Abstract
Rationale:
Fracture nonunion is a great challenge for orthopedic surgeons. Many surgical interventions are associated with significant pain and heavy economic burden. Therefore, our aim was to evaluate the outcomes of a new nonoperative treatment for fracture nonunion.
Patient concerns:
A 44-year-old man suffered closed fractures of the right tibia and left femur. Eleven months after surgery, there was no radiographic healing between fracture fragments.
Diagnoses:
Fracture nonunion of the right tibia and left femur.
Interventions:
The patient received systemic treatment with teriparatide (recombinant human Parathyroid Hormone 1–34) 20 μg/d for 8 months, with further observation at 4 months after discontinuation. During treatment, bone metabolic markers were measured to evaluate metabolic activity of osteoblasts and osteoclasts. The Ethics Committee of Qilu Hospital of Shandong University approved this study.
Outcomes:
Satisfactory healing of fracture nonunion was obtained without further intervention.
Lessons:
Anabolic treatment with teriparatide showed a positive effect on healing of fracture nonunion. Evaluation of bone metabolic markers during treatment is necessary to observe the curative effect. In view of the positive effect of teriparatide on healing of fracture nonunion in numerous animal models and clinical studies, it may be a promising alternative treatment for fracture nonunion in patients who are not suitable for surgical intervention.
Keywords: bone metabolic markers, fracture healing, nonunion, teriparatide
1. Introduction
Teriparatide was licensed for treatment of postmenopausal osteoporosis by the US Food and Drug Administration in 2002.[1] In recent years, the efficacy of teriparatide in promoting fracture healing has been reported in numerous animal models [2,3] and clinical studies.[4–6] Fracture nonunion remains a great challenge for orthopedic surgeons. To date, many surgical interventions are associated with significant pain and heavy economic burden. Therefore, based on the positive effect of teriparatide on healing of fracture delayed union or nonunion in previous studies, we present a case of tibial and femoral fracture nonunion treated with teriparatide, which obtained successful healing.
2. Case report
A 44-year-old man suffered closed fractures of the right tibia and left femur in a motor vehicle accident in January 2015. He underwent retrograde intramedullary nailing at another hospital. He had no postoperative infection. Medical history taking revealed no chronic diseases, hypertension, diabetes mellitus, smoking, alcohol abuse, or regular medication. Until 10 months postoperatively, there was no radiographic healing of the right tibia, and the patient experienced persistent pain during weight bearing. Radiographs obtained 11 months postoperatively revealed a persistent fracture gap, sclerosis of the fracture margin, and no evidence of bone bridging at the fracture site (Fig. 1A and B). Therefore, a diagnosis of nonunion was made. There was no clinical sign of infection based on erythrocyte sedimentation rate, C-reactive protein level, and leukocyte count. Other laboratory tests, including parathyroid hormone (PTH), serum alkaline phosphatase, phosphorus, calcium, and 1,25-(OH)2D3, were within normal range. The patient refused to undergo another operation; instead, off-label use of teriparatide was accepted (20 μg ih qd). During the 8 months of treatment, levels of PTH, C-terminal telopeptide of type I collagen (CTX), and N-terminal propeptide of type I collagen (P1NP) were measured at baseline, 1 month, 4 months and 8 months, and at 4 months after discontinuation (Table 1). P1NP and CTX levels were significantly elevated at baseline and maintained a steady state during the treatment period. No adverse effects were observed during or after treatment. After 4 months of treatment, radiographs showed a decrease of the fracture gap and bone bridging between fracture fragments (Fig. 1C and D). After 8 months of treatment, radiographs revealed continuous improvement of the fracture gap (Fig. 1E and F). Then, teriparatide was discontinued. Four months after discontinuation, radiographs showed complete fracture union (Fig. 1G and H). The patient's pain disappeared, and he returned to normal activity.
Figure 1.
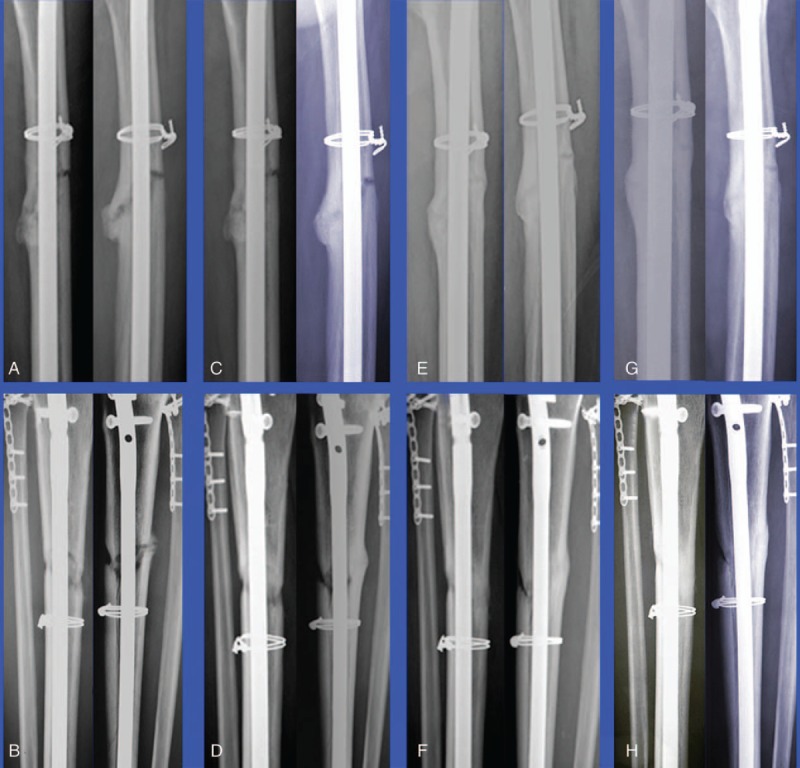
Serial anteroposterior and lateral plain radiographs of left tibial and right femoral fracture nonunion during treatment. (A and B) Nonunion before treatment. (C and D) Nonunion after a 4-month course of teriparatide. (E and F) Nonunion after an 8-month course of teriparatide. (G and H) Healing of nonunion at 4 months after discontinuation of teriparatide.
Table 1.
Changes in bone metabolic markers.

3. Discussion
Teriparatide, as a bone-forming agent, has been used to treat osteoporosis and has become a promising therapeutic agent to improve healing of fracture nonunion. The primary physiologic mechanism of teriparatide involves activation of osteoblasts; intermittently administered teriparatide can shift the bone resorption of osteoclasts to the activation of osteoblasts.[7–9] Teriparatide plays an important role in the coupling of osteolysis and osteogenesis and is an indispensable regulator in remodeling. Teriparatide has been demonstrated to improve the microarchitecture of bone, increase bone mineral density, and reduce the risk of vertebral and nonvertebral fractures.[10] Consistent with these pharmacokinetic characteristics, a rapid increase in biomarkers of bone formation (P1NP) and a gradual increase in biomarkers of bone resorption (CTX) have been observed, demonstrating activation of the metabolic activity of osteoblasts and osteoclasts, referred to as the bone anabolic window.[11] Bone turnover markers are widely used to evaluate metabolic disease, such as Paget disease and osteoporosis, but are used less often to evaluate healing of fracture nounion.[12] However, measurement of the specific molecular markers of osteoblasts and osteoclasts could improve the evaluation of fracture healing and detect the risk of nonunion.[13] P1NP may be a promising marker of nonunion, with 1 previous study showing that it decreased to normal levels during union.[14] In that same study, the changing rate of bone collagen synthesis was closely related to the changing rate of bone formation during fracture healing.
Prominent improvements in callus mineralization and volume, bone mineral content, and rate and strength of successful healing between fracture fragments have been demonstrated in both delayed union and nonunion models.[15] The important role of teriparatide was confirmed in a study by Ren et al,[16] who showed a lack of endogenous PTH (1–84) restrained fracture healing, whereas, if exogenous recombinant human Parathyroid Hormone (1–34) was combined with endogenous PTH (1–84), endochondral bone formation, callus remodeling, and mechanical bone strength were improved to promote fracture healing. Case reports [17,18] also have shown the advantages of teriparatide in cases of fracture nonunion that have innate difficulty in achieving healing. These results imply that teriparatide works effectively when the fracture gap is union, either surgical fixation or nonsurgical.
Today, correlational studies are limited by the deficiency of systematic studies. In view of the limited valid evidence regarding use of teriparatide in cases of chronic fracture nonunion, we depended considerably on retrospective case series and case reports. Nevertheless, the anecdotal evidence of the positive effect of teriparatide on healing of fracture nonunion offers guidance for clinical decision making. Better understanding of this effect may be expounded in future prospective experiments. However, based on our case, teriparatide is a promising anabolic therapy to improve healing of fracture nonunion in patients who are not suitable for surgical intervention.
Acknowledgments
The authors would like to thank the patient and his family for allowing us to use the medical documentation and information that led to the present article.
Footnotes
Abbreviations: CTX = C-terminal telopeptide of type I collagen, P1NP = N-terminal propeptide of type I collagen, PTH = parathyroid hormone.
The authors have no conflicts of interest to disclose.
References
- [1].Rubin MR, Cosman F, Lindsay R, et al. The anabolic effects of parathyroid hormone. Osteoporos Int 2002;13:267–77. [DOI] [PubMed] [Google Scholar]
- [2].Daugaard H, Elmengaard B, Andreassen TT, et al. The combined effect of parathyroid hormone and bone graft on implant fixation. J Bone Joint Surg Br 2011;93:131–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jacobson JA, Yanoso-Scholl L, Reynolds DG, et al. Teriparatide therapy and beta-tricalcium phosphate enhance scaffold reconstruction of mouse femoral defects. Tissue Eng Part A 2011;17:389–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Pietrogrande L, Raimondo E. Teriparatide in the treatment of non-unions: scientific and clinical evidences. Injury 2013;44Suppl 1:S54–7. [DOI] [PubMed] [Google Scholar]
- [5].Lee YK, Ha YC, Koo KH. Teriparatide, a nonsurgical solution for femoral nonunion? A report of three cases. Osteoporos Int 2012;23:2897–900. [DOI] [PubMed] [Google Scholar]
- [6].Chintamaneni S, Finzel K, Gruber BL. Successful treatment of sternal fracture nonunion with teriparatide. Osteoporos Int 2010;21:1059–63. [DOI] [PubMed] [Google Scholar]
- [7].Brunnemann CE, Reisinger EC, Ganzer D, et al. Parathyroid hormone injection to counteract delayed bone fractures. Dtsch Med Wochenschr 2010;135:1538–41. [DOI] [PubMed] [Google Scholar]
- [8].Chen G, Deng C, Li YP. TGF-beta and BMP signaling in osteoblast differentiation and bone formation. Int J Biol Sci 2012;8:272–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Barvencik F. Medication and bone metabolism: clinical importance for fracture treatment. Unfallchirurg 2015;118:1017–24. [DOI] [PubMed] [Google Scholar]
- [10].Nishikawa A, Ishida T, Taketsuna M, et al. Safety and effectiveness of daily teriparatide in a prospective observational study in patients with osteoporosis at high risk of fracture in Japan: final report. Clin Interv Aging 2016;11:913–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Miyauchi A. Relationship of pharmacokinetics, changes of bone turnover markers and BMD/fractures efficacy during treatment with anabolic agents; teriparatide daily and once weekly subcutaneous injections. Clin Calcium 2016;26:1583–95. [PubMed] [Google Scholar]
- [12].Cox G, Einhorn TA, Tzioupis C, et al. Bone-turnover markers in fracture healing. J Bone Joint Surg Br 2010;92:329–34. [DOI] [PubMed] [Google Scholar]
- [13].Coulibaly MO, Sietsema DL, Burgers TA, et al. Recent advances in the use of serological bone formation markers to monitor callus development and fracture healing. Crit Rev Eukaryot Gene Expr 2010;20:105–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Stoffel K, Engler H, Kuster M, et al. Changes in biochemical markers after lower limb fractures. Clin Chem 2007;53:131–4. [DOI] [PubMed] [Google Scholar]
- [15].Komrakova M, Stuermer EK, Werner C, et al. Effect of human parathyroid hormone hPTH (1–34) applied at different regimes on fracture healing and muscle in ovariectomized and healthy rats. Bone 2010;47:480–92. [DOI] [PubMed] [Google Scholar]
- [16].Ren Y, Liu B, Feng Y, et al. Endogenous PTH deficiency impairs fracture healing and impedes the fracture-healing efficacy of exogenous PTH (1–34). PLoS One 2011;6:e23060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mognetti B, Marino S, Barberis A, et al. Experimental stimulation of bone healing with teriparatide: histomorphometric and microhardness analysis in a mouse model of closed fracture. Calcif Tissue Int 2011;89:163–71. [DOI] [PubMed] [Google Scholar]
- [18].Rowshan HH, Parham MA, Baur DA, et al. Effect of intermittent systemic administration of recombinant parathyroid hormone (1–34) on mandibular fracture healing in rats. J Oral Maxillofac Surg 2010;68:260–7. [DOI] [PubMed] [Google Scholar]


