Abstract
Environmental exposure to metals and metalloids is associated with pregnancy loss in some but not all studies. We assessed arsenic, cadmium, mercury, and lead concentrations in 501 couples upon trying for pregnancy and followed them throughout pregnancy to estimate the risk of incident pregnancy loss. Using Cox proportional hazard models, we estimated hazard ratios (HR) and 95% confidence intervals (CIs) for pregnancy loss after covariate adjustment for each partner modeled individually then we jointly modeled both partners’ concentrations. Incidence of pregnancy loss was 28%. In individual partner models, the highest adjusted HRs were observed for female and male blood cadmium (HR=1.08; CI 0.81, 1.44; HR=1.09; 95% CI 0.84, 1.41, respectively). In couple based models, neither partner’s blood cadmium concentrations were associated with loss (HR=1.01; 95% CI 0.75, 1.37; HR=0.92; CI 0.68, 1.25, respectively). We observed no evidence of a significant relation between metal(loids) at environmentally relevant concentrations and pregnancy loss.
Keywords: arsenic, cadmium, epidemiology, lead, mercury, pregnancy, miscarriage, spontaneous abortion
1. Introduction
Contemporary human populations remain at risk for exposure to various environmental metals and metalloids through geographical [1], occupational [2, 3] or accidental contamination pathways [4]. Published reviews have focused on the reproductive and developmental toxicity (RADT) of individual metals and metalloids for human populations, including cadmium [5, 6], lead [7], mercury [8], and arsenic [9, 10]. Pregnancy loss is often considered when assessing the RADT of metal(loid)s, given that it represents embryonic or fetal mortality and has a high (25% to 31%) incidence when measured prospectively [11–14]. A recent review evaluated the collective evidence on the RADT of arsenic (As), cadmium (Cd), copper (Cu), lead (Pb), and mercury (Hg) and concluded that all but Hg were associated with spontaneous abortion [15]. Another review focusing specifically on low levels of metal(loid) exposures and male fertility concluded that evidence was strongest for Cd, Hg and Pb with less certainty for As [16]. Both reviews noted key methodologic limitations that impact the weighing of evidence, particularly very few prospective cohorts with exposures quantified during critical windows of human reproduction and development and adequate attention to potential confounders.
To date, we are unaware of research focusing on male and female partners’ exposures and pregnancy loss despite the couple dependent nature of pregnancy. In contrast to the ubiquitous nature of environmental metals and their designation as endocrine disrupters (EDCs) [17], or exogenous agents that can interfere with any aspect of hormone action [18], there are few epidemiologic studies focusing on metals at environmentally relevant concentrations. To date, much of our understanding about their RADT stems from an important literature focusing on higher exposed populations, such as occupational workers or residents of endemic geographic areas. Moreover pregnancy loss, per se, is not directly measured in most animal research, but rather relies on proxies such as resorption or late fetal deaths. Timing of demise is challenging to determine without prospective measurement. This data gaps precludes our understanding of the impact of metal(loids) on pregnancy loss among populations with environmentally relevant concentrations. Such concentrations are typical of those for most populations without unique occupational or geographical exposures, such as residence in an endemic region. In light of the importance of metal(loid) exposures during critical and sensitive windows of development for pregnancy outcomes, we sought to empirically assess these associations. Motivated by this gap, we sought to explore the individual relationships between environmentally relevant concentrations of three metals (cadmium, lead, mercury), one metalloid (arsenic) and incident pregnancy loss in a cohort of couples prospectively followed across sensitive windows of human reproduction.
2. Materials and Methods
2.1 Study population and participants
The study’s referent cohort is the LIFE Study that comprised 501 reproductive aged couples who were recruited in 2005–2009 upon discontinuing contraception with the intent of becoming pregnant. Using population-based sampling frameworks, we recruited couples from 16 counties in Michigan and Texas of which 42% of eligible individuals enrolled in the study. Complete details are provided elsewhere [19]. By design, inclusion criteria were minimal: female partners aged 18–40 and male partners aged ≥18 years who were in a committed relationship; no physician diagnosis of infertility/sterility; off contraception <2 months; and an ability to communicate in English or Spanish. Female partners also had to have menstrual cycles ranging between 21–42 days as required by the fertility monitor and without the use of injectable hormonal contraceptives in the past year given the uncertain timing for ovulation return. This interval captures the majority of menstruating women in light of its 21-day span. Of the 501 participating couples, the study cohort was restricted to the 344 (68%) pregnant couples (n=3 multiple gestation pregnancies were excluded), since pregnancy is a necessary criterion for loss. All pregnant women were followed through delivery.
2.2 Data collection
Data collection was multi-faceted and included in-person interviews with each partner, standardized anthropometric assessment for the estimation of measured body mass index (BMI), daily preconception journals that captured couples’ lifestyles and home pregnancy test results for female partners. In addition, female partners completed daily early pregnancy journals through 7 weeks post-conception then monthly journals until a loss or delivery. The preconception and early pregnancy (7 post-conception weeks) journal data on lifestyle were used to estimate female partners’ daily cigarette smoking and alcohol consumption during these sensitive windows of human reproduction and development. Male partners only completed daily journals during the preconception window. Approximately 80% of women completed daily journals for the first 7-weeks post-conception and monthly, thereafter, until delivery. All participating research sites received full institutional review board approval, and couples gave written informed consent at enrollment and before any data collection.
2.3 Estimation of conception, pregnancy and loss
Female partners used the Clearblue® Fertility Monitor (Inverness Medical Innovations, Waltham, MA), a urinary based home kit that is intended to help women time intercourse to ovulation to maximize their chances of becoming pregnant. When prompted, the women tested their urine for the detection of estrone-3-glucuronide and luteinizing hormone (LH), which gave a ‘high’ or ‘peak’ fertility prompt on the monitor’s display, respectively. The accuracy of the fertility monitor for detecting the LH surge is 99% [20]. Pregnancy was prospectively captured by women’s use of the Clearblue® digital home pregnancy test, which is sensitive in detecting 25 mIU/mL of human chorionic gonadotropin (hCG) and accurately used by women [21]. This pregnancy test kit has a low (0–0.3%) false positive rate [22]. Depending upon timing of loss, it was detected by conversion to a negative pregnancy test, clinical confirmation or return of menses. We use the term pregnancy loss rather than spontaneous abortion or stillbirth, terms typically defined by estimated gestation, to remove assumptions about the etiologic role of metals in embryonic/fetal mortality, the uncertain timing of actual pregnancy demise, and in light of no standardized endocrine criteria for defining loss [23].
2.4 Trace Element Analyses
At the enrollment home visit, the research nurse obtained whole blood specimens from all participants using supplies pre-screened and certified for trace element analysis. All blood specimens were analyzed for cadmium (Cd), lead (Pb) and mercury (Hg) in the Inorganic and Radiation Analytical Toxicology Branch, at the National Center for Environmental Health, Centers for Disease Control and Prevention (CDC). The analytical method for Pb, Cd and Hg in blood performed at CDC is based on inductively coupled plasma mass spectrometry (ICP-MS), and has been fully validated for use in establishing reference values for the US population via the National Health and Nutrition Examination Surveys [24]. In brief, whole blood is diluted with an alkaline reagent containing appropriate internal standards and analyzed for Pb, Cd and Hg using a PerkinElmer ELAN DRC II ICP-MS (PerkinElmer, Shelton, CT) calibrated with NIST-traceable standards. Method accuracy is assured via analysis of NIST SRM 955c Toxic Elements in Caprine Blood, which is certified for Cd, Pb and Hg at 4 concentration levels. Ongoing laboratory performance is monitored via satisfactory participation in numerous proficiency testing (PT) programs for trace elements in blood, including those operated by Centre de toxicolgie du Québec, and The New York State Department of Health. Typical limits of detection are 0.25 μg/dL for blood Pb, and 0.16 μg/L for both Cd and Hg in blood. In addition to blood, participants also provided a urine specimen that was analyzed for As, Cd and Pb in the Laboratory of Inorganic and Nuclear Chemistry at the Wadsworth Center, New York State Department of Health (NYSDOH) using well-established methods based on ICP-MS [25]. In brief, the Wadsworth Center lab also uses a PerkinElmer ELAN DRC II ICP-MS calibrated with NIST-traceable standards. Method accuracy is assured via analysis of NIST 2668 Toxic Elements in Frozen Human Urine, which is certified for As, Cd and Pb at two mass concentrations. Ongoing laboratory performance is monitored via satisfactory participation in numerous proficiency testing (PT) programs for trace elements in blood, including those operated by Centre de toxicolgie du Québec, the UK Trace Elements External Quality Assessment Scheme, and The New York State Department of Health’s PT program for Trace Elements. Typical limits of detection for As, Cd and Pb in urine are 1 μg/L, 0.02 μg/L, and 0.7 μg/L respectively. For both blood and urine, all instrument derived data, including zeros and negative values, were used for statistical analysis without substitution of values below laboratory LOD to avoid introducing bias when estimating human health outcomes [26, 27].
2.5 Statistical analysis
We first characterized the study cohort by sociodemographic characteristics of partners with significance assessed using either the Chi-square or the Kruskal-Wallis tests. We estimated the distributions of all metal(oids) and summarized them as medians (Md) and interquartile ranges (IQR) with significance by partner estimated with the Wilcoxon-Mann-Whitney test. Time-to-pregnancy loss was estimated using Cox proportional hazard modeling techniques to estimate hazard ratios (HRs) and corresponding 95% confidence intervals for each metal(loid) and partner [28]. We defined time-to-loss as the number of days from observed ovulation as measured by the peak LH day detected by the fertility monitor to the date of reported loss. We used the peak LH day for estimated date of conception, given the short ( 24 hours) survival time of the ovum for fertilization. For 59 (17%) menstrual cycles without ovulation data in the pregnancy cycle, we used the day of LH peak from previous cycles as captured by the fertility monitor. For 16 women (5%) with insufficient ovulation data, we estimated conception as occurring 14 days prior to the first positive pregnancy test. The proportional hazards assumption was assessed using graphical checks based upon martingale residuals, and found to be met.
We modeled each partner’s metal(loid) concentration and time-to-pregnancy loss after log transforming (x+1) exposures to normalize distributions and rescaling by the standard deviation to aid interpretation of the hazard ratios (HRs) and 95% confidence intervals (CIs). Separate models were run for each metal(loid) and partner. Given the low correlation between couples’ metal(loid) exposures, we jointly modeled both partners’ metal(loid) concentrations relative to time-to-pregnancy loss. Specifically, Spearman correlation coefficients for couples’ exposures ranged from 0.26 to 0.28 and 0.40 for urinary Pb, Cd and As, and from 0.40 to 0.41 and 0.55 for blood Pb, Cd and Hg, respectively. We further adjusted all models for age (year, continuous), BMI (≤24.9 lean/normal, 25.0–29.9 overweight and ≥30.0 obese), average number of daily alcoholic beverages consumed and cigarettes (left continuous) smoked prior to conception for both partners and also during early pregnancy for female partners. Because of the uncertainty about the inclusion of prior loss in models, we ran models with and without prior pregnancy loss but conditioned on gravidity, as not all women had a prior pregnancy (no prior pregnancy, prior pregnancy but no loss, prior pregnancy with a loss). For the urine-based metal(loid)s, we also included the log-transformed creatinine concentration (mg/dL) as a covariate. The joint models included covariates for both partners with the exception of age, given their high correlation. Instead, we modeled one partner’s age and the difference in couples’ ages (in years). To ensure a complete analytic file and to minimize selection bias, we imputed missing metal(loid) concentrations and covariates using Markov Chain Monte Carlo methods under the missing at random assumption [29].
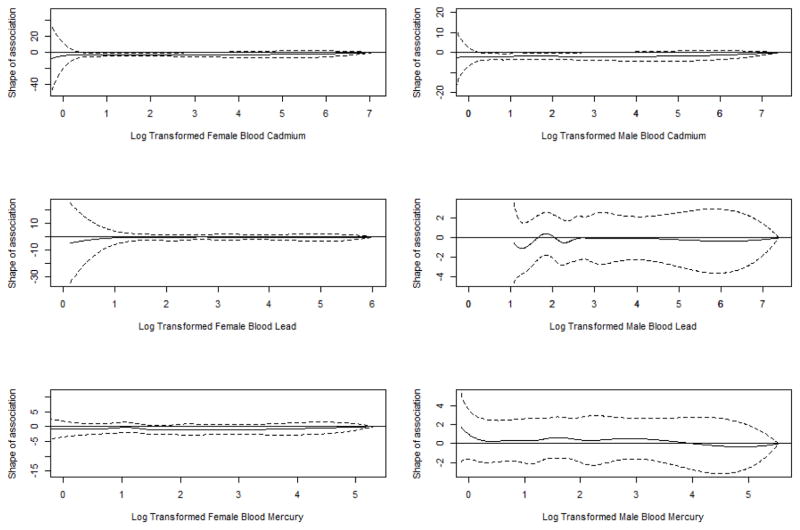
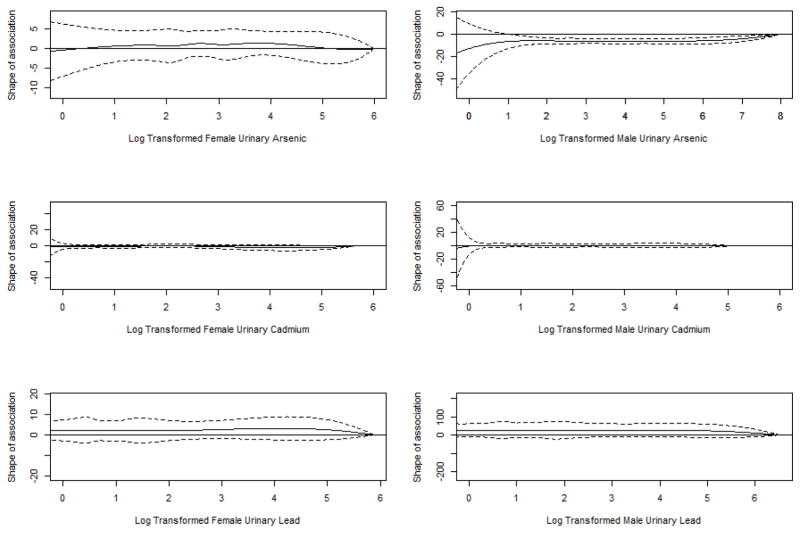
We assessed the linearity assumption underlying the association between metals and time-to-pregnancy loss using splines, and used inverse probability censoring weighting to correct for the couples who did not become pregnant. The weighting was performed in light of our earlier paper showing blood metals to be associated with a longer-time-to pregnancy [30], and to account for couples’ with higher exposures who did not become pregnant and, hence, are not included in the analysis. We used splines to assess any observed departures from linearity or thresholds and observed none (Figures 1 and 2). To this end, we used linear models for assessing exposures and pregnancy loss. We also conducted sensitivity analyses to assess the robustness of our findings. These included restricting our cadmium analysis to partners with concentrations >LOD, and also removing cigarette smoking as a covariate.
Figure 1.
Shape of the associations between the female’s and male partners’ blood metal concentrations and hazard of pregnancy loss - splines.
Findings for female partners are presented in the left-sided figures, and those for males in the right-sided figures.
Figure 2.
Shape of the associations between the female’s and male partners’ blood metal concentrations and hazard of pregnancy loss - splines.
Findings for female partners are presented in the left-sided figures, and those for males in the right-sided figures.
3. Results
Our cohort comprised mostly Non-Hispanic White couples who were highly educated, had household incomes ≥$70,000 and were covered by health insurance (Table 1). The mean ages of female and male partners were 29.8±3.9 and 31.6±4.6 years of age, and their mean BMIs suggested a heavier phenotype (27.0±6.7 and 29.7±5.5, respectively). The distributions for metal(loid)s by biospecimen are presented in Table 2 and reflect slight systematic differences in Md (IQR) concentrations by partner. Prevalence of cigarette smoking was low at enrollment, i.e., 7% and 11% of female and male partners, respectively. With the exception of blood cadmium, most partners had trace element concentrations above the LOD. The average time between enrollment and collection of biospecimens and pregnancy confirmation was 113 ± days.
Table 1.
Description of study cohort by partner.
| Characteristic | Females (n=344) n (%) | Males (n=344) n (%) |
|---|---|---|
| Age (years):a | ||
| 18–24 | 25 (7) | 10 (3) |
| 25–29 | 159 (46) | 113 (33) |
| 30–34 | 116 (34) | 133 (39) |
| ≥35 | 44 (13) | 88 (26) |
| Mean ± SD** | 29.8 ± 3.9 | 31.6 ± 4.6 |
| Body mass index (kg/m2):a | ||
| Lean/normal (≤24.9) | 167 (49) | 59 (17) |
| Overweight (25.0–29.9) | 92 (27) | 141 (41) |
| Obese (≥30.0) | 85 (25) | 144 (42) |
| Mean ± SD** | 27.0 ± 6.7 | 29.7 ± 5.5 |
| Self reported race/ethnicity: | ||
| Non-Hispanic White | 285 (84) | 285 (83) |
| Non-Hispanic Black | 6 (2) | 7 (2) |
| Hispanic | 29 (9) | 27 (8) |
| Other | 21 (6) | 23 (7) |
| Education:a | ||
| ≤High school/equivalent | 15 (4) | 18 (5) |
| College/graduate | 48 (14) | 86 (25) |
| Graduate school | 277 (82) | 237 (70) |
| Household income: | ||
| < $49,999 | 44 (13) | 37 (11) |
| $50,000 to $69,999 | 45 (13) | 53 (16) |
| ≥$70,000 | 246 (73) | 247 (73) |
| Health insurance: | ||
| Yes | 326 (96) | 321 (94) |
| No | 15 (4) | 21 (6) |
| Multivitamin > once/week in the past 3 months:a,b | ||
| Yes | 229 (67) | 158 (46) |
| No | 115 (33) | 186 (54) |
| Cigarette smoking upon enrollment | ||
| No | 321 (93) | 307 (89) |
| Yes | 23 (7) | 37 (11) |
| Average (±SD) # cigarettes/day | 0.49 (2) | 0.97 (3) |
| Average (±SD) # cigarettes/day during pregnancy | ||
| Parity conditional on gravidity: | ||
| Never pregnant | 133 (39) | -- |
| Pregnant, no prior births | 27 (8) | -- |
| Pregnant, ≥1 prior births | 181 (53) | -- |
| Menstrual cycles:b | ||
| Regular | 291 (85) | -- |
| Not regular | 53 (15) | -- |
p <0.001 as estimated with ANOVA techniques and the Chi-square statistic for continuous and categorical data, respectively.
Self-reported by women upon enrollment.
SD, standard deviation
Table 2.
Distribution of metal and metalloid concentrations by biospecimen and partner.
| Biospecimen | Female Partners | Male Partners | ||||
|---|---|---|---|---|---|---|
| % >LOD | Md | IQR | % >LOD | Md | IQR | |
| Blood | ||||||
| Cadmium (μg/L)a | 53 | 0.21 | 0.14, 0.30 | 36 | 0.17 | 0.12, 0.23 |
| Lead (μg/dL)a | 99 | 0.66 | 0.52, 0.82 | 100 | 1.00 | 0.76, 1.37 |
| Mercury (μg/L)b | 88 | 0.98 | 0.54, 1.71 | 91 | 1.18 | 0.62, 2.23 |
| Urine | ||||||
| Arsenic (μg/g)b | 97 | 11.45 | 6.83, 23.08 | 97 | 9.12 | 6.25, 16.52 |
| Cadmium (μg/g)a | 99 | 0.15 | 0.10, 0.22 | 99 | 0.10 | 0.07, 0.15 |
| Lead (μg/g) | 98 | 0.28 | 0.17, 0.44 | 100 | 0.31 | 0.19, 0.47 |
| Creatinine (mg/dL)a | 100 | 73.26 | 33.88, 131.25 | 100 | 145.3 | 70.22, 198.97 |
NOTE: Analysis restricted to the 344 couples achieving pregnancy. Urinary concentrations are creatinine adjusted (μg/g creatinine), and values were imputed for individuals with insufficient samples for quantification. Among study participants, blood and urine specimens were available for 337 and 284 female partners and 340 and 275 male partners, respectively.
Abbreviations: IQR, interquartile range; LOD, limit of detection; Md, median.
p <0.001;
p <0.01;
Wilcoxon-Mann-Whitney tests comparing median female and male metal(loid) concentrations.
None of the metal(loid)s irrespective of biospecimen (blood or urine) was associated with an increased risk of pregnancy loss even after covariate-adjustment (Table 3). In fact most adjusted HRs were around or below one, with only a few adjusted HRs being slightly above 1.0, i.e,, female partners’ blood Cd (1.08; CI 0.81, 1.44) and lead (1.01; CI 0.82, 1.25) concentrations. Only male partners’ blood Cd concentration unadjusted for covariates was positively associated with pregnancy loss (1.19; CI 1.01, 1.40), but the finding was not robust to covariate adjustment (1.09; CI 0.84, 1.41). When jointly modeling partners’ concentrations, females’ blood Cd (1.01; CI 0.75, 1.37) and both blood Pb (1.01; CI 0.80, 1.28) and urinary Pb (1.05; CI 0.83, 1.33) concentrations were positively associated with HR >1.0 when adjusting for covariates and the male partners’ concentrations. In joint models with both partners’ exposures modeled, none of the HRs were above 1 for male partners. Confidence intervals for all metal(loids) included one. Of note, the findings were robust in sensitivity analyses that did not include prior pregnancy history or without using inverse probability weighting (data not shown). The findings remained when removing smoking from the model or when restricting the Cd analysis to individual with concentrations >LOD (data not shown).
Table 3.
Individual partner and couples’ metal and metalloid concentrations and risk of incident pregnancy loss.
| Biospecimen & Partner | Individual Partner Model (n=344) | Couple Model (n=344) | ||
|---|---|---|---|---|
| Unadjusted HR (95% CI) | Adjusteda HR (95% CI) | Unadjusted HR (95% CI) | Adjustedb HR (95% CI) | |
| Female Partners | ||||
| Blood | ||||
| Cadmium (μg/L) | 1.22 (0.98, 1.52) | 1.08 (0.81, 1.44) | 1.15 (0.91, 1.44) | 1.01 (0.75, 1.37) |
| Lead (μg/dL) | 1.07 (0.89, 1.28) | 1.01 (0.82, 1.25) | 1.07 (0.87, 1.32) | 1.01 (0.80, 1.28) |
| Mercury (μg/L) | 0.94 (0.79, 1.12) | 0.90 (0.74, 1.09) | 0.96 (0.78, 1.19) | 0.92 (0.74, 1.16) |
| Urine (μg/g) | ||||
| Arsenic | 1.04 (0.86, 1.26) | 0.94 (0.74, 1.18) | 1.04 (0.85, 1.28) | 0.96 (0.73, 1.25) |
| Cadmium | 1.05 (0.87, 1.27) | 0.96 (0.73, 1.26) | 1.05 (0.86, 1.28) | 0.94 (0.71, 1.24) |
| Lead | 1.11 (0.93, 1.32) | 1.04 (0.84, 1.29) | 1.12 (0.94, 1.35) | 1.05 (0.83, 1.33) |
| Male Partner | ||||
| Blood | ||||
| Cadmium (μg/L) | 1.19 (1.01, 1.40) | 1.09 (0.84, 1.41) | 1.15 (0.97, 1.37) | 0.92 (0.68, 1.25) |
| Lead (μg/dL) | 1.03 (0.86, 1.23) | 0.95 (0.77, 1.17) | 1.00 (0.81, 1.23) | 0.96 (0.77, 1.22) |
| Mercury (μg/L) | 0.94 (0.80, 1.11) | 0.92 (0.77, 1.09) | 0.96 (0.78, 1.18) | 0.95 (0.76, 1.18) |
| Urine (μg/g) | ||||
| Arsenic | 1.01 (0.82, 1.24) | 0.99 (0.78, 1.26) | 0.99 (0.79, 1.24) | 0.95 (0.73, 1.24) |
| Cadmium | 1.02 (0.83, 1.26) | 0.91 (0.68, 1.22) | 1.02 (0.82, 1.26) | 0.87 (0.63, 1.21) |
| Lead | 0.96 (0.80, 1.17) | 0.90 (0.68, 1.19) | 0.94 (0.77, 1.14) | 0.88 (0.67, 1.16) |
NOTE: All metal concentrations were log-transformed (x+1) and rescaled by their standard deviations for analysis. Analysis accounted for inverse probability weighting.
Each partner’s model was adjusted for age (years), body mass index (≤25, 25< BMI <30, ≥30), history of prior loss conditional on gravidity (no prior pregnancy, prior pregnancy without loss, prior pregnancy with loss), and average number of daily alcoholic drinks consumed and cigarettes smoked during the preconception and early pregnancy windows for females and preconception for males. For urinary metals, we also adjusted for creatinine (mg/dL log-transformed) concentrations.
Couple based models adjusted for each partner’s metal concentration, age, difference in couples’ ages, body mass index, average number of daily alcoholic drinks consumed and cigarettes smoked during the preconception and early pregnancy window for females and preconception for males, and history of prior loss conditional on gravidity. For urinary metals, we also adjusted for partner’s creatinine (mg/dL log-transformed) concentrations.
4. Discussion
To our knowledge, our findings are the first to describe the relation between environmental metal(loid)s in a cohort of couples without known unique geographical or occupational exposures, who were recruited prior to conception and followed daily through 7 post-conception weeks and monthly thereafter for the capture of incident pregnancy loss. We did not observe any significant associations between As, Cd, Hg, or Pb and pregnancy loss, and our findings were robust in sensitivity analyses. Other notable study strengths include having individually measured metals in blood and urine for both partners of the couple, along with our ability to detect losses over the course of gestation, including during the preconception and early pregnancy sensitive windows when most losses occur. Our overall incidence of loss was 28% with most losses occurring early and plateauing at approximately 72 post-conception days, as previously reported [11]. Our incidence rate is well within the range (25% to 31%) reported in earlier preconception cohort studies [12–14], increasing our confidence in having captured most losses after the post-implantation window. Still, we do recognize the potential for having missed preimplantation pregnancies or those losses that fail to meet hCG thresholds needed for home pregnancy tests. Nonetheless, our findings are strengthened by having prospectively measured pregnancy loss, rather than relying on retrospectively reported loss that has been shown to underestimate pregnancy loss and disproportionately early losses [31]. In light of 90% of women currently using home pregnancy tests for identifying pregnancy, we feel the findings have relevancy for contemporary populations [http://www.clearblueeasy.com/healthcare/heritage-of-clearblue.php] and are not limited by reliance on retrospectively reported losses. The lack of an association irrespective of measuring metals in blood or (along with As) in urine suggests that neither acute nor chronic exposures at these concentrations, respectively, are associated with loss. Also of note is the relatively comparable distribution of Pb, Cd, Hg and As exposures for our cohort in comparison with U.S. biomonitoring data [24].
Weighing our findings relative to the existing literature is challenging, given that most research has focused on subpopulations with much higher concentrations in light of unique environmental exposures, and most previous research has relied upon self-reported pregnancy loss that may not reflect the continuum of loss across gestation [31]. Our cohort’s exposures were skewed toward lower concentrations, which may explain the lack of observed associations with metal(loids). In the As endemic areas of Bangladesh and West Bengal, India, results from prospective studies of pregnant women did not reflect higher odds of spontaneous abortion even for women with the highest urinary (>200 ug/L) concentrations [32, 33]. However, the latter study did observe an association for stillbirth (OR=6.07; 95% CI 1.54, 24.0). In our study, all losses occurred by 22 weeks precluding our ability to assess stillbirths. No association was noted between As concentrations between 0.8 and 1.9 μg/L in drinking water in a U.S. study and spontaneous abortion [34]. Another study compared estimated As concentrations in drinking water for women with and without pregnancy loss at 5–20 weeks gestation and reported no association for concentrations ranging from 0.0 to 175.1 μg/L [35]. A recent meta analysis assessing As and spontaneous abortion reported greater odds for high (≥50 μg/L) and low-to-moderate (<50 μg/L) concentrations (OR 1.98; 95% CI 1.27, 3.10 and OR 2.02; 95% CI 1.40, 2.91, respectively) [10]. However, none of the odds ratios for the three studies with individually measured low-to-moderate doses achieved significance. Also of interest is the added attention the authors paid to methodology in this review. While the overall odds ratio achieved significance (OR 2.02; 95% CI 1.40, 2.91) even when restricting to studies with biomarker or individual data (2.20; 1.04, 3.46), significance was lost when relying on prospective cohort studies (1.45; 0.99, 2.12) or published research deemed of high quality (>7 on Newcastle-Ottawa Scale) (1.45; 0.99, 1.12).
While small, we observed the highest HRs for female blood Cd concentration and pregnancy loss. Of the few studies focusing on Cd and pregnancy loss, one relied on residence in a polluted area as a proxy of exposure while the other measured blood concentrations in 69 pregnant women. A higher prevalence of reported pregnancy loss was observed for women residing in the contaminated versus uncontaminated area (10% and 2.8%, respectively) [36]. In another study, Nigerian women reporting 3+ prior pregnancy losses had a higher mean blood cadmium level than women without a history (0.46 and 0.25 μg/L; p<0.05) [37]. These Cd concentrations were within range for women in our cohort.
Some of the early evidence in support of lead and pregnancy loss stems from a case control study of pregnant women whose blood lead levels were measured at varying times before 12 weeks gestation with telephone follow-up to ascertain loss [38]. The risk of spontaneous abortion was reported to double per 5 μg/dL increase in blood Pb (OR 1.8; 95% CI 1.1, 3.1). Careful interpretation of the findings is needed in light of a low prevalence of loss (5%). An older review of the literature focusing on Pb exposure and spontaneous abortion concluded that Pb exposure >30 μg/dL in men and between 5–9 μg/dL in women might be associated with an increased risk of spontaneous abortion [7]. In a cross-sectional study of pregnant women enrolled before 14 weeks gestation who were queried on prior history of spontaneous abortion, a 0.1% increase in the plasma/blood Pb ratio was associated with an increase (incidence rate ratio 1.18; p<0.05) in spontaneous abortion history [39]. However, no data were reported on measured plasma and blood Pb concentrations and outcome for the index pregnancy. A recent study focusing on low lead exposure in an occupational cohort of ceramic workers reported a positive trend between regular biomonitoring of exposure and miscarriage in the following 12 months, though prevalence was only 5% [3].
We were unable to locate data focusing on couples’ mercury exposures and pregnancy loss. An earlier and frequently cited occupational study reported that male partners’ urinary Hg concentration >50 μg/L was associated with a doubling (OR=2.26; 95% CI 0.99, 5.23) of the odds of spontaneous abortion in female partners [40]. In some studies, occupational exposure to metallic Hg among dental workers has been linked to menstrual disorders and spontaneous abortion when measuring exposure in hair [41].
Our findings do not support an association between either blood or urinary metal(loid)s at environmentally relevant concentrations and pregnancy loss, corroborating earlier studies reaching similar conclusions for lower relative to higher exposures that might be more reflective for general populations. These findings should not be interpreted as suggesting no potential RADT, as our earlier study focusing on three blood metals reported female cadmium and male lead levels at the environmental concentrations to be associated with diminished fecundity, as measured by a longer time to pregnancy [30]. However, collectively, our findings suggest that specific trace elements may diminish fecundity, but if couples are able to achieve pregnancy they are not at higher risk of loss. This is the rationale for our use of inverse probability weighting to account for couples not achieving pregnancy and who are systematically excluded from the analysis.
Cautious interpretation of our findings is needed in light of potential limitations including the possibility that some pregnancies and losses were missed, though we know of no a priori reason why such misclassification on outcome would be systematically associated with metal concentrations as couples did not know their levels. Model specification is always a concern but we observed little difference in point and interval estimates after adjustments, and our findings were robust in sensitivity analyses, including the removal of history of prior loss from models given the varying perspectives on how best to handle prior history. Another limitation is that we may be underpowered to detect small associations between the exposures and pregnancy loss in the context of our cohort size. Similarly, we may be underpowered to detect possible synergistic effects should they exist. Also, we only had measurements for AS and not metabolites. Perhaps future research capable of delineating mode of actions may help inform how best to weigh evidence from varying exposure profiles [42]. As reiterated for many environmental exposures, continued efforts to assess mixtures of EDCs including metals is needed keeping with the manner in which populations are exposed. The exposome conceptual framework is one such strategy and is well suited to the assessment of RADT [43]. A clearer delineation of the role of metal(loids) at low concentrations might aid communities’ concerns when accidental exposures arise, while working to develop public health initiatives consistent with calls about the preventability of miscarriage and stillbirth [44]. In conclusion, we found no evidence of an adverse relation between any of the metal(loids) considered in this work at environmentally relevant concentrations and incident hCG pregnancy loss.
Highlights.
A preconception cohort had metal(loids) measured to assess risk of incident pregnancy loss.
No significant associations were observed between metal(loids) concentrations and loss.
The findings were robust across partner, biospecimen (blood or urine) and statistical model.
Acknowledgments
Funded by the National Institutes of Health’s Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (contracts N01-HD-3–3355; N01-HD-3–3356; NOH-HD-3–3358; HHSN27500001, and HHSN27500002). Analysis of blood for metals was performed by the Centers for Disease Control and Prevention under an Interagency Agreement with the NICHD. The authors declare they have no known or potential competing financial interests.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hug SM, Joardar JC, Parvin S, Correll R, Naidu R. Arsenic contamination in food-chain: transfer of arsenic into food materials through groundwater irrigation. J Health Popul Nutr. 2006;24:305–316. [PMC free article] [PubMed] [Google Scholar]
- 2.Bonde JPE, Kolstad H. Fertility of Danish battery workers exposed to lead. Int J Epidemiol. 1997;26(6):1281–1288. doi: 10.1093/ije/26.6.1281. [DOI] [PubMed] [Google Scholar]
- 3.Paredes Alpaca R, Forastiere R, Pirani M. Low exposure to lead and reproductive health: a cohort study of female workers in the ceramic industry of Emilia-Romagna (Northern Italy) Epidemiol Prev. 2013;37(6):367–375. [PubMed] [Google Scholar]
- 4.Edwards M. Fetal death and reduced birth rates associated with exposure to lead- contaminated drinking water. Environ Sci Technol. 2013;48:739–746. doi: 10.1021/es4034952. [DOI] [PubMed] [Google Scholar]
- 5.Pollack AZ, Ranasinghe S, Sjaarda LA, Mumford SL. Cadmium and reproductive health in women. A systematic review of the epidemiologic evidence. Curr Environ Health Rep. 2014;1(2):172–184. doi: 10.1007/s40572-014-0013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson J, Bannigan J. Cadmium: toxic effects on the reproductive system and the embryo. Reprod Toxicol. 2008;25:304–315. doi: 10.1016/j.reprotox.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Bellinger DC. Teratogen update: lead and pregnancy. Birth Defects Res (Part A) 2005;73:409–420. doi: 10.1002/bdra.20127. [DOI] [PubMed] [Google Scholar]
- 8.Gardella JR, Hill JA. Environmental toxins associated with recurrent pregnancy loss. Sem Reprod Med. 2000;18(4):407–424. doi: 10.1055/s-2000-13731. [DOI] [PubMed] [Google Scholar]
- 9.Bloom MS, Fitzgerald EF, Kim K, Neamtiu I, Gurzau ES. Spontaneous pregnancy loss in humans and exposure to arsenic in drinking water. Int J Hygiene Environ Health. 2010;213:401–413. doi: 10.1016/j.ijheh.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Quansah R, Armah FA, Essumang DK, Luginaah I, Clarke E, Marfoh K, et al. Association of arsenic with adverse pregnancy outcomes/infant mortality: A systematic review and meta-analysis. Environ Health Perspect. 2015;123(5):412–421. doi: 10.1289/ehp.1307894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buck Louis GM, Sapra KJ, Schisterman EF, Lynch CD, Maisog JM, Grantz KL, et al. Lifestyle and pregnancy loss in a contemporary cohort of women recruited prior to conception, LIFE Study. Fertil Steril. 2016;106(1):180–188. doi: 10.1016/j.fertnstert.2016.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang X, Chen C, Wang L, Chen D, Guang W, French J. Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril. 2003;79:577–584. doi: 10.1016/s0015-0282(02)04694-0. [DOI] [PubMed] [Google Scholar]
- 13.Wilcox AJ, Weinberg CR, O’Connor JF, Baird DD, Schlatterer JP, Canfield RE, et al. Incidence of early loss of pregnancy. New Engl J Med. 1988;319:189–194. doi: 10.1056/NEJM198807283190401. [DOI] [PubMed] [Google Scholar]
- 14.Zinamen MJ, Clegg ED, Brown CC, O’Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996;65:503–509. [PubMed] [Google Scholar]
- 15.Rahman A, Pearson L-A, Nermell B, El Arifeen S, Ekström E-C, Smith AH, et al. Arsenic exposure and risk of spontaneous abortion, stillbirth, and infant mortality. Epidemiol. 2010;21(6):797–804. doi: 10.1097/EDE.0b013e3181f56a0d. [DOI] [PubMed] [Google Scholar]
- 16.Wirth JJ, Mijal RS. Adverse effects of low level heavy metal exposure on male reproductive function. Syst Biol Reprod Med. 2010;56(2):147–167. doi: 10.3109/19396360903582216. [DOI] [PubMed] [Google Scholar]
- 17.Georgescu B, Georgescu C, Daraban S, Bouaru A, Pascalau S. Heavy metals acting as endocrine disrupters. Anim Sci Biotech. 2011;44(2):89–93. [Google Scholar]
- 18.Zoeller RT, Brown TR, Doan LL, Gore AC, Skakkebaek NE, Soto AM, et al. Endocrine-disrupting chemicals and public health protection: a statement of principles from The Endocrine Society. Endocrinology. 2012;153:4097–110. doi: 10.1210/en.2012-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buck Louis GM, Schisterman EF, Sweeney AM, Wilcosky TC, Gore-Langton R, Lynch CD, et al. Designing prospective cohort studies for assessing reproductive and developmental toxicity during sensitive windows of human reproduction and development – the LIFE Study. Paediatr Perinat Epidemiol. 2011;25:413–424. doi: 10.1111/j.1365-3016.2011.01205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Behre HM, Kuhlage J, Gahner C, Sonntag B, Schem C, Schneider HPG, et al. Prediction of ovulation by urinary hormone measurements with the home use ClearPlan® Fertility Monitor: comparison with transvaginal ultrasound scans and serum hormone measurements. Hum Reprod. 2000;15:2478–2482. doi: 10.1093/humrep/15.12.2478. [DOI] [PubMed] [Google Scholar]
- 21.Johnson S, Cushion M, Bond S, Godbert S, Pike J. Comparison of analytical sensitivity and women’s interpretation of home pregnancy tests. Clin Chem Lab Med. 2015;53:391–402. doi: 10.1515/cclm-2014-0643. [DOI] [PubMed] [Google Scholar]
- 22.Tomlinson C, Marshall J, Ellis JE. Comparison of accuracy and certainty of results of six home pregnancy tests available over-the-counter. Curr Med Res Opin. 2008;24:1645–1649. doi: 10.1185/03007990802120572. [DOI] [PubMed] [Google Scholar]
- 23.Lohstroh PN, Overstreet JW, Stewart DR, Nakajima ST, Cragun JR, Boyers SP, et al. Secretion and excretion of human chorionic gonadotropin during early pregnancy. Fertil Steril. 2005;83:1000–1011. doi: 10.1016/j.fertnstert.2004.10.038. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) Fourth National Report on Human Exposure to Environmental Chemicals. Atlanta, GA: 2009. https://www.cdc.gov/exposurereport/pdf/fourthreport.pdf. [Google Scholar]
- 25.Minnich MG, Miller DC, Parsons PJ. Determination of As, Cd, Pb, and Hg in urine using inductively coupled plasma mass spectrometry with the direct injection high efficiency nebulizer. Spectrochim Acta Part B At Spectrosc. 2008;63(3):389–395. [Google Scholar]
- 26.Richardson DB, Ciampi A. Effects of exposure measurement error when an exposure variable is constrained by a lower limit. Am J Epidemiol. 2003;157:355–363. doi: 10.1093/aje/kwf217. [DOI] [PubMed] [Google Scholar]
- 27.Schisterman EF, Vexler A, Whitcomb BW, Liu A. The limitations due to exposure detection limits for regression models. Am J Epidemiol. 2006;163:374–383. doi: 10.1093/aje/kwj039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cox DR. Regression models and life-tables. JRSS, Series B (Methodological) 1972:187–200. [Google Scholar]
- 29.Schafer J. Analysis of incomplete multivariate data. New York: Chapman and Hall; 1997. [Google Scholar]
- 30.Buck Louis GM, Sundaram R, Schisterman EF, Sweeney AM, Lynch CD, Gore-Langton RE, et al. Heavy metals and couple fecundity, the LIFE Study. Chemosphere. 2012;87:1201–1207. doi: 10.1016/j.chemosphere.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilcox AJ, Horney LF. Accuracy of spontaneous abortion recall. Am J Epidemiol. 1984;120(5):727–733. doi: 10.1093/oxfordjournals.aje.a113940. [DOI] [PubMed] [Google Scholar]
- 32.Rahman A, Kumarathasan P, Gomes J. Infant and mother related outcomes from exposures to metals with endocrine disrupting properties during pregnancy. Sci Sci total Environ. 2016 doi: 10.1016/j.scitotenv.2016.06.134. http://dx.doi.org/10.1016/j.scitotenv.2016.06.134. [DOI] [PubMed]
- 33.Von Ehrenstein OS, Guha Mazumder DN, Hira-Smith M, Ghosh N, Yuan Y, Windham G, et al. Pregnancy outcomes, infant mortality, and arsenic in drinking water in West Bengal, India. Am J Epidemiol. 2006;163(7):662–669. doi: 10.1093/aje/kwj089. [DOI] [PubMed] [Google Scholar]
- 34.Aschengrau A, Zierler S, Cohen A. Quality of community drinking water and the occurrence of spontaneous abortion. Arch Environ Health. 1989;44:283–290. doi: 10.1080/00039896.1989.9935895. [DOI] [PubMed] [Google Scholar]
- 35.Bloom MS, Neamtiu JA, Surdu S, Pop C, Rodica Lupsa I, et al. Consumption of low-modeerate level asrsenic contaminated water does not increase spontaneous pregnancy loss: a case control study. Environ Res. 2014;13:81. doi: 10.1186/1476-069X-13-81. http://www.ehjournal.net/content/13/1/81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu SY, Tian J, Wang MZ, Pan BJ, Lu HD, Wang ZM, et al. The effect of cadmium pollution on reproductive health in females. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25(10):852–855. [PubMed] [Google Scholar]
- 37.Ajayi OO, Charles-Davies MA, Arinola OG. Progesterone, selected heavy metals and micronutrients in pregnant Nigerian women with a history of recurrent spontaneous abortion. African Health Sci. 2012;12(2):153–159. doi: 10.4314/ahs.v12i2.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Borja-Aburto VH, Hertz-Picciotto I, Lopez MR, Farias P, Rios C, Blanco J. Blood lead levels measured prospectively and risk of spontaneous abortion. Am J Epidemiol. 1999;150(6):590–597. doi: 10.1093/oxfordjournals.aje.a010057. [DOI] [PubMed] [Google Scholar]
- 39.Lamadrid-Figueroa K, Téllez-Rojo MM, Hernández-Avila M, Trejo-Valdivia B, Solano-González M, Mercado-Garcia A, et al. Association between the plasma/whole blood lead ratio and history of spontaneous abortion: a nested cross-sectional study. BMC Pregnancy Childbirth. 2007;7:22. doi: 10.1186/1471-2393-7-22. http://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cordier S, Deplan F, Mandereau L, Hemon D. Paternal exposure to mercury and spontaneous abortions. Br J Indust Med. 1991;48:375–381. doi: 10.1136/oem.48.6.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sikorski R, Juszkiewicz T, Paszkowski T, Szprengler-Juszkiewicz T. Women in dental surgeries: reproductive hazards in occupational exposure to metallic mercury. Arch Occup Environ Health. 1987;59(6):551–557. doi: 10.1007/BF00377918. [DOI] [PubMed] [Google Scholar]
- 42.Ivicoli I, Fontana L, Bergamaschi A. The effects of metals as endocrine disruptors. J Toxicol Environ Health B Crit Rev. 2009;12(3):206–223. doi: 10.1080/10937400902902062. [DOI] [PubMed] [Google Scholar]
- 43.Buck Louis GM, Yeung E, Sundaram R, Laughon SK, Zhang C. The exposome –exciting opportunities for discoveries in reproductive and perinatal epidemiology. Paediatr Perinat Epidemiol. 2013;27(3):229–236. doi: 10.1111/ppe.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hogue CJ. Preventable pregnancy loss is a public health problem. Invited commentary. Am J Epidemiol. 2016;183(8):709–712. doi: 10.1093/aje/kww004. [DOI] [PubMed] [Google Scholar]