as normal. On this basis the following clinical implications can be given:
Risk awareness and risk willingness should be addressed at follow-up taking into account the wide range of perceptions of falls.
Fall prevention programs must be wisely constructed to be perceived as relevant as individuals avoid viewing themselves as disabled despite their SCI
Falling technique and ability to get up after a fall should be practiced when necessary
Dysfunctional concerns about falling should be addressed in rehabilitation and follow-up.
Clinical message.
Perceptions of falls, fall risk and fall-related injuries, in the context of ambulating individuals with SCI, seems to be based both on minimizing fall risk and concerns, and on willingness to increase fall risk in order to maintain identity as normal.
Acknowledgments
We are grateful to all the participants in the study. Special thanks is given to the SCIP FALLs Study research group for discussions and valuable views, to Marika Augutis, Sundsvall Hospital, Sweden and to Gunnbjørg Aune and Grace Romsland, Sunnaas Rehabilitation Hospital, Norway for reviewing the manuscript and giving valuable comments.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants through the Department of Research, Sunnaas Rehabilitation Hospital, Norway.
References
- 1. Ahoniemi E, Alaranta H, Hokkinen EM, Valtonen K, Kautiainen H. Incidence of traumatic spinal cord injuries in Finland over a 30-year period. Spinal Cord. 2008;46:781–784. [DOI] [PubMed] [Google Scholar]
- 2. Brotherton SS, Krause JS, Nietert PJ. Falls in individuals with incomplete spinal cord injury. Spinal Cord. 2007;45:37–40. [DOI] [PubMed] [Google Scholar]
- 3. Saunders LL, DiPiro ND, Krause JS, Brotherton S, Kraft S. Risk of Fall-Related Injuries among Ambulatory Participants with Spinal Cord Injury. Topics in Spinal Cord Injury Rehabilitation. 2013;19:259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Phonthee S, Saengsuwan J, Siritaratiwat W, Amatachaya S. Incidence and factors associated with falls in independent ambulatory individuals with spinal cord injury: a 6-month prospective study. Phys Ther. 2013;93:1061–1072. [DOI] [PubMed] [Google Scholar]
- 5. Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33:368–373. [DOI] [PubMed] [Google Scholar]
- 6. Boswell-Ruys CL, Harvey LA, Delbaere K, Lord SR. A Falls Concern Scale for people with spinal cord injury (SCI-FCS). Spinal Cord. 2010;48:704–709. [DOI] [PubMed] [Google Scholar]
- 7. Nilsagård Y DE, Gunnarson L-G, Boström K. Factors perceived as being related to accidental falls by persons with multiple sclerosis. Disabil Rehabil. 2009;31:1301–1310. [DOI] [PubMed] [Google Scholar]
- 8. Bailey C, Jones D, Goodall D. What is the evidence of the experience of having a fall across the life course? A qualitative synthesis. Disability and Health Journal. 2014;7:273–284. [DOI] [PubMed] [Google Scholar]
- 9. Hagen EM, Eide GE, Rekand T, Gilhus NE, Gronning M. A 50-year follow-up of the incidence of traumatic spinal cord injuries in Western Norway. Spinal Cord. 2010;48:313–318. [DOI] [PubMed] [Google Scholar]
- 10. Baxter LA. Content analysis. In: Montgomery BM, Duck S. (eds). Studying Interpersonal Interaction. London: The Guilford Press, 1991, pp. 239–254. [Google Scholar]
- 11. Patton MQ. Qualitative Research & Evaluation Methods. 3rd ed. Thousand Oaks, CA: SAGE publications Inc, 2002. [Google Scholar]
- 12. Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative Content Analysis: A Focus on Trustworthiness. Sage Open. 2014;4:1–10. [Google Scholar]
- 13. Schreier M. Qualitative Content Analysis in Practice. London: SAGE, 2012. [Google Scholar]
- 14. Lamb SE, Jorstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network E, Outcomes Consensus G. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53: 1618–1622. [DOI] [PubMed] [Google Scholar]
- 15. Fuemmeler B, Taylor L, Metz A, Jr, Brown R. Risk-Taking and Smoking Tendency Among Primarily African American School Children: Moderating Influences of Peer Susceptibility. J Clin Psychol Med Settings. 2002;9:323–330. [Google Scholar]
- 16. Lach HW. Incidence and risk factors for developing fear of falling in older adults. Public Health Nurs. 2005;22:45–52. [DOI] [PubMed] [Google Scholar]
- 17. Jørgensen V, Butler Forslund E, Opheim A, Franzén E, Wahman K, Hultling C, et al. Factors Associated with Recurrent Falls in Individuals with Traumatic Spinal Cord Injury – a Multi-Center Study. Arch Phys Med Rehabil (accepted 24 April 2016). [DOI] [PubMed] [Google Scholar]
- 18. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. [DOI] [PubMed] [Google Scholar]
- 19. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. [DOI] [PubMed] [Google Scholar]
- 20. Watson N. Well, I Know this is Going to Sound Very Strange to You, but I Don’t See Myself as a Disabled Person: Identity and disability. Disability & Society. 2002;17:509–527. [Google Scholar]
- 21. Quale AJ, Schanke AK. Resilience in the face of coping with a severe physical injury: a study of trajectories of adjustment in a rehabilitation setting. Rehabil Psychol. 2010;55:12–22. [DOI] [PubMed] [Google Scholar]
- 22. Peter C, Muller R, Cieza A, Geyh S. Psychological resources in spinal cord injury: a systematic literature review. Spinal Cord. 2012;50:188–201. [DOI] [PubMed] [Google Scholar]
- 23. Angel S, Kirkevold M, Pedersen BD. Rehabilitation as a fight: A narrative case study of the first year after a spinal cord injury. International Journal of Qualitative Studies on Health and Well-being. 2009;4:28–38. [Google Scholar]
- 24. Gibson BE, Teachman G. Critical approaches in physical therapy research: investigating the symbolic value of walking. Physiother Theory Pract. 2012;28:474–84. [DOI] [PubMed] [Google Scholar]
- 25. Angel S, Kirkevold M, Pedersen BD. Getting on with life following a spinal cord injury: Regaining meaning through six phases. International Journal of Qualitative Studies on Health and Well-being. 2009;4:39–50. [Google Scholar]
- 26. Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as Analysis and Risk as Feelings: Some thoughts about Affect, Reason, Risk and Rationality. Risk Anal. 2004;24:311–322. [DOI] [PubMed] [Google Scholar]
- 27. Wajda DA, Motl RW, Sosnoff JJ. Dual task cost of walking is related to fall risk in persons with multiple sclerosis. J Neurol Sci. 2013;335:160–163. [DOI] [PubMed] [Google Scholar]
- 28. Saverino A, Moriarty A, Playford D. The risk of falling in young adults with neurological conditions: a systematic review. Disabil Rehabil. 2014;36:963–977. [DOI] [PubMed] [Google Scholar]
- 29. Tamburella F, Scivoletto G, Molinari M. Balance training improves static stability and gait in chronic incomplete spinal cord injury subjects: a pilot study. Eur J Phys Rehabil Med. 2013;49:353–364. [PubMed] [Google Scholar]
- 30. McInnes E, Seers K, Tutton L. Older people’s views in relation to risk of falling and need for intervention: a meta-ethnography. J Adv Nurs. 2011;67:2525–2536. [DOI] [PubMed] [Google Scholar]
- 31. Finlayson ML, Peterson EW. Falls, Aging, and Disability. Phys Med Rehabil Clin N Am. 2010;21:357–373. [DOI] [PubMed] [Google Scholar]
- 32. Zijlstra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley L, Kempen GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc. 2007;55:603–615. [DOI] [PubMed] [Google Scholar]
- 33. Delbaere K, Crombez G, van Haastregt JC, Vlaeyen JW. Falls and catastrophic thoughts about falls predict mobility restriction in community-dwelling older people: A structural equation modelling approach. Aging Ment Health. 2009;13:587–592. [DOI] [PubMed] [Google Scholar]
- 34. Hagen EM, Rekand T, Gilhus NE, Gronning M. Traumatic spinal cord injuries–incidence, mechanisms and course. Tidsskr Nor Laegeforen. 2012;132:831–837. [DOI] [PubMed] [Google Scholar]
- 35. Lannem AM, Sorensen M, Froslie KF, Hjeltnes N. Incomplete spinal cord injury, exercise and life satisfaction. Spinal Cord. 2009;47:295–300. [DOI] [PubMed] [Google Scholar]