Abstract
Background:
Funding models influence provision and development of palliative care services. As palliative care integrates into mainstream health care provision, opportunities to develop funding mechanisms arise. However, little has been reported on what funding models exist or how we can learn from them.
Aim:
To assess national models and methods for financing and reimbursing palliative care.
Design:
Initial literature scoping yielded limited evidence on the subject as national policy documents are difficult to identify, access and interpret. We undertook expert consultations to appraise national models of palliative care financing in England, Germany, Hungary, Republic of Ireland, New Zealand, The Netherlands, Norway, Poland, Spain, Sweden, Switzerland, the United States and Wales. These represent different levels of service development and a variety of funding mechanisms.
Results:
Funding mechanisms reflect country-specific context and local variations in care provision. Patterns emerging include the following:
Provider payment is rarely linked to population need and often perpetuates existing inequitable patterns in service provision.
Funding is frequently characterised as a mixed system of charitable, public and private payers.
The basis on which providers are paid for services rarely reflects individual care input or patient needs.
Conclusion:
Funding mechanisms need to be well understood and used with caution to ensure best practice and minimise perverse incentives. Before we can conduct cross-national comparisons of costs and impact of palliative care, we need to understand the funding and policy context for palliative care in each country of interest.
Keywords: Financing, reimbursement mechanisms, palliative care, hospice, health care systems
What is already known about the topic?
Financing models influence provision and development of palliative care services.
Comparisons of the regulation of palliative care in several European countries have been published.1
What this paper adds?
Models of palliative care and funding flows in a range of countries are described in a consistent and systematic way for the first time.
This study demonstrates that palliative care financing is often characterised by a mixed-payer system, that provider payment may perpetuate existing inequitable patterns in service provision and that reimbursement for services rarely reflects individual care input or patient needs.
It also shows that palliative care is not always integrated into health systems financing.
Implications for practice, theory or policy
Cross-national comparisons of costs and impact of palliative care depend on understanding national funding and policy context.
Reshaping funding models requires active involvement of palliative care leaders to ensure best practice and minimise perverse incentives.
Background
Provision of health and social care towards the end of life is a major resource burden, with estimates of spending in the last year of life ranging from 10% of all health care costs in The Netherlands2 and 13% in the United States of America (USA)3 to as high as 25% of Medicare hospice spending4 and 29% of English National Health Service hospital spending.5 Changing demographics, with an ageing population, longer chronic disease trajectories and greater co-morbidity, provide further incentives to improve quality and capacity of care for the dying. These factors create an urgent need to develop sustainable, widely accepted, patient-centred and cost-effective models for the funding and allocation of resources, while promoting high-quality palliative care across settings, and to deliver overall efficiency for the health and social care systems. Despite this, there is limited understanding of how much the actual costs of care provision relate to reimbursed costs, let alone how these costs compare with outcomes;6 this is true in palliative care as for other areas of care.
Palliative care funding arrangements should be understood in a wider system of health, social and informal care. Funding, availability and use of these health, social and informal sectors are each connected to palliative care provision. For example, the availability of grants to support informal carers may for instance reduce the need for hospital admissions. Similarly, the level and funding of general palliative care, which is provided by care professionals whose main focus is treating patients with life-limiting disease but who do not focus solely on palliative care,7,8 influences specialist palliative care.
However, in order to examine funding arrangements with sufficient detail to be useful, this article will focus on ‘specialist’ or ‘dedicated’ palliative care services. Variation in palliative care services exists not only in the type and content of services provided but also in the ways that palliative care services are funded. Differences in funding mechanisms may in fact drive differences in the type and content of services, as well as how many patients are served and when in their disease course. Within each country, funding models tend to change over time, offering opportunities for palliative care leaders to shape future funding mechanisms for palliative care.
This study therefore aims to review the international experience of funding for specialist palliative care services. Objectives are (1) to identify and appraise national models of palliative care financing and (2) to compare the identified funding models and draw critical lessons from international experience.
Methods
Initially, a literature review was conducted to elicit methods used internationally for commissioning specialist palliative care services for adults. However, the literature retrieved was not sufficient to draw a complete picture of service and funding arrangements, even after additional targeted literature searches. Relevant materials were difficult to identify as they were often only available in the language of origin. Access to resources proved difficult, as detailed policy documents are not always publicly available. Moreover, interpretation of these documents was highly dependent on a country-specific context, which is not always made explicit in most documents. We therefore undertook expert consultations, to gain an in-depth understanding of local arrangements for palliative care funding, and the context in which they operate.
Countries were selected to represent high-income countries (Europe, North America and Oceania), different levels of palliative care development and a diversity of funding models. A topic guide for the consultations was compiled to create a complete overview of the current state of palliative care provision, its funding mechanisms, (imminent or proposed) future changes and main challenges, based on Deber et al.9 framework for analysis of health service financing (see below) and Mason et al.10 international review of mental health services financing.
Country experts, defined as people with an active interest in palliative care policy and/or funding, were approached to participate in this work themselves or to propose other experts. Expert consultations were arranged to take place face-to-face or by telephone, and in one case by email correspondence. Detailed summaries based on the notes taken during the conversation were written by the interviewer (no audio recordings were made). These were then sent to the expert for review and correction. Where possible, consultation with an additional country expert was conducted to verify and supplement the information provided by the first expert (10 of 14 country experts were verified by a second expert). Preference was given to experts who did not know one another; however, given the small size of this field of interest, this was not always possible (5 of 10 countries had experts who had not worked together). Clarification and additional justification (literature) was sought when information provided by the experts was contradictory. If no consensus was found, this is described as such in the ‘Results’ section. All country experts were invited to comment on the manuscript and invited as co-authors.
Theoretical framework
In the absence of unequivocal scientific evidence in favour or against methods for payment of health care providers, consideration of the incentives and disincentives of different options provides more meaningful information. Deber et al.9 present a useful theoretical framework to aid categorisation of different funding options and to establish their relative benefits. It takes into account ‘the relationship between policy goals, health care organisation, and payment approaches’, to determine which mechanisms are most suitable given the context in which they are considered. The framework consists of three components: (A) Need, demand and utilisation, (B) Funding flows and (C) Basis of payment (details in Figure 1 and Table 1). We focus on component B (Funding flows), in particular the aspects ‘who pays?’ and ‘who allocates?’, and component C (Basis of payment) to gain a good understanding of palliative care financing.
Figure 1.
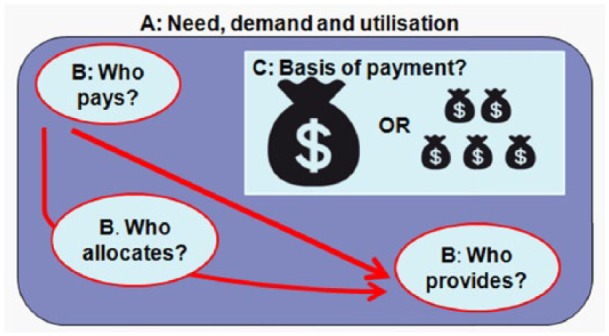
Streams of funding and reimbursement in health care.9
Table 1.
Elements of models of funding and reimbursement of health care.9
| A: The relationship among need, demand and utilisation and how this relates to the rationale for public involvement. This informs the context in which the palliative care services are provided. |
| B: The nature of funding flows and how this affects the policy levers, consisting of: |
| Financing – Who pays for services? |
| This could be individuals, public or private third-party payers (insurers), or mixed payment systems. |
| Delivery – Who provides the services? |
| Options include public sector, not-for-profit firms with paid workers, not-for-profit volunteers, for profit small business, for profit investor owned, or individuals and their families. |
| Allocation – Who allocates resources? |
| This is the link between financing and delivery and recognises variation in the incentives inherent in various arrangements (the framework distinguishes between organisational structures and bases for payment). |
| C: The potential basis for payment, on which resources can flow to those delivering care. Examples include block contracts, payment per bed day and per head (capitation). |
Results
A total of 14 countries were included in the review: Australia, England, Germany, Hungary, the Republic of Ireland, New Zealand, The Netherlands, Norway, Poland, Spain, Sweden, Switzerland, the USA, and Wales. Across these countries, palliative care and hospice services are provided that can be categorised by the setting of care: (1) specific palliative or hospice inpatient units, (2) hospital-based advisory services (inpatient or outpatient) and (3) community-based services in usual place of residence, inpatient hospice-based and community-based inpatient and outpatient and advisory services. However, there is much variation in organisation of these services between countries. Throughout this article, different countries are highlighted to illustrate strengths and shortcomings of funding arrangements and their consequences for service provision. Country-specific funding details were last updated in April 2015. Since this is a fast-changing area of work, it is possible that funding arrangements have changed since.
Need, demand and utilisation (A)
The relationship between need, demand, and utilisation informs the context in which palliative care services are provided. Mismatches between policy goals and palliative care funding mechanisms can leave needs unmet. We provide examples below of these mismatches, illustrating limitations in access to services from a range of issues, which are supported by policy goals but constrained by funding arrangements (Table 1).
Early access to palliative care services is an internationally recognised policy goal.11 In the United States, access to the hospice benefit is only available when life expectancy is less than 6 months, and when active treatment is discontinued,12 although there are current moves to change this. While palliative care may be available to patients who are in an earlier disease stage, this policy continues to limit the chances of considering palliative care treatment early and uptake of hospice benefit.
In Hungary, a single payment is received for each day on which the community-based palliative care team visits the patient, irrespective of the number or length of visits. Funding for each patient is limited to 150 visits over a longer period, but approximately 5% of patients require more than 150 days care. Charitable funding can usually cover these costs, but this is less secure, and leads to inequalities in service provision on the basis of illness duration and for those diagnoses with longer trajectories of illness.
In Hungary, non-cancer patients may account for up to 20% of all patients cared for in community-based and inpatient services, to receive statutory funding. If services want to provide to a larger proportion of non-cancer patients, cross-subsidisation by the provider is required. Although other types of services may be available to non-cancer patients, this arrangement principally means unequal access to care based on diagnosis. Similarly, in Poland, no reimbursement is received unless the illness is specified on a particular list.
Geographical variation in palliative care provision is a problem in many countries, as services are often more available in urban areas. In Wales, start-up funding has been made available to encourage service development in areas with high need. The absence of incentives for service provision in rural areas could be perceived as a shortcoming or missed opportunity in current funding arrangements, as this sustains inequity of access to services.
The nature of funding flows (B)
The nature of funding flows between financing, service delivery and allocation roles in a funding model impacts the delivery of palliative care services. Table 2 provides an overview of the national arrangements for collection of funding in each country, highlighting whether palliative care is part of the main funding system, whether a dedicated palliative care budget exists, and reliance on charitable funds and out-of-pocket payments (or co-payments).
Table 2.
Overview of funding collection for palliative care services.
| Country | Integration in predominant system for funding collection | Dedicated palliative care budget | Main allocation mechanism | Reliance on charitable funds (self-reported) | Out-of-pocket payments |
|---|---|---|---|---|---|
| Australia | − | + | Public third party | − | − |
| England | + | + | Public third party | + | − |
| Germany | + | − | Public and private third party | + | − |
| Hungary | + | + | Public third party, some through hospital budget | + | − |
| Ireland | + | + | Public third party, some through general health care budget | + | + (private insurance cover available) |
| New Zealand | + | + | Public third party, some through hospital budget | + | − |
| The Netherlands | + | + | Hospital: private third party, Hospice: private third parties | + | + (private insurance cover available) |
| Norway | + | + | Public third party | − | − |
| Poland | + | + | Public third party | + | − |
| Spain | + | + | Public third party | + | − |
| Sweden | + | + | Public third party | − | − |
| Switzerland | + | + | Public and private third parties | − | + |
| USA | + | + | Public and private third parties | + | + |
| Wales | + | + | Public third party | + | − |
Integration of palliative care funding in predominant system for revenue collection
In most countries, funding for palliative care services is financed through the same system as mainstream heath financing. However, mixed funding models exist in most countries, meaning that service providers depend on multiple resources.
Hospital-based services tend to have a higher proportion of their costs covered through the main funding framework (either public or private insurance), in comparison with community-based services providing specific palliative care outside the hospital. In some countries, this may be explained by the development of community-based palliative care services by the charitable sector. In some countries, the proportion of government contributions towards palliative or hospice inpatient units running costs is fixed (i.e. 70% in New Zealand), but in other countries statutory funding seems to be unequally distributed. In England (the United Kingdom), for instance, a 14-fold variation in palliative care spend per death was observed between primary care trusts across the country.13 Similarly, the percentage of total income from statutory funding ranges widely between different hospice inpatient units in the United Kingdom, from 20% to 50%, relying on charitable income such as donations or return on investments to cover remaining costs.14
Dedicated palliative care budget
Predictable funding streams help services adopt sustainable models of care and support service development with long-term perspectives. Anecdotally, in The Netherlands, the introduction of a new funding mechanism for palliative care for hospital-consult/advisory services in 2012, the introduction of academic hospital expert centres and criteria for palliative care consultation in oncology have provided increased visibility and stability for hospital palliative care,15 but continuous efforts are needed. The absence of ongoing dedicated financing from the main health care funder – often a government – leads to services relying on resources to be made available by other means.
Allocation mechanism
The mechanisms for allocating funds (usually a public or private third party) determine whether resources are readily available to services. Despite central regulation of palliative care services in Hungary, for example, outpatient palliative care services do not receive government funding. Services therefore rely on funding to be made available from the general hospital budgets, and facilities and equipment from the oncology wards, offering limited stability and sustainability in service provision. Similarly, payment of government funding in Spain is unpredictable and unreliable, making it necessary to turn to more stable charitable funding.
In Germany, resource allocation is locally negotiated between providers and insurance companies, which causes limited transparency and local variation in funding availability.
High reliance on charitable funds (self-reported)
In the majority of countries, strong charitable support of palliative care services is reported. The strong links with the charitable sector provide access to additional sources of funding. In Poland, services receive a payment per bed day (per diem) from the National Health Fund (NHF). Public and charitable organisations receive a similar amount of funding if their services are financed by the NHF, but the latter are able to top this funding up. This leads to variation in services available to patients, a so-called post-code lottery. Dependency on charitable funding may provide less stable funding flows in the current economic climate.
Considerable out-of-pocket payments
In Switzerland, The Netherlands, Ireland and the USA, patients are required to pay (part) of the service fees directly to the service provider, often referred to as ‘out of pocket’ payments or co-payments. Optional supplementary insurance is available to cover additional service costs in The Netherlands and Ireland, but comes at a higher insurance premium. Those who do not take out supplementary insurance pay additional costs out of pocket. Inappropriate out-of-pocket arrangements can limit access to and use of services. In Germany, patients were required to make out-of-pocket payment for their stay in hospice inpatient units of up to €90 per day, when statutory and insurance funding combined were insufficient. Social funding was available for people who were unable to afford this fee. However, this led to fear of opening up one’s financial administration and potentially involving family, causing fear and embarrassment. As a consequence, access to hospice inpatient units was reduced for some, often less advantaged, groups. This led to a policy response to ban the out-of-pocket payment and require statutory/insurance funding to cover 90% of hospice running costs. Hospice inpatient units must now raise 10% of expenses through charity.16 With new legislation for hospice and palliative care in Germany, this has now been reduced to 5%.
Transparency of funding flows
Funding flows impact quality, availability and access to services. Smaller services may be disadvantaged in navigating and negotiating funding. Moreover, variation in funding streams between different types of care and between different service providers complicate comparisons of ‘value for money’, restraining responsible service development.
The basis for payment (C)
Table 3 shows whether payment for palliative care services is integrated in each country’s main payment mechanism, as well as the basis for payment. In five countries included in this work, the basis of payment to providers is not organised in the same way as other types of care. A probable explanation lies in palliative care service development in the charitable sector, prolonging early public funding arrangements even when these have become the main source of revenue. Where payment for palliative care services follows the country’s main payment system, this is the result of newly arising opportunities for integration. In Germany and Australia, for example, integration in the main system has started with hospital-based palliative care and follows the main payment system for hospital care accordingly. Similarly, in Poland, payment for palliative care in outpatient settings follows the payment mechanism for long-term care. In The Netherlands, the split between payment mechanisms for acute care and long-term care is followed for hospital- and community-based palliative care services, respectively.
Table 3.
Basis for payment.
| Country | Integration in main payment mechanism | Non-activity-based payment | Activity-based payment |
|---|---|---|---|
| Australia | + (only for hospital-based inpatient services) | + | + |
| England | − | + | + (local initiatives only, national testing underway) |
| Germany | + (only for hospital-based inpatient services support teams) | + | + |
| Hungary | + | + | + |
| Ireland | − | + | − |
| New Zealand | − | + | − (testing unsatisfactory) |
| The Netherlands | + | + | + |
| Norway | + | + | + |
| Poland | + (in long-term care payment mechanism) | − | + |
| Spain | + | + | + |
| Sweden | + | + | + |
| Switzerland | − | − | + |
| USA | + | + | + |
| Wales | + | + | − |
The basis on which payments to providers of services are made can be categorised as non-activity-based and activity-based. In non-activity-based payment, the amount of resource received by the service provider does not increase when service provision increases. With activity-based payment, providers receive more funds when the level of service provision increases.
In most countries, a mix of activity-based and non-activity-based payment exists, although the split between them can be on different levels. In Spain, for example, hospital-based services receive activity-based funding (per diem), whereas community-based services receive non-activity-based funding (capitation). In Norway, 50% of revenue for hospital-based services is non-activity-based (block contract) and 50% is activity-based (per care episode). In Germany’s community-based services on the other hand, provider and insurer preferences determine whether payment is activity- or non-activity-based (e.g. per diem or block contract, with variation in length). Similarly, in the hospital setting, payment is activity-based, either per diem (20%) or episode based (80%) in line with preferences and negotiations.
Table 4 provides an overview of non-activity-based payment mechanisms. Non-activity-based funding does not increase along with provision, therefore largely shifting the financial risk of service provision to the provider, especially in situations of ageing population, longer chronic disease trajectories and greater co-morbidity, leading to increasing demand. In England, Germany, Ireland, New Zealand and Norway, block contracts are often used to pay for services. These are frequently based on historical allocation and lack a clear rationale, although sometimes adjustments are made for population and service characteristics. A more sophisticated site-specific budget exists in Australia, which is based on actual expenses and characteristics of service provision. Spain, Sweden and Wales employ capitation-based resource allocation, in which the level of funding depends on the size of the population covered, irrespective of actual service provision to that population. Failing to adjust for more resource-intense rural services can negatively affect care, as reported in Spain.
Table 4.
Non-activity-based payment mechanisms.
| Country | Basis for payment |
|---|---|
| Australia | Site-specific budget |
| England | Block contacts (historical) Spot purchasing |
| Germany | Block contacts |
| Hungary | Reallocation from general hospital budget/other departments |
| Ireland | Block contracts (historical; based on population served, services provided) |
| New Zealand | Block contracts (historical) Hospital-based: reallocation from general hospital budget |
| The Netherlands | Capitation (network care) and overall budgets for service regulation |
| Norway | Block contracts (based on population characteristics and area served) |
| Spain | Capitation (population in area, no urban/rural weighting) |
| Sweden | Site-specific budget or capitation |
| USA | Reallocation from general hospital budget |
| Wales | Capitation |
Activity-based funding increases with more service provision, which reduces the financial risk to the service provider in the context of increasing demand but increases the risk when demand diminishes. Table 5 provides an overview of the different activity-based payment mechanisms in place.
Table 5.
Activity-based payment mechanisms.
| Country | Unit of care | Variables used |
|---|---|---|
| Australia | Care episode | Patient-level: phase of illness, age, performance score Handling outliers: per diem outlier payments for very short/long stay patients, as well as service use and patient-level variables like intensive care unit use, indigeneity and radiotherapy use |
| England | Care episodea | Service-level: care settinga
Patient-level: phase of illness, functional status, problem severity |
| Germany | Per diem Care episode |
None Length of stay: 6 or less, 7–13, 14–20, 21 or more days of treatment17 |
| Hungary | Per diem | +10%–20% in rural areas Handling outliers: capped to 150 days of care |
| The Netherlands | Per diem (hospice-based) Care episode (hospital-based) |
Service-level: overnight stays, diagnostic assessment and treatment (outpatient care and number of contacts) |
| Norway | Care episode | Service-level: service characteristics |
| Poland | Per diem/per visit | +20% and 70% (enteral and parenteral nutrition) |
| Spain | Per diem | None |
| Sweden | Per diem | Service-level: referral mechanism |
| Switzerland | Per diem Care episodea |
None Patient-level: stability, symptoms, family burden/support issuesa Process-level: decision-making processes, organisational characteristics |
| USA | Per diem Per encounter or procedure (billing) |
None Complexity and setting |
Currently undergoing testing.
The most common example of activity-based funding in palliative care is a payment per bed day. Sometimes adjustment of the standard daily rate takes place, for example, for rural provision in Hungary, and for each referral mechanism in Sweden.
The level at which these payments and adjustments are set determines the effect it will have on financial viability and service provision. When payments are set below the average costs of service provision for their patient group, services do not break even. Services run a financial risk taking on patients – especially more complex patients – that require resource-intense treatment. Per diem or payments without adjustment for complexity or needing frequent or prolonged visits may cause problems. Service providers with a heavier caseload may be pushed to ‘cherry pick’ those who are less complex and easier to treat, although there is no evidence this happens, making it difficult for the severely ill to access services.
Another type of activity-based funding reimburses different rates based on a variable that predicts the level of resource use within a defined time period (per care episode or spell). This reduces the financial risk of overpayment to the funder, while reducing the risk of underpayment to the service provider, as the amount reimbursed more closely matches the expenditure. Outside palliative care, diagnosis may be a good predictor of resource use and therefore a suitable basis for payment in the form of diagnosis-related groups (DRGs). Within palliative care, however, diagnosis does not accurately predict the level of care input required and thus resource use.17
In The Netherlands, Germany and Norway, episode of care-based payment of hospital-based advisory services is therefore based on service characteristics and/or provision (length of treatment/hours of care provided). Patient characteristic-based payment has been explored in New Zealand and Australia. In New Zealand, the system was rejected out of fear of ‘cherry picking’ and overprovision of certain services (including bereavement care).
In Australia, on the other hand, a patient characteristic-based payment model has been successfully introduced in New South Wales and is being rolled out nationally. The amount of reimbursement received per patient varies by performance status, phase of illness, care setting and age. If variables are chosen correctly, these payment mechanisms draw appropriate levels of resource to address different levels of patient need.18 Similar patient-characteristic payment models are now proposed and explored in England and Switzerland.
Further specification of a payment model can be a top-up – with a non-palliative care DRG running alongside or replacement tariff. Supplementary regulations are required to care for ‘Outliers’, patients with very low or high resource intensity, and fairly share the financial risk. In Australia, this is handled with per diem payments for patients with very short or long stays, as well as service use and patient-level variables like intensive care unit use, indigenous background and radiotherapy use.
Along with increased availability of public funds, in recent years, public authorities have posed criteria and quality standards on palliative care service providers not only to be eligible for public funding but also to oncology departments to provide palliative care services. The availability of a specialised clinician is a common structural requirement, and comprehensive (multidisciplinary) assessment a common procedural requirement, both intended to push service development. In The Netherlands, it is obliged to have multiple medical specialties in the multidisciplinary team and more teams build relationships with community care. We have not come across outcome indicators as requirements for funding. In Sweden, some services have lost government support after failing to meet audit criteria.
Discussion
We have applied a model for funding and reimbursement of health care services on palliative care funding models and described the diverse models and funding flows in a consistent and systematic way for the first time. This shows a wide variation in funding mechanisms for hospital and community-based palliative care services, reflecting both national differences in financial context and care provision, as well as some common themes. First, funding is rarely linked to population need and often perpetuates existing – inequitable – patterns in service provision. Second, palliative care funding is frequently characterised as a mixed system of charitable, public and private payers. Theoretically, multiple sources of funding lead to increased funding; in practice, however, it can cause responsibilities to be unclear, administrative complexities, and unclear sustainability. Third, the basis on which providers are paid for services is rarely based on care input and individual patient-level needs. This is recognised in the gradual move from non-activity-based funding (e.g. block contracts) to activity-based reimbursement (e.g. per diems, procedure-based DRGs). Activity-based payment can be further refined in casemix based models through which the level of payment is adjusted for individual patient-level need, which requires further research into accurate predictors of care use.
The variability in funding mechanisms has two major implications for health economics research on palliative care across countries. First is that the ability to conduct large-scale health economics research on palliative care is dependent on having a clear signal of palliative care provision in the administrative data generated, and the strength of the data signal is driven by the funding model. In the United States, for example, there is a very clear data signal for Hospice, because it is a distinct insurance benefit, but no or weak signal for specialist palliative care outside of Hospice, because the patients, activities and providers are not distinctly called out as specialist palliative care. The nature of the data signal will also vary by specific funding mechanism. Countries that base palliative care funding on patient needs and complexity may generate data on patients with different levels of complexity or need, which could be useful in economics-focused research. Countries that use activity-based funding may generate data on the frequency, intensity and duration of palliative care services that could also be very useful in such research. Researchers seeking to conduct international or multi-national research on the use, timing and impact of palliative care must first understand what data will be available regarding palliative care patients and palliative care services.
The second implication of this study is in regard to the interpretation of economics research from one country to another. Knowing what entity (patient, hospital, service area, private insurer or public insurer) is at financial risk for over-utilisation of costly services at the end of life (e.g. hospital admissions) is crucial for understanding how the research on economics of palliative care (e.g. cost reduction; avoidance of hospitalisations) would incentivise the investment and provision of palliative care in hospitals and community settings. This analysis has been done for the USA,19 but to our knowledge has not yet applied to other countries. Similarly one country may shift costs from private insurance or government payers to the patients and families more or less than another; it is therefore critical to know the extent to which that is happening and whether researchers are measuring patients’ out-of-pocket costs in the countries where palliative care financial impact is being studied.
This work has provided some clarity as to how and where funding mechanisms might act as policy levers. Table 6 summarises how funding arrangements can be applied to support the development of acceptable and effective palliative care through listing desirable features of a palliative care funding model. Funding models must be used to reward excellence, while minimising ‘perverse’ incentives. Through engagement in reshaping funding and reimbursement mechanisms, patient care can be improved, high-quality care rewarded and equity ensured. To improve a local palliative care funding model, it is important to understand the context in which it operates. The international financial crisis has posed economic pressure on health systems internationally, with governments taking steps to increase out-of-pocket payments, decrease care coverage and cut expenditures.20,21 The solutions to some of the cost crises in health care lie with systematic understanding of costs and funding flows and better awareness of the relationship between outcomes and costs.6 At the same time, investments in palliative and end-of-life care are being suggested as areas of opportunity to increase health systems’ value for money.22 This opens a window of opportunity to attract funding and shape funding systems to produce better care outcomes. However, detailed understanding of the costs and outcomes of different palliative care models, the relation with non-palliative care interventions and their interactions is required to foresee the effects of new structural and financial arrangements. Here, clinical teams and palliative care providers share the responsibility in leading improvements and reducing variation in care by defining good practice and measuring their activity, costs and outcomes.22,23 Through active involvement in funding reform, we can stimulate the development of palliative care.
Table 6.
Desirable features of a funding model for palliative care.
| Desirable features of a funding model for palliative care should be to aid acceptable and effective delivery to those that need it including: |
| • Support for the goal of getting appropriately early access to palliative care (not just at the end of life) |
| • Support for an appropriate mix of services with palliative and curative intent |
| • Support for services in the most appropriate location |
| • Avoiding financial hardship to service users and families |
| • Providing stable and predictable funding that allows services to be planned and developed in a coherent way |
| • Support services with clear entitlements, and that are easy to understand and navigate, and which avoid unnecessary administration and transaction costs |
Acknowledgments
The authors would like to thank the following people for supplying country-specific details in the early stages of this study: Veronica Snow and Anthony Byrne (Wales), W Jansen (The Netherlands), P Calvo Pérez (Spain), G Eckerdal (Sweden), K Parrott and J Richter (Australia), S Booiman and J Lyon (New Zealand), A Cialkowska-Rysz, B Kozlowska and B Łyszczarz (Poland).
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This article presents independent research funded by the National Institute for Health Research (NIHR) in the United Kingdom, under the Programme Grants for Applied Research scheme (RP-PG-1210-12015). It is also partly funded by the NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC) Funding scheme, through CLAHRC South London. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research or the Department of Health. CLAHRC South London is part of the NIHR and is a partnership between King’s Health Partners, St. George’s, University London, and St George’s Healthcare NHS Trust.
References
- 1. Beek KV, Woitha K, Ahmed N, et al. Comparison of legislation, regulations and national health strategies for palliative care in seven European countries (Results from the Europall research group): a descriptive study. BMC Health Serv Res 2013; 13(1): 275, http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-13-275 (accessed 22 October 2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Polder JJ, Barendregt JJ, van Oers H. Health care costs in the last year of life – the Dutch experience. Soc Sci Med 2006; 63(7): 1720–1731. [DOI] [PubMed] [Google Scholar]
- 3. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care. Am J Public Health 2015; 105(12): 2411–2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Riley GF, Lubitz JD. Long-term trends in medicare payments in the last year of life. Health Serv Res 2010; 45(2): 565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barnato AE. End-of-life spending: can we rationalise costs? Crit Q 2007; 49(3): 84–92. [Google Scholar]
- 6. Kaplan R, Porter M. How to solve the cost crisis in health care. Harv Bus Rev 2011; 89(9): 46–52. [PubMed] [Google Scholar]
- 7. European Association for Palliative Care. White Paper on standards and norms for hospice and palliative care in Europe: part 1. Eur J Palliat Care 2009; 16(6): 278–289. [Google Scholar]
- 8. European Association for Palliative Care. White Paper on standards and norms for hospice and palliative care in Europe: part 2. Eur J Palliat Care 2010; 17(1): 22–33. [Google Scholar]
- 9. Deber R, Hollander MJ, Jacobs P. Models of funding and reimbursement in health care: a conceptual framework. Can Public Adm 2008; 51(3): 381–405. [Google Scholar]
- 10. Mason A, Goddard M, Myers L, et al. How international experience can inform the funding of mental health care in England. J Ment Health 2011; 20(3): 234–248. [DOI] [PubMed] [Google Scholar]
- 11. Connor SR, Bermedo MCS. Global atlas of palliative care at the end of life (Worldwide palliative care alliance, World Health Organization), 2014, http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- 12. Centers for Medicare & Medicaid services. Medicare hospice benefits, 2016, https://www.medicare.gov/Pubs/pdf/02154.pdf
- 13. Hughes-Hallett T, Craft A, Davies C, et al. Funding the right care and support for everyone: creating a fair and transparent funding system. The final report of the Palliative Care Funding Review London, The Palliative Care Funding Review, London, July 2011, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/215107/dh_133105.pdf [DOI] [PubMed]
- 14. Hospice UK. Hospice accounts 2014. London: Hospice UK, 2014. [Google Scholar]
- 15. Brinkman-Stoppelenburg A, Boddaert M, Douma J, et al. Palliative care in Dutch hospitals: a rapid increase in the number of expert teams, a limited number of referrals. BMC Health Serv Res 2016; 16(1), http://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-016-1770-2 (accessed 22 October 2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoffmann C, van Ginneken E, Busse R. Better funding model for inpatient hospice units. Health Policy Monitor, 2016, http://www.hpm.org/en/Surveys/TU_Berlin_-_D/14/Better_funding_model_for_Inpatient_Hospice_Units.html [Google Scholar]
- 17. Lee LA, Eagar KM, Smith MC. Subacute and non-acute casemix in Australia. Med J Australia 1998; 169: S22–S25. [DOI] [PubMed] [Google Scholar]
- 18. Eagar K, Gordon R, Green J, et al. An Australian casemix classification for palliative care: lessons and policy implications of a national study. Palliat Med 2004; 18(3): 227–233. [DOI] [PubMed] [Google Scholar]
- 19. Cassel JB, Kerr KM, Kalman NS, et al. The business case for palliative care: translating research into program development in the U.S. J Pain Symptom Manage 2015; 50(6): 741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Giovanella L, Stegmüller K. The financial crisis and health care systems in Europe: universal care under threat? Trends in health sector reforms in Germany, the United Kingdom, and Spain. Cad Saúde Pública 2014; 30(11): 2263–2281. [DOI] [PubMed] [Google Scholar]
- 21. The King’s Fund. The budget: health and social care funding, 2015, http://www.kingsfund.org.uk/publications/articles/briefing-budget-july-2015 (accessed 26 March 2016).
- 22. Alderwick H. Better value in the NHS: the role of changes in clinical practice. London: King’s Fund, 2015. [Google Scholar]
- 23. Schenker Y, Arnold R. The next era of palliative care. JAMA 2015; 314(15): 1565. [DOI] [PMC free article] [PubMed] [Google Scholar]


