Abstract
Primary Sjögren syndrome (pSS) is a chronic systemic autoimmune disease characterized by xerophthalmia, xerostomia, and potential peripheral or central neurological involvement. In pSS, the prevalence of cognitive disorders is generally sparse across literature and the impact of pain on cognitive profile is unclear. The aim of this study was to determine the relation between pain, cognitive complaint, and impairment in a very homogenous population of 10 pSS patients with painful small fiber neuropathy (PSFN) and spontaneous cognitive complaint. Neurological exam, neuropsychological assessment, clinical evaluation measuring pain level, fatigue, anxiety, depression, and cognitive complaint were performed. Our results showed that 100% of patients had cognitive dysfunction especially in executive domain (80%). The most sensitive test was the Wisconsin Card Sorting Test (WCST), abnormal in 70% of our population. Moreover, we found clear cut significant correlations between pain levels and 3 measures of WCST: the number of errors (R = –0.768, P = .0062), perseverations (R = 0.831, P = .0042), and categories (R = 0.705, P = .02). In the literature review, the impact of pain is underexplored and results could be discordant. In a homogeneous cohort of pSS patients with PSFN, a cognitive complaint seems to be a valid reflection of cognitive dysfunction marked by a specific executive profile found with the WCST. In this preliminary study, this profile is linked to the level of pain and highlights that an appropriate management of pain control and a cognitive readaptation in patients could improve the quality of life.
Keywords: cognition, cognitive impairment, executive functions, neuropathy, pain, Sjögren syndrome, small fiber neuropathy
1. Introduction
Primary Sjögren syndrome (pSS) is a chronic systemic autoimmune disease characterized by glandular involvement as xerophthalmia, xerostomia, cutaneous xerosis, and potential extra-glandular manifestations. Among them, the neurological involvement is one of the most frequent occurring in around 20% of cases.[1–3] The peripheral neurological involvement is well characterized and includes 3 groups of neuropathies: ataxic, sensorimotor, or painful. One of the most frequent pSS-peripheral neuropathy is the painful small fiber neuropathy (PSFN) that might concern up to 10% of pSS patients.[4] Regarding cognition, the prevalence of impairment is not uniform and varies across studies from 11% to 100%.[5–17] This finding could be due to a heterogeneous population recruitment. Usually, pSS patients report abnormal concentration abilities relating difficulties to follow a conversation, to find the proper words, to finish what they are doing or to forget what they are looking for.[18] The observed cognitive profile is characteristic of a fronto-subcortical alteration with memory, attention, and executive disorders.[7,9,16,17,19] Similar cognitive deficits can be observed in chronic pain[20,21]; however, little is known about the potential synergic impact of pain associated with pSS.
Previous works have studied heterogeneous groups of patients either with pSS and/or pain. Our objective was first to determine the relation between pain level, cognitive complaints, and impairment in a homogenous cohort of pSS with PSFN, and second to carry out an exhaustive review of cognitive dysfunction in PSS.
2. Methods
The key element of the study design is the inclusion of a very homogenous group of PSFN with cognitive complaint in order to evaluate their cognitive performances.
2.1. Study subjects
We previously set up a study assessing the prevalence and the features of pSS-associated PSFN.[4] This study was approved by the Ile de France VI (Pitié-Salpétrière University Hospital) Ethical committee on March 25, 2009, and each patient gave a written informed consent prior to investigation. In this study, clinical data including neurological exams and cognitive measures were prospectively recorded. For the current study, we performed extensive and specific investigations in a homogenous group of patients with a PSFN reporting cognitive complaint. Between October 2012 and January 2014, 12 patients fulfilling 2002-American-European Criteria Group for pSS and followed in the Department of Internal Medicine of Lariboisiere Hospital were included. The inclusion criteria were: (1) the presence of spontaneous cognitive complaint, (2) the presence of definite PSFN with at least 2 of the 3 PSFN criteria: (i) clinical signs and symptoms of small fiber impairment, with distribution consistent with peripheral neuropathy (length or nonlength dependent neuropathy); (ii) alteration of small fiber neurophysiological investigation (laser evoked potentials; quantitative sensory testing; sympathetic skin reflex recording); (iii) reduced intraepidermal nerve fiber density by skin biopsy.[22] All patients with other neurological disorders or psychiatric diseases according to usual criteria were excluded.[23]
2.2. Assessment procedure
To investigate how pain might impact cognitive functions in pSS, we performed neuropsychometric battery, health clinical questionnaires, and neurological examination in all eligible patients.
2.3. Clinical evaluation
Taking account the cognitive complaints, all patients had a neurological examination at the Cognitive Neurology Center of Saint-Louis Lariboisière Fernand-Widal Hospital to evaluate neurological symptoms, to exclude other neurological diseases and to record all potential other causes of cognitive complaint and impairment. The day of the cognitive assessment, health clinical questionnaires were administrated to evaluate pain, fatigue, depression, anxiety, and cognitive symptoms. Levels of pain and fatigue were measured by visual analog scales (VAS) scoring from 0 to 10 (0: no pain/fatigue, 10: extreme pain/fatigue). Next, other measures were recorded with 2 auto-questionnaires: 1/ Hospital Anxiety and Depression Scale (HADS) to evaluate levels of anxiety and depression (a score equal to or above 11 was considered as significant scores of depression or anxiety),[24] 2/Mac Nair autoquestionnaire to estimate the intensity of cognitive complaint (a cut off score above 15 is reflecting a high cognitive complaint).[25] Brain and spinal cord MRI were performed in all included patients.
2.4. Neuropsychological evaluation
One month after the neurological examination, all patients were administered a complete neuropsychometric battery lasting approximately 2 hours. Each following cognitive domain was evaluated: 1/ global functioning: Mini Mental State Examination (MMSE),[26] 2/ memory: Free and Cued Selective Reminded Test (FCSRT),[27] 10/36 test,[28] and recall of Rey Osterrieth Complex Figure (ROCF),[29] 3/ attention/concentration: d2 test,[30] Trail Making Test (TMT) part A,[31] digit span,[32] spatial span,[33] Stroop Test denomination and reading part,[31] 4/ speed processing: Symbol digit modalities test (SDMT),[34] 5/ executive functions/working memory: Letter-Number sequencing,[33] phonemic fluency,[35] TMT part B,[31] Stroop test interference part,[31] Similarities,[32] and Wisconsin Card Sorting Test (WCST),[31] 6/ instrumental functions: DO-80,[36] categorical fluency,[35] Mahieux battery,[37] ROCF[29] and 3 subtests of Visual Object and Spatial Perception (VOSP)[38] such as Screening, Silhouettes, Number Location. All scores were statistically processed in z-scores to classify each neuropsychological performance using demographically corrected norms for each test (with regards to age and educational level). We defined a cognitive disorder when a subject obtained a score below −1.65 SD from average norms based on current French practice.[39]
2.5. Statistical analysis
The percentages of pathological results in all explored cognitive domains were calculated. We then analyzed the correlation between VAS pain and the various cognitive tests using non-parametric Spearman's rank correlations. P-values were 2-tailed and values ≤0.05 were considered as statistically significant. Analyses were performed using SAS 9.2 (SAS Institute, Cary, NC).
2.6. Literature review
We searched the National Library of Medicine's MEDLINE database (Bethesda, MD) for relevant literature using the keywords “Sjögren,” “Gougerot,” “Gougerot Sjögren,” “cognition,” “cognitive dysfunction,” “cognitive impairment,” and “cognitive decline.” We have selected papers in which neuropsychological evaluation was performed. The bibliographies of all selected articles were reviewed. Together, at our knowledge, 20 articles published between 1985 and 2016 in the international literature were included in this review.
3. Results
3.1. Description of the study group
A total of 12 patients were consecutively included. Two patients were excluded because of pre-existing dementia due to other pathologia. All 10 included patients fulfilled the 2002-AECG criteria for PSS. Thus, all patients with negative anti-SSA and SSB antibodies (7 patients out of 10) had a positive lip biopsy with a focus score ≥1.
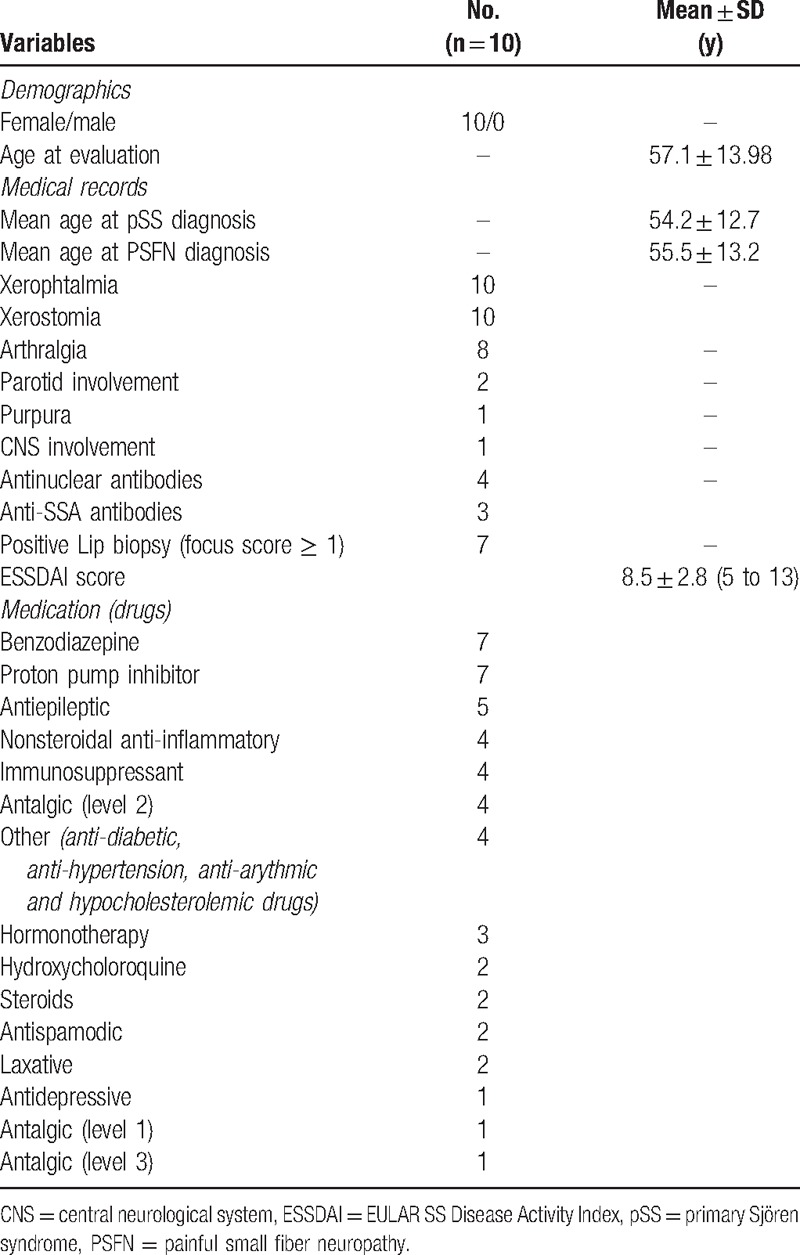
All medical demographic data are summarized in Table 1. Regarding health clinical questionnaires, 87.5% had a significant cognitive complaint on the McNair scale, the mean duration of complaint was 21.5 ± 17 months. Respectively, 30% and 20% of patients had significant scores of anxiety (mean: 8.80 ± 6.01) and depression (mean: 6.20 ± 4.31) on HADS. Mean pain quotation was 3.08 ± 2.23 and fatigue 3.96 ± 2.49. All patients were treated by 1 or several treatments that could impact cognition.[40,41] No significant abnormalities were found on brain and spinal cord MRI.
Table 1.
Medical demographics data.
3.2. Neuropsychological profiles (descriptive analysis)
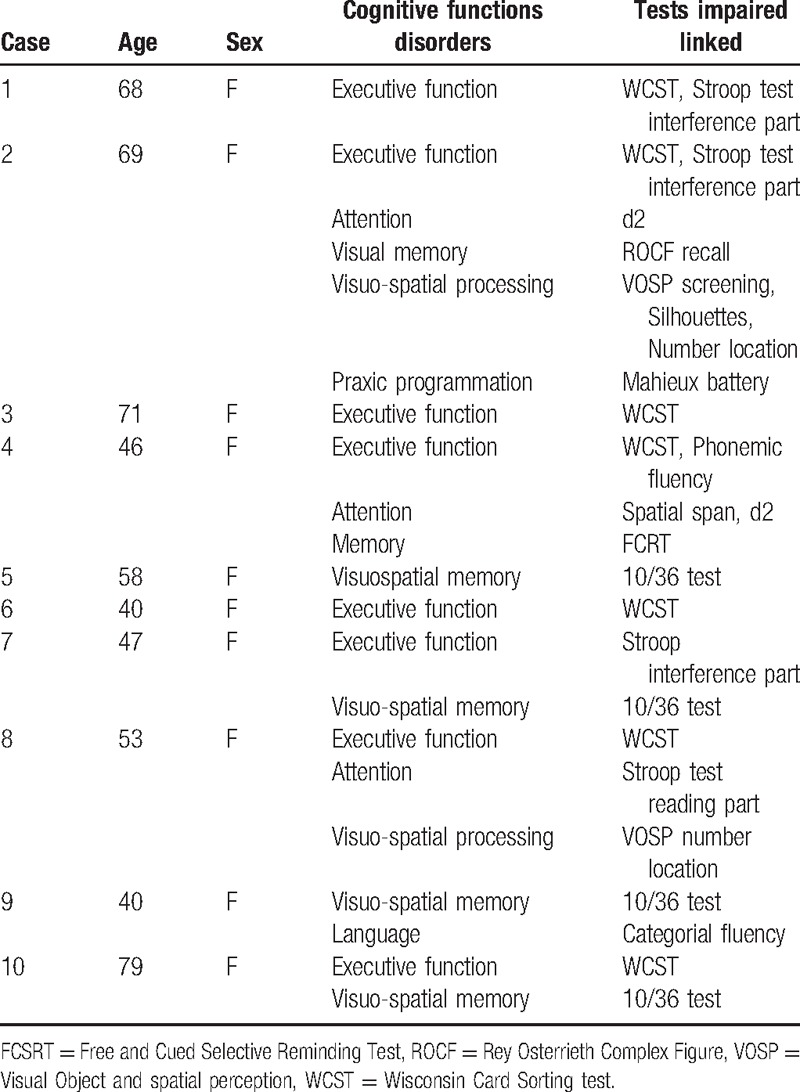
All subject performances are summarized in Table 2. According to our definition, all patients display a normal MMSE (mean MMSE: 28.4 ± 1.17) with a mild cognitive disturbance in several neuropsychological tests: 80% of patients had an executive impairment, 50% had a memory disorder especially on visuo-spatial memory tests, 30% of patients displayed attentional deficits and 20% had visuo-spatial processing disorders. No significant reduction of speed processing was found. The executive domain was the most affected domain in our population and the most sensitive was the WCST. 70% of patients have pathological performances using the WCST, 30% with Stroop test and 10% with the phonemic fluency. Performances on TMT-B, Letter-Number sequencing, and Similarities were normal in all patients. Finally, 10% of patients had praxic programmation disorders and language difficulties, but these findings seem to be linked to an executive disorder of planification or word finding retrieval. Our results were consistent with a fronto-sub-cortical profile associated with memory and visuo-spatial deficits.
Table 2.
Neuropsychological profile by subject with cognitive functions disorders and tests impaired related.
3.3. Health clinical scales and cognition correlations
Figure 1 shows significant correlations between chronic pain and cognitive functioning. The findings reveal that the pain level is correlated with the 3 measures of WCST executive test. We observed a positive correlation with the number of errors and perseverations of this test and a negative correlation with the number of categories found by subject. It means that, in a test of ranking cards where the subject needs to find strategies of classification, the magnitude of the chronic pain has a positive significant correlation with the number of errors and perseverations and negative significant association with the correct category of classification. Hence, the majority of pSS patients with PSFN had difficulties to maintain a complex activity and shifted quickly between strategies depending upon exterior feedbacks.
Figure 1.
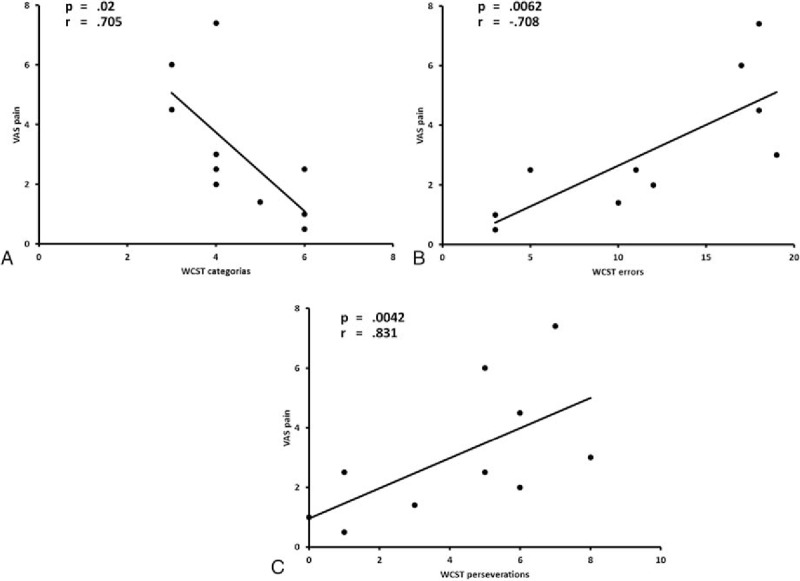
Spearman correlations between pain and the 3 measures of WCST executive test: number of categories (A), number of errors (B), and number of perseverations (C). VAS = Visuo-Anologic Scale, WCST = Wisconsin Card Sorting Test.
The other health clinical questionnaires showed a positive correlation between the levels of pain and anxiety and between anxiety and depression (Fig. 2). There was no correlation between pain and fatigue nor between levels of complaint and all other health clinical measures as well as between executive tests and cognitive complaints.
Figure 2.
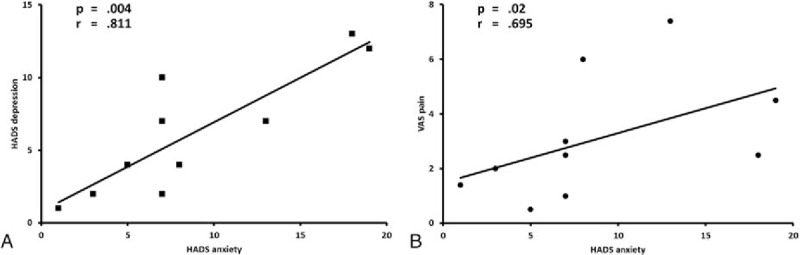
Spearman correlations between anxiety and depression (A) and between pain and Anxiety (B). HADS = Hospital Anxiety and Depression Scale, VAS = Visuo-Anologic Scale.
4. Discussion and literature review
The 10 patients that fulfilled both pSS and PSFN criteria with cognitive complaints have a typical Mild Cognitive Impairment (MCI).[42] A specific cognitive profile of impairment with the 3 measures of WCST was detected, concerning the capacity of abstraction to find adaptative strategies to a given situation, and the ability to maintain a complex thought in memory and to adapt themselves to external feedback. Furthermore, we found a significant and positive correlation between the intensity of pain and the performance of executive functions.
With regard to literature review, 20 articles explored pSS cognition between 1985 and 2016, 17 focused on mild cognitive impairment, and 3 studied dementia in pSS. The main goals of these studies were (1) to explore general neurological complications,[5–7,11] (2) to study the relation between brain imaging and cognitive impairment,[8,12,15–17,43] (3) to assess the impact of clinical features on cognition,[9,18,44] (4) to follow the evolution of cognitive disorders,[45] (5) to describe a study case,[14] (6) to analyze the difference between lupus and pSS,[10] and (7) to adapt a test of cognitive complaint for pSS.[13] Overall, 473 pSS patients were explored and a fronto-sub-cortical alteration with attentional, executive, memory and visuo-spatial disorders was described. However, the prevalence of the cognitive impairment was highly variable in the studies probably due to heterogeneity of patient populations and to analytical factors. On the one hand, patient selection was based on pSS criteria including patients with variable extraglandular manifestations associated or not with cognitive disorders and on the other hand, analytical strategies were variable: 11 studies carried out group analyses compared to control groups,[8–10,12,13,15,16,18,43–45] 12 studies compared patient's performances to normative data,[5–12,15–17,43] whereas 6 reports gave a specific cut-off to define a cognitive impairment.[6,9,10,12,15,43]
Pain is a major clinical symptom of pSS; however, with only 3 studies, the impact of pain on cognition seems underexplored [9,12,13] comparatively to depression (12 studies) [6–10,12,13,16,18,43–45] and fatigue (8 studies).[8–10,12,13,18,44,45] In these 3 studies on pain, Segal et al found discordant results. First, in 2010, the findings did not show any impact of pain on cognitive performance [12] whereas in 2012 and 2014, the new results revealed some involvement of cognitive profiles. In 2014, this author found differences in pain levels according to the intensity of the cognitive complaints [13] and, in 2012, a significant correlation between pain and executive performances particularly with TMT-B and Stroop test in pSS patients was detected.[9]
In contrast in our study, we did not find any correlation with these 2 tests, only with WCST, but pSS patients performed normally TMT-B, only 30% had abnormal performances of Stroop test and 70% had pathological scores of WCST. Taken together, these results seem discordant but Segal et al did not carry out an extensive description of neuropsychological results and have compared only pSS patients to a control group. Hence, pathological performances by test were not available. Moreover, patient selection included subjects with various extraglandular manifestation.
In our homogeneous cohort, we used normative data as in daily clinical practice. With a specific cognitive evaluation, we found a very pathological and congruent cognitive profile in all patients. Moreover, our results are in accordance with Verdejo-Garcia et al[46] showing in patients with fibromyalgia a correlation between levels of pain and WCST and with Segal et al[13] who found differences on WCST between pSS groups with low and high cognitive complaints. Patients with higher subjective cognitive complaints had poorer performances of WCST.
Altogether our results showed that the cognitive evaluation of pSS patients with PSFN using the specific test of WCST seems to be crucial to objectify cognitive impairment as other neuropsychological tests exploring executive functions usually performed. These preliminary results underline the fact that the levels of pain and cognitive complaint are key signs of the presence of a cognitive impairment. Moreover, our results highlight that a better evaluation of cognitive complaints in this population could lead to a better management of pain and to the instauration of a cognitive readaptation to improve the quality of life of these patients. Indeed, some studies in this population have shown that a poor quality of life is mostly correlated with major clinical symptoms as pain or fatigue and with cognitive dysfunctions especially of the executive domain.[44,47]
Our study is an original pilot study to understand and objectify the complaint of our painful pSS patients with PSFN. The small number of included patients is a significant limit and we agree that our results should be considered with caution. The potential impact of some treatments (i.e., benzodiazepine, antidepressive drugs, and anti-epileptic drugs) on neuropsychological symptoms should also be highlighted. Furthermore, some selection bias have to be considered: (1) all patients had a PSFN and, as already reported, display a low rate of anti-nuclear antibody reflecting a peculiar pSS subgroup [3,4,48–50] (2) all patients were complaining about their cognitive functions leading to a possible overestimation of the prevalence of cognitive impairment. Consequently, our conclusion need to be drawn with caution and further studies in larger controlled cohorts including the EULAR SS Patient Reported Index (ESSPRI) score at the date of the neurocognitive evaluation are needed.
In summary, cognitive complaints have to be explored in pSS with PSFN to improve the medical and daily life management. Nevertheless, our first preliminary results showed that chronic pain in pSS needs to be looked after because of its relation with executive disorder, the most important cognitive impairment in pSS that might have the most clear cut impact in professional and daily life.
Acknowledgments
The authors thank the patients who were involved in this study. They also thank Odile Padie and Aurore Halgand for welcoming the patients and caring for them. These persons give us permission to be named in this section.
Footnotes
Abbreviations: ESSDAI = EULAR SS Disease Activity Index, ESSPRI = EULAR SS Patient Reported Index, FCSRT = Free and Cued Selective Reminded Test, HADS = Hospital Anxiety and Depression Scale, MCI = Mild Cognitive Impairment, MMSE = Mini Mental State Examination, PSFN = painful small fiber neuropathy, pSS = primary Sjögren syndrome, ROCF = Rey Osterrieth Complex Figure, SDMT = Symbol digit modalities test, TMT = Trail Making Test, VAS = visual analog scales, VOSP = Visual Object and Spatial Perception, WCST = Wisconsin Card Sorting Test.
CP and DS collaborated equally to the study.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Barendregt PJ, van den Bent MJ, van Raaij-van den Aarssen VJ, et al. Involvement of the peripheral nervous system in primary Sjögren's syndrome. Ann Rheum Dis 2001;60:876–81. [PMC free article] [PubMed] [Google Scholar]
- [2].Garcia-Carrasco M, Ramos-Casals M, Rosas J, et al. Primary Sjögren syndrome: clinical and immunologic disease patterns in a cohort of 400 patients. Medicine 2002;81:270–80. [DOI] [PubMed] [Google Scholar]
- [3].Sene D, Jallouli M, Lefaucheur JP, et al. Peripheral neuropathies associated with primary Sjögren syndrome: immunologic profiles of nonataxic sensory neuropathy and sensorimotor neuropathy. Medicine 2011;90:133–8. [DOI] [PubMed] [Google Scholar]
- [4].Sene D, Cacoub P, Authier FJ, et al. Sjogren syndrome-associated small fiber neuropathy: characterization from a prospective series of 40 cases. Medicine 2013;92:e10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Delalande S, de Seze J, Fauchais AL, et al. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine 2004;83:280–91. [DOI] [PubMed] [Google Scholar]
- [6].Lafitte C, Amoura Z, Cacoub P, et al. Neurological complications of primary Sjögren's syndrome. J Neurol 2001;248:577–84. [DOI] [PubMed] [Google Scholar]
- [7].Morreale M, Marchione P, Giacomini P, et al. Neurological involvement in primary Sjögren syndrome: a focus on central nervous system. PLoS One 2014;9:e84605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mataro M, Escudero D, Ariza M, et al. Magnetic resonance abnormalities associated with cognitive dysfunction in primary Sjögren syndrome. J Neurol 2003;250:1070–6. [DOI] [PubMed] [Google Scholar]
- [9].Segal BM, Pogatchnik B, Holker E, et al. Primary Sjögren's syndrome: cognitive symptoms, mood, and cognitive performance. Acta Neurol Scand 2012;125:272–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Harboe E, Tjensvoll AB, Maroni S, et al. Neuropsychiatric syndromes in patients with systemic lupus erythematosus and primary Sjögren syndrome: a comparative population-based study. Ann Rheum Dis 2009;68:1541–6. [DOI] [PubMed] [Google Scholar]
- [11].Malinow KL, Molina R, Gordon B, et al. Neuropsychiatric dysfunction in primary Sjögren's syndrome. Ann Intern Med 1985;103:344–50. [DOI] [PubMed] [Google Scholar]
- [12].Segal BM, Mueller BA, Zhu X, et al. Disruption of brain white matter microstructure in primary Sjögren's syndrome: evidence from diffusion tensor imaging. Rheumatology (Oxford) 2010;49:1530–9. [DOI] [PubMed] [Google Scholar]
- [13].Segal BM, Rhodus N, Moser Sivils KL, et al. Validation of the brief cognitive symptoms index in Sjögren syndrome. J Rheumatol 2014;41:2027–33. [DOI] [PubMed] [Google Scholar]
- [14].Blanc F, Fleury M, Korganow AS, et al. Cognition disorders and associated behaviors associated with Gougerot–Sjögren syndrome. Rev Neurol (Paris) 2009;165:F267–272. [PubMed] [Google Scholar]
- [15].Blanc F, Longato N, Jung B, et al. Cognitive dysfunction and dementia in primary Sjögren's syndrome. ISRN Neurol 2013;2013:501327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Le Guern V, Belin C, Henegar C, et al. Cognitive function and 99mTc-ECD brain SPECT are significantly correlated in patients with primary Sjögren syndrome: a case-control study. Ann Rheum Dis 2010;69:132–7. [DOI] [PubMed] [Google Scholar]
- [17].Belin C, Moroni C, Caillat-Vigneron N, et al. Central nervous system involvement in Sjögren's syndrome: evidence from neuropsychological testing and HMPAO-SPECT. Ann Med Interne (Paris) 1999;150:598–604. [PubMed] [Google Scholar]
- [18].Epstein LC, Masse G, Harmatz JS, et al. Characterization of cognitive dysfunction in Sjögren's syndrome patients. Clin Rheumatol 2014;33:511–21. [DOI] [PubMed] [Google Scholar]
- [19].Segal BM, Pogatchnik B, Henn L, et al. Pain severity and neuropathic pain symptoms in primary Sjögren's syndrome: a comparison study of seropositive and seronegative Sjögren's syndrome patients. Arthritis Care Res 2013;65:1291–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol 2011;93:385–404. [DOI] [PubMed] [Google Scholar]
- [21].Berryman C, Stanton TR, Jane Bowering K, et al. Evidence for working memory deficits in chronic pain: a systematic review and meta-analysis. Pain 2013;154:1181–96. [DOI] [PubMed] [Google Scholar]
- [22].Devigili G, Tugnoli V, Penza P, et al. The diagnostic criteria for small fibre neuropathy: from symptoms to neuropathology. Brain 2008;131(pt 7):1912–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Association AP. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. 2000. [DOI] [PubMed] [Google Scholar]
- [24].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- [25].Derouesne CDJM, Boyer P, Lubin S, et al. Empirical evaluations of the Cognitive Difficulties Scale for assessment of memory of memory complaints in general practice: a study of 1628 cognitively normal subjects aged 45–75 years. Int J Geriatr Psychiatry 1993;8:599–607. [Google Scholar]
- [26].Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- [27].Grober EBH. Genuine memory deficits in dementia. Dev Neuropsychol 1987;3:13–36. [Google Scholar]
- [28].Dujardin K, Sockeel P, Cabaret M, et al. BCcogSEP: a French test battery evaluating cognitive functions in multiple sclerosis. Rev Neurol (Paris) 2004;160:51–62. [DOI] [PubMed] [Google Scholar]
- [29].A. R. Test de copie et Reproduction de Mémoire de Figures Geométriques Complexes. 1959. [Google Scholar]
- [30].Brickenkamp R ZEaH. The d2 Test of Attention. 1998. [Google Scholar]
- [31].Godefroy O, Azouvi P, Robert P, et al. Dysexecutive syndrome: diagnostic criteria and validation study. Ann Neurol 2010;68:855–64. [DOI] [PubMed] [Google Scholar]
- [32].D. W. Wechsler Adult Intelligence Scale—Third Edition. 1997. [Google Scholar]
- [33].Wechsler D. Wechsler Memory Scale—Third edition. Administration and scoring manual. 1997. [Google Scholar]
- [34].Smith A. Symbol Digits Modalities Test. 1992. [Google Scholar]
- [35].Cardebat D, Doyon B, Puel M, et al. Formal and semantic lexical evocation in normal subjects. Performance and dynamics of production as a function of sex, age and educational level. Acta Neurol Belg 1990;90:207–17. [PubMed] [Google Scholar]
- [36].Metz-Lutz MNKKH, Deloche G. Standardisation d’un test de dénomination orale: contrôle des effets de l’âge, du sexe et du niveau de scolarité chez les sujets adultes normaux. Neuropsychol Rev 1991;1:73–95. [Google Scholar]
- [37].Mahieux-Laurent F, Fabre C, Galbrun E, et al. Groupe de reflexion sur les praxies du CI-d-FS. Validation of a brief screening scale evaluating praxic abilities for use in memory clinics. Evaluation in 419 controls, 127 mild cognitive impairment and 320 demented patients. Rev Neurol (Paris) 2009;165:560–7. [DOI] [PubMed] [Google Scholar]
- [38].Warrington EK JM. The Visual Object and Space Perception Battery. 1991. [Google Scholar]
- [39].Les JP. Eustache AA. Evaluations psychométriques. Editions Solal, Neuropsychologie Clinique Des Démences: Evaluation et Prise en Charge. Marseille: 1995. [Google Scholar]
- [40].Mula M, Trimble MR. Antiepileptic drug-induced cognitive adverse effects: potential mechanisms and contributing factors. CNS Drugs 2009;23:121–37. [DOI] [PubMed] [Google Scholar]
- [41].Cancelli I, Beltrame M, Gigli GL, et al. Drugs with anticholinergic properties: cognitive and neuropsychiatric side-effects in elderly patients. Neurol Sci 2009;30:87–92. [DOI] [PubMed] [Google Scholar]
- [42].Petersen RC. Clinical practice. Mild cognitive impairment. N Engl J Med 2011;364:2227–34. [DOI] [PubMed] [Google Scholar]
- [43].Lauvsnes MB, Maroni SS, Appenzeller S, et al. Memory dysfunction in primary Sjögren's syndrome is associated with anti-NR2 antibodies. Arthritis Rheum 2013;65:3209–17. [DOI] [PubMed] [Google Scholar]
- [44].Kocer B, Tezcan ME, Batur HZ, et al. Cognition depression, fatigue, and quality of life in primary Sjögren's syndrome: correlations. Brain Behav 2016;6:e00586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Martinez S, Caceres C, Mataro M, et al. Is there progressive cognitive dysfunction in Sjögren syndrome? A preliminary study. Acta Neurol Scand 2010;122:182–8. [DOI] [PubMed] [Google Scholar]
- [46].Verdejo-Garcia A, Lopez-Torrecillas F, Calandre EP, et al. Executive function and decision-making in women with fibromyalgia. Arch Clin Neuropsychol 2009;24:113–22. [DOI] [PubMed] [Google Scholar]
- [47].Cornec D, Devauchelle-Pensec V, Mariette X, et al. Severe health-related quality-of-life impairment in active primary Sjögren's syndrome is driven by patient-reported outcomes: data from a large therapeutic trial. Arthritis Care Res 2016;In press. [DOI] [PubMed] [Google Scholar]
- [48].Jamilloux Y, Magy L, Hurtevent JF, et al. Immunological profiles determine neurological involvement in Sjögren's syndrome. Eur J Int Med 2014;25:177–81. [DOI] [PubMed] [Google Scholar]
- [49].Carvajal Alegria G, Guellec D, Mariette X, et al. Epidemiology of neurological manifestations in Sjögren's syndrome: data from the French ASSESS Cohort. RMD Open 2016;2:e000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Birnbaum J. Sensory neuronopathy associated with tumor necrosis factor inhibitor therapy. Neurol Clin Pract 2014;4:516–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


